Effectiveness of Graded Weight-Bearing Exercises on Pain, Function, Proprioception, and Muscle Strength in Individuals with Knee Osteoarthritis: A Randomized Controlled Trial
Abstract
1. Introduction
2. Materials and Methods
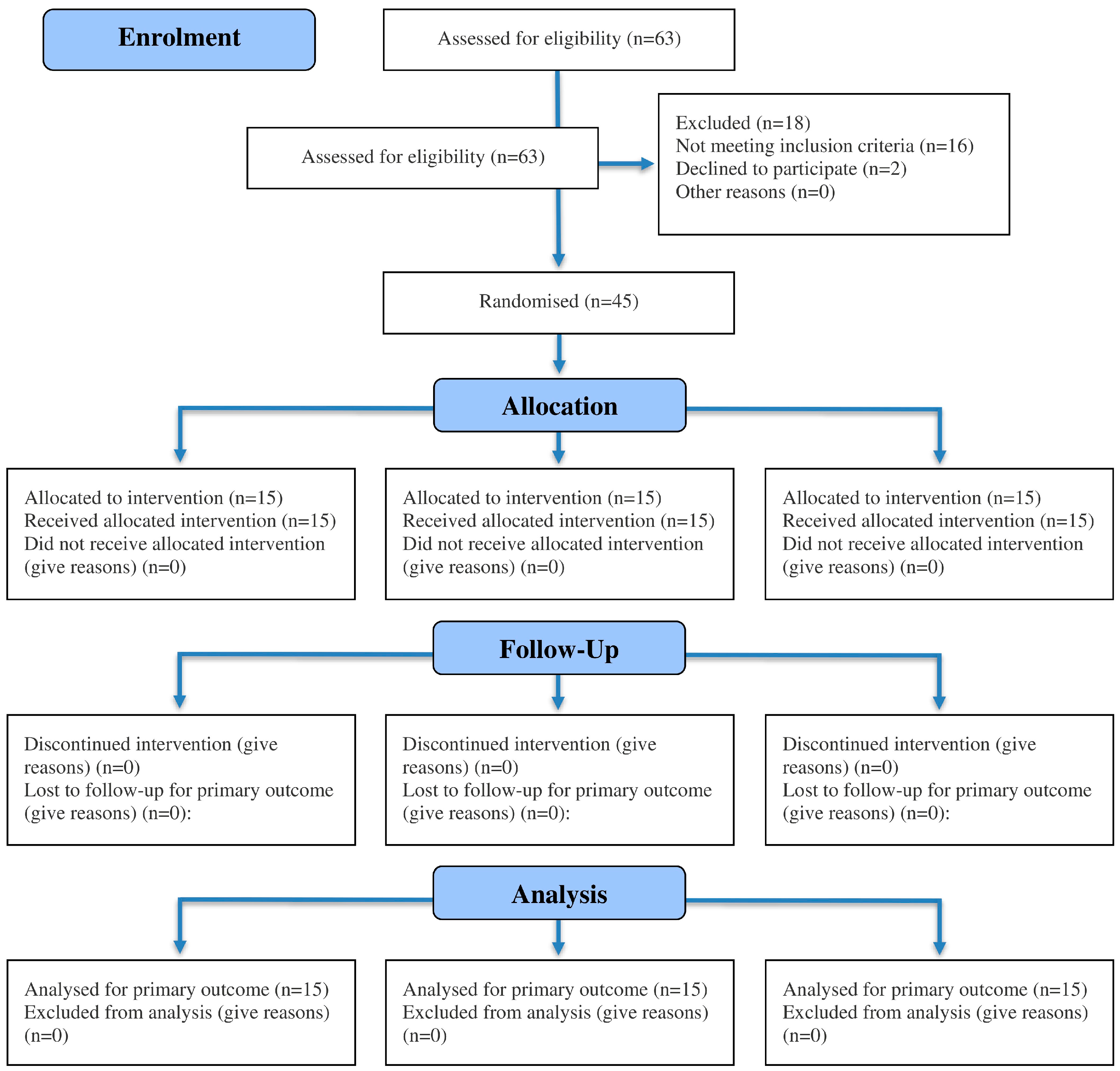
2.1. Study Design
2.2. Recruitment, Allocation, and Blinding
2.3. Power Calculation
2.4. Eligibility Criteria
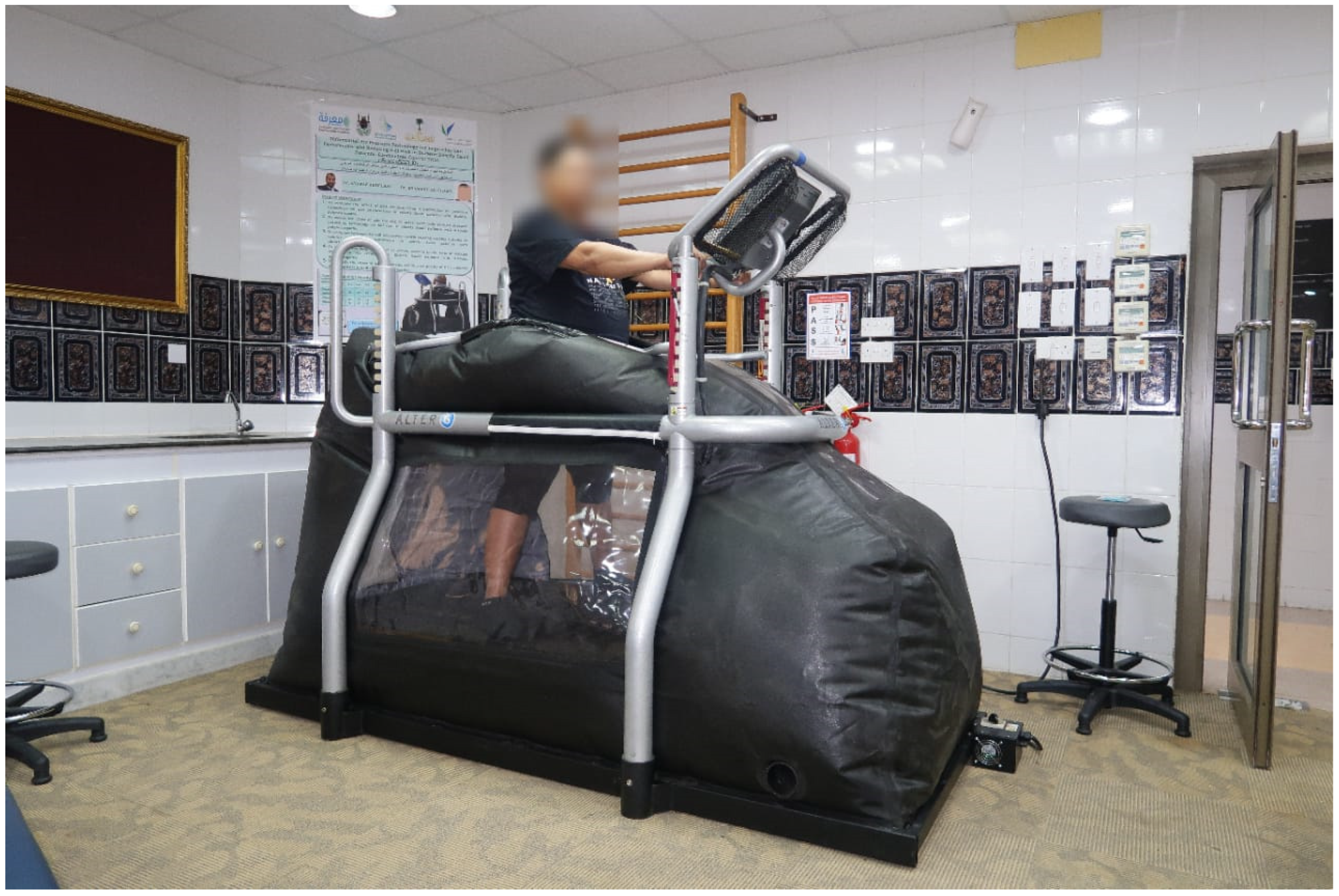
2.5. Interventions
2.6. Outcome Measures
2.7. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| OA | Osteoarthritis |
| Knee OA | Knee osteoarthritis |
| BMI | body mass index |
| CKCE | Closed kinetic chain exercises |
| OKCE | Open kinetic chain exercises |
| GWBE | Graded weight-bearing exercises |
| RCT | Randomized controlled trial |
| VAS | Visual Analogue Scale |
| WOMAC | Western Ontario and McMaster Universities Arthritis Index |
| 6-MWT | Six-Minute Walk Test |
| MT | Muscle torque |
| MANOVA | Multivariate analysis of variance |
| SD | Standard deviation |
| Prop-45 | Proprioception at 45° |
References
- Arden, N.; Blanco, F.; Cooper, C.; Guermazi, A.; Hayashi, D.; Hunter, D.; Javaid, M.K.; Rannou, F.; Roemer, F.; Reginster, J.-Y. Atlas of Osteoarthritis; Springer: London, UK, 2014. [Google Scholar]
- Fransen, M.; McConnell, S.; Harmer, A.R.; van der Esch, M.; Simic, M.; Bennell, K.L. Exercise for osteoarthritis of the knee: A Cochrane systematic review. Br. J. Sports Med. 2015, 49, 1554–1557. [Google Scholar] [CrossRef]
- Cui, A.; Li, H.; Wang, D.; Zhong, J.; Chen, Y.; Lu, H. Global, regional prevalence, incidence and risk factors of knee osteoarthritis in population-based studies. eClinicalMedicine 2020, 29, 100587. [Google Scholar] [CrossRef] [PubMed]
- Al-Arfaj, A.; Al-Boukai, A. Prevalence of radiographic knee osteoarthritis in Saudi Arabia. Clin. Rheumatol. 2002, 21, 142–145. [Google Scholar] [CrossRef]
- Steultjens, M.; Dekker, J.; van Baar, M.; Oostendorp, R.; Bijlsma, J. Range of joint motion and disability in patients with osteoarthritis of the knee or hip. Rheumatology 2000, 39, 955–961. [Google Scholar] [CrossRef]
