A Comparison of Health-Related Quality of Life in Patients with Periprosthetic Joint Infection, Patients with Fracture-Related Infections and the General Population—A Multicenter Analysis of 384 Patients from the Section “Musculoskeletal Infections” of the German Society for Orthopaedics and Traumatology
Abstract
1. Introduction
2. Materials and Methods
Statistical Analysis
3. Results
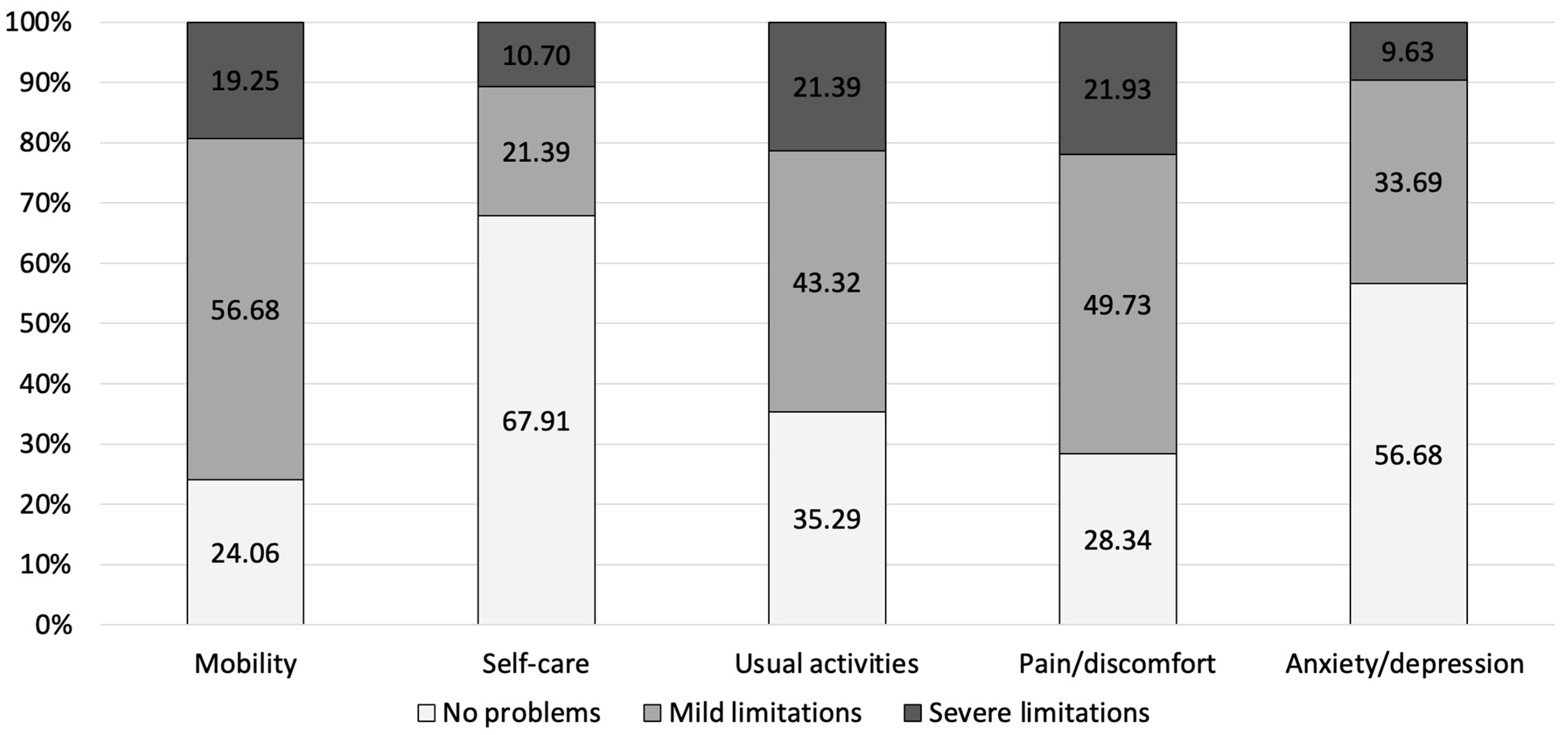
3.1. HRQoL in PJI and FRI Patients
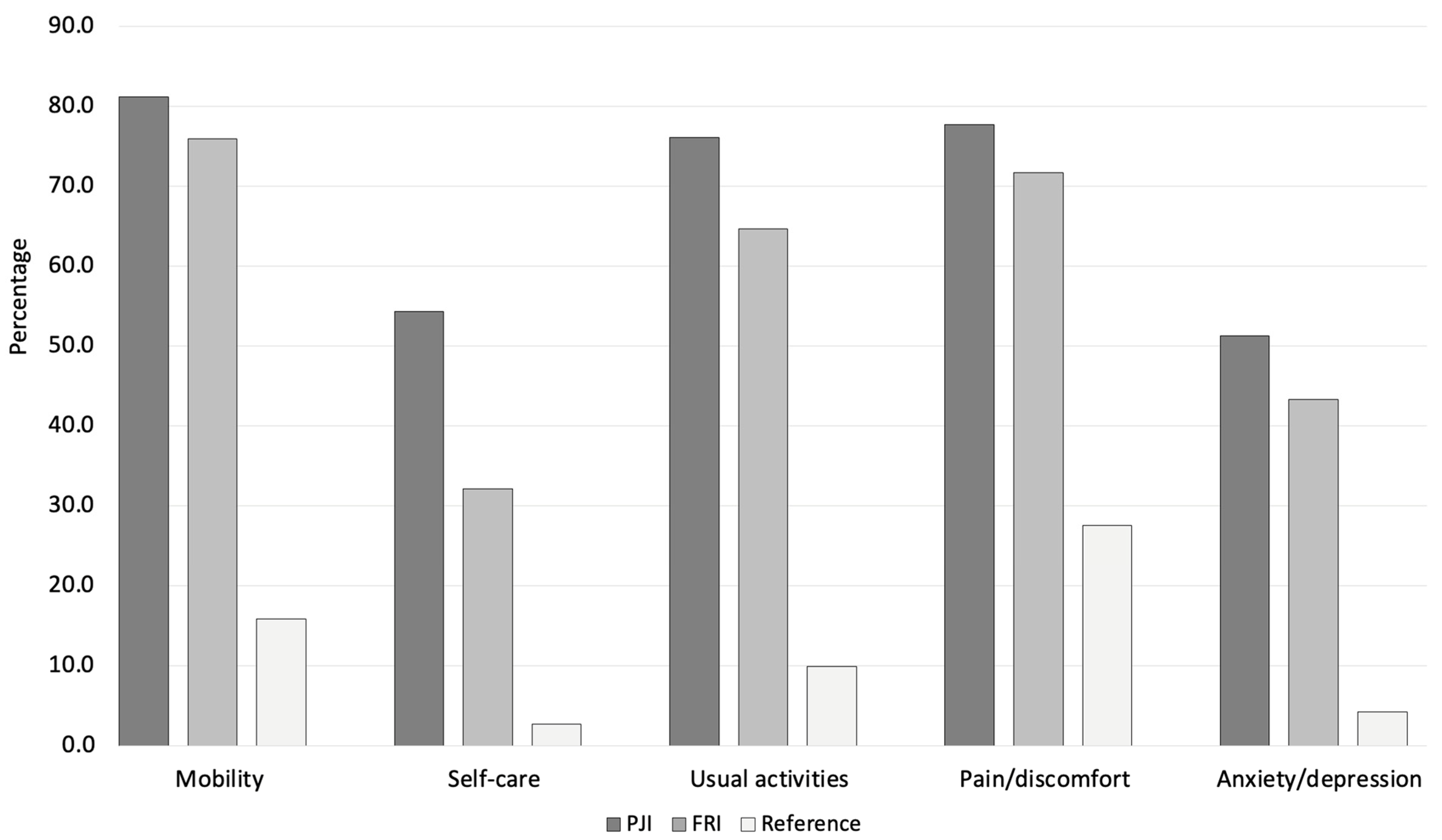
3.2. Comparison of HRQoL Outcomes Between PJI and FRI Patients with Age-Matched Reference Data from the German General Population
3.3. Comparison of HRQoL Between Patients with PJI and FRI
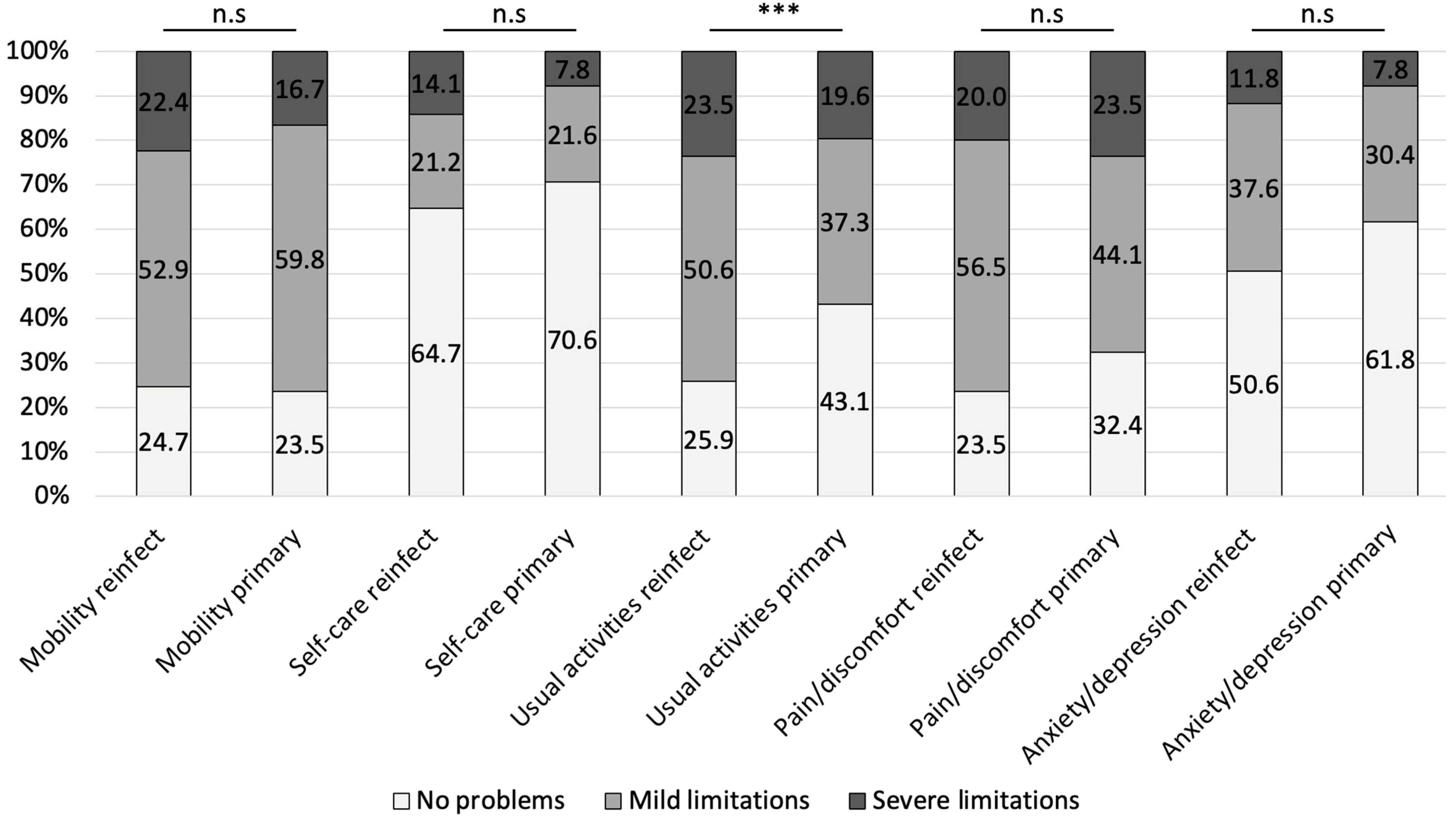
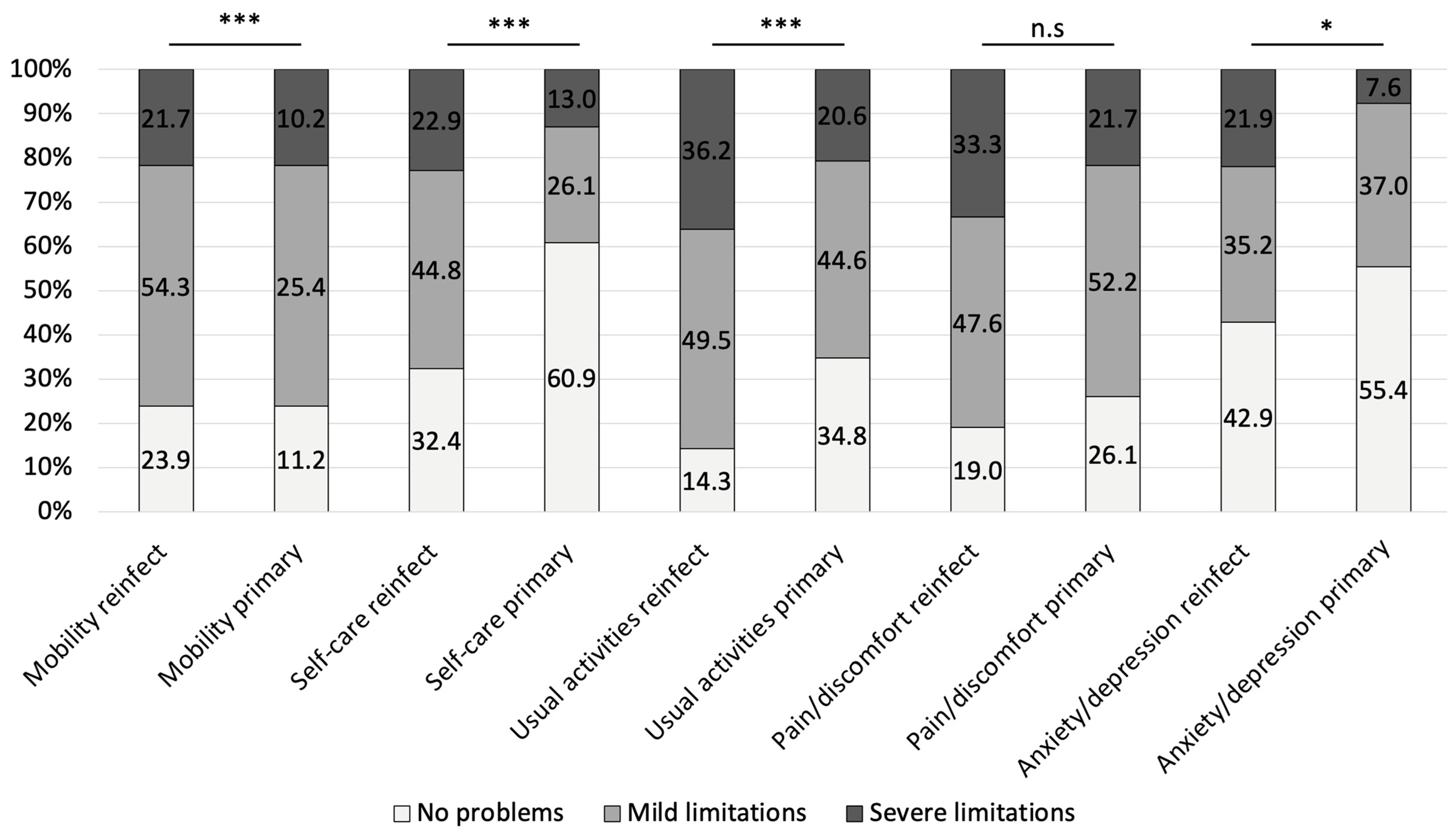
3.4. Impact of Recurrence of Infection After Index Treatment Versus Primary Infection on Patient-Reported HRQoL Outcomes
4. Discussion
Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Nelson, S.B.; Pinkney, J.A.; Chen, A.F.; Tande, A.J. Periprosthetic Joint Infection: Current Clinical Challenges. Clin. Infect. Dis. 2023, 77, e34–e45. [Google Scholar] [CrossRef] [PubMed]
- Moriarty, T.F.; Metsemakers, W.-J.; Morgenstern, M.; Hofstee, M.I.; Vallejo Diaz, A.; Cassat, J.E.; Wildemann, B.; Depypere, M.; Schwarz, E.M.; Richards, R.G. Fracture-Related Infection. Nat. Rev. Dis. Primer 2022, 8, 67. [Google Scholar] [CrossRef]
- Alt, V.; McNally, M.; Wouthuyzen-Bakker, M.; Metsemakers, W.-J.; Marais, L.; Zalavras, C.; Morgenstern, M. The FRI Classification—A New Classification of Fracture-Related Infections. Injury 2024, 55, 111831. [Google Scholar] [CrossRef]
