1. Background
Gynecomastia (GM) is a common benign breast condition in males characterized primarily by abnormal proliferation of glandular breast tissue, clinically manifesting as unilateral or bilateral breast enlargement often accompanied by varying degrees of adipose tissue accumulation [
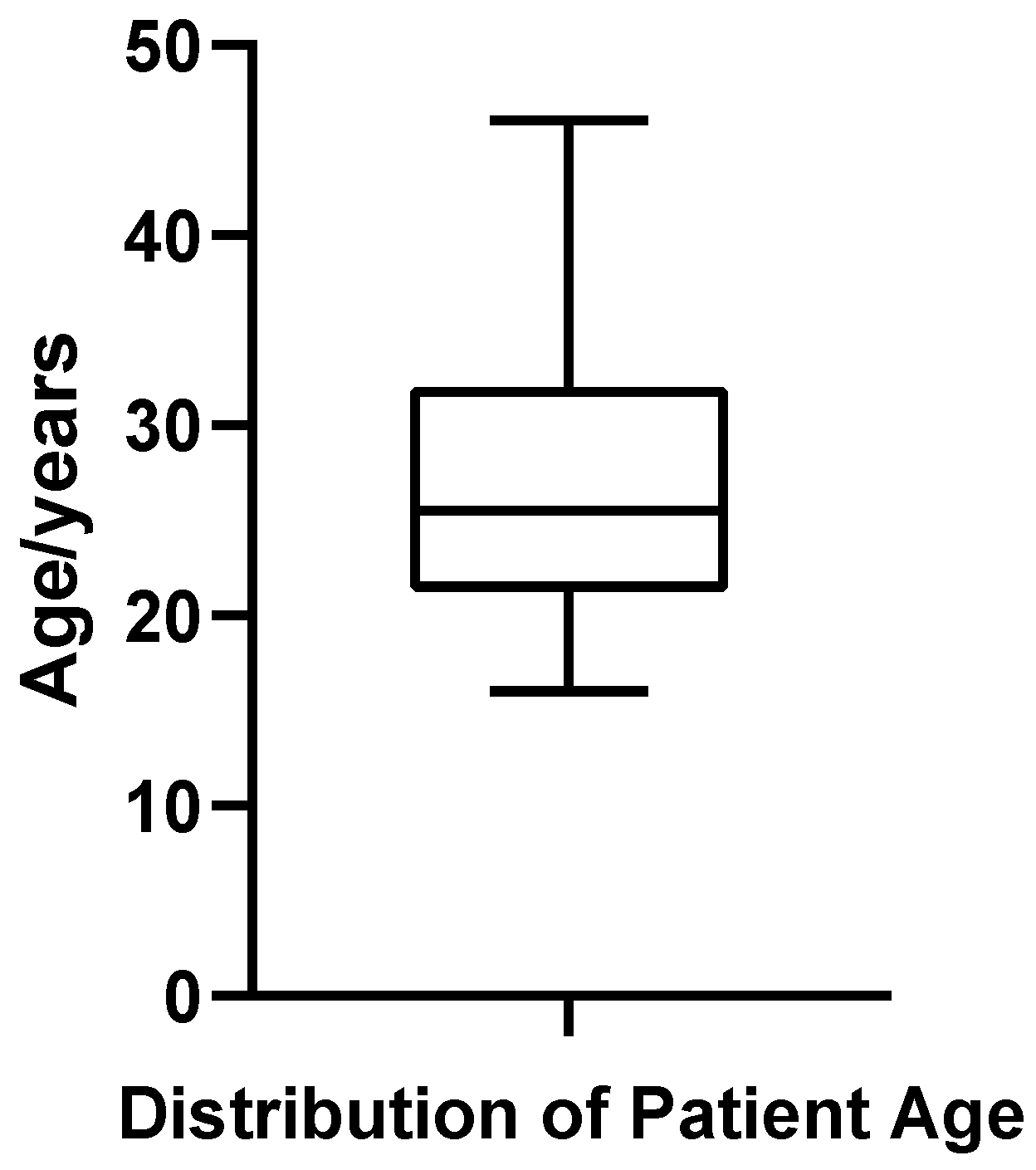
1]. GM occurs frequently among males across various age groups, with prevalence rates exceeding 50% in adolescents and approximately 40% among elderly men [
2]. Although GM generally does not cause significant physiological impairment, the conspicuous breast appearance often results in substantial psychological distress, especially among adolescent and young adult males, who commonly experience anxiety, low self-esteem, and even depression, negatively impacting their quality of life and social adaptability [
3]. Therefore, the diagnosis and management of GM have increasingly drawn attention from plastic surgeons, highlighting the critical importance of accurately evaluating the tissue composition and volumetric characteristics of the breast in GM patients during treatment planning.
Currently, clinical diagnosis of GM primarily relies on patient history, physical examination, and imaging studies, with imaging examinations playing a pivotal role. Breast ultrasonography, commonly utilized as the initial screening modality for GM, offers advantages such as being radiation-free, cost-effective, and convenient [
4]. However, the accuracy of ultrasound examinations heavily depends on operator expertise, and conventional two-dimensional ultrasound images cannot precisely delineate the spatial anatomy and volumetric characteristics of glandular and adipose tissues. Mammography, frequently employed in screening for breast diseases in females, can identify dense glandular tissues; however, due to the generally thin and small size of male breast tissue and overlapping densities between glandular and adipose components, clear delineation is challenging [
5]. Furthermore, the radiation exposure associated with mammography limits its routine application in male breast disorders.
In recent years, Magnetic Resonance Imaging (MRI), with its superior soft-tissue contrast, non-invasiveness, and lack of radiation exposure, has increasingly become an essential imaging modality for diagnosing, differentiating, and preoperative evaluation of GM patients. MRI provides significant advantages, including non-invasiveness, radiation-free imaging, high soft-tissue contrast resolution, and robust three-dimensional visualization, enabling clearer and more accurate spatial anatomical delineation between glandular and adipose tissues [
6]. Advanced MRI techniques, such as T1-weighted imaging, fat suppression methods, dynamic contrast-enhanced MRI, and diffusion-weighted imaging, effectively differentiate glandular from adipose tissues and hold substantial value in excluding malignant breast lesions [
7,
8].
Despite the substantial advantages of MRI in the diagnosis and differential diagnosis of gynecomastia (GM), current MRI studies have predominantly relied on qualitative, two-dimensional imaging assessments and lesion identification, lacking comprehensive three-dimensional (3D) structural and volumetric analysis of glandular and adipose tissues in the male breast [
5]. Consequently, clinical treatment decisions often depend heavily on subjective physician judgment without clear, quantitative imaging support. In recent years, MRI-based 3D segmentation and reconstruction technologies have gained widespread application in clinical investigations of neurological diseases and head-and-neck tumors [
9,
10]. Integrating advanced algorithms such as the active contour (Snake) model, these techniques have demonstrated precise tissue boundary delineation and accurate 3D anatomical reconstruction capabilities [
11]. By leveraging MRI-based 3D segmentation and reconstruction methods, it is possible to precisely quantify the spatial distribution and volumes of glandular and adipose tissues in GM patients, providing objective and quantitative metrics to guide diagnosis, inform treatment strategies, and facilitate outcome assessment.