- Kumm, J.; Tamm, A.; Lintrop, M.; Tamm, A. Association between ultrasonographic findings and bone/cartilage biomarkers in patients with early-stage knee osteoarthritis. Calcif. Tissue Int. 2009, 85, 514–520. [Google Scholar] [CrossRef]
- Rogers, M.W.; Wilder, F.V. The association of BMI and knee pain among persons with radiographic knee osteoarthritis: A cross-sectional study. BMC Musculoskelet. Disord. 2008, 9, 163. [Google Scholar] [CrossRef]
- Liang, J.; Lang, S.; Zheng, Y.; Wang, Y.; Chen, H.; Yang, J.; Luo, Z.; Lin, Q.; Ou, H. The effect of anti-gravity treadmill training for knee osteoarthritis rehabilitation on joint pain, gait, and EMG: Case report. Medicine 2019, 98, e18090. [Google Scholar] [CrossRef]
- Vincent, K.R.; Conrad, B.P.; Fregly, B.J.; Vincent, H.K. The pathophysiology of osteoarthritis: A mechanical perspective on the knee joint. PM R 2012, 4, S3–S9. [Google Scholar] [CrossRef] [PubMed]
- Fadil, A.; Muaidi, Q.I.; Alayat, M.S.; AlMatrafi, N.A.; Subahi, M.S.; Alshehri, M.A. The effectiveness of closed kinetic chain exercises in individuals with knee osteoarthritis: A systematic review and meta-analysis. PLoS ONE 2025, 20, e0322475. [Google Scholar] [CrossRef]
- Bennell, K.L.; Nelligan, R.K.; Kimp, A.J.; Schwartz, S.; Kasza, J.; Wrigley, T.; Metcalf, B.; Hodges, P.; Hinman, R. What type of exercise is most effective for people with knee osteoarthritis and co-morbid obesity? The TARGET randomized controlled trial. Osteoarthr. Cartil. 2020, 28, 755–765. [Google Scholar] [CrossRef] [PubMed]
- Peeler, J.; Christian, M.; Cooper, J.; Leiter, J.; MacDonald, P. Managing knee osteoarthritis: The effects of body weight supported physical activity on joint pain, function, and thigh muscle strength. Clin. J. Sport Med. 2015, 25, 518–523. [Google Scholar] [CrossRef]
- Adegoke, B.O.; Sanya, A.O.; Ogunlade, S.O.; Olagbegi, O.M. The effectiveness of open versus closed kinetic chain exercises on pain, function and range of motion in patients with knee osteoarthritis. Balt. J. Health Phys. Act. 2019, 11, 39–52. [Google Scholar] [CrossRef]
- Brosseau, L.; Taki, J.; Desjardins, B.; Thevenot, O.; Fransen, M.; Wells, G.A.; Imoto, A.M.; Toupin-April, K.; Westby, M.; Gallardo, I.C.Á.; et al. The Ottawa panel clinical practice guidelines for the management of knee osteoarthritis. Part one: Introduction, and mind-body exercise programs. Clin. Rehabil. 2017, 31, 582–595. [Google Scholar] [CrossRef] [PubMed]
