Anxiety and Depression in Adolescents with Prelingual Hearing Loss: Prevalence and Risk Factors
Abstract
1. Introduction
2. Materials and Methods
2.1. Participants
2.2. Instruments
2.2.1. Anxiety and Depression Symptoms
2.2.2. Factors Associated with Anxiety and Depression Symptoms
- (a)
- Communication difficulty: The ‘times’ subscale of the Self-Assessment of Communication—Adolescent (SAC-A) was used [32] to assess self-reported communication difficulty. This subscale asks six questions about difficulties hearing and understanding at different times, including when talking in groups of people and listening to the radio or TV. Each question in the subscale is scored from 1 (“almost never”) to 5 (“almost always”). Scores are summed, and higher summed scores indicate greater handicap. The ‘times’ subscale of the Significant Other Assessment of Communication—Adolescent (SOAC-A) [32] was used to assess the parent/carer-reported communication difficulty. SOAC-A is identical to SAC-A, except for asking the questions from the parent’s perspective of the child (e.g., “Is it hard for your child to…”). The internal consistency (Cronbach’s alpha) of SAC-A is 0.85, indicating acceptable internal consistency [33].
- (b)
- Expressive language: The Communication Checklist—Self Report (CC-SR) [34] is a participant/self-reported measure of language structure, pragmatic skills, and social engagement. The language structure subscale used in the present study measures expressive use of grammar and language in social situations (e.g., leaving out or substituting sounds in words; mixing up words like “he” and “him”). For the purposes of scoring, responses were scored as numerical values between 0 (“less than once a week”) to 3 (“several times a day”) and converted to z-scores. For the parent-version, the Communication Checklist—Adult (CC-A) [35] was used. The items and scoring method are identical to the CC-SR, except for reporting in the third person (e.g., “S/he mixes up words that sound similar”). Higher z-scores indicate better language. The internal consistency of CC-A items (Cronbach’s alpha) ranges between 0.91 and 0.97. For CC-SR, the range is between 0.83 and 0.93, indicating acceptable internal consistency [34].
- (c)
- Non-verbal IQ: The norm-referenced Test of Non-Verbal Intelligence (TONI-4) was used [36]. It is designed to require minimal language from both the administrator and the test taker. Index scores are calculated such that 100 is the mean, with a standard deviation of 15. TONI-4 has a Cronbach’s alpha of 0.96, suggesting high internal consistency [36].
- (d)
- Prosocial behaviour: The prosocial subscale of the 25-item self- and parent-reported Strengths and Difficulties (SDQ) questionnaire [37,38] designed for children 11–17 years was used. The SDQ probes the frequency of behaviours related to prosocial behaviour (e.g., whether the person is considerate of other people’s feelings) on a three-point scale (“not true” (0), “somewhat true” (1), “certainly true” (2)). Scores were converted to z-scores using published norms [39]. Higher z-scores indicate better prosocial behaviour. The internal consistency (Cronbach’s alpha) of the self-reported prosocial behaviour scale is 0.65, suggesting acceptable internal consistency [38].
- (e)
- Peer relations: The peer relations subscale of the SDQ that measures the child’s relationship to their peers was used. Higher z-scores indicate less difficulties. The internal consistency (Cronbach’s alpha) of the self-reported peer relations scale is 0.61, suggesting acceptable internal consistency [38].