- Harris, E.; Clement, N.; MacLullich, A.; Farrow, L. The Impact of an Ageing Population on Future Increases in Hip Fracture Burden: Insights from the Scottish Hip Fracture Audit. Bone Jt. J. 2024, 106-B, 62–68. [Google Scholar] [CrossRef]
- Shichman, I.; Roof, M.; Askew, N.; Nherera, L.; Rozell, J.C.; Seyler, T.M.; Schwarzkopf, R. Projections and Epidemiology of Primary Hip and Knee Arthroplasty in Medicare Patients to 2040–2060. JB JS Open Access 2023, 8, e22.00112. [Google Scholar] [CrossRef]
- Pan, X.; Wang, J.; Lin, Z.; Dai, W.; Shi, Z. Depression and Anxiety Are Risk Factors for Postoperative Pain-Related Symptoms and Complications in Patients Undergoing Primary Total Knee Arthroplasty in the United States. J. Arthroplast. 2019, 34, 2337–2346. [Google Scholar] [CrossRef]
- Harmer, J.R.; Wyles, C.C.; Duong, S.Q.; Morgan Iii, R.J.; Maradit-Kremers, H.; Abdel, M.P. Depression and Anxiety Are Associated with an Increased Risk of Infection, Revision, and Reoperation Following Total Hip or Knee Arthroplasty. Bone Jt. J. 2023, 105-B, 526–533. [Google Scholar] [CrossRef]
- Lueck, E.; Schlaepfer, T.E.; Schildberg, F.A.; Randau, T.M.; Hischebeth, G.T.; Jaenisch, M.; Ossendorff, R.; Wirtz, D.C.; Wimmer, M.D. The Psychological Burden of a Two-Stage Exchange of Infected Total Hip and Knee Arthroplasties. J. Health Psychol. 2022, 27, 470–480. [Google Scholar] [CrossRef]
