Exploring Lumbar Spine Posture and Movement in Sitting: A Comparison Between Laboratory and Real-World Measures
Abstract
1. Introduction
2. Materials and Methods
2.1. Participants
2.2. Experimental Setup
2.3. Experimental Procedure
2.3.1. Laboratory Testing
- Upright sitting: participants were instructed to “sit normally” in an upright position on a stool without a backrest (10 s) with their arms crossed and knees flexed at 90°.
- Questionnaire sitting: participants were instructed to “sit as you prefer” on a stool while completing an online questionnaire (2–5 min) via their smartphone.
- Unstable sitting: participants maintained balance while sitting on an unstable surface [19,20]. Part of an aluminium hemisphere (undersurface of the seat; radius: 250 mm; height of seat: 195 mm) and an adjustable footplate to accommodate 90° knee flexion were attached to the seat. A safety bar was placed in case of balance loss. Participants maintain balance during trials with eyes open (EO unstable sitting) and closed (EC unstable sitting) and were instructed to “sit relaxed and upright as quietly as possible”. Six trials were performed (duration 60 s, rest ~60 s) in random order of three with EO and EC.
2.3.2. Real-World Testing (48 h)
2.4. Data Processing
2.4.1. Estimation of Spine Orientation
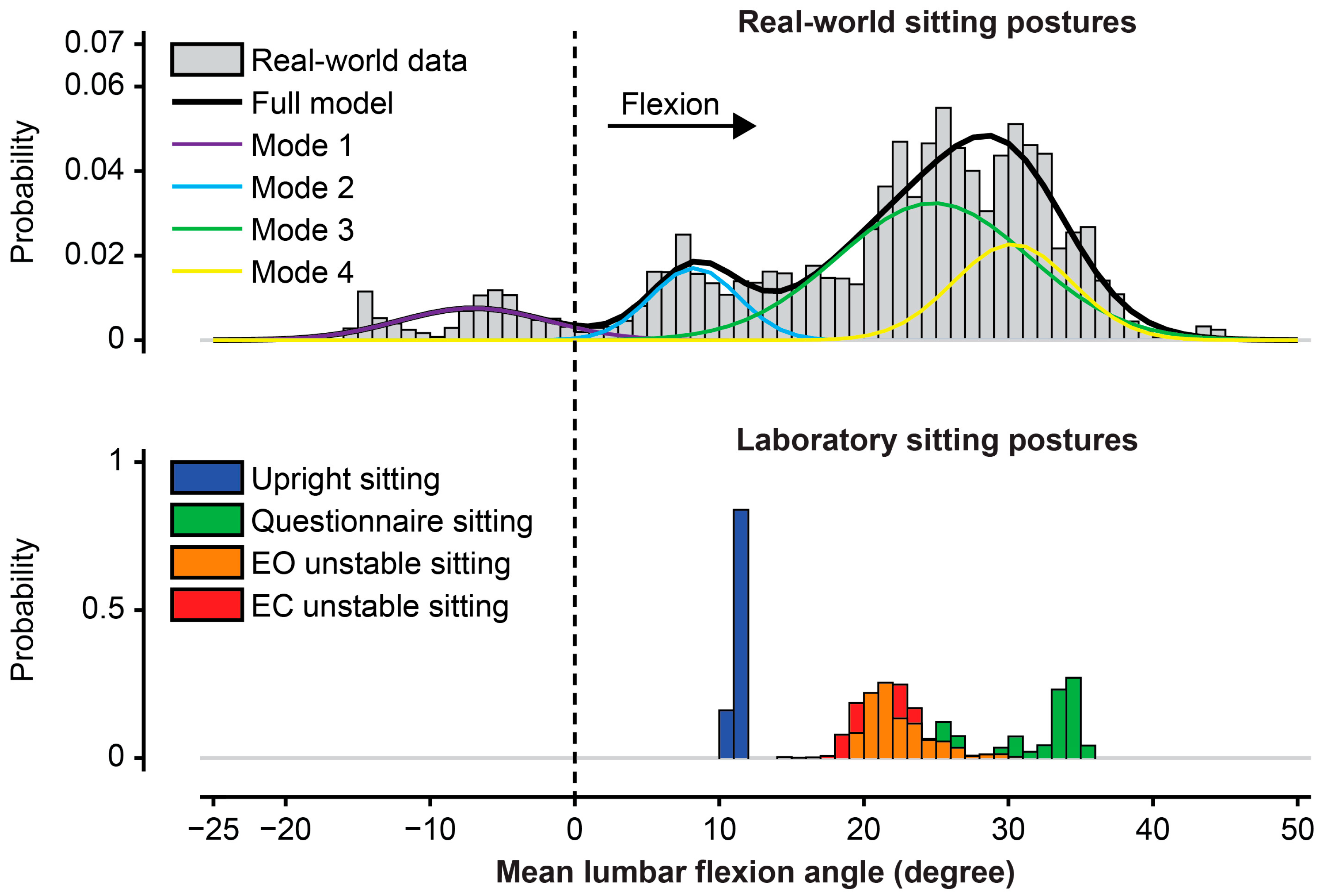
2.4.2. Modelling Distributions of Real-World Spinal Postures
2.4.3. Outcome Measures
2.5. Statistical Analysis
3. Results
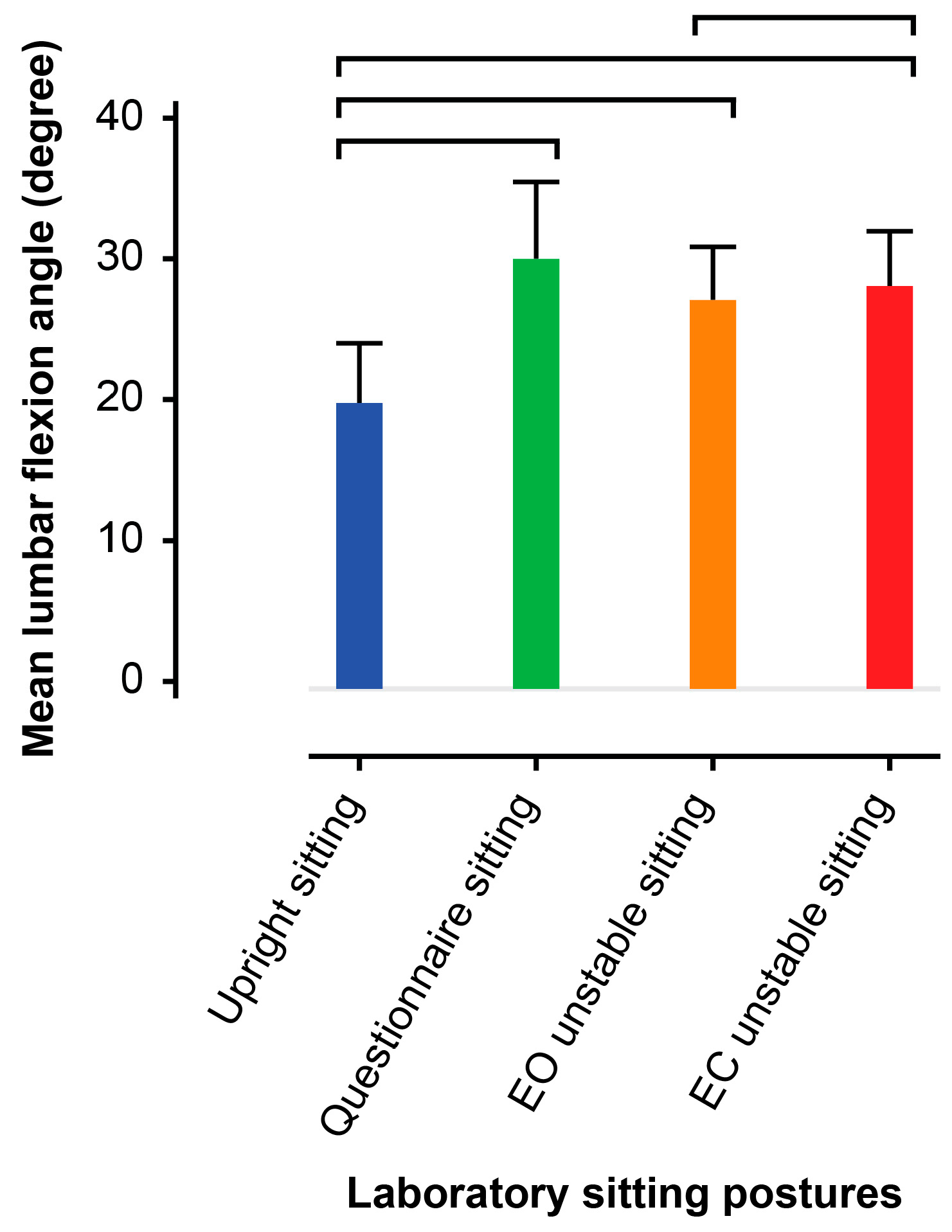
3.1. Characteristics of Laboratory Sitting
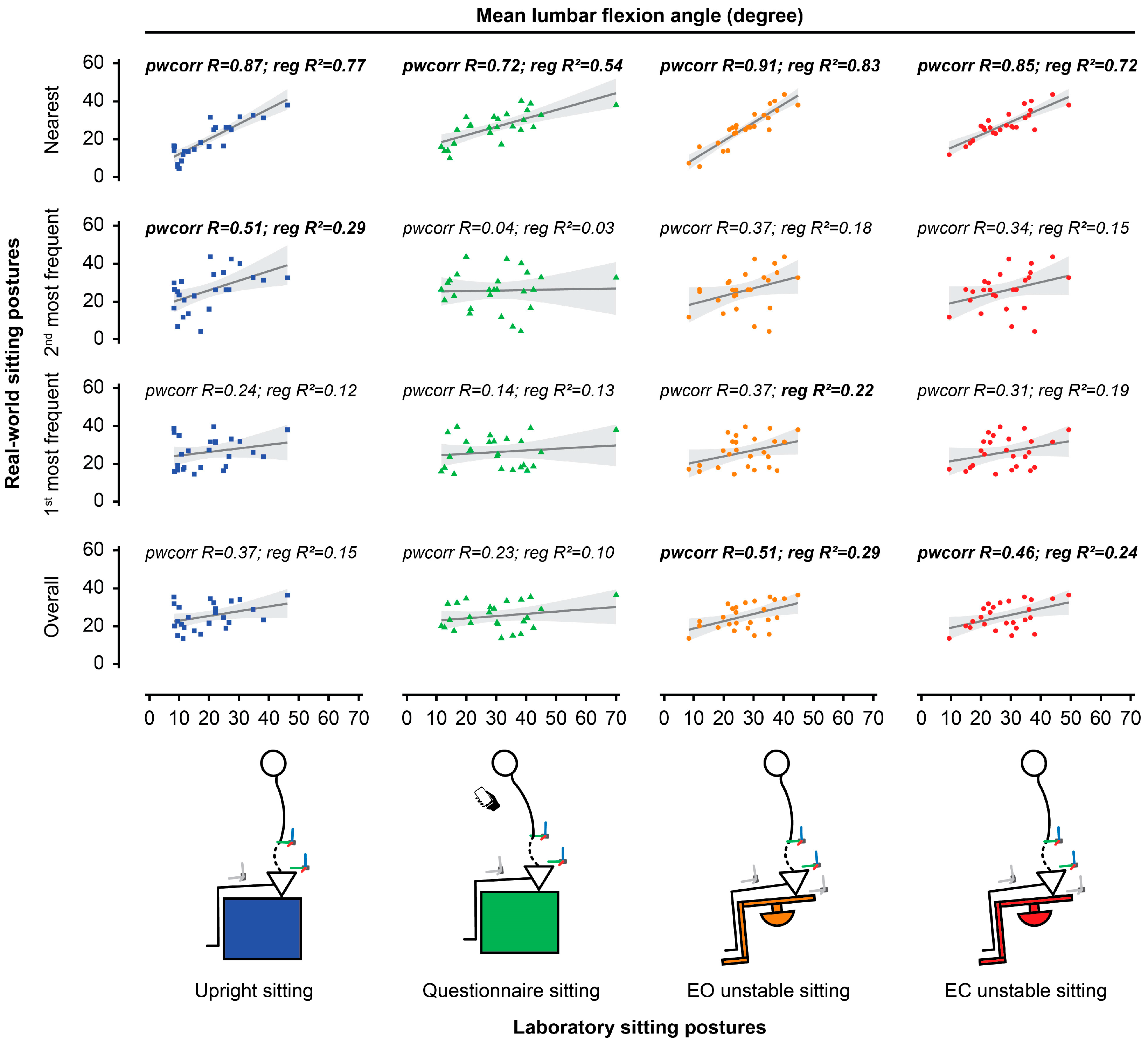
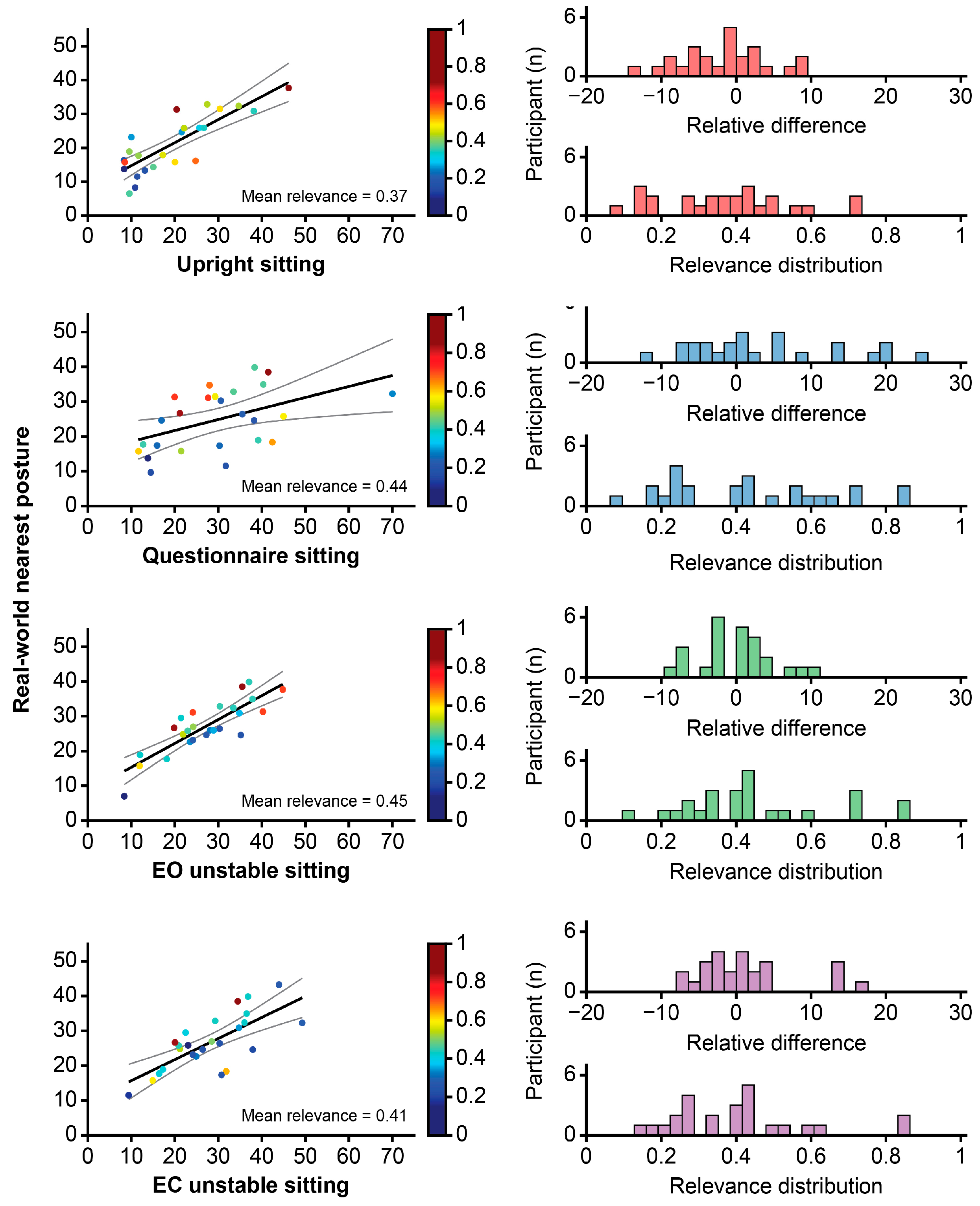
3.2. Relationship Between Laboratory and Real-World Sitting Postures
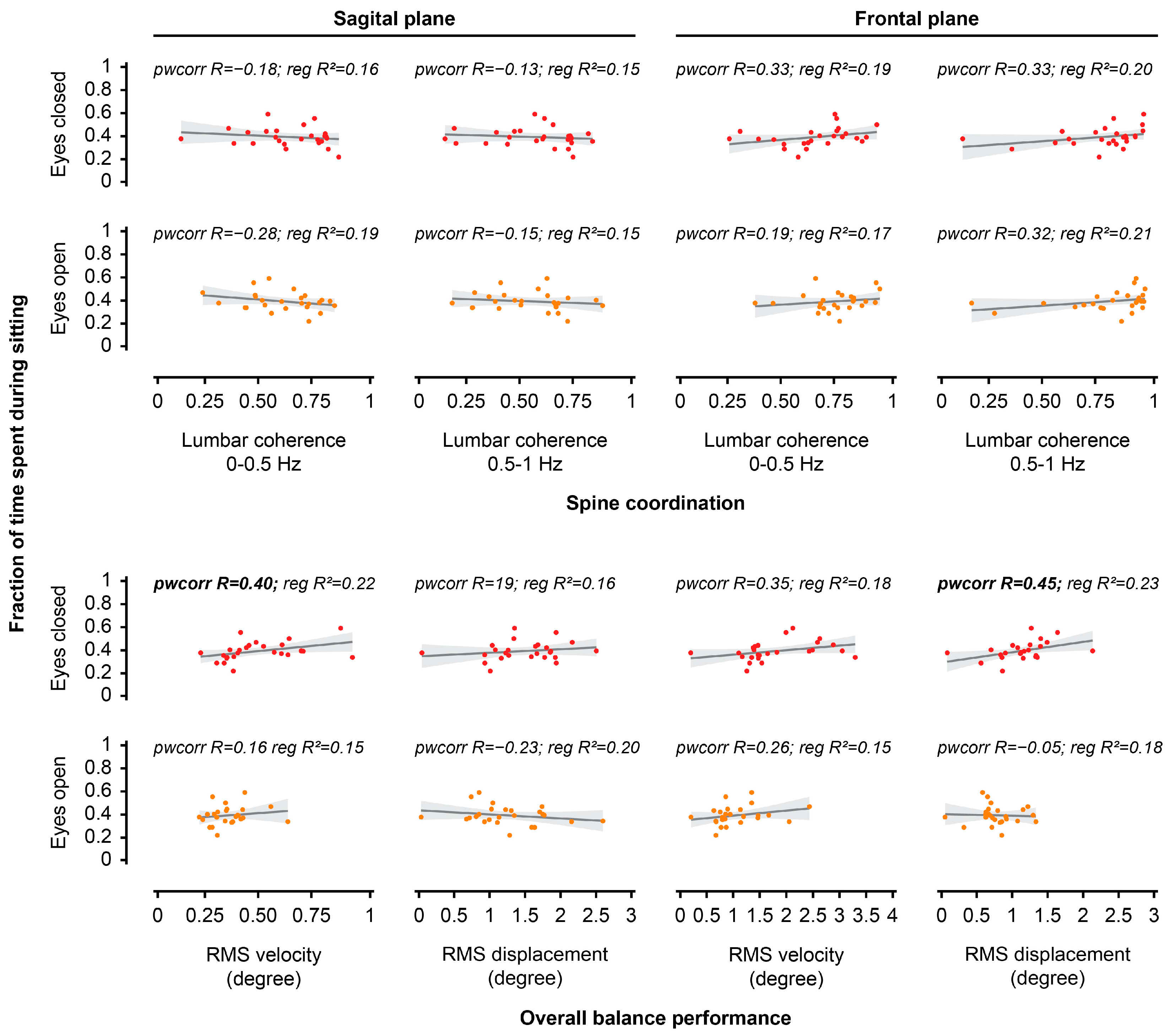
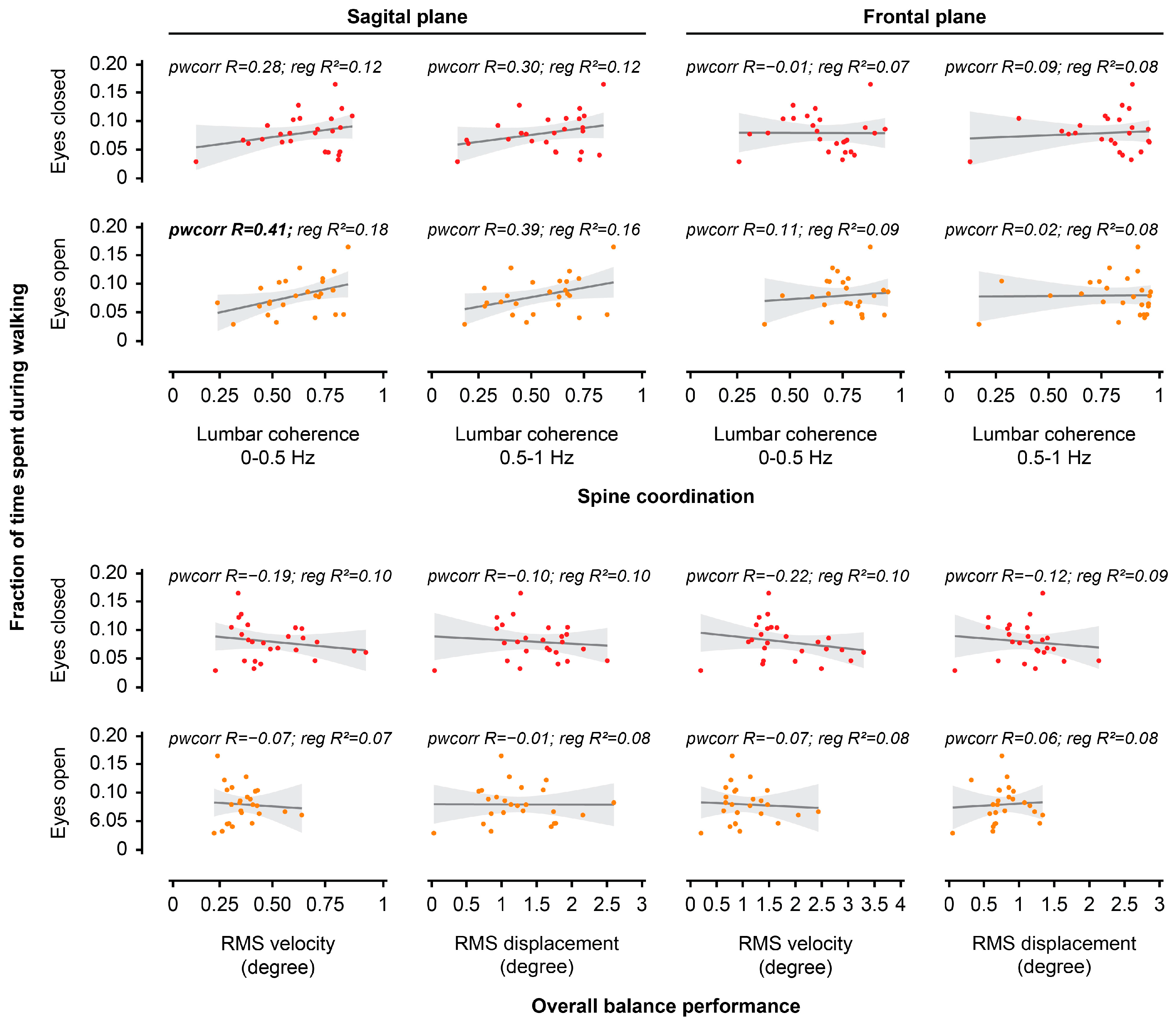
3.3. Relationship Between Performance During Unstable Sitting in the Laboratory and Sedentary/Activity Behaviours in the Real World
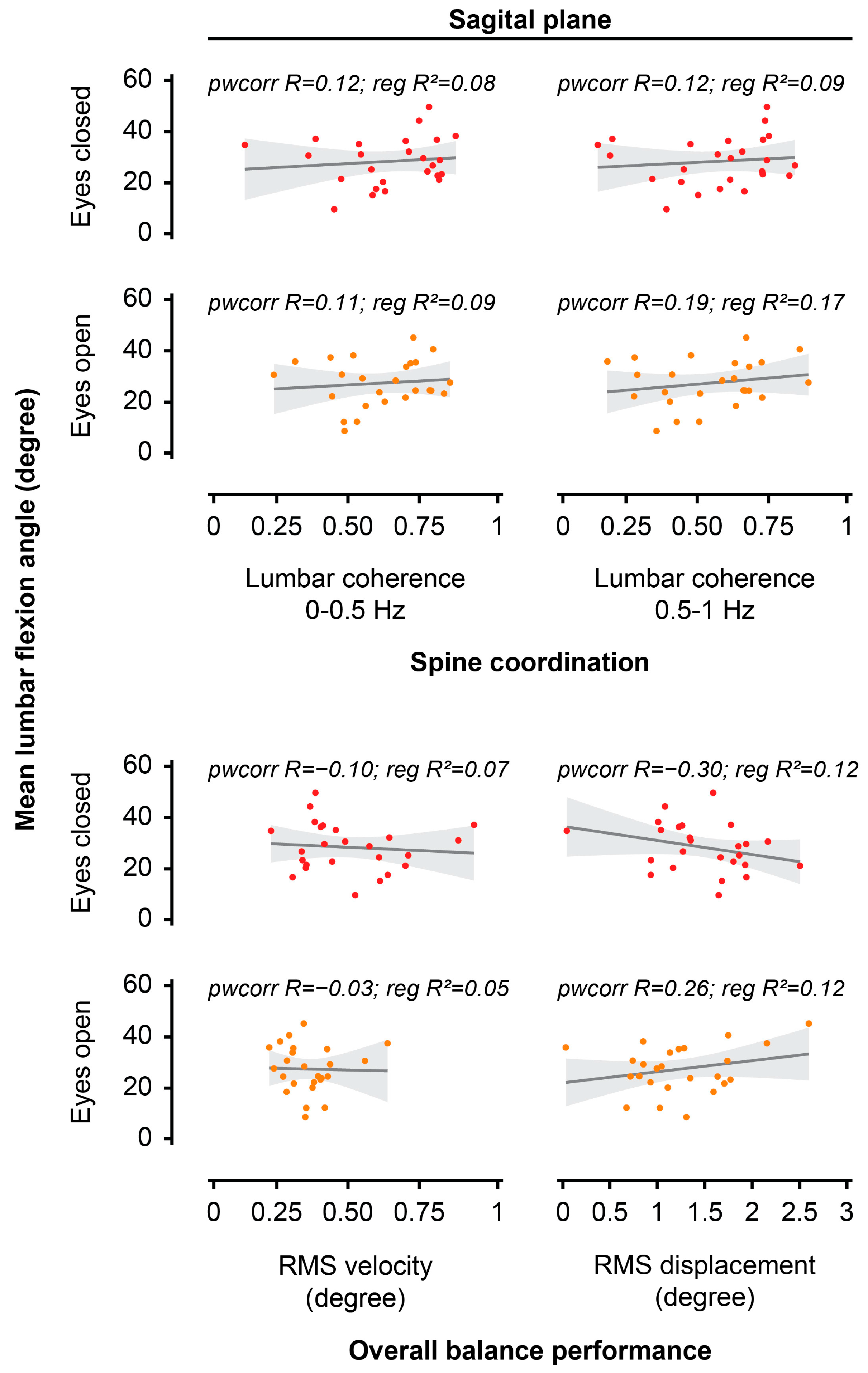
3.4. Relationship Between Spine Posture and Performance During Unstable Sitting
4. Discussion
4.1. Relationship Between Laboratory and Real-World Sitting Postures
4.2. Relationship Between Performance During Unstable Sitting in the Laboratory and Real-World Sedentary/Activity Behaviours
4.3. Relationship Between Spine Posture and Performance During Unstable Sitting
4.4. Methodological Considerations
4.5. Clinical Implications
