Symmetry After Breast Reconstruction Surgery: A Comparison of Immediate vs. Delayed-Immediate Breast Reconstruction Using Smartphone-Based 3D Surface Imaging
Abstract
1. Introduction
2. Material and Methods
2.1. Study Protocol
2.2. Patient Preparation
2.3. Three-Dimensional Data Acquisition
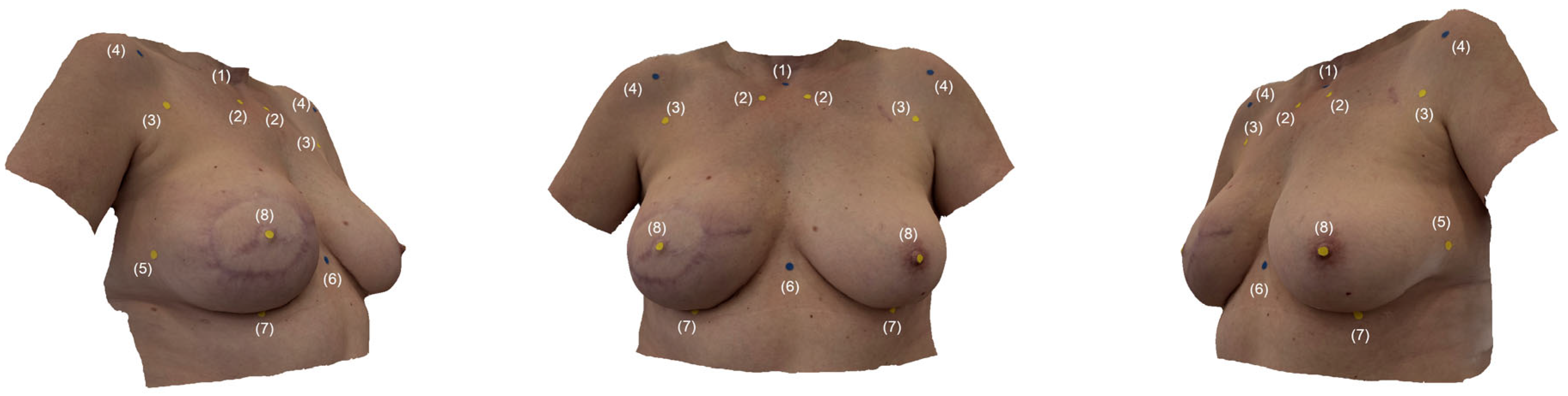
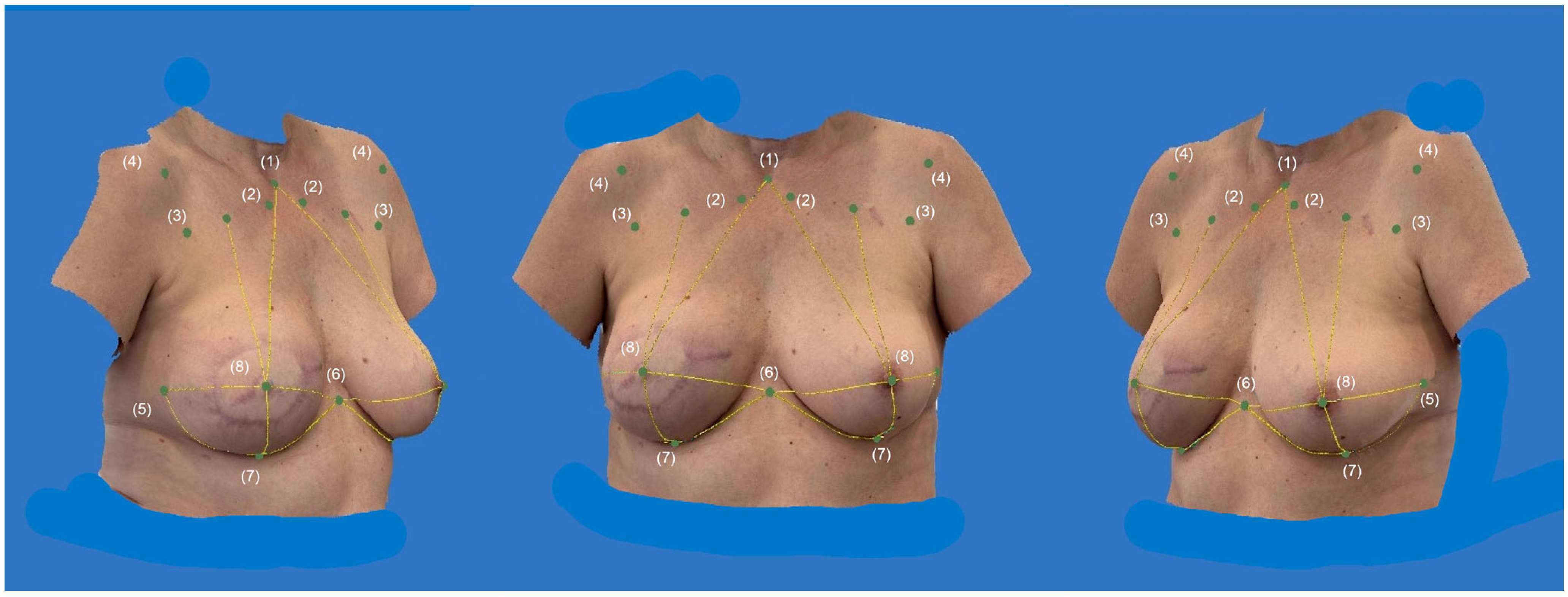
2.4. Digital Anthropometric Examination
2.5. Statistical Analysis
3. Results
3.1. Patient Demographics
3.2. Anthropometric Examination and Symmetry Index
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Bray, F.; Laversanne, M.; Sung, H.; Ferlay, J.; Siegel, R.L.; Soerjomataram, I.; Jemal, A. Global cancer statistics 2022: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J. Clin. 2024, 74, 229–263. [Google Scholar] [CrossRef] [PubMed]
- Siegel, R.L.; Giaquinto, A.N.; Jemal, A. Cancer statistics, 2024. CA Cancer J. Clin. 2024, 74, 12–49. [Google Scholar] [CrossRef] [PubMed]
- Gerber, B.; Marx, M.; Untch, M.; Faridi, A. Breast Reconstruction Following Cancer Treatment. Dtsch. Aerzteblatt Online 2015, 112, 593. [Google Scholar] [CrossRef] [PubMed]
- Houghton, S.C.; Hankinson, S.E. Cancer Progress and Priorities: Breast Cancer. Cancer Epidemiol. Biomark. Prev. 2021, 30, 822–844. [Google Scholar] [CrossRef] [PubMed]
- Kronowitz, S.J.; Hunt, K.K.; Kuerer, H.M.; Babiera, G.; McNeese, M.D.; Buchholz, T.A.; Strom, E.A.; Robb, G.L. Delayed-Immediate Breast Reconstruction. Plast. Reconstr. Surg. 2004, 113, 1617–1628. [Google Scholar] [CrossRef]
- Malata, C.M.; McIntosh, S.A.; Purushotham, A.D. Immediate breast reconstruction after mastectomy for cancer. Br. J. Surg. 2002, 87, 1455–1472. [Google Scholar] [CrossRef]
- Kronowitz, S.J. Delayed-Immediate Breast Reconstruction: Technical and Timing Considerations. Plast. Reconstr. Surg. 2010, 125, 463–474. [Google Scholar] [CrossRef]
- Thamm, O.C.; Andree, C. Immediate Versus Delayed Breast Reconstruction. Clin. Plast. Surg. 2018, 45, 119–127. [Google Scholar] [CrossRef]
- Huis ’T Veld, E.A.; Long, C.; Sue, G.R.; Chattopadhyay, A.; Lee, G.K. Analysis of Aesthetic Outcomes and Patient Satisfaction After Delayed-Immediate Autologous Breast Reconstruction. Ann. Plast. Surg. 2018, 80, S303–S307. [Google Scholar] [CrossRef]