- Wimalan, B.; Rupp, M.; Alt, V.; Walter, N. The Patients’ Perspective—A Qualitative Analysis of Experiencing a Fracture-Related Infection. Front. Psychol. 2023, 14, 1126826. [Google Scholar] [CrossRef] [PubMed]
- Aichmair, A.; Pastl, D.; Frank, B.J.H.; Simon, S.; Mitterer, J.A.; Dominkus, M.; Hofstaetter, J.G. High Demand for Psychological Support in Patients Who Have Periprosthetic Hip and Knee Joint Infections: An Analysis of 13,976 Patients. J. Arthroplast. 2024, 39, 2575–2580. [Google Scholar] [CrossRef] [PubMed]
- Knebel, C.; Menzemer, J.; Pohlig, F.; Herschbach, P.; Burgkart, R.; Obermeier, A.; Von Eisenhart-Rothe, R.; Mühlhofer, H.M.L. Peri-Prosthetic Joint Infection of the Knee Causes High Levels of Psychosocial Distress: A Prospective Cohort Study. Surg. Infect. 2020, 21, 877–883. [Google Scholar] [CrossRef]
- Walter, N.; Loew, T.; Hinterberger, T.; Alt, V.; Rupp, M. Managing More than Bones: The Psychological Impact of a Recurrent Fracture-Related Infection. Bone Jt. Open 2024, 5, 621–627. [Google Scholar] [CrossRef]
- McNally, M.; Sousa, R.; Wouthuyzen-Bakker, M.; Chen, A.F.; Soriano, A.; Vogely, H.C.; Clauss, M.; Higuera, C.A.; Trebše, R. The EBJIS Definition of Periprosthetic Joint Infection: A Practical Guide for Clinicians. Bone Jt. J. 2021, 103-B, 18–25. [Google Scholar] [CrossRef]
- Metsemakers, W.J.; Morgenstern, M.; McNally, M.A.; Moriarty, T.F.; McFadyen, I.; Scarborough, M.; Athanasou, N.A.; Ochsner, P.E.; Kuehl, R.; Raschke, M.; et al. Fracture-Related Infection: A Consensus on Definition from an International Expert Group. Injury 2018, 49, 505–510. [Google Scholar] [CrossRef]