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| LBP | Low back pain |
| BMI | Body mass index |
| L5/S1 | Lumbosacral junction |
| T12/L1 | Thoracolumbar junction |
| EO | Eyes open |
| EC | Eyes closed |
| GMMs | Gaussian Mixture Models |
| RMS | Root mean square |
| pwcorr | Pairwise correlation |
| R2 | Determination coefficient |
References
- Owen, N.; Healy, G.N.; Matthews, C.E.; Dunstan, D.W. Too much sitting: The population health science of sedentary behavior. Exerc. Sport Sci. Rev. 2010, 38, 105–113. [Google Scholar] [CrossRef]
- Mörl, F.; Bradl, I. Lumbar posture and muscular activity while sitting during office work. J. Electromyogr. Kinesiol. 2013, 23, 362–368. [Google Scholar] [CrossRef]
- Soares, C.; Shimano, S.G.N.; Marcacine, P.R.; Fernandes, L.F.R.M.; de Castro, L.L.P.T.; de Walsh, I.A.P. Ergonomic interventions for work in a sitting position: An integrative review. Rev. Bras. Med. Trab. 2023, 21, e20230059. [Google Scholar] [CrossRef]
- Kim, S.; Lee, I.; Kang, S.H.; Jin, S. Significance of lower body postures in chair design. Hum. Factors 2023, 65, 575–591. [Google Scholar] [CrossRef]
- Alshehri, M.A.; Alzahrani, H.; van den Hoorn, W.; Klyne, D.M.; Vette, A.H.; Hendershot, B.D.; Roberts, B.W.; Larivière, C.; Barbado, D.; Vera-Garcia, F.J.; et al. Trunk postural control during unstable sitting among individuals with and without low back pain: A systematic review with an individual participant data meta-analysis. PLoS ONE 2024, 19, e0296968. [Google Scholar] [CrossRef]
- Claeys, K.; Brumagne, S.; Deklerck, J.; Vanderhaeghen, J.; Dankaerts, W. Sagittal evaluation of usual standing and sitting spinal posture. J. Bodyw. Mov. Ther. 2016, 20, 326–333. [Google Scholar] [CrossRef]
- Kwon, Y.; Kim, J.W.; Heo, J.H.; Jeon, H.M.; Choi, E.B.; Eom, G.M. The effect of sitting posture on the loads at cervico-thoracic and lumbosacral joints. Technol. Health Care 2018, 26, 409–418. [Google Scholar] [CrossRef] [PubMed]
- In, T.S.; Jung, J.H.; Jung, K.S.; Cho, H.Y. Spinal and pelvic alignment of sitting posture associated with smartphone use in adolescents with low back pain. Int. J. Environ. Res. Public Health 2021, 18, 8369. [Google Scholar] [CrossRef] [PubMed]
- Dankaerts, W.; O’Sullivan, P.; Burnett, A.; Straker, L. Differences in sitting postures are associated with nonspecific chronic low back pain disorders when patients are subclassified. Spine 2006, 31, 698–704. [Google Scholar] [CrossRef] [PubMed]