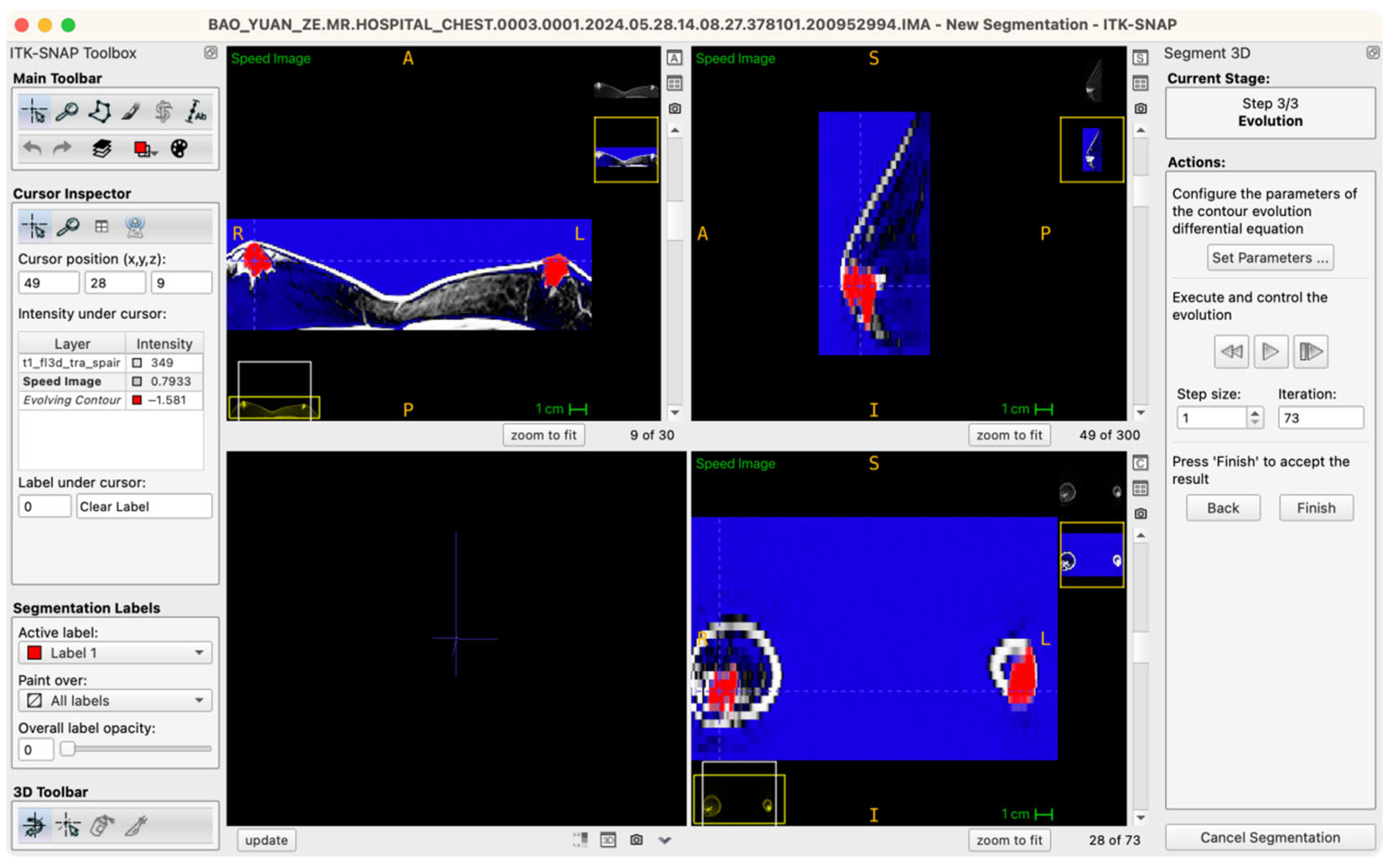
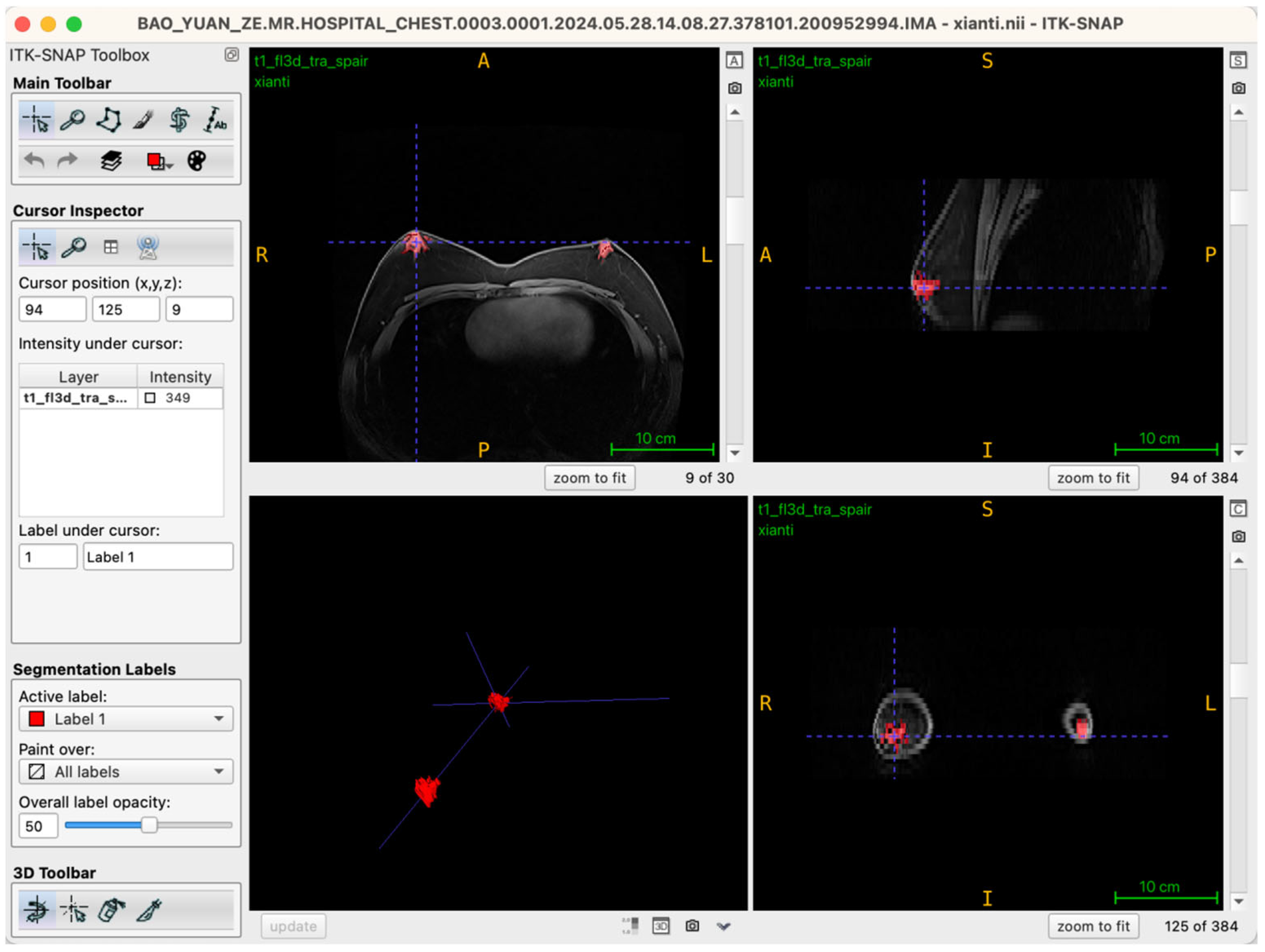
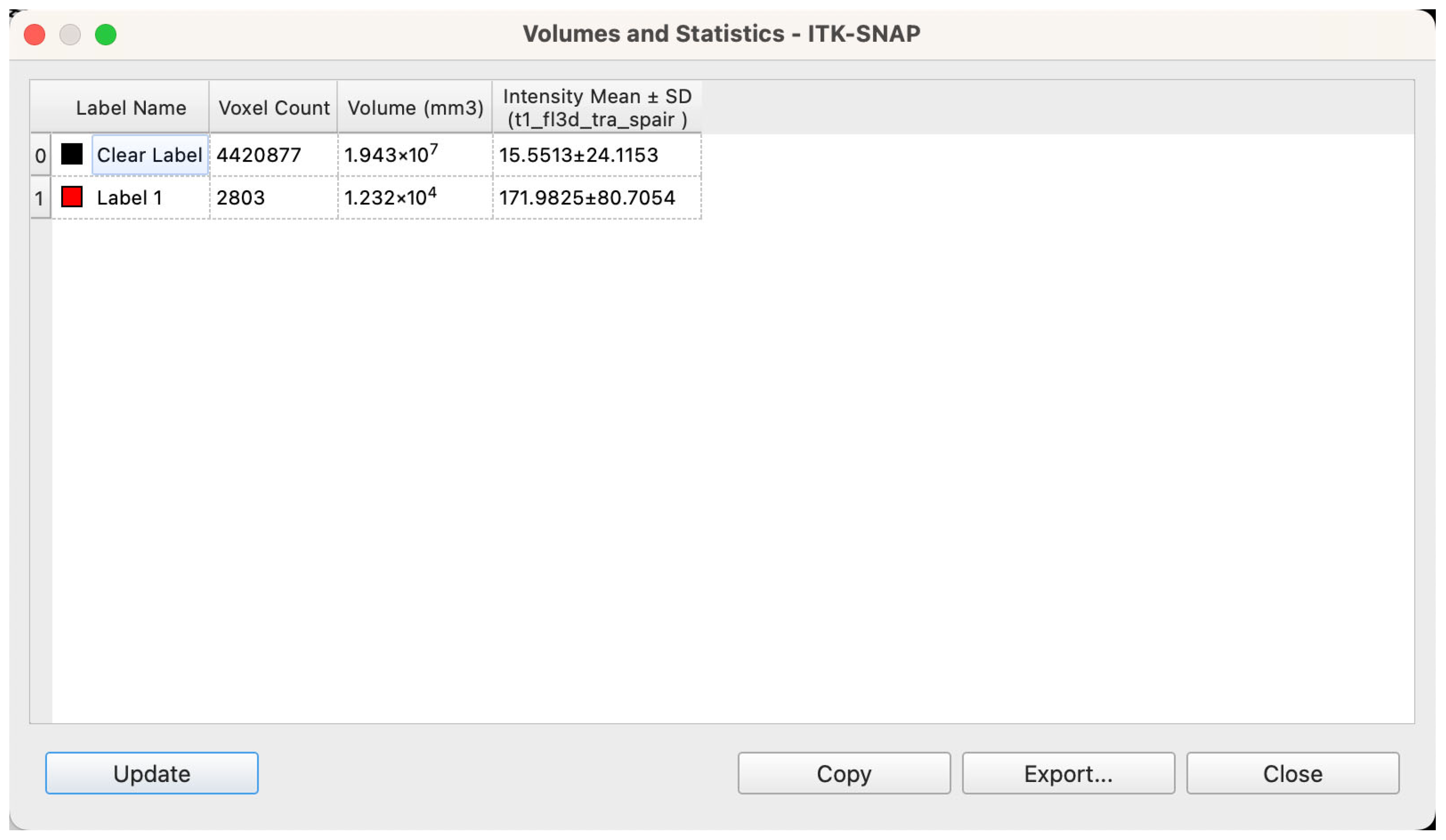
Therefore, the current study employs MRI-based 3D segmentation and reconstruction technology as its core methodological approach to quantitatively analyze the spatial characteristics of glandular and adipose tissues in 52 patients diagnosed with bilateral GM. Specifically, the study first involves the collection of MRI imaging data from clinically diagnosed bilateral GM patients, clearly defining MRI scanning equipment, sequences, and parameters to establish a standardized imaging database. Subsequently, using the ITK-SNAP (version 4.0) software [
12], semi-automatic 3D segmentation and reconstruction of breast MRI images are performed to accurately measure glandular and adipose tissue volumes, thereby characterizing the volumetric distribution of these tissues across the patient cohort.
In summary, this study aims to verify the applicability and advantages of MRI-based 3D segmentation and reconstruction technology in volumetric analysis of glandular and adipose tissues among GM patients. The goal is to establish an objective, precise, and quantitative imaging foundation to inform clinical diagnosis and treatment decisions, thereby promoting a transition from subjective clinical judgment toward quantitative and precise evaluation in GM management.