- Girgin, N.; Atici, A.; Akpinar, P.; Aktas, I.; Yuksek, F. Effects of open versus closed kinetic chain exercises in patients with knee osteoarthritis. J. Phys. Med. Rehabil. Sci. 2020, 23, 65–72. [Google Scholar] [CrossRef]
- Boonstra, A.M.; Schiphorst Preuper, H.R.; Reneman, M.F.; Posthumus, J.B.; Stewart, R.E. Reliability and validity of the visual analogue scale for disability in patients with chronic musculoskeletal pain. Int. J. Rehabil. Res. 2008, 31, 165–169. [Google Scholar] [CrossRef]
- Alghadir, A.; Anwer, S.; Iqbal, Z.A.; Alsanawi, H.A. Cross-cultural adaptation, reliability and validity of the Arabic version of the reduced Western Ontario and McMaster Universities Osteoarthritis Index in patients with knee osteoarthritis. Disabil. Rehabil. 2016, 38, 689–694. [Google Scholar] [CrossRef] [PubMed]
- van Doormaal, M.C.M.; Meerhoff, G.A.; Vliet Vlieland, T.P.M.; Peter, W.F. A clinical practice guideline for physical therapy in patients with hip or knee osteoarthritis. Musculoskelet. Care 2020, 18, 575–587. [Google Scholar] [CrossRef]
- Dobson, F.; Hinman, R.S.; Hall, M.; Marshall, C.; Sayer, T.; Anderson, C.; Newcomb, N.; Stratford, P.; Bennell, K. Reliability and measurement error of the Osteoarthritis Research Society International (OARSI) recommended performance-based tests of physical function in people with hip and knee osteoarthritis. Osteoarthr. Cartil. 2017, 25, 1792–1796. [Google Scholar] [CrossRef]
- Ateef, M.; Kulandaivelan, S.; Tahseen, S. Test-retest reliability and correlates of 6-minute walk test in patients with primary osteoarthritis of knees. Indian J. Rheumatol. 2016, 11, 192–196. [Google Scholar] [CrossRef]
- Drouin, J.M.; Valovich-McLeod, T.C.; Shultz, S.J.; Gansneder, B.M.; Perrin, D.H. Reliability and validity of the Biodex system 3 pro isokinetic dynamometer velocity, torque and position measurements. Eur. J. Appl. Physiol. 2004, 91, 22–29. [Google Scholar] [CrossRef]