- Misir, A.; Kizkapan, T.B.; Tas, S.K.; Yildiz, K.I.; Ozcamdalli, M.; Yetis, M. Lumbar spine posture and spinopelvic parameters change in various standing and sitting postures. Eur. Spine J. 2019, 28, 1072–1081. [Google Scholar] [CrossRef]
- Alshehri, M.A.; van den Hoorn, W.; Klyne, D.M.; Hodges, P.W. Coordination of hip and spine in individuals with acute low back pain during unstable sitting. Spine J. 2024, 24, 768–782. [Google Scholar] [CrossRef] [PubMed]
- Alshehri, M.A.; van den Hoorn, W.; Klyne, D.M.; van Dieën, J.H.; Cholewicki, J.; Hodges, P.W. Poor lumbar spine coordination in acute low back pain predicts persistent long-term pain and disability. Eur. Spine J. 2024, 33, 1234–1245. [Google Scholar] [CrossRef] [PubMed]
- Hodges, P.W.; Danneels, L. Changes in structure and function of the back muscles in low back pain: Different time points, observations, and mechanisms. J. Orthop. Sports Phys. Ther. 2019, 49, 464–476. [Google Scholar] [CrossRef]
- Cholewicki, J.; Silfies, S.P.; Shah, R.A.; Greene, H.S.; Reeves, N.P.; Alvi, K.; Goldberg, B. Delayed trunk muscle reflex responses increase the risk of low back injuries. Spine 2005, 30, 2614–2620. [Google Scholar] [CrossRef]
- Coenen, P.; Kingma, I.; Boot, C.R.; Twisk, J.W.; Bongers, P.M.; van Dieën, J.H. Cumulative low back load at work as a risk factor of low back pain: A prospective cohort study. J. Occup. Rehabil. 2013, 23, 11–18. [Google Scholar] [CrossRef]
- Hodges, P.W.; van den Hoorn, W. A vision for the future of wearable sensors in spine care and its challenges: Narrative review. J. Spine Surg. 2022, 8, 103–113. [Google Scholar] [CrossRef]
- Claus, A.P.; Hides, J.A.; Moseley, G.L.; Hodges, P.W. Thoracic and lumbar posture behaviour in sitting tasks and standing: Progressing the biomechanics from observations to measurements. Appl. Ergon. 2016, 53, 161–168. [Google Scholar] [CrossRef]
- Kuo, Y.L.; Huang, K.Y.; Kao, C.Y.; Tsai, Y.J. Sitting posture during prolonged computer typing with and without a wearable biofeedback sensor. Int. J. Environ. Res. Public Health 2021, 18, 5430. [Google Scholar] [CrossRef] [PubMed]
- Cholewicki, J.; Polzhofer, G.; Radebold, A. Postural control of trunk during unstable sitting. J. Biomech. 2000, 33, 1733–1737. [Google Scholar] [CrossRef]