4. Discussion
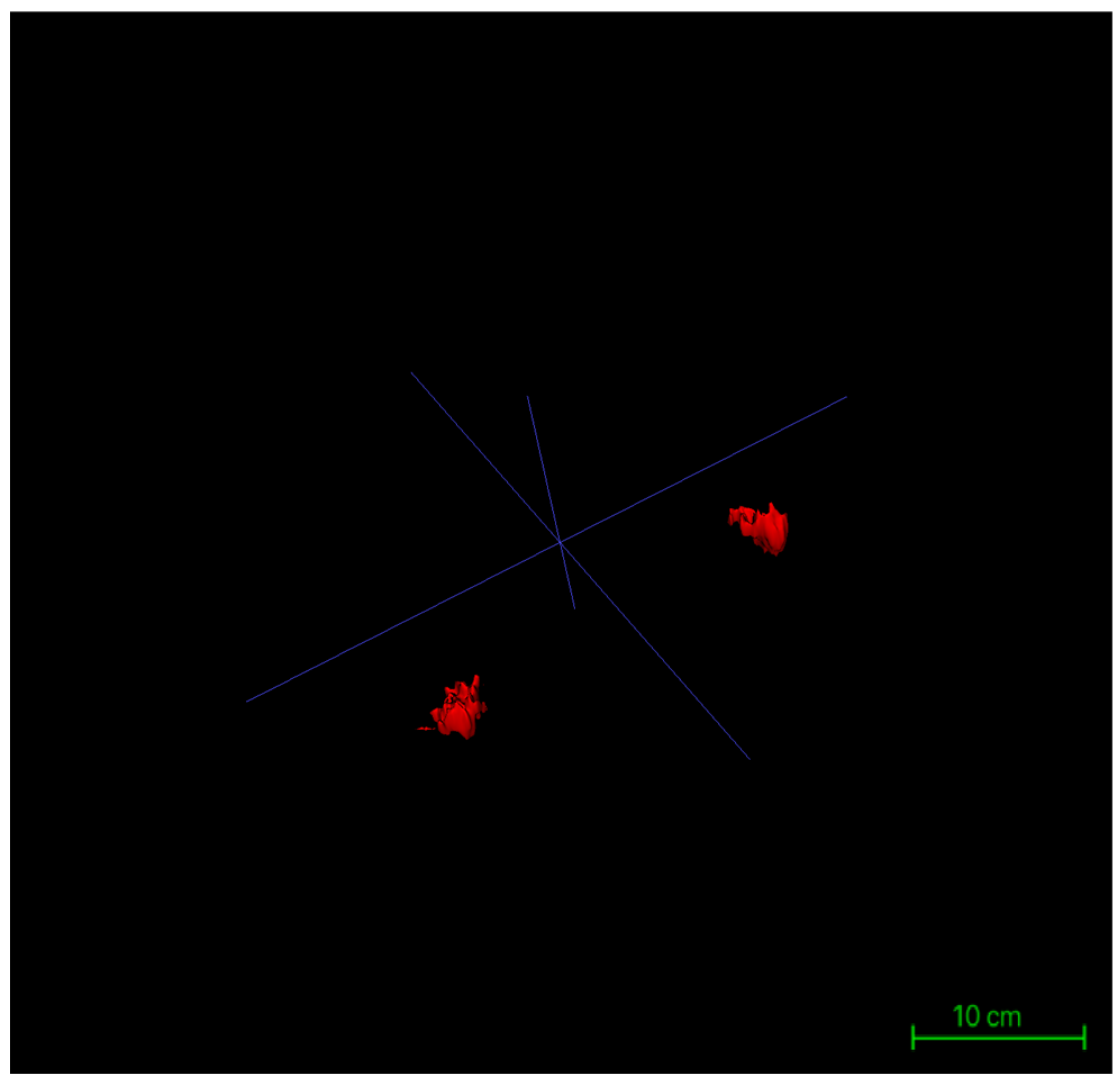
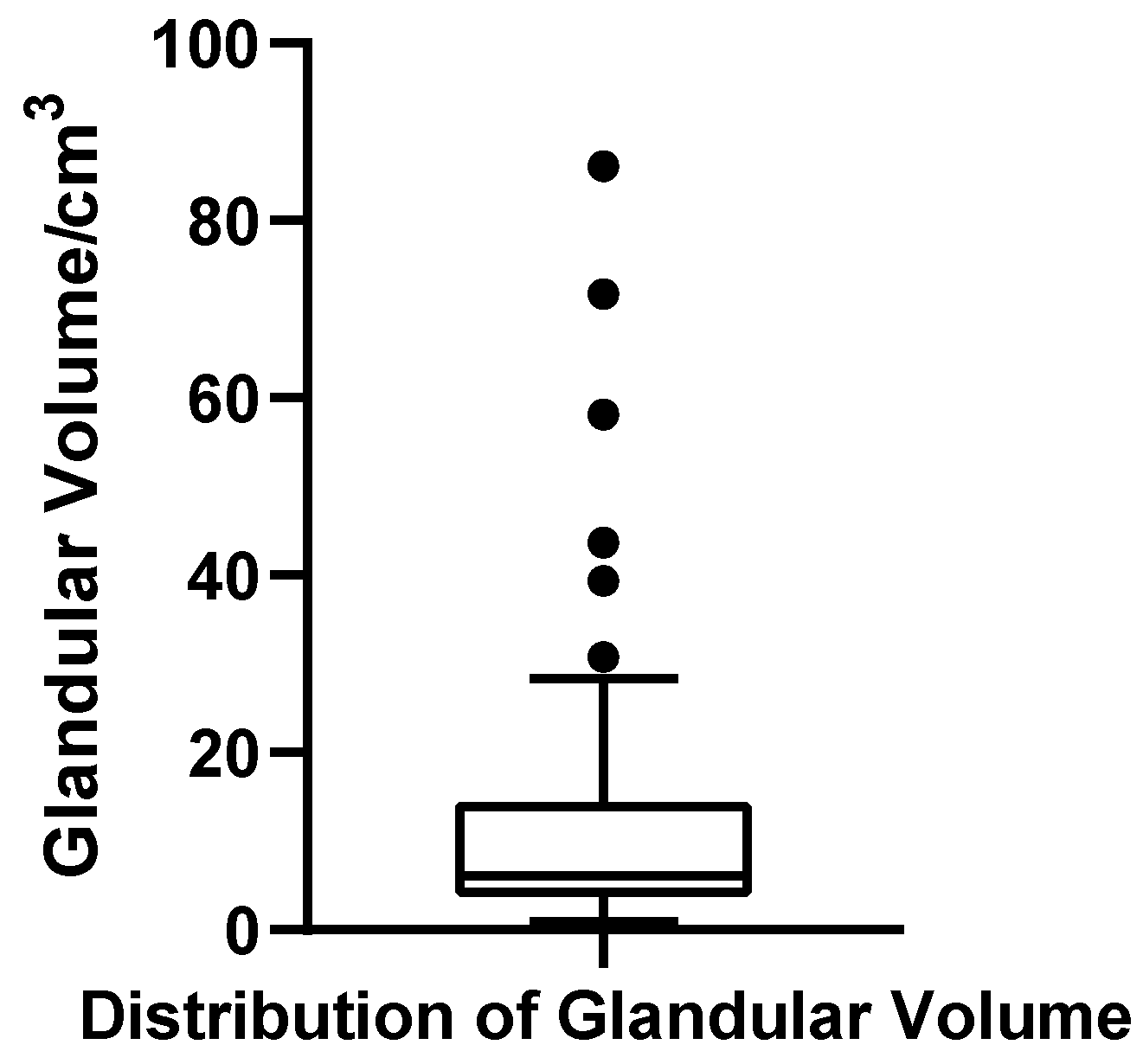
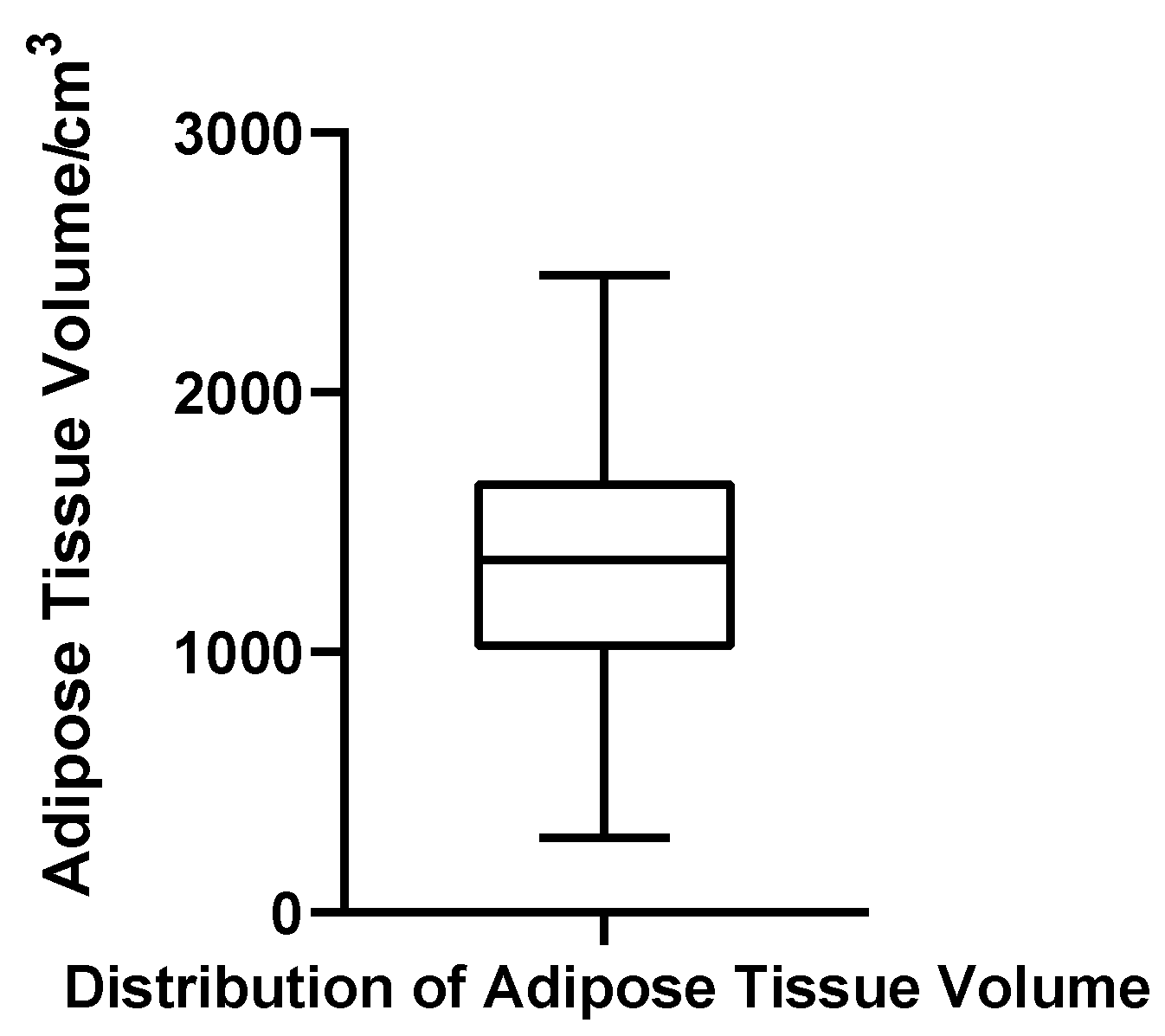
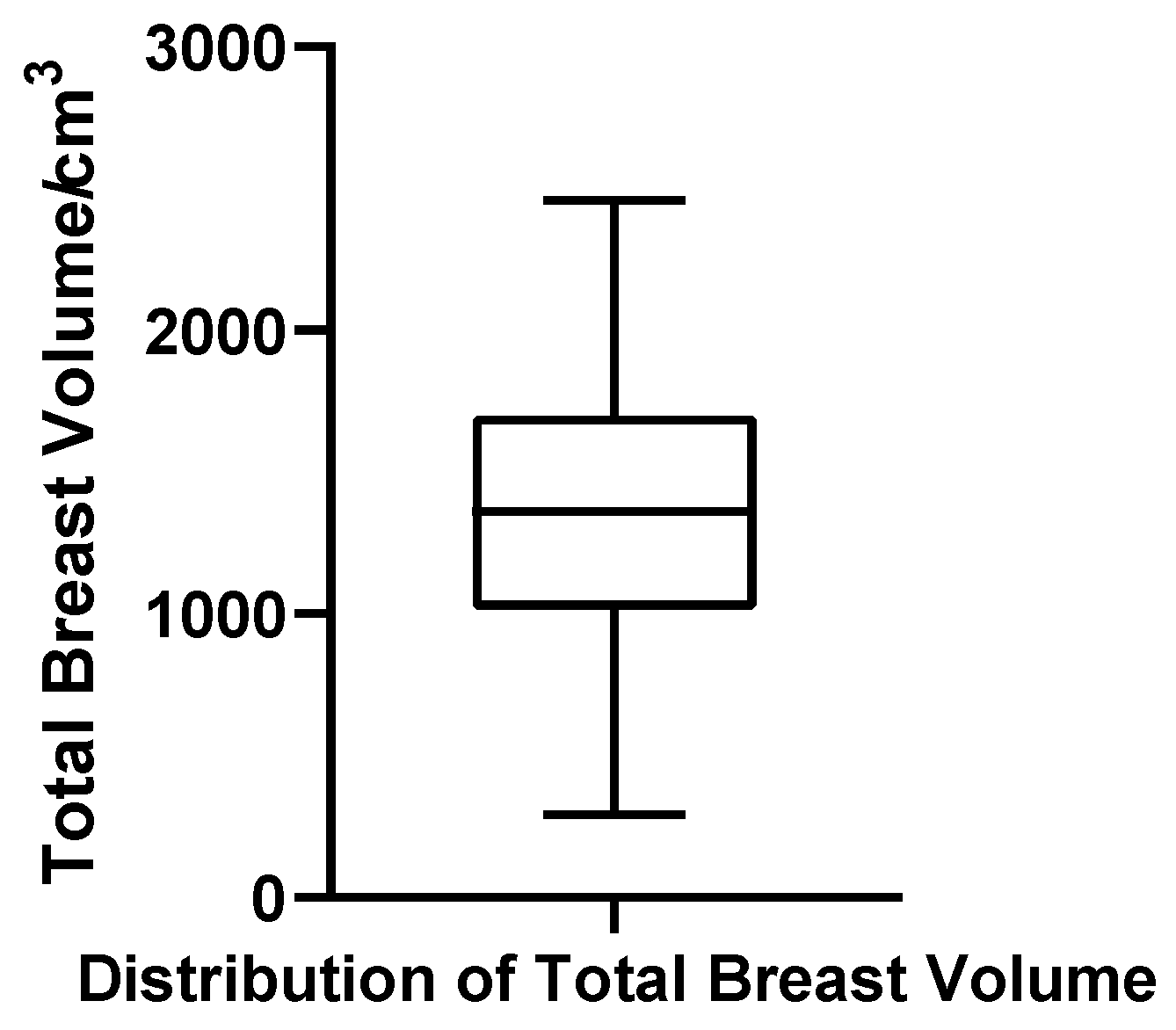
In this study, we conducted a comprehensive volumetric assessment of the male breast in 52 patients with bilateral gynecomastia who were scheduled to undergo surgical correction. Using MRI-based three-dimensional segmentation and reconstruction, we generated anatomically continuous models of both glandular and adipose tissues, allowing for precise quantification of their volumetric features.