- (f)
- Additional disabilities: Participants with HL as well as their parents or carers were asked whether the adolescent had “any conditions, disabilities or special needs diagnosed” and responded by ticking boxes or entering any condition indicated as “Other”. For the regressions, the presence of any one additional disability was used as the predictor. Reported additional disabilities included autism spectrum disorder, cerebral palsy, intellectual/developmental disability, attention deficit hyperactivity disorder, attention deficit disorder, vision impairment, learning disability, craniofacial abnormality, and musculoskeletal disorders.
- (g)
- Parent happiness: Parents/carers were asked “Overall, how satisfied are you with life as a whole these days?” and indicated their answer on a scale from 1 (“Not at all satisfied”) to 10 (“Completely satisfied”).
- (h)
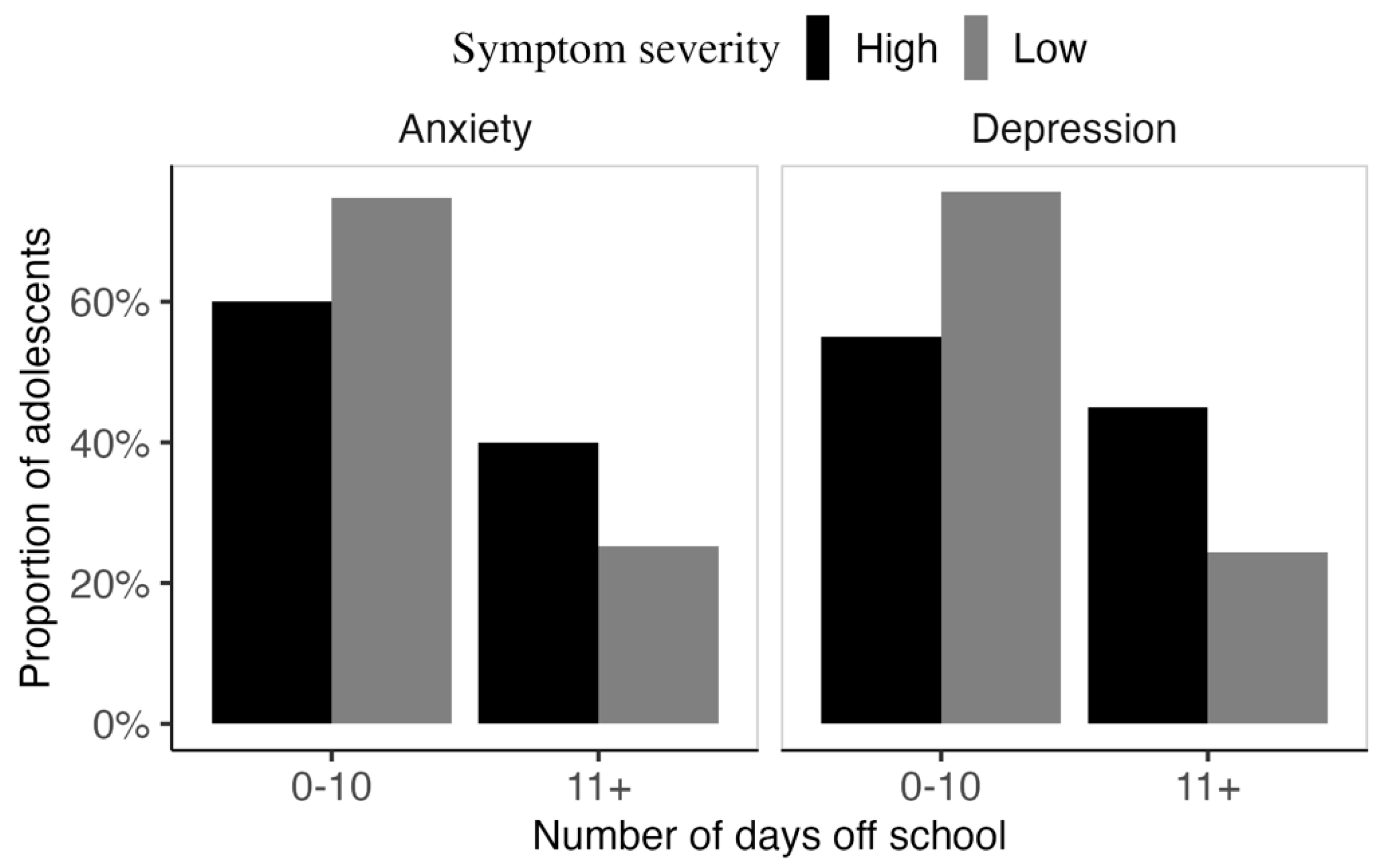
- School days off: To assess whether there was any association between the reported anxiety and depression symptoms and absenteeism, adolescents were asked to estimate the number of days they did not attend school over the past 12 months because of sickness.
2.3. Statistical Analysis
3. Results
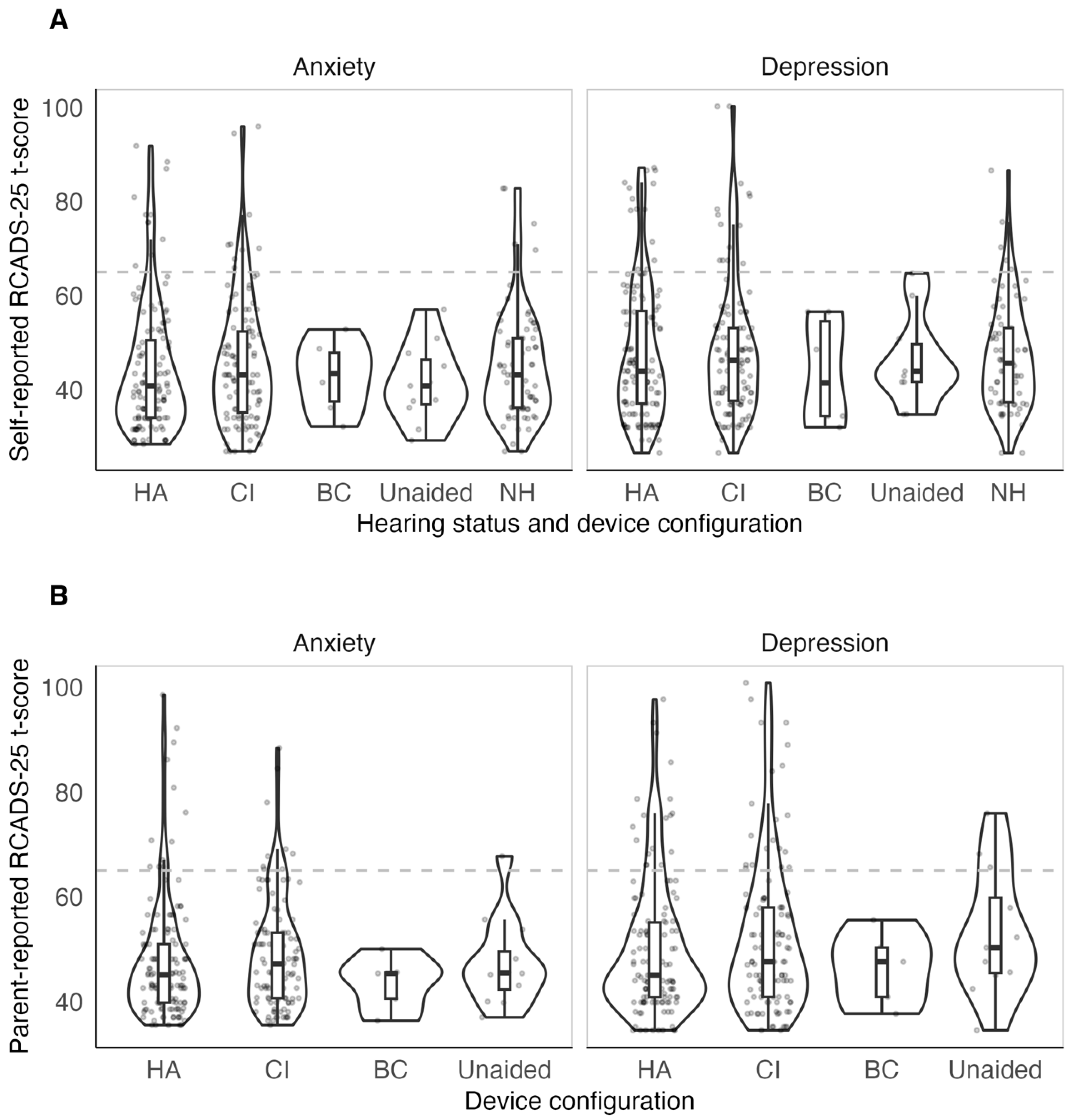
3.1. Anxiety and Depression Symptoms of Adolescents with HL and NH
3.2. Factors Associated with Self-Reported Anxiety Symptoms in HA and CI Users
3.3. Factors Associated with Self-Reported Depression Symptoms in HA and CI Users
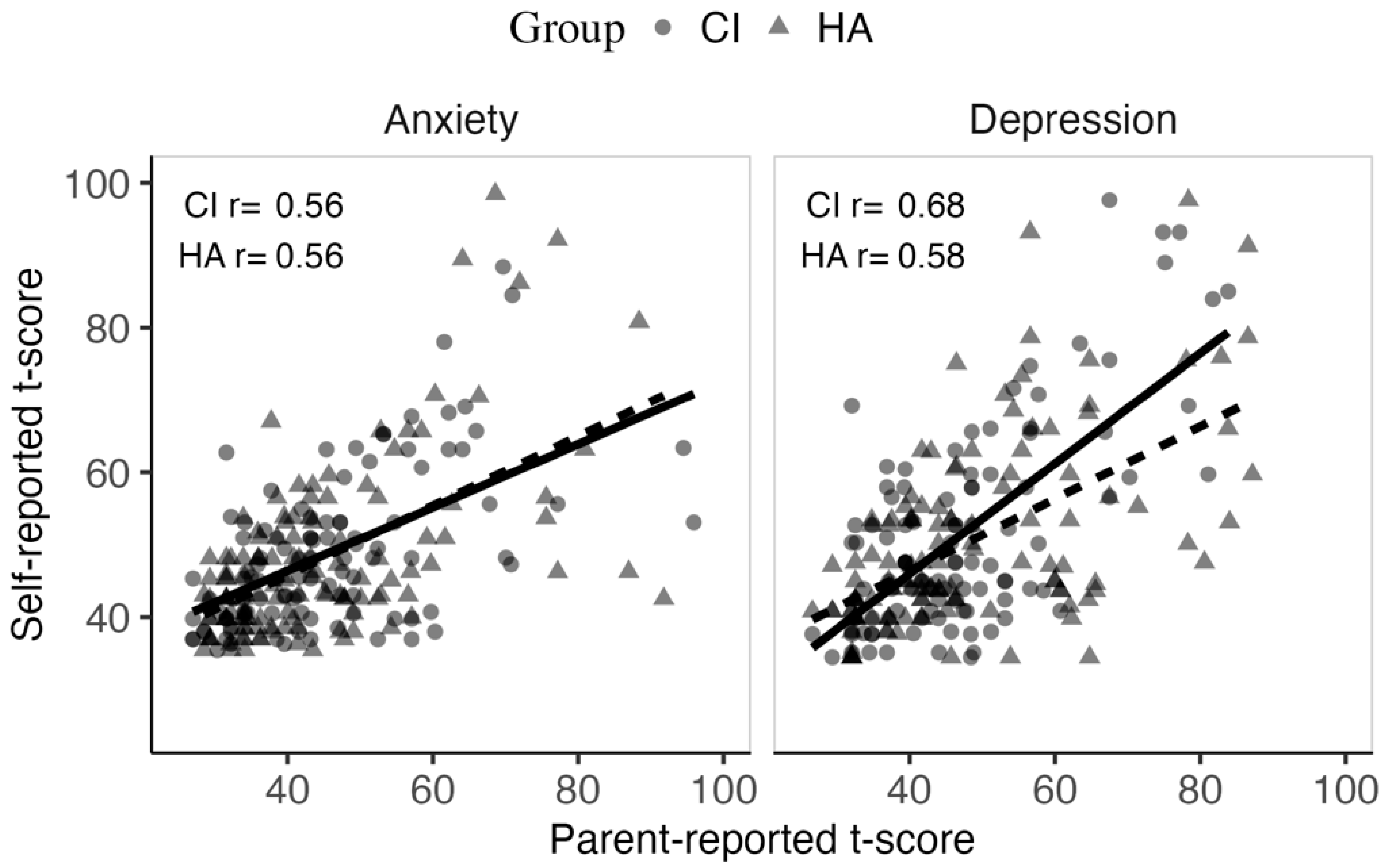
3.4. Association Between Parent and Self-Reported Anxiety and Depression Symptoms in HA and CI Users
3.5. Factors Associated with Parent-Report Anxiety and Depression Symptoms
3.6. Relation Between Anxiety and Depression Symptoms and Days off School
4. Discussion
4.1. Prevalence of Clinically Relevant Anxiety and Depression Levels Did Not Vary Significantly Between Adolescents with and Without HL
4.2. Influential Factors of Mental Well-Being in Adolescents: Gender, Expressive Language, Communication Difficulty and Psychosocial Behaviour
4.3. A Multi-Informant Approach Is Favourable to Assess Mental Health Challenges in Adolescents
4.4. Clinical Implications
4.5. Strengths and Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Theunissen, S.C.; Rieffe, C.; Netten, A.P.; Briaire, J.J.; Soede, W.; Schoones, J.W.; Frijns, J.H. Psychopathology and its risk and protective factors in hearing-impaired children and adolescents: A systematic review. JAMA Pediatr. 2014, 168, 170–177. [Google Scholar] [CrossRef]
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders, 4th ed.; Text Revision; American Psychiatric Association: Washington, DC, USA, 2000. [Google Scholar] [CrossRef]
- Jaycox, L.H.; Stein, B.D.; Paddock, S.; Miles, J.N.; Chandra, A.; Meredith, L.S.; Tanielian, T.; Hickey, S.; Burnam, M.A. Impact of teen depression on academic, social, and physical functioning. Pediatrics 2009, 124, e596–e605. [Google Scholar] [CrossRef] [PubMed]
- de Lijster, J.M.; Dieleman, G.C.; Utens, E.M.W.J.; Dierckx, B.; Wierenga, M.; Verhulst, F.C.; Legerstee, J.S. Social and academic functioning in adolescents with anxiety disorders: A systematic review. J. Affect. Disord. 2018, 230, 108–117. [Google Scholar] [CrossRef]