- Alshehri, M.A.; van den Hoorn, W.; Klyne, D.; Hodges, P.W. Coordination of hip and spine to maintain equilibrium in unstable sitting revealed by spectral analysis. J. Neurophysiol. 2021, 126, 1458–1469. [Google Scholar] [CrossRef]
- Roberts, B.W.; Gholibeigian, F.; Lewicke, J.; Vette, A.H. Spatial and temporal relation of kinematics and muscle activity during unstable sitting. J. Electromyogr. Kinesiol. 2020, 52, 102418. [Google Scholar] [CrossRef]
- Simpson, L.; Maharaj, M.M.; Mobbs, R.J. The role of wearables in spinal posture analysis: A systematic review. BMC Musculoskelet. Disord. 2019, 20, 55. [Google Scholar] [CrossRef]
- Papi, E.; Koh, W.S.; McGregor, A.H. Wearable technology for spine movement assessment: A systematic review. J. Biomech. 2017, 64, 186–197. [Google Scholar] [CrossRef] [PubMed]
- Larivière, C.; Mecheri, H.; Shahvarpour, A.; Gagnon, D.; Shirazi-Adl, A. Criterion validity and between-day reliability of an inertial-sensor-based trunk postural stability test during unstable sitting. J. Electromyogr. Kinesiol. 2013, 23, 899–907. [Google Scholar] [CrossRef] [PubMed]
- Mjøsund, H.L.; Boyle, E.; Kjaer, P.; Mieritz, R.M.; Skallgård, T.; Kent, P. Clinically acceptable agreement between the ViMove wireless motion sensor system and the Vicon motion capture system when measuring lumbar region inclination motion in the sagittal and coronal planes. BMC Musculoskelet. Disord. 2017, 18, 124. [Google Scholar] [CrossRef] [PubMed]
- Khurelbaatar, T.; Kim, K.; Lee, S.; Kim, Y.H. Consistent accuracy in whole-body joint kinetics during gait using wearable inertial motion sensors and in-shoe pressure sensors. Gait Posture 2015, 42, 65–69. [Google Scholar] [CrossRef] [PubMed]
- Kos, A.; Tomažič, S.; Umek, A. Evaluation of smartphone inertial sensor performance for cross-platform mobile applications. Sensors 2016, 16, 477. [Google Scholar] [CrossRef] [PubMed]
- Riddick, R.; Smits, E.; Faber, G.; Shearwin, C.; Hodges, P.; van den Hoorn, W. Estimation of human spine orientation with inertial measurement units (IMU) at low sampling rate: How low can we go? J. Biomech. 2023, 157, 111726. [Google Scholar] [CrossRef]
- Cotter, B.D.; Nairn, B.C.; Drake, J.D. Should a standing or seated reference posture be used when normalizing seated spine kinematics? J. Biomech. 2014, 47, 2371–2377. [Google Scholar] [CrossRef]
- Jacobs, J.V.; Dimitrova, D.M.; Nutt, J.G.; Horak, F.B. Can stooped posture explain multidirectional postural instability in patients with Parkinson’s disease? Exp. Brain Res. 2005, 166, 78–88. [Google Scholar] [CrossRef]