- Sadeghi, H.; Hakim, M.N.; Hamid, T.A.; Bin Amri, S.; Razeghi, M.; Farazdaghi, M.; Shakoor, E. The effect of exergaming on knee proprioception in older men: A randomized controlled trial. Arch. Gerontol. Geriatr. 2017, 69, 144–150. [Google Scholar] [CrossRef]
- Daneshjoo, A.; Sadeghi, H.; Yaali, R.; Behm, D.G. Comparison of unilateral and bilateral strength ratio, strength, and knee proprioception in older male fallers and non-fallers. Exp. Gerontol. 2023, 175, 112161. [Google Scholar] [CrossRef]
- Maffiuletti, N.A.; Bizzini, M.; Desbrosses, K.; Babault, N.; Munzinger, U. Reliability of knee extension and flexion measurements using the Con-Trex isokinetic dynamometer. Clin. Physiol. Funct. Imaging 2007, 27, 346–353. [Google Scholar] [CrossRef]
- Lai, Z.; Lee, S.; Chen, Y.; Wang, L. Comparison of whole-body vibration training and quadriceps strength training on physical function and neuromuscular function of individuals with knee osteoarthritis: A randomised clinical trial. J. Exerc. Sci. Fit. 2021, 19, 150–157. [Google Scholar] [CrossRef]
- Moreira, V.M.P.S.; da Silva Soares, F.; Hattori, W.T.; Dionisio, V.C. A comparison of the efficacy of nonweight-bearing and weight-bearing exercise programmes on function and pain pressure thresholds in knee osteoarthritis: A randomised study. Eur. J. Physiother. 2021, 23, 171–178. [Google Scholar] [CrossRef]
- Desai, R.R.; Damsam, A.R.; Palekar, T.J. Efficacy of open versus closed kinetic chain exercises on dynamic balance and health status in individuals with osteoarthritis of knee joint: A quasi-experimental study. J. Clin. Diagn. Res. 2022, 16, YC01–YC05. [Google Scholar] [CrossRef]
- Fox, R.; Daunton, N.; Corcoran, M. Study of adaptation to altered gravity through systems analysis of motor control. Adv. Space Res. 1998, 22, 245–253. [Google Scholar] [CrossRef]
- Ferreira, L.G.P.; Genebra, C.V.D.S.; Maciel, N.M.; Arca, E.A.; Fiorelli, A.; Vitta, A.D. Multisensory and closed kinetic chain exercises on the functional capacity and balance in elderly women: Blinded randomized clinical trial. Fisioter. Mov. 2017, 30, 259–266. [Google Scholar] [CrossRef]