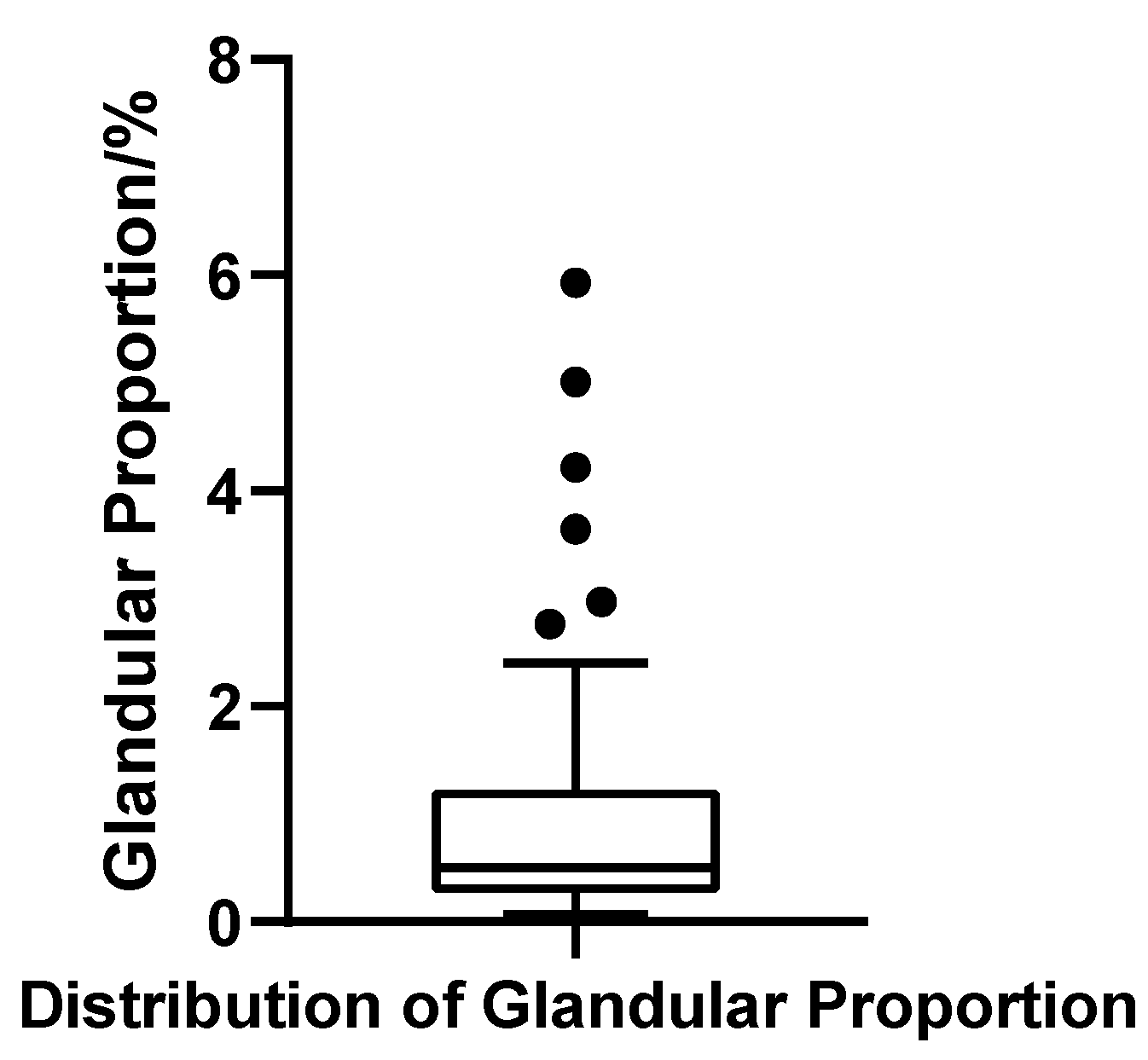
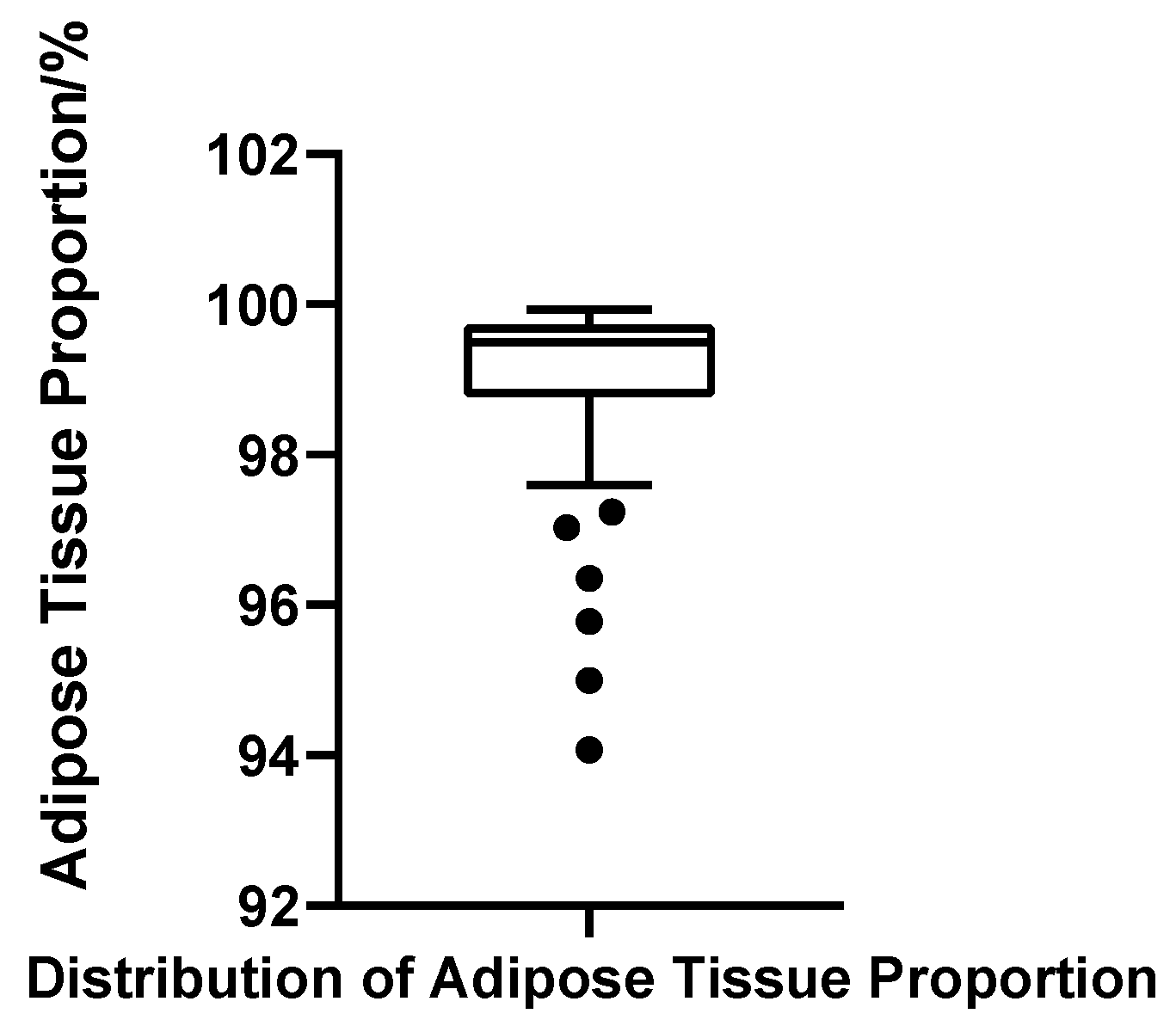
One of the most striking findings was the overwhelmingly low proportion of glandular tissue within the total breast volume in this surgical cohort. The average glandular ratio was only 1.04%, with a median of 0.50%, underscoring a predominant pattern of fatty proliferation. Notably, over 90% of the patients demonstrated glandular contributions of less than 3%, indicating that the majority of cases requiring surgery were characterized by fat-dominant hypertrophy rather than extensive glandular overgrowth. This finding challenges the conventional reliance on subjective intraoperative impressions or two-dimensional imaging assessments and underscores the value of objective structural quantification in preoperative planning [
14].