- Devlin, N.; Parkin, D.; Janssen, B. An Introduction to EQ-5D Instruments and Their Applications. In Methods for Analysing and Reporting EQ-5D Data; Springer International Publishing: Cham, Switherland, 2020; pp. 1–22. ISBN 978-3-030-47621-2. [Google Scholar]
- Szende, A.; Janssen, B.; Cabases, J. (Eds.) Self-Reported Population Health: An International Perspective Based on EQ-5D; Springer: Dordrecht, The Netherlands, 2014; ISBN 978-94-007-7595-4. [Google Scholar]
- Cohen, J. Statistical Power Analysis for the Behavioral Sciences; Routledge: London, UK, 2013; ISBN 978-1-134-74270-7. [Google Scholar]
- Hegde, V.; Bracey, D.N.; Johnson, R.M.; Dennis, D.A.; Jennings, J.M. Increased Prevalence of Depressive Symptoms in Patients Undergoing Revision for Periprosthetic Joint Infection. Arthroplast. Today 2022, 13, 69–75. [Google Scholar] [CrossRef] [PubMed]
- Walter, N.; Rupp, M.; Baertl, S.; Hinterberger, T.; Alt, V. Prevalence of Psychological Comorbidities in Bone Infection. J. Psychosom. Res. 2022, 157, 110806. [Google Scholar] [CrossRef] [PubMed]
- Krenn, V.T.; Bönigk, M.S.; Trampuz, A.; Liebisch, M.; Perka, C.; Meller, S. Coping with Chronic Periprosthetic Joint Infection after Failed Revision of Total Knee and Hip Arthroplasty: A Qualitative Study on Patient’s Experiences in Treatment and Healing. PLoS ONE 2025, 20, e0319509. [Google Scholar] [CrossRef]