- Beauchet, O.; Annweiler, C.; Lecordroch, Y.; Allali, G.; Dubost, V.; Herrmann, F.R.; Kressig, R.W. Walking speed-related changes in stride time variability: Effects of decreased speed. J. Neuroeng. Rehabil. 2009, 6, 32. [Google Scholar] [CrossRef] [PubMed]
- Zhu, W.; Li, Y.; Wang, B.; Zhao, C.; Wu, T.; Liu, T.; Sun, F. Objectively measured physical activity is associated with static balance in young adults. Int. J. Environ. Res. Public Health 2021, 18, 10787. [Google Scholar] [CrossRef]
- Alsufiany, M.B.; Lohman, E.B.; Daher, N.S.; Gang, G.R.; Shallan, A.I.; Jaber, H.M. Non-specific chronic low back pain and physical activity: A comparison of postural control and hip muscle isometric strength: A cross-sectional study. Medicine 2020, 99, e18892. [Google Scholar] [CrossRef]
- Maitre, J.; Paillard, T. Postural effects of vestibular manipulation depend on the physical activity status. PLoS ONE 2016, 11, e0162966. [Google Scholar] [CrossRef]
- Onofrei, R.R.; Amaricai, E. Postural balance in relation with vision and physical activity in healthy young adults. Int. J. Environ. Res. Public Health 2022, 19, 5021. [Google Scholar] [CrossRef] [PubMed]
- Cooper, R.; Stamatakis, E.; Hamer, M. Associations of sitting and physical activity with grip strength and balance in mid-life: 1970 British Cohort Study. Scand. J. Med. Sci. Sports 2020, 30, 2371–2381. [Google Scholar] [CrossRef] [PubMed]
- Glofcheskie, G.O.; Brown, S.H.M. Athletic background is related to superior trunk proprioceptive ability, postural control, and neuromuscular responses to sudden perturbations. Hum. Mov. Sci. 2017, 52, 74–83. [Google Scholar] [CrossRef] [PubMed]
- Kim, S.S.; Lim, K.; Choi, W.J. Effect on the center of pressure of vision, floor condition, and the height of center of mass during quiet standing. Phys. Ther. Korea 2021, 28, 154–160. [Google Scholar] [CrossRef]
- Ligorio, G.; Sabatini, A.M. Dealing with magnetic disturbances in human motion capture: A survey of techniques. Micromachines 2016, 7, 43. [Google Scholar] [CrossRef]
| Outcome | Pairwise Correlation | Linear Regression Analysis | ||||
|---|---|---|---|---|---|---|
| Coef. a | 95% CI | p-Value | Coef. b | 95% CI | p-Value | |
| Real world: overall posture | ||||||
| Laboratory: | ||||||
| Upright sitting | 0.37 | −0.03, 0.67 | 0.067 | 0.25 | −0.03, 0.54 | 0.074 |