- Albino, F.P.; Patel, K.M.; Smith, J.R.; Nahabedian, M.Y. Delayed versus Delayed-Immediate Autologous Breast Reconstruction: A Blinded Evaluation of Aesthetic Outcomes. Arch. Plast. Surg. 2014, 41, 264–270. [Google Scholar] [CrossRef]
- Nahabedian, M.Y.; Galdino, G. Symmetrical Breast Reconstruction: Is There a Role for Three-Dimensional Digital Photography? Plast. Reconstr. Surg. 2003, 112, 1582–1590. [Google Scholar] [CrossRef] [PubMed]
- Hartmann, R.; Weiherer, M.; Schiltz, D.; Seitz, S.; Lotter, L.; Anker, A.; Palm, C.; Prantl, L.; Brébant, V. A Novel Method of Outcome Assessment in Breast Reconstruction Surgery: Comparison of Autologous and Alloplastic Techniques Using Three-Dimensional Surface Imaging. Aesthetic Plast. Surg. 2020, 44, 1980–1987. [Google Scholar] [CrossRef] [PubMed]
- Cohen, O.; Small, K.; Lee, C.; Petruolo, O.; Karp, N.; Choi, M. Is Unilateral Implant or Autologous Breast Reconstruction Better in Obtaining Breast Symmetry? Breast J. 2016, 22, 75–82. [Google Scholar] [CrossRef] [PubMed]
- Sampathkumar, U.; Bui, T.; Liu, J.; Nowroolizarki, Z.; Bordes, M.C.; Hanson, S.E.; Reece, G.P.; Markey, M.K.; Merchant, F.A. Objective Analysis of Breast Symmetry in Female Patients Undergoing Breast Reconstruction After Total Mastectomy. Aesthetic Surg. J. Open Forum 2023, 5, ojac090. [Google Scholar] [CrossRef] [PubMed]
- Henseler, H.; Smith, J.; Bowman, A.; Khambay, B.S.; Ju, X.; Ayoub, A.; Ray, A.K. Subjective versus objective assessment of breast reconstruction. J. Plast. Reconstr. Aesthet. Surg. 2013, 66, 634–639. [Google Scholar] [CrossRef]
- Rudy, H.L.; Lu, Y.-H.; Rothchild, E.; Tepper, O.M.; Weichman, K. Expanding Access to 3D Technology in Plastic Surgery of the Breast: Validation of the iPhone Against the Vectra H2. Aesthet. Surg. J. 2024, 44, sjae170. [Google Scholar] [CrossRef]
- Hartmann, R.; Weiherer, M.; Schiltz, D.; Baringer, M.; Noisser, V.; Hösl, V.; Eigenberger, A.; Seitz, S.; Palm, C.; Prantl, L.; et al. New aspects in digital breast assessment: Further refinement of a method for automated digital anthropometry. Arch. Gynecol. Obstet. 2021, 303, 721–728. [Google Scholar] [CrossRef]