- Mur, I.; Jordán, M.; Rivera, A.; Pomar, V.; González, J.C.; López-Contreras, J.; Crusi, X.; Navarro, F.; Gurguí, M.; Benito, N. Do Prosthetic Joint Infections Worsen the Functional Ambulatory Outcome of Patients with Joint Replacements? A Retrospective Matched Cohort Study. Antibiotics 2020, 9, 872. [Google Scholar] [CrossRef]
- Wildeman, P.; Rolfson, O.; Söderquist, B.; Wretenberg, P.; Lindgren, V. What Are the Long-Term Outcomes of Mortality, Quality of Life, and Hip Function after Prosthetic Joint Infection of the Hip? A 10-Year Follow-up from Sweden. Clin. Orthop. 2021, 479, 2203–2213. [Google Scholar] [CrossRef]
- Shichman, I.; Sobba, W.; Beaton, G.; Polisetty, T.; Nguyen, H.B.; Dipane, M.V.; Hayes, E.; Aggarwal, V.K.; Sassoon, A.A.; Chen, A.F.; et al. The Effect of Prosthetic Joint Infection on Work Status and Quality of Life: A Multicenter, International Study. J. Arthroplast. 2023, 38, 2685–2690.e1. [Google Scholar] [CrossRef] [PubMed]
- Walter, N.; Mohokum, M.; Loew, T.; Rupp, M.; Alt, V. Healing beyond the Joint: Addressing Mental Health in Periprosthetic Joint Infection in a Prospective Longitudinal Study. J. Psychosom. Res. 2024, 177, 111559. [Google Scholar] [CrossRef]
- Walter, N.; Loew, T.; Hinterberger, T.; Mohokum, M.; Alt, V.; Rupp, M. Mental Health Implications of Fracture-Related Infections: A Longitudinal Quality of Life Study. Bone Jt. Res. 2025, 14, 136–142. [Google Scholar] [CrossRef]
- Khalili, P.; Tevell, S.; Fischer, P.; Hailer, N.P.; Wolf, O. Analysis of Fracture-Related Infections from Swedish Insurance Claims between 2011 and 2021. Sci. Rep. 2023, 13, 22662. [Google Scholar] [CrossRef]
