Should Chronic Subretinal Hemorrhage Be Treated Surgically?
Abstract
1. Introduction
2. Case Presentation
2.1. Functioning Prior to Treatment
- Difficulty with depth perception and spatial orientation,
- Impairments in tasks requiring precise binocular coordination (e.g., manual work, cycling),
- Recurrent headaches related to overuse of the left eye,
- Inability to continue his previous profession, which required good stereoscopic vision (he had previously worked as an assembler).
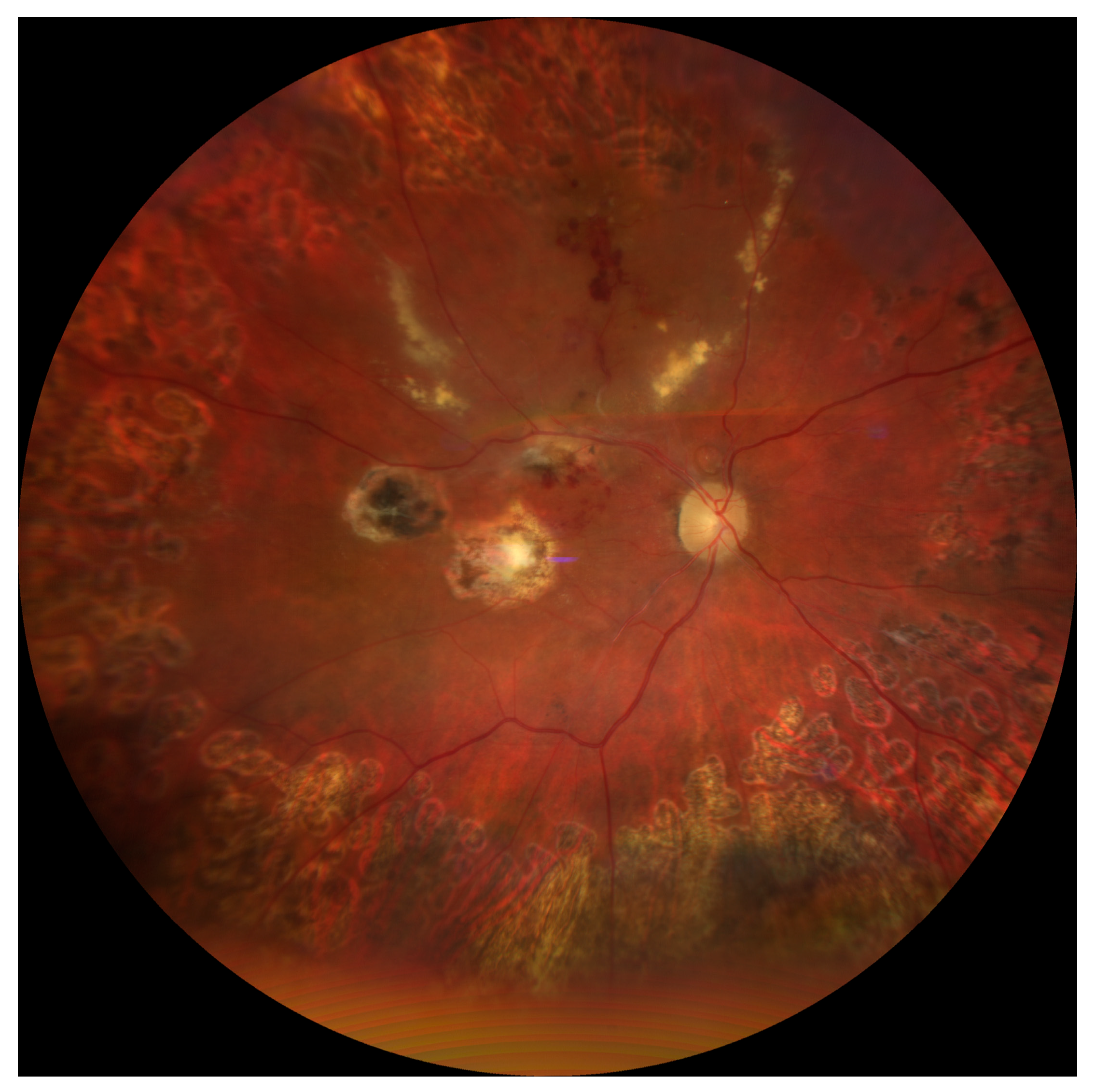
2.2. Baseline Examination
- Anterior segment—inferior corneal scar, partial post-traumatic sectoral cataract,
- Vitreous—presence of dense, chronic hemorrhagic remnants,
- Retina—multiple intraretinal hemorrhages, signs of post-traumatic retinopathy.
Imaging Studies
- Optical coherence tomography (OCT): thinning of the outer retinal layers in the macula, presence of submacular blood remnants, disrupted photoreceptor architecture, and discontinuity of the IS/OS junction; vitreomacular tractional changes within the inner retinal layers.
- B-scan ultrasonography: dense echogenic material corresponding to vitreous hemorrhage, irregular and undulating retinal attachment in the posterior pole suggestive of tractional component.
- Fluorescein angiography (FA): leakage from perifoveal vessels, areas of hypofluorescence corresponding to blood clots, and hyperfluorescent foci consistent with scarring.