- Vogt, M.; Rips, A.; Emmelmann, C. Comparison of iPad Pro®’s LiDAR and TrueDepth Capabilities with an Industrial 3D Scanning Solution. Technologies 2021, 9, 25. [Google Scholar] [CrossRef]
- Han, W.Y.; Lee, S.J.; Chang, H.P.; Heo, J.; Eom, J.S.; Kim, E.K.; Han, H.H. Development of Three-Dimensional Breast Scan and Measurement Application Using Laser Imaging Detection and Ranging (LiDAR) Sensor on iPhone. Plast. Reconstr. Surg. 2023, 152, 1183e–1187e. [Google Scholar] [CrossRef]
- Thurzo, A.; Strunga, M.; Havlínová, R.; Reháková, K.; Urban, R.; Surovková, J.; Kurilová, V. Smartphone-Based Facial Scanning as a Viable Tool for Facially Driven Orthodontics? Sensors 2022, 22, 7752. [Google Scholar] [CrossRef]
- Choudhary, A.; Vandevender, J.; Yang, K.; Kazmouz, S.; Edgar, M.; Lentskevich, M.; Juarez, C.; Mendoza, J.; Bartelt, K.; Nguyen, A.; et al. Comparison of methodologies for craniofacial soft-tissue cephalometrics: The value of virtual reality. J. Plast. Reconstr. Aesthet. Surg. 2024, 91, 35–45. [Google Scholar] [CrossRef] [PubMed]
- Rudy, H.L.; Wake, N.; Yee, J.; Garfein, E.S.; Tepper, O.M. Three-Dimensional Facial Scanning at the Fingertips of Patients and Surgeons: Accuracy and Precision Testing of iPhone X Three-Dimensional Scanner. Plast. Reconstr. Surg. 2020, 146, 1407–1417. [Google Scholar] [CrossRef] [PubMed]
- Van Lint, L.; Christiaens, L.; Stroo, V.; Bila, M.; Willaert, R.; Sun, Y.; Van Dessel, J. Accuracy Comparison of 3D Face Scans Obtained by Portable Stereophotogrammetry and Smartphone Applications. J. Med. Biol. Eng. 2023, 43, 550–560. [Google Scholar] [CrossRef]
- Andrews, J.; Alwafi, A.; Bichu, Y.M.; Pliska, B.T.; Mostafa, N.; Zou, B. Validation of three-dimensional facial imaging captured with smartphone-based photogrammetry application in comparison to stereophotogrammetry system. Heliyon 2023, 9, e15834. [Google Scholar] [CrossRef] [PubMed]
- D‘Ettorre, G.; Farronato, M.; Candida, E.; Quinzi, V.; Grippaudo, C. A comparison between stereophotogrammetry and smartphone structured light technology for three-dimensional face scanning. Angle Orthod. 2022, 92, 358–363. [Google Scholar] [CrossRef] [PubMed]