- Molla, R.Y.; Sadeghi, H.; Kahlaee, A.H. The effect of early progressive resistive exercise therapy on balance control of patients with total knee arthroplasty: A randomized controlled trial. Top. Geriatr. Rehabil. 2017, 33, 286–294. [Google Scholar] [CrossRef]
- Jan, M.H.; Lin, J.J.; Liau, J.J.; Lin, Y.F.; Lin, D.H. Investigation of clinical effects of high- and low-resistance training for patients with knee osteoarthritis: A randomized controlled trial. Phys. Ther. 2008, 88, 427–436. [Google Scholar] [CrossRef] [PubMed]
- Jan, M.H.; Lin, C.H.; Lin, Y.F.; Lin, J.J.; Lin, D.H. Effects of weight-bearing versus nonweight-bearing exercise on function, walking speed, and position sense in participants with knee osteoarthritis: A randomized controlled trial. Arch. Phys. Med. Rehabil. 2009, 90, 897–904. [Google Scholar] [CrossRef]
- Lin, D.H.; Lin, Y.F.; Chai, H.M.; Han, Y.C.; Jan, M.H. Comparison of proprioceptive functions between computerized proprioception facilitation exercise and closed kinetic chain exercise in patients with knee osteoarthritis. Clin. Rheumatol. 2007, 26, 520–528. [Google Scholar] [CrossRef] [PubMed]
- Patil, S.; Steklov, N.; Bugbee, W.D.; Goldberg, T.; Colwell, C.W., Jr.; D’Lima, D.D. Anti-gravity treadmills are effective in reducing knee forces. J. Orthop. Res. 2013, 31, 672–679. [Google Scholar] [CrossRef] [PubMed]
- Miyoshi, T.; Shirota, T.; Yamamoto, S.I.; Nakazawa, K.; Akai, M. Effect of the walking speed on the lower limb joint angular displacements, joint moments and ground reaction forces during walking in water. Disabil. Rehabil. 2004, 26, 724–732. [Google Scholar] [CrossRef]
- Palke, L.; Schneider, S.; Karich, B.; Mende, M.; Josten, C.; Böhme, J.; Henkelmann, R. Anti-gravity treadmill rehabilitation improves gait and muscle atrophy in patients with surgically treated ankle and tibial plateau fractures after one year: A randomised clinical trial. Clin. Rehabil. 2022, 36, 87–98. [Google Scholar] [CrossRef]
- Baizabal-Carvallo, J.F.; Alonso-Juarez, M.; Fekete, R. Anti-gravity treadmill training for freezing of gait in Parkinson’s disease. Brain Sci. 2020, 10, 739. [Google Scholar] [CrossRef] [PubMed]