- Buijs, M.A.S.; Haidari, S.; IJpma, F.F.A.; Hietbrink, F.; Govaert, G.A.M. What Can They Expect? Decreased Quality of Life and Increased Postoperative Complication Rate in Patients with a Fracture-Related Infection. Injury 2024, 55, 111425. [Google Scholar] [CrossRef] [PubMed]
- Walter, N.; Rupp, M.; Hierl, K.; Pfeifer, C.; Kerschbaum, M.; Hinterberger, T.; Alt, V. Long-Term Patient-Related Quality of Life after Fracture-Related Infections of the Long Bones. Bone Jt. Res. 2021, 10, 321–327. [Google Scholar] [CrossRef] [PubMed]
- Rupp, M.; Walter, N.; Popp, D.; Hitzenbichler, F.; Heyd, R.; Geis, S.; Kandulski, M.; Thurn, S.; Betz, T.; Brochhausen, C.; et al. Multidisciplinary Treatment of Fracture-Related Infection Has a Positive Impact on Clinical Outcome—A Retrospective Case Control Study at a Tertiary Referral Center. Antibiotics 2023, 12, 230. [Google Scholar] [CrossRef] [PubMed]
- Carlson, V.R.; Dekeyser, G.J.; Certain, L.; Pupaibool, J.; Gililland, J.M.; Anderson, L.A. Clinical Experience with a Coordinated Multidisciplinary Approach to Treating Prosthetic Joint Infection. Arthroplast. Today 2020, 6, 360–362. [Google Scholar] [CrossRef]
- Hotchen, A.J.; Wismayer, M.G.; Robertson-Waters, E.; McDonnell, S.M.; Kendrick, B.; Taylor, A.; Alvand, A.; McNally, M. The Joint-Specific BACH Classification: A Predictor of Outcome in Prosthetic Joint Infection. eClinicalMedicine 2021, 42, 101192. [Google Scholar] [CrossRef] [PubMed]

| Variable | PJI |
|---|---|
| Total number of patients | 197 |
| Mean age in years | 70.1 ± 11.1 |
| Sex (female/male) | 85/112 |