- Chong, Y.; Liu, X.; Shi, M.; Huang, J.; Yu, N.; Long, X. Three-dimensional facial scanner in the hands of patients: Validation of a novel application on iPad/iPhone for three-dimensional imaging. Ann. Transl. Med. 2021, 9, 1115. [Google Scholar] [CrossRef]
- Akan, B.; Akan, E.; Şahan, A.O.; Kalak, M. Evaluation of 3D Face-Scan images obtained by stereophotogrammetry and smartphone camera. Int. Orthod. 2021, 19, 669–678. [Google Scholar] [CrossRef]
- Quinzi, V.; Polizzi, A.; Ronsivalle, V.; Santonocito, S.; Conforte, C.; Manenti, R.J.; Isola, G.; Lo Giudice, A. Facial Scanning Accuracy with Stereophotogrammetry and Smartphone Technology in Children: A Systematic Review. Children 2022, 9, 1390. [Google Scholar] [CrossRef]
- Hartmann, R.; Nieberle, F.; Palm, C.; Brébant, V.; Prantl, L.; Kuehle, R.; Reichert, T.E.; Taxis, J.; Ettl, T. Utility of Smartphone-based Three-dimensional Surface Imaging for Digital Facial Anthropometry. JPRAS Open 2024, 39, 330–343. [Google Scholar] [CrossRef]


| Demographic Data | ||||||||
|---|---|---|---|---|---|---|---|---|
| Variables | Immediate (n = 13) | Delayed-Immediate (n = 13) | ||||||
| Min. | Max. | Mean | SD | Min. | Max. | Mean | SD | |
| Age | 32.0 | 58.0 | 48.3 | 6.6 | 38.0 | 64.0 | 53.1 | 9.4 |
| Height | 160 | 172 | 166 | 6 | 158 | 180 | 169 | 6 |
| Weight | 60.0 | 116.0 | 78 | 15.5 | 58.0 | 110.0 | 72 | 13.9 |
| BMI | 24.1 | 39.7 | 28.2 | 4.6 | 20.3 | 37.6 | 25.4 | 4.5 |
| Time since first diagnosis | 2.5 | 16.3 | 5.3 | 3.6 | 1.9 | 16.0 | 5.7 | 4.1 |
| Flap weight | 453 | 1550 | 729 | 379 | 250 | 857 | 516 | 159 |
| T-Test for Independent Samples and Mean Values | |||||||||
|---|---|---|---|---|---|---|---|---|---|
| Variables | |||||||||
| Mean | Levene’s Test | 95% CI | T-test | Cohen’s d | |||||
| Immediate | Delayed-Immediate | p | Mean Diff. | Std. Error Diff. | Lower | Upper | p | Point Estimates | |
| Age | 48.3 | 53.1 | 0.09 | −4.8 | 3.2 | −11.3 | 1.8 | 0.15 | 0.81 |
| Height | 166 | 169 | 0.52 | −3.0 | 2.3 | −7.5 | 1.75 | 0.21 | −0.5 |
| Weight | 78 | 72 | 0.58 | 5.6 | 5.8 | −6.4 | 17.5 | 0.35 | 0.38 |
| BMI | 28.2 | 25.4 | 0.81 | 2.9 | 1.8 | −0.8 | 6.6 | 0.12 | 0.63 |
| Time since first diagnosis | 5.3 | 5.7 | 0.49 | −0.4 | 1.5 | −3.6 | 2.8 | 0.80 | −0.51 |