- Landsberger, S.A.; Diaz, D.R.; Spring, N.Z.; Sheward, J.; Sculley, C. Psychiatric diagnoses and psychosocial needs of outpatient deaf children and adolescents. Child Psychiatry Hum. Dev. 2014, 45, 42–51. [Google Scholar] [CrossRef]
- van Eldik, T. Mental health problems of Dutch youth with hearing loss as shown on the Youth Self Report. Am. Ann. Deaf. 2005, 150, 11–16. [Google Scholar] [CrossRef]
- Hancock, K.J.; Brennan-Jones, C.G.; Vithiatharan, R.; Payne, D.; Runions, K.; Lin, A.; Eikelboom, R.H. Mental health problems among 4–17-year-olds with hearing problems: Results from a nationally representative study. Hear. Balance Commun. 2017, 15, 145–155. [Google Scholar] [CrossRef]
- Kim, S.Y.; Kim, H.J.; Park, E.K.; Joe, J.; Sim, S.; Choi, H.G. Severe hearing impairment and risk of depression: A national cohort study. PLoS ONE 2017, 12, e0179973. [Google Scholar] [CrossRef] [PubMed]
- Fellinger, J.; Holzinger, D.; Gerich, J.; Goldberg, D. Mental distress and quality of life in the hard of hearing. Acta Psychiatr. Scand. 2007, 115, 243–245. [Google Scholar] [CrossRef]
- Butcher, E.; Cortina-Borja, M.; Dezateux, C.; Knowles, R. The association between childhood hearing loss and self-reported peer victimisation, depressive symptoms, and self-harm: Longitudinal analyses of a prospective, nationally representative cohort study. BMC Public Health 2022, 22, 1045. [Google Scholar] [CrossRef] [PubMed]
- Theunissen, S.C.; Rieffe, C.; Kouwenberg, M.; Soede, W.; Briaire, J.J.; Frijns, J.H. Depression in hearing-impaired children. Int. J. Pediatr. Otorhinolaryngol. 2011, 75, 1313–1317. [Google Scholar] [CrossRef]
- Li, H.; Prevatt, F. Deaf and hard of hearing children and adolescents in China: Their fears and anxieties. Am. Ann. Deaf. 2010, 155, 458–466. [Google Scholar] [CrossRef]
- Madhesh, A.; Almohammed, O.A. Prevalence of depression, anxiety, and stigma among high school students with deafness and its association with their quality of school life: A national study from Saudi Arabia. Res. Dev. Disabil. 2025, 156, 104894. [Google Scholar] [CrossRef]
- Vostanis, P.; Hayes, M.; Du Feu, M.; Warren, J. Detection of behavioural and emotional problems in deaf children and adolescents: Comparison of two rating scales. Child Care Health Dev. 1997, 23, 233–246. [Google Scholar] [CrossRef]
- Dammeyer, J. Psychosocial development in a Danish population of children with cochlear implants and deaf and hard-of-hearing children. J. Deaf Stud. Deaf Educ. 2010, 15, 50–58. [Google Scholar] [CrossRef]
- Theunissen, S.C.; Rieffe, C.; Kouwenberg, M.; De Raeve, L.; Soede, W.; Briaire, J.J.; Frijns, J.H. Anxiety in children with hearing aids or cochlear implants compared to normally hearing controls. Laryngoscope 2012, 122, 654–659. [Google Scholar] [CrossRef]
- Fellinger, J.; Holzinger, D.; Sattel, H.; Laucht, M.; Goldberg, D. Correlates of mental health disorders among children with hearing impairments. Dev. Med. Child Neurol. 2009, 51, 635–641. [Google Scholar] [CrossRef]
- Barker, D.H.; Quittner, A.L.; Fink, N.E.; Eisenberg, L.S.; Tobey, E.A.; Niparko, J.K.; CDaCI Investigative Team. Predicting behavior problems in deaf and hearing children: The influences of language, attention, and parent-child communication. Dev. Psychopathol. 2009, 21, 373–392. [Google Scholar] [CrossRef] [PubMed]
- van Eldik, T.; Treffers, P.D.; Veerman, J.W.; Verhulst, F.C. Mental health problems of deaf Dutch children as indicated by parents’ responses to the child behavior checklist. Am. Ann. Deaf. 2004, 148, 390–395. [Google Scholar] [CrossRef] [PubMed]