- Duran, U.D.; Duran, M.; Tekin, E.; Demir, Y.; Aydemir, K.; Aras, B.; Yasar, E. Comparison of the effectiveness of anti-gravity treadmill exercises and underwater walking exercises on cardiorespiratory fitness, functional capacity and balance in stroke patients. Acta Neurol. Belg. 2023, 123, 423–432. [Google Scholar] [CrossRef]
| Characteristics | GWBE + OCKE | CKCE + OCKE | OCKE | p Value |
|---|---|---|---|---|
| Age | 52.6 ± 5.7 | 51.4 ± 4.9 | 51.8 ± 6.3 | 0.840 |
| Female, N (%) | 14 (93%) | 10 (66%) | 12 (85%) | - |
| Weight | 89.4 ± 18.6 | 97.2 ± 13.8 | 93.4 ± 17.3 | 0.447 |
| Height | 165.6 ± 9.3 | 167 ± 9.8 | 165.4 ± 8.7 | 0.876 |
| BMI | 37.6 ± 5.8 | 37.8 ± 6.3 | 37.3 ± 5.9 | 0.974 |
| Duration of illness | 38.3 ± 8.7 | 42.7 ± 9.2 | 41.2 ± 7.6 | 0.365 |
| K-L score—grade II | 9 (60%) | 11 (73%) | 8 (53%) | - |
| K-L score—grade III | 6 (40%) | 4 (40%) | 7 (47%) | - |
| Variable | GWBE + OCKE | CKCE + OCKE | OCKE | p Value | |
|---|---|---|---|---|---|
| VAS | Pre-treatment | 5.94 ± 0.71 | 6.04 ± 0.71 | 6.27 ± 0.99 | 0.5274 |
| Post-treatment | 1.69 ± 0.42 | 2.20 ± 0.66 | 2.36 ± 0.39 | 0.0021 a | |
| Mean difference | 4.253 | 3.847 | 3.913 | ||
| p value | <0.0001 b | <0.0001 b | <0.0001 b | ||
| WOMAC | Pre-treatment | 61.13 ± 4.32 | 62.00 ± 3.87 | 61.86 ± 3.50 | 0.8088 |
| Post-treatment | 37.73 ± 4.61 | 42.73 ± 3.26 | 45.73 ± 3.73 | <0.0001 a | |
| Mean difference | 23.4 | 19 | 16.133 | ||
| p value | <0.0001 b | <0.0001 b | <0.0001 b | ||
| 6-MWT | Pre-treatment | 306.40 ± 18.38 | 303.53 ± 16.04 | 305.30 ± 13.25 | 0.8857 |
| Post-treatment | 337.67 ± 11.84 | 321.00 ± 14.45 | 314.00 ± 14.64 | <0.0001 a | |
| Mean difference | −31.267 | −17.467 | −8.733 | ||
| p value | <0.0001 b | <0.0001 b | <0.0001 b | ||
| Prop-45 | Pre-treatment | 6.10 ± 0.18 | 6.22 ± 0.21 | 6.24 ± 0.23 | 0.1304 |
| Post-treatment | 4.67 ± 0.36 | 5.93 ± 0.23 | 6.17 ± 0.28 | <0.0001 a | |
| Mean difference | 1.427 | 0.2933 | 0.07333 | ||
| p value | <0.0001 b | <0.0001 b | 0.0853 | ||
| MT-60°/s | Pre-treatment | 78.87 ± 7.77 | 76.33 ± 7.02 | 73.80 ± 6.37 | 0.1592 |
| Post-treatment | 80.06 ± 8.77 | 76.73 ± 6.96 | 73.86 ± 6.61 | 0.0893 | |
| Mean difference | −1.2 | −0.4 | −0.066 | ||
| p value | 0.0510 | 0.4793 | 0.8800 | ||
| MT-120°/s | Pre-treatment | 59.46 ± 4.29 | 60.80 ± 5.07 | 61.60 ± 5.70 | 0.5110 |