| Questionnaire sitting | 0.23 | −0.18, 0.57 | 0.267 | 0.18 | −0.08, 0.43 | 0.167 |
| EO unstable sitting | 0.51 | 0.14, 0.75 | 0.009 | 0.41 | 0.12, 0.70 | 0.008 |
| EC unstable sitting | 0.46 | 0.09, 0.73 | 0.019 | 0.36 | 0.07, 0.66 | 0.018 |
| Real world: 1st most frequent posture | ||||||
| Laboratory: | ||||||
| Upright sitting | 0.24 | −0.17, 0.58 | 0.251 | 0.20 | −0.14, 0.54 | 0.232 |
| Questionnaire sitting | 0.14 | −0.27, 0.51 | 0.492 | 0.20 | −0.10, 0.49 | 0.177 |
| EO unstable sitting | 0.37 | −0.04, 0.67 | 0.073 | 0.37 | 0.01, 0.73 | 0.043 |
| EC unstable sitting | 0.31 | −0.10, 0.63 | 0.132 | 0.32 | −0.04, 0.68 | 0.078 |
| Real world: 2nd most frequent posture | ||||||
| Laboratory: | ||||||
| Upright sitting | 0.51 | 0.14, 0.75 | 0.010 | 0.52 | 0.13, 0.90 | 0.011 |
| Questionnaire sitting | 0.04 | −0.37, 0.42 | 0.867 | 0.07 | −0.32, 0.46 | 0.696 |
| EO unstable sitting | 0.36 | −0.04, 0.66 | 0.073 | 0.45 | −0.02, 0.92 | 0.060 |
| EC unstable sitting | 0.34 | −0.06, 0.65 | 0.096 | 0.40 | −0.06, 0.86 | 0.084 |
| Real world: nearest posture | ||||||
| Laboratory: | ||||||
| Upright sitting | 0.87 | 0.73, 0.94 | <0.001 | 0.80 | 0.60, 1.00 | <0.001 |
| Questionnaire sitting | 0.72 | 0.46, 0.87 | <0.001 | 0.41 | 0.20, 0.62 | 0.001 |
| EO unstable sitting | 0.91 | 0.80, 0.96 | <0.001 | 0.96 | 0.76, 1.17 | <0.001 |
| EC unstable sitting | 0.85 | 0.68, 0.93 | <0.001 | 0.68 | 0.48, 0.88 | <0.001 |
| Outcome | Pairwise Correlation | Linear Regression Analysis | ||||
|---|---|---|---|---|---|---|
| Coef. a | 95% CI | p-Value | Coef. b | 95% CI | p-Value | |
| Real-world time spent during sitting | ||||||
| Laboratory—overall balance performance: | ||||||
| Sagittal RMS velocity—EO | 0.16 | −0.25, 0.52 | 0.447 | 0.02 | −0.37, 0.41 | 0.904 |
| Sagittal RMS velocity—EC | 0.40 | 0.00, 0.68 | 0.049 | 0.14 | −0.06, 0.33 | 0.164 |
| Sagittal RMS displacement—EO | −0.23 | −0.58, 0.18 | 0.261 | −0.04 | −0.10, 0.03 | 0.238 |
| Sagittal RMS displacement—EC | 0.19 | −0.22, 0.55 | 0.353 | 0.02 | −0.05, 0.09 | 0.566 |
| Frontal RMS velocity—EO | 0.26 | −0.15, 0.60 | 0.208 | 0.01 | −0.08, 0.10 | 0.818 |
| Frontal RMS velocity—EC | 0.35 | −0.06, 0.65 | 0.089 | 0.03 | −0.03, 0.08 | 0.349 |
| Frontal RMS displacement—EO | −0.05 | −0.44, 0.35 | 0.813 | −0.05 | −0.18, 0.07 | 0.368 |
| Frontal RMS displacement—EC | 0.45 | 0.06, 0.72 | 0.025 | 0.07 | −0.03, 0.16 | 0.148 |