| Anatomical localization | |
| Hip | 107 (54.3%) |
| Knee | 79 (40.1%) |
| Shoulder | 11 (5.6%) |
| Patients with prior infection | 92 (46.7%) |
| Number of surgeries for index treatment | 1.8 (range 1–8) |
| Recurrence of infection | 36 (18.3%) |
| Variable | FRI |
|---|---|
| Total number of patients | 187 |
| Mean age in years | 58.0 ± 15.0 |
| Sex (female/male) | 69/118 |
| Anatomical localization | |
| Femur | 23 (12.3%) |
| Acetabulum | 3 (1.6%) |
| Tibia | 94 (50.3%) |
| Fibula | 6 (3.2%) |
| Ankle | 22 (11.8%) |
| Foot | 13 (7.0%) |
| Ulna | 2 (1.1%) |
| Radius | 5 (2.7%) |
| Patients with prior infection | 57 (30.5%) |
| Number of surgeries for index treatment | 2.5 (range 1–16) |
| Recurrence of infection | 48 (25.7%) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Gramlich, Y.; Walter, N.; Frese, J.; Steinhausen, E.S.; Holz, M.; Lazic, I.; Morgenstern, M.; Schaper, B.; Gravius, S.; Hansberg, J.; et al. A Comparison of Health-Related Quality of Life in Patients with Periprosthetic Joint Infection, Patients with Fracture-Related Infections and the General Population—A Multicenter Analysis of 384 Patients from the Section “Musculoskeletal Infections” of the German Society for Orthopaedics and Traumatology. J. Clin. Med. 2025, 14, 7649. https://doi.org/10.3390/jcm14217649