- Percy-Smith, L.; Jensen, J.H.; Cayé-Thomasen, P.; Thomsen, J.; Gudman, M.; Lopez, A.G. Factors that affect the social well-being of children with cochlear implants. Cochlear Implant. Int. 2008, 9, 199–214. [Google Scholar] [CrossRef]
- Fellinger, J.; Holzinger, D.; Beitel, C.; Laucht, M.; Goldberg, D.P. The impact of language skills on mental health in teenagers with hearing impairments. Acta Psychiatr. Scand. 2009, 120, 153–159. [Google Scholar] [CrossRef] [PubMed]
- Sahli, S.; Arslan, U.; Belgin, E. Depressive emotioning in adolescents with cochlear implant and normal hearing. Int. J. Pediatr. Otorhinolaryngol. 2009, 73, 1774–1779. [Google Scholar] [CrossRef]
- Huber, M.; Kipman, U. The mental health of deaf adolescents with cochlear implants compared to their hearing peers. Int. J. Audiol. 2011, 50, 146–154. [Google Scholar] [CrossRef] [PubMed]
- Kouwenberg, M.; Rieffe, C.; Theunissen, S.C.P.M. Intrapersonal and interpersonal factors related to self-reported symptoms of depression in DHH youth. Int. J. Ment. Health Deaf. 2011, 1, 46–57. [Google Scholar]
- van Gent, T.; Goedhart, A.W.; Hindley, P.A.; Treffers, P.D. Prevalence and correlates of psychopathology in a sample of deaf adolescents. J. Child Psychol. Psychiatry Allied Discip. 2007, 48, 950–958. [Google Scholar] [CrossRef] [PubMed]
- De Los Reyes, A.; Kazdin, A.E. Informant discrepancies in the assessment of childhood psychopathology: A critical review, theoretical framework, and recommendations for further study. Psychol. Bull. 2005, 131, 483–509. [Google Scholar] [CrossRef]
- Clarke-Stewart, K.A.; Allhusen, V.D.; McDowell, D.J.; Thelen, L.; Call, J.D. Identifying psychological problems in young children: How do mothers compare with child psychiatrists? J. Appl. Dev. Psychol. 2003, 23, 589–624. [Google Scholar] [CrossRef]
- Ching, T.Y.; Leigh, G.; Dillon, H. Introduction to the longitudinal outcomes of children with hearing impairment (LOCHI) study: Background, design, sample characteristics. Int. J. Audiol. 2013, 52 (Suppl. S2), S4–S9. [Google Scholar] [CrossRef]
- Ebesutani, C.; Reise, S.P.; Chorpita, B.F.; Ale, C.; Regan, J.; Young, J.; Higa-McMillan, C.; Weisz, J.R. The Revised Child Anxiety and Depression Scale-Short Version: Scale reduction via exploratory bifactor modeling of the broad anxiety factor. Psychol. Assess. 2012, 24, 833–845. [Google Scholar] [CrossRef]
- Australian Bureau of Statistics, 2006. 2033.0.55.001-Socio-Economic Indexes for Areas (SEIFA). 2006. Available online: https://www.abs.gov.au/AUSSTATS/abs@.nsf/Lookup/2033.0.55.001Main+Features12006 (accessed on 1 July 2025).
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders, 4th ed.; American Psychiatric Association: Washington, DC, USA, 1994. [Google Scholar] [CrossRef]
- Elkayam, J.; English, K. Counseling adolescents with hearing loss with the use of self-assessment/significant other questionnaires. J. Am. Acad. Audiol. 2003, 14, 485–499. [Google Scholar] [CrossRef] [PubMed]
- Wright, K.; English, K.; Elkayam, J. Reliability of the Self-Assessment of Communication–Adolescent. J. Educ. Audiol. 2010, 16, 30–36. [Google Scholar]
- Bishop, D.V.M.; Whitehouse, A.J.O.; Sharp, M. Communication Checklist–Self Report (CC-SR); Pearson: London, UK, 2009. [Google Scholar]
- Whitehouse, A.J.O.; Bishop, D.V.M. Communication Checklist–Adult (CC-A); Pearson: London, UK, 2009. [Google Scholar]