Beyond the anatomical insights, this study introduces a methodological advancement in the imaging evaluation of gynecomastia. The application of a high-resolution T1_FL3D_TRA_SPAIR sequence, combined with semi-automated, multi-label segmentation using ITK-SNAP software, enabled us to independently delineate glandular and adipose tissues and extract their respective volumes with high fidelity. The resulting workflow is not only precise and efficient but also traceable and reproducible—features critical for both clinical application and future research. This framework provides a scalable template for quantitative structural assessment in other morphologically complex soft-tissue regions.
Importantly, our findings are grounded in a highly selected clinical population—namely, patients seen at the Department of Aesthetic and Reconstructive Breast Surgery of the Plastic Surgery Hospital, Chinese Academy of Medical Sciences, who had opted for surgical intervention. This group does not represent the full spectrum of gynecomastia but rather a subset with substantial structural abnormalities, significant subjective distress, and clear surgical indications. In the context of clinical decision-making, such patients are highly representative of those who truly benefit from preoperative anatomical modeling. Although no formal sample size calculation was performed, the inclusion of 52 bilateral surgical cases provided more than adequate power for the descriptive and reproducibility-focused objectives of this study. Because the aim was not hypothesis testing but rather detailed structural quantification and methodological validation, this cohort size was sufficient to reveal distributional patterns, capture inter-individual heterogeneity, and support robust segmentation repeatability.
Compared with those with mild or incidental gynecomastia, the surgical cohort typically presents with pronounced morphological alterations, including visibly enlarged breast volume, aberrant tissue distribution, and aesthetically concerning deformities. For these patients, preoperative structural quantification offers critical value in tailoring surgical techniques and managing expectations. Furthermore, most had undergone endocrine evaluation prior to surgery, making their imaging features more reflective of the disease’s morphological endpoint. As such, the observed glandular and adipose composition likely mirrors intraoperative realities and the primary determinants of postoperative contour, reinforcing the clinical utility of this imaging-based approach.
In clinical practice, the histopathological composition of gynecomastia (GM) is notably heterogeneous. Although an increase in breast volume is a shared manifestation across cases, the internal tissue architecture—specifically the balance between glandular and adipose components—varies substantially among individuals [
15]. By leveraging three-dimensional segmentation and modeling, the present study offers a precise quantification of this gland-fat ratio in a surgical GM cohort, thereby uncovering a predominant pattern of “fat-dominant structure” in bilateral cases. This finding not only provides objective confirmation of prior observations largely based on subjective or two-dimensional imaging interpretations but also establishes a foundational framework for structural subtyping in GM.
From a surgical standpoint, the relative proportion of glandular versus adipose tissue plays a pivotal role in determining the optimal approach [
16]. In patients with minimal glandular hypertrophy, liposuction alone may suffice to restore normal contour. Conversely, in cases characterized by marked glandular proliferation, more targeted excision strategies—including complete gland removal—are warranted to address localized prominence, nipple protrusion, or asymmetry [
17]. Therefore, accurate preoperative characterization of male breast tissue composition is instrumental not only for procedural planning and outcome prediction but also for facilitating informed discussions with patients. In our institution, this consideration underpins the routine adoption of preoperative MRI for surgical candidates with clinically significant gynecomastia, as high-resolution volumetric assessment provides objective insight into tissue composition, strengthens surgical planning, and ultimately supports more predictable outcomes. Especially within the context of modern plastic surgery’s movement toward minimally invasive and individualized interventions, such imaging-based quantification may soon become standard practice.
In designing the segmentation and volumetric analysis protocol for this study, careful consideration was given to the structural complexity, boundary ambiguity, and consistency demands inherent to male breast tissue. A high-precision modeling workflow was established, centered around the ITK-SNAP platform, which enabled the semi-automated, dual-label, and anatomically distinct segmentation of both glandular and intramammary adipose tissue. This approach represents a methodological advancement in male breast imaging: seed point initialization was coupled with active contour evolution via the Snake algorithm, allowing boundary refinement to proceed adaptively. This strategy significantly minimized operator-dependent variability while ensuring high inter-subject consistency in segmentation contours, thereby meeting the rigorous image quality demands of structural volumetric studies [
18]. Real-time 3D rendering and synchronized multi-planar correction during the segmentation process further empowered operators to interactively refine boundaries in anatomically challenging regions, enhancing the accuracy and fidelity of the final models.
The successful implementation of this segmentation strategy was fundamentally enabled by the T1_FL3D_TRA_SPAIR sequence, which served as a technical backbone by providing high-resolution, high-contrast MR images. This sequence combines two advanced imaging principles: Fast Low Angle Shot 3D (FL3D), a rapid gradient echo technique, and Spectral Adiabatic Inversion Recovery (SPAIR), a fat suppression strategy optimized for spectral selectivity. FL3D employs low flip angles, short echo times, and abbreviated repetition intervals to acquire three-dimensional datasets with high in-plane resolution within clinically acceptable scan durations; in our protocol, voxels were anisotropic (0.94 × 0.94 × 5.0 mm) rather than isotropic [
19]. Accordingly, high in-plane resolution—rather than isotropy—enabled reliable multiplanar review and accurate surface reconstruction, which proved critical for maintaining anatomical continuity and delineating gland–fat interfaces [
20]. Moreover, FL3D is particularly advantageous in breast MRI due to its intrinsic resilience to motion artifacts caused by respiration, cardiac pulsation, or chest wall movement, thereby ensuring image stability and enhancing soft tissue clarity [
21]. In this study, the use of FL3D ensured clear demarcation and homogeneous signal representation of both glandular and adipose tissues at the source image level, facilitating reliable seed placement and Snake evolution. Complementing this, SPAIR provided uniform and robust fat suppression without compromising water signal integrity [
22]. Compared with conventional short inversion time recovery (STIR) or chemical shift selective methods, SPAIR offers superior tolerance to magnetic field inhomogeneities, making it particularly suited for high-susceptibility regions such as the chest and breasts [
23]. Within the acquired image sets, glandular tissue—rich in water content—appeared as high signal intensity, whereas fat was effectively suppressed and rendered hypointense. This stark contrast significantly improved the label classification accuracy in ITK-SNAP and reduced the likelihood of boundary ambiguity or segmentation artifacts. The synergistic combination of FL3D and SPAIR optimized both spatial resolution and tissue contrast, enabling high-fidelity 3D reconstructions of glandular and adipose compartments. When integrated with ITK-SNAP’s semi-automated contour evolution and multi-label modeling capabilities, this protocol facilitated not only the independent identification and volumetric extraction of target structures but also their anatomically faithful visualization. As a result, the entire segmentation pipeline demonstrated excellent standardization, reproducibility, and inter-subject spatial coherence, laying a robust imaging foundation for subsequent quantitative analysis and statistical modeling.