| Laboratory—spine coordination: | ||||||
| Sagittal lumbar coherence (0–0.5 Hz)—EO | −0.28 | −0.61, 0.13 | 0.173 | −0.12 | −0.36, 0.11 | 0.274 |
| Sagittal lumbar coherence (0–0.5 Hz)—EC | −0.18 | −0.54, 0.23 | 0.384 | −0.05 | −0.25, 0.14 | 0.568 |
| Sagittal lumbar coherence (0.5–1 Hz)—EO | −0.15 | −0.52, 0.26 | 0.463 | −0.05 | −0.26, 0.17 | 0.650 |
| Sagittal lumbar coherence (0.5–1 Hz)—EC | −0.13 | −0.50, 0.28 | 0.525 | −0.02 | −0.21, 0.17 | 0.843 |
| Frontal lumbar coherence (0–0.5 Hz)—EO | 0.19 | −0.22, 0.55 | 0.353 | 0.09 | −0.15, 0.33 | 0.458 |
| Frontal lumbar coherence (0–0.5 Hz)—EC | 0.33 | −0.07, 0.64 | 0.106 | 0.10 | −0.10, 0.30 | 0.300 |
| Frontal lumbar coherence (0.5–1 Hz)—EO | 0.32 | −0.08, 0.64 | 0.117 | 0.10 | −0.06, 0.25 | 0.222 |
| Frontal lumbar coherence (0.5–1 Hz)—EC | 0.33 | −0.08, 0.64 | 0.112 | 0.10 | −0.07, 0.27 | 0.232 |
| Real-world time spent during walking | ||||||
| Laboratory—overall balance performance: | ||||||
| Sagittal RMS velocity—EO | −0.07 | −0.45, 0.33 | 0.733 | −0.00 | −0.16, 0.16 | 0.977 |
| Sagittal RMS velocity—EC | −0.19 | −0.54, 0.22 | 0.364 | −0.03 | −0.11, 0.06 | 0.492 |
| Sagittal RMS displacement—EO | −0.01 | −0.40, 0.39 | 0.980 | −0.00 | −0.03, 0.02 | 0.821 |
| Sagittal RMS displacement—EC | −0.10 | −0.48, 0.31 | 0.628 | −0.01 | −0.04, 0.02 | 0.468 |
| Frontal RMS velocity—EO | −0.07 | −0.45, 0.34 | 0.754 | −0.00 | −0.04, 0.04 | 0.966 |
| Frontal RMS velocity—EC | −0.22 | −0.57, 0.19 | 0.291 | −0.01 | −0.03, 0.01 | 0.451 |
| Frontal RMS displacement—EO | 0.06 | −0.34, 0.45 | 0.762 | 0.01 | −0.04, 0.06 | 0.676 |
| Frontal RMS displacement—EC | −0.12 | −0.49, 0.29 | 0.564 | −0.01 | −0.05, 0.03 | 0.567 |
| Laboratory—spine coordination: | ||||||
| Sagittal lumbar coherence (0–0.5 Hz)—EO | 0.41 | 0.02, 0.69 | 0.042 | 0.07 | −0.02, 0.17 | 0.119 |
| Sagittal lumbar coherence (0–0.5 Hz)—EC | 0.28 | −0.13, 0.61 | 0.174 | 0.04 | −0.04, 0.12 | 0.301 |
| Sagittal lumbar coherence (0.5–1 Hz)—EO | 0.39 | −0.01, 0.68 | 0.056 | 0.06 | −0.03, 0.14 | 0.168 |
| Sagittal lumbar coherence (0.5–1 Hz)—EC | 0.30 | −0.11, 0.62 | 0.151 | 0.04 | −0.04, 0.11 | 0.325 |
| Frontal lumbar coherence (0–0.5 Hz)—EO | 0.11 | −0.30, 0.48 | 0.608 | 0.03 | −0.07, 0.13 | 0.578 |
| Frontal lumbar coherence (0–0.5 Hz)—EC | −0.01 | −0.40, 0.39 | 0.979 | 0.00 | −0.08, 0.08 | 0.998 |