- Brown, L.; Sherbenou, R.J.; Johnsen, S.K. Test of Nonverbal Intelligence-4 (TONI-4); PRO-ED: Austin, TX, USA, 2010. [Google Scholar]
- Goodman, R. The Strengths and Difficulties Questionnaire: A research note. J. Child Psychol. Psychiatry Allied Discip. 1997, 38, 581–586. [Google Scholar] [CrossRef] [PubMed]
- Goodman, R.; Meltzer, H.; Bailey, V. The Strengths and Difficulties Questionnaire: A pilot study on the validity of the self-report version. Eur. Child Adolesc. Psychiatry 1998, 7, 125–130. [Google Scholar] [CrossRef]
- Mellor, D. Normative data for the strengths and difficulties questionnaire in Australia. Aust. Psychol. 2005, 40, 215–222. [Google Scholar] [CrossRef]
- Hodes, M.; Schow, R.; Brockett, J. New support for hearing aid measures: The computerized SAC and SOAC. Hear. Rev. 2009, 16, 26–36. [Google Scholar]
- R Core Team. R: A Language and Environment for Statistical Computing; R Foundation for Statistical Computing: Vienna, Austria, 2024. [Google Scholar]
- van Buuren, S.; Groothuis-Oudshoorn, K. mice: Multivariate imputation by chained equations in R. J. Stat. Softw. 2011, 45, 1–67. [Google Scholar] [CrossRef]
- Alarcón, G.; Forbes, E.E. Prosocial Behavior and Depression: A Case for Developmental Gender Differences. Curr. Behav. Neurosci. Rep. 2017, 4, 117–127. [Google Scholar] [CrossRef]
- Kochel, K.P.; Ladd, G.W.; Rudolph, K.D. Longitudinal associations among youth depressive symptoms, peer victimization, and low peer acceptance: An interpersonal process perspective. Child Dev. 2012, 83, 637–650. [Google Scholar] [CrossRef]
- Boivin, M.; Hymel, S.; Bukowski, W.M. The roles of social withdrawal, peer rejection, and victimization by peers in predicting loneliness and depressed mood in childhood. Dev. Psychopathol. 1995, 7, 765–785. [Google Scholar] [CrossRef]
- Nantel-Vivier, A.; Pihl, R.O.; Côté, S.; Tremblay, R.E. Developmental association of prosocial behaviour with aggression, anxiety and depression from infancy to preadolescence. J. Child Psychol. Psychiatry Allied Discip. 2014, 55, 1135–1144. [Google Scholar] [CrossRef]
- Long, J.; Attuquayefio, T.; Hudson, J.L. Factors Associated with Anxiety Symptoms in Australian Deaf or Hard of Hearing Children. J. Deaf Stud. Deaf Educ. 2021, 26, 13–20. [Google Scholar] [CrossRef]
- Kovacs, M.; Devlin, B. Internalizing Disorders in Childhood. J. Child Psychol. Psychiatry Allied Discip. 1998, 39, 47–63. [Google Scholar] [CrossRef]
- Cejas, I.; Coto, J.; Sanchez, C.; Holcomb, M.; Lorenzo, N.E. Prevalence of Depression and Anxiety in Adolescents with Hearing Loss. Otol. Neurotol. 2021, 42, e470–e475. [Google Scholar] [CrossRef] [PubMed]
- Chorpita, B.F.; Yim, L.; Moffitt, C.; Umemoto, L.A.; Francis, S.E. Assessment of symptoms of DSM-IV anxiety and depression in children: A revised child anxiety and depression scale. Behav. Res. Ther. 2000, 38, 835–855. [Google Scholar] [CrossRef] [PubMed]
- Chronister, B.N.; Gonzalez, E.; Lopez-Paredes, D.; Suarez-Torres, J.; Gahagan, S.; Martinez, D.; Barros, J.; Jacobs, D.R.; Checkoway, H., Jr.; Suarez-Lopez, J.R. Testosterone, estradiol, DHEA and cortisol in relation to anxiety and depression scores in adolescents. J. Affect. Disord. 2021, 294, 838–846. [Google Scholar] [CrossRef] [PubMed]
- Luo, D.; Dashti, S.G.; Sawyer, S.M.; Vijayakumar, N. Pubertal hormones and mental health problems in children and adolescents: A systematic review of population-based studies. eClinicalMedicine 2024, 76, 102828. [Google Scholar] [CrossRef]