| Flap weight | 729 | 516 | 0.16 | 212.7 | 127.6 | −57.9 | 483.3 | 0.12 | −0.10 |
| Descriptive Statistics | ||||||||
|---|---|---|---|---|---|---|---|---|
| Variables | Immediate (n = 13) | Delayed-Immediate (n = 13) | ||||||
| Min. | Max. | Mean | SD | Min. | Max. | Mean | SD | |
| (1) SN—N (R) | 19.7 | 36.9 | 24.8 | 4.3 | 17.4 | 27.3 | 23.0 | 3.0 |
| (2) LBP—N (R) | 6.8 | 12.8 | 9.0 | 1.8 | 5.6 | 9.8 | 7.9 | 1.3 |
| (3) UBP—N (R) | 12.8 | 29.3 | 17.9 | 4.2 | 10.0 | 20.4 | 16.3 | 3.2 |
| (4) Xi—N (R) | 9.9 | 17.4 | 12.8 | 2.1 | 9.0 | 14.6 | 12.3 | 1.5 |
| (5) LaBP—N (R) | 8.9 | 19.4 | 14.3 | 2.5 | 8.8 | 14.3 | 10.9 | 1.7 |
| (6) SN—N (L) | 18.7 | 29.4 | 24.6 | 3.1 | 18.4 | 29.6 | 24.3 | 3.8 |
| (7) LBP—N (L) | 5.8 | 11.9 | 8.4 | 1.7 | 6.1 | 10.2 | 8.0 | 1.3 |
| (8) UBP—N (L) | 11.4 | 22.3 | 17.4 | 3.3 | 11.1 | 23.6 | 17.8 | 3.9 |
| (9) Xi—N (L) | 10.3 | 14.9 | 13.4 | 1.2 | 9.3 | 16.3 | 13.2 | 2.0 |
| (10) LaBP—N (L) | 8.7 | 16.2 | 13.1 | 2.5 | 9.3 | 14.9 | 11.8 | 1.9 |
| (11) Breast width (R) | 20.2 | 36.9 | 27.1 | 3.8 | 17.9 | 27.4 | 23.2 | 2.7 |
| (12) IMF-Length (R) | 20.7 | 37.5 | 25.7 | 4.3 | 18.7 | 25.6 | 22.7 | 2.3 |
| (13) Breast width (L) | 19.0 | 29.8 | 26.4 | 3.1 | 20.3 | 30.5 | 25.1 | 3.4 |
| (14) IMF-Length (L) | 16.8 | 30.9 | 24.9 | 3.6 | 20.0 | 29.4 | 24.2 | 3.2 |
| (15) SI | 0.74 | 0.97 | 0.85 | 0.06 | 0.78 | 0.97 | 0.88 | 0.06 |
| T-Test for Independent Samples and Mean Values | |||||||||
|---|---|---|---|---|---|---|---|---|---|
| Variables | |||||||||
| Mean | Levene’s Test | 95% CI | T-Test | Cohen’s d | |||||
| Immediate | Delayed-Immediate | p | Mean Diff. | Std. Error Diff. | Lower | Upper | p | Point Estimates | |
| (1) SN—N (R) | 24.8 | 23.0 | 0.71 | 1.7 | 1.5 | −1.3 | 4.7 | 0.24 | 0.5 |
| (2) LBP—N (R) | 9.0 | 7.9 | 0.52 | 1.2 | 0.6 | −0.1 | 2.5 | 0.07 | 0.5 |
| (3) UBP—N (R) | 17.9 | 16.3 | 0.71 | 1.6 | 1.4 | −1.4 | 4.6 | 0.27 | 0.6 |
| (4) Xi—N (R) | 12.8 | 12.3 | 0.13 | 0.5 | 0.7 | −1 | 2.1 | 0.46 | 0.7 |
| (5) LaBP—N (R) | 14.3 | 10.9 | 0.46 | 3.4 | 0.8 | 1.6 | 5.1 | <0.001 | 0.7 |
| (6) SN—N (L) | 24.6 | 24.3 | 0.30 | 0.3 | 1.3 | −2.5 | 3.1 | 0.83 | 0.9 |
| (7) LBP—N (L) | 8.4 | 8.0 | 0.32 | 0.4 | 0.6 | −0.8 | 1.7 | 0.47 | 0.4 |