Gramlich Y, Walter N, Frese J, Steinhausen ES, Holz M, Lazic I, Morgenstern M, Schaper B, Gravius S, Hansberg J, et al. A Comparison of Health-Related Quality of Life in Patients with Periprosthetic Joint Infection, Patients with Fracture-Related Infections and the General Population—A Multicenter Analysis of 384 Patients from the Section “Musculoskeletal Infections” of the German Society for Orthopaedics and Traumatology. Journal of Clinical Medicine. 2025; 14(21):7649. https://doi.org/10.3390/jcm14217649
Chicago/Turabian StyleGramlich, Yves, Nike Walter, Jasper Frese, Eva Simone Steinhausen, Mathias Holz, Igor Lazic, Mario Morgenstern, Björn Schaper, Sascha Gravius, Jobst Hansberg, and et al. 2025. "A Comparison of Health-Related Quality of Life in Patients with Periprosthetic Joint Infection, Patients with Fracture-Related Infections and the General Population—A Multicenter Analysis of 384 Patients from the Section “Musculoskeletal Infections” of the German Society for Orthopaedics and Traumatology" Journal of Clinical Medicine 14, no. 21: 7649. https://doi.org/10.3390/jcm14217649
APA StyleGramlich, Y., Walter, N., Frese, J., Steinhausen, E. S., Holz, M., Lazic, I., Morgenstern, M., Schaper, B., Gravius, S., Hansberg, J., Gruszka, D., Clauss, M., Schnetz, M., Schoop, R., Janoud, S., Schlossmacher, B., Christensen, J.-H., Meller, S., & Alt, V. (2025). A Comparison of Health-Related Quality of Life in Patients with Periprosthetic Joint Infection, Patients with Fracture-Related Infections and the General Population—A Multicenter Analysis of 384 Patients from the Section “Musculoskeletal Infections” of the German Society for Orthopaedics and Traumatology. Journal of Clinical Medicine, 14(21), 7649. https://doi.org/10.3390/jcm14217649