| HA | CI | BC | Unaided | NH | ||
|---|---|---|---|---|---|---|
| Number | 127 | 106 | 6 | 11 | 69 | |
| Age at test (years) | mean (SD; min–max) | 17.14 (0.7; 16–19.3) | 16.96 (0.7; 16–19.2) | 16.9 (0.5; 16.3–17.6) | 17.17 (0.7; 16.4–18.9) | 16.81 (0.6; 16–18) |
| Gender | Female | 54 (42.5%) | 52 (49.1%) | 3 (50%) | 3 (27.3%) | 30 (43.5%) |
| Male | 73 (57.5%) | 54 (50.9%) | 3 (50%) | 8 (72.7%) | 39 (56.5%) | |
| Non-verbal IQ | mean (SD; min–max) | 97.73 (10.1; 71–122) | 96.66 (11.9; 70–122) | 96.25 (11.2; 85–111) | 88.62 (10.6; 70–107) | 100.46 (10.3; 83–122) |
| Better ear 4-freq average (dB HL) | mean (SD; min–max) | 51.01 (15.1; 23.8–105) | 112.51 (23.2; 30–125) | 63.12 (5; 53.8–67.5) | 31.82 (11.4; 20–51.2) | 19 (0; 19–19) |
| Better ear HL degree | Normal | 0 (0%) | 0 (0%) | 0 (0%) | 0 (0%) | 69 (100%) |
| Mild | 33 (26%) | 2 (1.9%) | 0 (0%) | 7 (63.6%) | 0 (0%) | |
| Moderate | 84 (66.1%) | 7 (6.6%) | 6 (100%) | 4 (36.4%) | 0 (0%) | |
| Severe | 10 (7.9%) | 97 (91.5%) | 0 (0%) | 0 (0%) | 0 (0%) | |
| Age at first hearing device (months) | mean (SD; min–max) | 10.68 (10.2; 1.2–35.8) | 8.62 (8.9; 0.9–34.3) | 2.23 (1.2; 1.2–3.9) | 13.11 (10.1; 2.5–36.4) | NA |
| Age at first CI (months) | mean (SD; min–max) | NA | 37.68 (39.6; 5–184) | NA | NA | NA |
| Device configuration | Unilateral | 4 (3.1%) | 7 (6.6%) | 1 (16.7%) | NA | NA |
| Bilateral | 123 (96.9%) | 77 (72.6%) | 5 (83.3%) | NA | NA | |
| Bimodal | NA | 22 (20.8%) | NA | NA | NA | |
| Additional Disabilities | Yes | 54 (42.5%) | 37 (34.9%) | 4 (66.7%) | 4 (36.4%) | 0 (0%) |
| No | 73 (57.5%) | 69 (65.1%) | 2 (33.3%) | 7 (63.6%) | 69 (100%) | |
| Device use all day | Yes | 88 (69.3%) | 93 (87.7%) | 6 (100%) | 0 (0%) | 0 (0%) |
| No | 35 (27.6%) | 12 (11.3%) | 0 (0%) | 7 (63.6%) | 0 (0%) | |
| Declined to answer | 4 (3.1%) | 1 (0.9%) | 0 (0%) | 4 (36.4%) | NA | |
| IRSAD quartile | 1 | 12 (9.4%) | 11 (10.4%) | 1 (16.7%) | 2 (18.2%) | 10 (14.5%) |
| 2 | 22 (17.3%) | 19 (17.9%) | 0 (0%) | 2 (18.2%) | 14 (20.3%) | |
| 3 | 29 (22.8%) | 20 (18.9%) | 5 (83.3%) | 2 (18.2%) | 18 (26.1%) | |
| 4 (most advantage) | 64 (50.4%) | 56 (52.8%) | 0 (0%) | 5 (45.5%) | 27 (39.1%) | |
| School type | Distance education | 1 (0.8%) | 0 (0%) | 0 (0%) | 0 (0%) | 0 (0%) |
| Homeschool | 1 (0.8%) | 0 (0%) | 0 (0%) | 0 (0%) | 0 (0%) | |
| Mainstream | 109 (85.8%) | 92 (86.8%) | 6 (100%) | 11 (100%) | 69 (100%) | |
| Special education | 4 (3.1%) | 3 (2.8%) | 0 (0%) | 0 (0%) | 0 (0%) | |
| Not at school | 12 (9.4%) | 9 (8.5%) | 0 (0%) | 0 (0%) | 0 (0%) | |
| Declined to answer | 0 (0%) | 2 (1.9%) | 0 (0%) | 0 (0%) | 0 (0%) |
| Anxiety | Depression | ||||||||
|---|---|---|---|---|---|---|---|---|---|
| Informant | Group | N | Mean (SD) | High Severity, n (%) | Low Severity, n (%) | N | Mean (SD) | High Severity, n (%) | Low Severity, n (%) |
| Self | HL | 250 | 44.78 (13.4) | 20 (8%) | 230 (92%) | 250 | 47.85 (14.3) | 28 (11.2%) | 222 (88.8%) |
| Self | NH | 69 | 45.23 (12.1) | 5 (7.2%) | 64 (92.8%) | 69 | 47.03 (11.6) | 5 (7.2%) | 64 (92.8%) |
| Parent | HL | 258 | 48.19 (11) | 22 (8.5%) | 236 (91.5%) | 259 | 51 (13.6) | 41 (15.8%) | 218 (84.2%) |
| NH, HA, CI (n = 302) | Estimate (SE) | t (df) | p Value |
|---|---|---|---|
| (Intercept) | 39.32 (6.8) | 5.78 (225.7) | <0.001 |
| Group: HA (reference NH) | −0.48 (1.7) | −0.28 (291.9) | 0.779 |
| Group: CI (reference NH) | −1.65 (1.8) | −0.92 (292.0) | 0.359 |