| (8) UBP—N (L) | 17.4 | 17.8 | 0.36 | −0.4 | 1.4 | −3.3 | 2.5 | 0.77 | 0.4 |
| (9) Xi—N (L) | 13.4 | 13.2 | 0.06 | 0.1 | 0.6 | −1.2 | 1.5 | 0.82 | 0.5 |
| (10) LaBP—N (L) | 13.1 | 11.8 | 0.43 | 1.2 | 0.9 | −0.5 | 3 | 0.17 | 0.3 |
| (11) Breast width (R) | 27.1 | 23.2 | 0.67 | 3.9 | 1.3 | 1.2 | 6.6 | 0.01 | 0.3 |
| (12) IMF-Length (R) | 25.7 | 22.7 | 0.23 | 3.1 | 1.4 | 0.2 | 5.9 | 0.03 | 0.4 |
| (13) Breast width (L) | 26.4 | 25.1 | 0.44 | 1.3 | 1.3 | −1.3 | 3.9 | 0.31 | 1.6 |
| (14) IMF-Length (L) | 24.9 | 24.2 | 0.62 | 0.7 | 1.3 | −2.1 | 3.4 | 0.61 | 1.5 |
| (15) SI | 0.85 | 0.88 | 0.36 | −0.03 | 0.02 | −0.08 | 0.02 | 0.23 | 2.0 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Hartmann, R.; Chrobot, N.; Festbaum, C.; Alfertshofer, M.; Obermeier, K.T.; Smolka, W.; Ettl, T.; Prantl, L.; Brébant, V. Symmetry After Breast Reconstruction Surgery: A Comparison of Immediate vs. Delayed-Immediate Breast Reconstruction Using Smartphone-Based 3D Surface Imaging. J. Clin. Med. 2025, 14, 7622. https://doi.org/10.3390/jcm14217622
Hartmann R, Chrobot N, Festbaum C, Alfertshofer M, Obermeier KT, Smolka W, Ettl T, Prantl L, Brébant V. Symmetry After Breast Reconstruction Surgery: A Comparison of Immediate vs. Delayed-Immediate Breast Reconstruction Using Smartphone-Based 3D Surface Imaging. Journal of Clinical Medicine. 2025; 14(21):7622. https://doi.org/10.3390/jcm14217622
Chicago/Turabian StyleHartmann, Robin, Nikolas Chrobot, Christian Festbaum, Michael Alfertshofer, Katharina Theresa Obermeier, Wenko Smolka, Tobias Ettl, Lukas Prantl, and Vanessa Brébant. 2025. "Symmetry After Breast Reconstruction Surgery: A Comparison of Immediate vs. Delayed-Immediate Breast Reconstruction Using Smartphone-Based 3D Surface Imaging" Journal of Clinical Medicine 14, no. 21: 7622. https://doi.org/10.3390/jcm14217622
APA StyleHartmann, R., Chrobot, N., Festbaum, C., Alfertshofer, M., Obermeier, K. T., Smolka, W., Ettl, T., Prantl, L., & Brébant, V. (2025). Symmetry After Breast Reconstruction Surgery: A Comparison of Immediate vs. Delayed-Immediate Breast Reconstruction Using Smartphone-Based 3D Surface Imaging. Journal of Clinical Medicine, 14(21), 7622. https://doi.org/10.3390/jcm14217622