| Frontal lumbar coherence (0.5–1 Hz)—EO | 0.02 | −0.38, 0.41 | 0.939 | 0.00 | −0.07, 0.07 | 0.963 |
| Frontal lumbar coherence (0.5–1 Hz)—EC | 0.09 | −0.32, 0.47 | 0.666 | 0.01 | −0.06, 0.09 | 0.712 |
| Outcome | Pairwise Correlation | Linear Regression Analysis | ||||
|---|---|---|---|---|---|---|
| Coef. a | 95% CI | p-Value | Coef. b | 95% CI | p-Value | |
| Mean lumbar flexion angle | ||||||
| Overall balance performance: | ||||||
| RMS velocity—EO | −0.03 | −0.42, 0.37 | 0.898 | −10.73 | −57.11, 35.65 | 0.635 |
| RMS velocity—EC | −0.10 | −0.48, 0.31 | 0.640 | −9.00 | −33.87, 15.88 | 0.460 |
| RMS displacement—EO | 0.26 | −0.16, 0.59 | 0.218 | 4.89 | −2.42, 12.19 | 0.179 |
| RMS displacement—EC | −0.30 | −0.62, 0.11 | 0.149 | −5.50 | −13.78, 2.78 | 0.182 |
| Spine coordination: | ||||||
| Lumbar coherence (0–0.5 Hz)—EO | 0.11 | −0.30, 0.48 | 0.603 | 15.02 | −12.64, 42.68 | 0.272 |
| Lumbar coherence (0–0.5 Hz)—EC | 0.12 | −0.29, 0.49 | 0.579 | 9.92 | −13.67, 33.51 | 0.392 |
| Lumbar coherence (0.5–1 Hz)—EO | 0.19 | −0.22, 0.55 | 0.351 | 20.55 | −3.45, 44.55 | 0.089 |
| Lumbar coherence (0.5–1 Hz)—EC | 0.12 | −0.29, 0.49 | 0.577 | 11.97 | −10.93, 34.86 | 0.289 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Alshehri, M.A.; Riddick, R.; Besomi, M.; van den Hoorn, W.; Klyne, D.M.; Hodges, P.W. Exploring Lumbar Spine Posture and Movement in Sitting: A Comparison Between Laboratory and Real-World Measures. J. Clin. Med. 2025, 14, 7518. https://doi.org/10.3390/jcm14217518
Alshehri MA, Riddick R, Besomi M, van den Hoorn W, Klyne DM, Hodges PW. Exploring Lumbar Spine Posture and Movement in Sitting: A Comparison Between Laboratory and Real-World Measures. Journal of Clinical Medicine. 2025; 14(21):7518. https://doi.org/10.3390/jcm14217518
Chicago/Turabian StyleAlshehri, Mansour Abdullah, Ryan Riddick, Manuela Besomi, Wolbert van den Hoorn, David M. Klyne, and Paul W. Hodges. 2025. "Exploring Lumbar Spine Posture and Movement in Sitting: A Comparison Between Laboratory and Real-World Measures" Journal of Clinical Medicine 14, no. 21: 7518. https://doi.org/10.3390/jcm14217518
APA StyleAlshehri, M. A., Riddick, R., Besomi, M., van den Hoorn, W., Klyne, D. M., & Hodges, P. W. (2025). Exploring Lumbar Spine Posture and Movement in Sitting: A Comparison Between Laboratory and Real-World Measures. Journal of Clinical Medicine, 14(21), 7518. https://doi.org/10.3390/jcm14217518