| Gender: Male (reference female) | −5.57 (1.3) | −4.18 (290.5) | <0.001 |
| Non-verbal IQ | 1.23 (0.7) | 1.82 (218.8) | 0.070 |
| SES | −0.35 (0.7) | −0.52 (290.5) | 0.603 |
| Expressive language | −5.19 (0.6) | −9.03 (283.8) | <0.001 |
| Adjusted R2 | 27.30% | ||
| HA (n = 127) | Estimate (SE) | t (df) | p value |
| (Intercept) | 46.38 (6.3) | 7.35 (114.9) | <0.001 |
| Gender: Male (reference female) | −1.93 (2.3) | −0.83 (114.9) | 0.406 |
| Additional Disabilities: Yes (reference none) | −1.52 (2.2) | −0.70 (115.4) | 0.484 |
| Expressive language | −3.75 (1.1) | −3.49 (112.0) | 0.001 |
| Age at first HA fit | −1.75 (1.1) | −1.64 (115.5) | 0.104 |
| Prosocial behaviour | −1.45 (1.1) | −1.33 (112.7) | 0.186 |
| Peer relations | −1.94 (1.0) | −1.94 (112.5) | 0.055 |
| Communication difficulty | 0.57 (0.3) | 2.13 (114.6) | 0.036 |
| BE 4freq PTA | −1.01 (0.7) | −1.36 (115.4) | 0.176 |
| Adjusted R2 | 31.70% | ||
| CI (n = 106) | Estimate (SE) | t (df) | p value |
| (Intercept) | 16.59 (10.6) | 1.57 (94.4) | 0.120 |
| Gender: Male (reference female) | −4.01 (2.3) | −1.77 (94.5) | 0.079 |
| Additional Disabilities: Yes (reference none) | −3.16 (2.4) | −1.31 (94.5) | 0.192 |
| Expressive language | −3.10 (0.9) | −3.38 (93.2) | 0.001 |
| Age at first CI | 2.20 (1.5) | 1.48 (94.3) | 0.142 |
| Prosocial behaviour | 1.62 (1.0) | 1.58 (93.9) | 0.118 |
| Peer relations | −1.22 (1.0) | −1.25 (94.4) | 0.214 |
| Communication difficulty | 0.89 (0.3) | 3.40 (94.6) | 0.001 |
| BE 4freq PTA | 0.77 (0.6) | 1.38 (94.2) | 0.170 |
| Adjusted R2 | 31.70% |
| NH, HA, CI (n = 302) | Estimate (SE) | t (df) | p Value |
|---|---|---|---|
| (Intercept) | 37.78 (7.1) | 5.35 (266.4) | <0.001 |
| Group: HA (reference NH) | 1.56 (1.8) | 0.85 (291.7) | 0.397 |
| Group: CI (reference NH) | −0.10 (1.9) | −0.05 (292.3) | 0.959 |
| Gender: Male (reference female) | −4.85 (1.4) | −3.40 (290.1) | 0.001 |
| Non-verbal IQ | 1.87 (0.7) | 2.68 (265.2) | 0.008 |
| SES | −1.59 (0.7) | −2.23 (291.4) | 0.026 |
| Expressive language | −4.89 (0.6) | −7.99 (287.0) | <0.001 |
| Adjusted R2 | 24.20% | ||
| HA (n = 127) | Estimate (SE) | t (df) | p value |
| (Intercept) | 31.82 (12.5) | 2.54 (108.1) | 0.012 |
| Gender: Male (reference female) | 0.61 (2.4) | 0.25 (112.0) | 0.801 |
| Non-verbal IQ | 2.03 (1.2) | 1.74 (106.9) | 0.085 |
| Additional Disabilities: Yes (reference none) | −0.48 (2.2) | −0.21 (112.8) | 0.831 |
| SES | −1.03 (1.2) | −0.88 (111.8) | 0.379 |
| Expressive language | −3.53 (1.2) | −3.02 (109.2) | 0.003 |
| Age at first HA fit | −1.45 (1.3) | −1.11 (113.2) | 0.271 |
| Prosocial behaviour | −3.44 (1.1) | −3.05 (111.1) | 0.003 |
| Peer relations | −2.14 (1.1) | −1.98 (110.2) | 0.050 |
| Communication difficulty | 0.62 (0.3) | 2.17 (112.5) | 0.032 |
| BE 4freq PTA | −1.32 (0.8) | −1.71 (113.3) | 0.090 |
| Adjusted R2 | 35.30% | ||
| CI (n = 106) | Estimate (SE) | t (df) | p value |
| (Intercept) | 14.07 (16.0) | 0.88 (89.8) | 0.380 |
| Gender: Male (reference female) | −4.47 (2.5) | −1.79 (92.4) | 0.077 |
| Non-verbal IQ | 2.02 (1.1) | 1.91 (85.3) | 0.059 |
| Additional Disabilities: Yes (reference none) | −0.90 (2.6) | −0.34 (91.6) | 0.735 |
| SES | −2.03 (1.2) | −1.74 (92.9) | 0.086 |
| Expressive language | −2.48 (1.1) | −2.28 (87.9) | 0.025 |
| Age at first CI | 1.24 (1.6) | 0.76 (92.3) | 0.450 |
| Prosocial behaviour | −1.15 (1.1) | −1.02 (91.8) | 0.309 |
| Peer relations | −2.16 (1.1) | −2.03 (92.3) | 0.045 |