This study provides a dual contribution: on one hand, the establishment of a reproducible MRI-based 3D segmentation and reconstruction workflow tailored for gynecomastia; on the other hand, the volumetric characterization of glandular and adipose tissues derived from this workflow. These two aspects are inseparable, as the credibility of volumetric findings relies on methodological rigor, while the volumetric distributions in turn demonstrate the workflow’s clinical applicability. To ensure robustness, consistency, and anatomical validity of the image segmentation results, this study adopted a stringent quality control framework throughout the 3D modeling process. All segmentation procedures were performed by a single, well-trained operator using a standardized workflow to minimize inter-operator variability. Key procedural elements—including seed placement, label assignment, and activation of the Snake algorithm—were executed under consistent logic. Software platform, version, and image resolution parameters were uniformly applied across all cases to mitigate systemic bias introduced by technical heterogeneity.
For seed initialization, the radius was empirically standardized between 3.0 and 6.0 voxels, a range optimized to match the in-plane spatial resolution (0.9375 mm) and slice thickness (5.0 mm) of the T1-weighted MRI images, as well as the expected anatomical dimensions of the glandular tissue. In pilot experiments, radii below 3.0 voxels frequently resulted in inadequate region growth, necessitating redundant placements, whereas values exceeding 6.0 voxels often led to overgrowth into adjacent adipose compartments. This calibrated range proved efficient and anatomically compatible during segmentation, aligning with parameter values commonly reported in 3D volumetric modeling literature [
18].
To further enhance structural fidelity, each segmentation label underwent layer-by-layer inspection using ITK-SNAP’s synchronized tri-planar review function. Particular attention was paid to boundary continuity and signal transitions, especially in anatomically ambiguous zones. This post-segmentation validation ensured spatial closure and topological integrity of both glandular and adipose compartments, thereby reinforcing the accuracy of subsequent volumetric extraction and statistical measurements.
To address potential concerns regarding operator dependency and methodological reproducibility—common critiques in semi-automated segmentation workflows—the study prioritized process standardization from the outset. A detailed standard operating procedure (SOP) was developed and enforced, covering all critical steps of the segmentation pipeline. In selected cases, repeat segmentations and cross-operator validations were performed to evaluate procedural reproducibility. These methodological safeguards collectively established a traceable and replicable modeling framework that supports internal stability and external transferability.
A key methodological decision was to perform volumetry at the patient level using bilateral totals rather than per-side outputs. This choice was pre-specified to maximize measurement validity under our acquisition and segmentation conditions. First, side-specific partitioning would require an operator-defined midline in the supine orientation, where anterior chest wall flattening and a blunted intermammary sulcus provide no consistent anatomical substrate across slices; with anisotropic voxels (0.94 × 0.94 × 5.0 mm), such partitioning magnifies through-plane partial-volume and staircase artifacts. Second, our validated SOP is optimized for bilateral envelope closure with seed-based active contours and tri-planar verification; imposing post hoc left–right cuts would introduce additional manual heuristics outside the validated workflow, shifting label boundaries and degrading repeatability. Third, clinically meaningful per-side ground truth was not available: combined gland excision with liposuction does not yield side-pure, volumetrically reliable specimens (aspirate volumes are confounded by tumescent fluid and intraoperative sculpting). For these reasons, all statistical inferences were made at the patient level (bilateral totals, N = 52), which preserves independence, aligns with the bilateral nature of surgical planning, and—critically—avoids operator-dependent partition error that per-side outputs would introduce under the present protocol.
Despite the methodological rigor employed in segmentation and volume analysis, several intrinsic limitations and external constraints of this study warrant explicit acknowledgment. First, the MRI data were acquired using a fixed protocol on a 1.5 T SIEMENS Aera scanner, employing the default T1_FL3D_TRA_SPAIR sequence with a slice thickness of 5 mm. While this parameter setting ensures efficient scan time and spatial continuity, the relatively coarse through-plane resolution may limit the accurate delineation of small or poorly defined glandular structures. Such limitations introduce the potential for underestimation of glandular volume, particularly in cases with indistinct anatomical boundaries [
24]. Nonetheless, the high in-plane resolution of 0.94 × 0.94 mm preserved boundary sharpness and enabled reliable multiplanar verification and surface reconstruction, thereby partially mitigating the volumetric distortion typically associated with anisotropic voxels. To further address this risk, the study incorporated multiple quality assurance strategies during segmentation, including synchronized multiplanar inspection, targeted seed-point refinement in critical slices, and comprehensive 3D verification of spatial closure. These measures served to minimize segmentation artifacts arising from limited z-axis resolution and to safeguard the anatomical integrity and volumetric completeness of the extracted data. Second, all imaging was performed in the supine position with an anterior body array coil, a setup intentionally adopted because it mirrors intraoperative positioning and therefore aligns closely with the aim of preoperative planning. Although this differs from the conventional prone position with a dedicated breast coil used in diagnostic breast MRI, the supine configuration was advantageous for surgical relevance and provided consistent volumetric data across patients. While direct correction factors or intraoperative validation were not applied in this study, the standardized acquisition protocol and reproducible segmentation workflow mitigate concerns about positional variability, and future investigations may further examine potential differences between supine and prone acquisitions. Third, the study population consisted exclusively of bilateral gynecomastia (GM) patients scheduled for surgical intervention, a cohort characterized by prominent clinical symptoms, substantial structural hypertrophy, and documented preoperative imaging. As such, the derived tissue composition patterns and statistical associations are most applicable to diagnostic imaging and preoperative planning scenarios in symptomatic surgical candidates. Extrapolation of these findings to broader GM populations—including pubertal self-resolving cases, asymptomatic individuals, or patients with unilateral involvement—should be approached with caution, as structural profiles may differ substantially and limit statistical comparability. In addition, intraoperative excised tissue weights or pathology-based volumetric validation were not available in this cohort, since glandular excision was frequently combined with liposuction, and aspirated fat volumes are confounded by irrigation fluid and sculpting. As a result, reliable side-specific or specimen-based volumetric correspondence could not be established. This limitation does not undermine the objectives of the present work, which were confined to preoperative structural modeling and descriptive quantification. Nonetheless, future studies incorporating dedicated validation subsets—such as cases with isolated glandular excision or prospectively recorded specimen weights—will be essential to further strengthen the translational accuracy of MRI-based volumetry.
From a technical standpoint, the segmentation pipeline developed here features well-defined parameters, scalable outputs, and a modular architecture that supports cross-institutional replication and integration into machine learning workflows. These attributes position the current framework as a foundational tool for establishing a standardized imaging database of male breast morphology. Coupled with artificial intelligence, the model holds potential for training automated classifiers capable of preoperative tissue categorization, ultimately enabling more accurate and individualized clinical decision-making. Future iterations may also integrate imaging data with endocrine profiles, genotypic information, and metabolic parameters to build multidisciplinary predictive models for gynecomastia risk and progression.