| Post-treatment | 60.06 ± 4.89 | 61.93 ± 5.80 | 61.46 ± 6.18 | 0.6450 | |
| Mean difference | −0.6 | −1.13 | 0.133 | ||
| p value | 0.1442 | 0.2254 | 0.7284 | ||
| MT-180°/s | Pre-treatment | 45.73 ± 5.23 | 46.60 ± 3.66 | 44.33 ± 5.39 | 0.4377 |
| Post-treatment | 45.86 ± 5.43 | 47.66 ± 3.86 | 44.60 ± 5.95 | 0.2735 | |
| Mean difference | −0.1333 | −1.06 | −0.2667 | ||
| p value | 0.8178 | 0.4400 | 0.6330 |
| Variable | Group | Comparison | MD | p Value | |
|---|---|---|---|---|---|
| VAS | Pre-treatment | GWBE + OCKE | CKCE + OCKE | −0.106 | p > 0.05 b |
| GWBE + OCKE | OCKE | −0.33 | p > 0.05 b | ||
| CKCE + OCKE | OCKE | −0.22 | p > 0.05 b | ||
| Post-treatment | GWBE + OCKE | CKCE + OCKE | −0.5133 | 0.0250 a | |
| GWBE + OCKE | OCKE | −0.6733 | 0.0020 a | ||
| CKCE + OCKE | OCKE | −0.16 | p > 0.05 b | ||
| WOMAC | Pre-treatment | GWBE + OCKE | CKCE + OCKE | −0.8667 | p > 0.05 b |
| GWBE + OCKE | OCKE | −0.7333 | p > 0.05 b | ||
| CKCE + OCKE | OCKE | 0.1333 | p > 0.05 b | ||
| Post-treatment | GWBE + OCKE | CKCE + OCKE | −5.267 | 0.0020 a | |
| GWBE + OCKE | OCKE | −8 | 0.0001 a | ||
| CKCE + OCKE | OCKE | −2.73 | p > 0.05 b | ||
| 6-MWT | Pre-treatment | GWBE + OCKE | CKCE + OCKE | 2.867 | p > 0.05 b |
| GWBE + OCKE | OCKE | 1.133 | p > 0.05 b | ||
| CKCE + OCKE | OCKE | −1.733 | p > 0.05 b | ||
| Post-treatment | GWBE + OCKE | CKCE + OCKE | 16.667 | 0.0050 a | |
| GWBE + OCKE | OCKE | 23.667 | 0.0001 a | ||
| CKCE + OCKE | OCKE | 7 | p > 0.05 b | ||
| Prop-45 | Pre-treatment | GWBE + OCKE | CKCE + OCKE | −0.1193 | p > 0.05 b |
| GWBE + OCKE | OCKE | −0.146 | p > 0.05 b | ||
| CKCE + OCKE | OCKE | −0.02667 | p > 0.05 b | ||
| Post-treatment | GWBE + OCKE | CKCE + OCKE | −1.253 | 0.0001 a | |
| GWBE + OCKE | OCKE | −1.5 | 0.0001 a | ||
| CKCE + OCKE | OCKE | −0.2467 | p > 0.05 b | ||
| MT-60°/s | Pre-treatment | GWBE + OCKE | CKCE + OCKE | 2.533 | p > 0.05 b |
| GWBE + OCKE | OCKE | 5.067 | p > 0.05 b | ||
| CKCE + OCKE | OCKE | 2.533 | p > 0.05 b | ||
| Post-treatment | GWBE + OCKE | CKCE + OCKE | 3.333 | p > 0.05 b | |
| GWBE + OCKE | OCKE | 6.2 | p > 0.05 b | ||
| CKCE + OCKE | OCKE | 2.86 | p > 0.05 b | ||