| Communication difficulty | 0.81 (0.3) | 2.81 (92.5) | 0.006 |
| BE 4freq PTA | 0.36 (0.6) | 0.59 (92.3) | 0.556 |
| Adjusted R2 | 36.30% |
| Subscale | Group | Low—Both | High—Both | High—Parent Only | High—Self Only |
|---|---|---|---|---|---|
| Anxiety | CI | 89/104 (85.6) | 3/104 (2.9) | 6/104 (5.8) | 6/104 (5.8) |
| HA | 106/123 (86.2) | 5/123 (4.1) | 6/123 (4.9) | 6/123 (4.9) | |
| Depression | CI | 82/105 (78.1) | 10/105 (9.5) | 9/105 (8.6) | 4/105 (3.8) |
| HA | 98/123 (79.7) | 6/123 (4.9) | 11/123 (8.9) | 8/123 (6.5) |
| Parent-rated Anxiety | |||
| HA, CI (n = 241) | Estimate (SE) | t (df) | p value |
| (Intercept) | 43.85 (8.0) | 5.47 (187.3) | <0.001 |
| Group: CI (reference HA) | −0.17 (2.3) | −0.07 (226.4) | 0.941 |
| Gender: Male (reference female) | −3.95 (1.2) | −3.16 (226.0) | 0.002 |
| Non-verbal IQ | 0.55 (0.6) | 0.86 (148.8) | 0.392 |
| Additional Disability: Yes (reference None) | 1.43 (1.3) | 1.09 (226.7) | 0.277 |
| SES | −1.71 (0.6) | −2.74 (226.3) | 0.007 |
| Parent happiness | −0.78 (0.4) | −1.77 (213.7) | 0.078 |
| Parent-rated Expressive language | 0.11 (0.7) | 0.16 (207.0) | 0.875 |
| Parent-rated prosocial behaviour | 1.55 (0.6) | 2.62 (225.8) | 0.009 |
| Parent rated peer relations | −3.65 (0.7) | −5.40 (226.6) | <0.001 |
| Parent-rated communication difficulties | 0.64 (0.1) | 4.48 (222.3) | <0.001 |
| BE 4freq PTA | 0.04(0.3) | 0.11 (226.4) | 0.911 |
| Adjusted R2 | 32.02% | ||
| Parent-rated Depression | |||
| HA, CI (n = 242) | Estimate (SE) | t (df) | p value |
| (Intercept) | 43.17 (9.6) | 4.49 (170.5) | <0.001 |
| Group: CI (reference HA) | 1.89 (2.7) | 0.70 (226.6) | 0.486 |
| Gender: Male (reference female) | −4.16 (1.5) | −2.83 (226.2) | 0.005 |
| Non-verbal IQ | 0.97 (0.8) | 1.22 (109.9) | 0.225 |
| Additional Disability: Yes (reference None) | 2.17 (1.5) | 1.40 (227.4) | 0.162 |
| SES | −1.71 (0.7) | −2.33 (225.9) | 0.021 |
| Parent happiness | −1.20 (0.5) | −2.38 (227.4) | 0.018 |
| Parent-rated Expressive language | 0.93 (0.8) | 1.10 (201.4) | 0.273 |
| Parent-rated prosocial behaviour | −0.60 (0.7) | −0.86 (227.0) | 0.389 |
| Parent rated peer relations | −4.37 (0.8) | −5.51 (227.3) | <0.001 |
| Parent-rated communication difficulties | 0.85 (0.2) | 5.01 (216.4) | <0.001 |
| BE 4freq PTA | −0.19 (0.4) | −0.50 (226.7) | 0.62 |
| Adjusted R2 | 38.10% |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Easwar, V.; Gavrilis, J.; Söderström, P.; Ching, T.; Leigh, G.; Zhang, V. Anxiety and Depression in Adolescents with Prelingual Hearing Loss: Prevalence and Risk Factors. J. Clin. Med. 2025, 14, 7538. https://doi.org/10.3390/jcm14217538
Easwar V, Gavrilis J, Söderström P, Ching T, Leigh G, Zhang V. Anxiety and Depression in Adolescents with Prelingual Hearing Loss: Prevalence and Risk Factors. Journal of Clinical Medicine. 2025; 14(21):7538. https://doi.org/10.3390/jcm14217538
Chicago/Turabian StyleEaswar, Vijayalakshmi, Jason Gavrilis, Pelle Söderström, Teresa Ching, Greg Leigh, and Vicky Zhang. 2025. "Anxiety and Depression in Adolescents with Prelingual Hearing Loss: Prevalence and Risk Factors" Journal of Clinical Medicine 14, no. 21: 7538. https://doi.org/10.3390/jcm14217538
APA StyleEaswar, V., Gavrilis, J., Söderström, P., Ching, T., Leigh, G., & Zhang, V. (2025). Anxiety and Depression in Adolescents with Prelingual Hearing Loss: Prevalence and Risk Factors. Journal of Clinical Medicine, 14(21), 7538. https://doi.org/10.3390/jcm14217538