| MT-120°/s | Pre-treatment | GWBE + OCKE | CKCE + OCKE | −1.33 | p > 0.05 b |
| GWBE + OCKE | OCKE | −2.13 | p > 0.05 b | ||
| CKCE + OCKE | OCKE | −0.8 | p > 0.05 b | ||
| Post-treatment | GWBE + OCKE | CKCE + OCKE | −1.86 | p > 0.05 b | |
| GWBE + OCKE | OCKE | −1.4 | p > 0.05 b | ||
| CKCE + OCKE | OCKE | 0.46 | p > 0.05 b | ||
| MT-180°/s | Pre-treatment | GWBE + OCKE | CKCE + OCKE | −0.86 | p > 0.05 b |
| GWBE + OCKE | OCKE | 1.4 | p > 0.05 b | ||
| CKCE + OCKE | OCKE | 2.2 | p > 0.05 b | ||
| Post-treatment | GWBE + OCKE | CKCE + OCKE | −1.8 | p > 0.05 b | |
| GWBE + OCKE | OCKE | 1.26 | p > 0.05 b | ||
| CKCE + OCKE | OCKE | 3.06 | p > 0.05 b |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Fadil, A.; Muaidi, Q.I.; Alayat, M.S.; Subahi, M.S.; Sroge, R.A.; Awali, A.; Alshehri, M.A. Effectiveness of Graded Weight-Bearing Exercises on Pain, Function, Proprioception, and Muscle Strength in Individuals with Knee Osteoarthritis: A Randomized Controlled Trial. J. Clin. Med. 2025, 14, 7685. https://doi.org/10.3390/jcm14217685
Fadil A, Muaidi QI, Alayat MS, Subahi MS, Sroge RA, Awali A, Alshehri MA. Effectiveness of Graded Weight-Bearing Exercises on Pain, Function, Proprioception, and Muscle Strength in Individuals with Knee Osteoarthritis: A Randomized Controlled Trial. Journal of Clinical Medicine. 2025; 14(21):7685. https://doi.org/10.3390/jcm14217685
Chicago/Turabian StyleFadil, Ammar, Qassim Ibrahim Muaidi, Mohamed Salaheldien Alayat, Moayad S. Subahi, Roaa A. Sroge, Abdulaziz Awali, and Mansour Abdullah Alshehri. 2025. "Effectiveness of Graded Weight-Bearing Exercises on Pain, Function, Proprioception, and Muscle Strength in Individuals with Knee Osteoarthritis: A Randomized Controlled Trial" Journal of Clinical Medicine 14, no. 21: 7685. https://doi.org/10.3390/jcm14217685
APA StyleFadil, A., Muaidi, Q. I., Alayat, M. S., Subahi, M. S., Sroge, R. A., Awali, A., & Alshehri, M. A. (2025). Effectiveness of Graded Weight-Bearing Exercises on Pain, Function, Proprioception, and Muscle Strength in Individuals with Knee Osteoarthritis: A Randomized Controlled Trial. Journal of Clinical Medicine, 14(21), 7685. https://doi.org/10.3390/jcm14217685