2.3. Therapeutic Decision
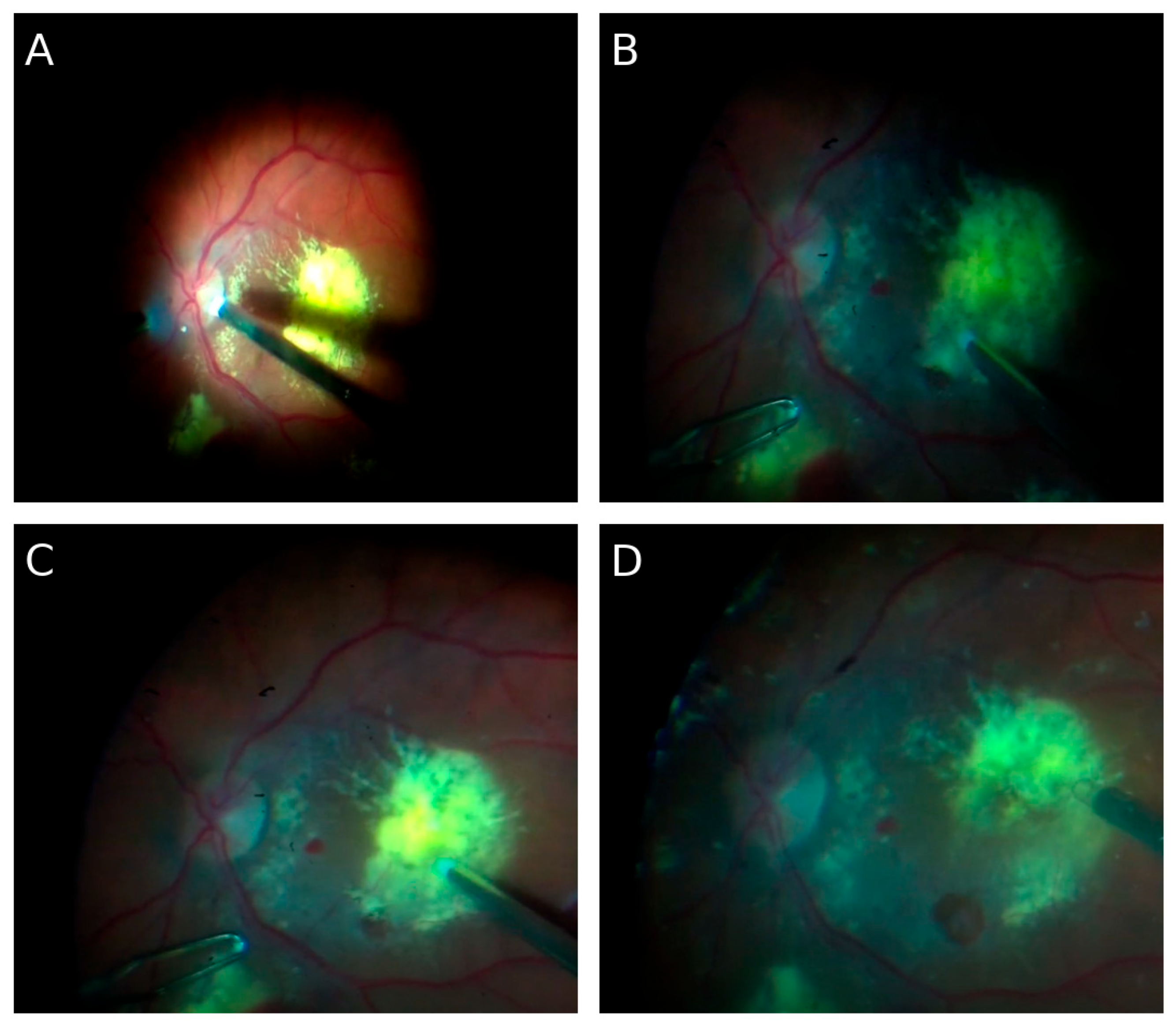
2.3.1. Surgical Interventions
- Postoperative course: Two weeks postoperatively, partial improvement in visual axis clarity was achieved, although functional acuity remained low (object recognition, but no reading improvement). OCT showed partial clearance of the submacular space and limited re-approximation of photoreceptor architecture.
- Postoperative course: The retina remained fully attached postoperatively. OCT confirmed reattachment and partial restoration of inner retinal layers. Visual acuity was 1.6 logMAR.
- Postoperative course: The retina remained permanently attached. OCT showed no new hemorrhages or vitreoretinal tractions. Visual acuity gradually improved in the following weeks.
2.3.2. Perioperative and Pharmacological Management
2.4. Final Outcome and Long-Term Follow-Up
- Right eye visual acuity—0.3 Snellen (0.52 logMAR),
- OCT—complete macular reattachment, thinning of photoreceptor layers, no active hemorrhage,
- B-scan—no traction, no retinal detachment,
- FA—no active leakage.
Final Effect
2.5. Case Summary
3. Discussion
3.1. Pathophysiology of Subretinal and Vitreous Hemorrhage
- Mechanical effects: blood mass displaces and detaches the retina, exerting pressure on the outer photoreceptor segments and impairing their metabolic function.
- Inflammatory effects: the presence of blood in the subretinal space induces microglial activation and macrophage migration, contributing to fibrosis and proliferative vitreoretinopathy (PVR) [19].
3.2. The Role of Exposure Time
- Biochemical transformation of blood remnants—in the subretinal space, which lacks an active phagocytic system, hemoglobin breakdown products may gradually transform into less reactive forms (e.g., hemosiderin, ferritin) [25]. In the present case, after more than a decade, primary hemoglobin toxicity may have subsided, leaving less harmful deposits.
- Patient-related factors—at the time of trauma, the patient was approximately 40 years old (relatively young), which may have supported partial functional reserve and neuronal plasticity, enhancing the potential for retinal reorganization [26].
- Absence of systemic comorbidities (e.g., diabetes, hypertension) limited additional damaging influences and may have preserved regenerative capacity [27].
3.3. Comparison with the Literature
- Chen et al. [10] described massive subretinal hemorrhages where early PPV combined with tPA led to recovery of visual acuity up to 0.4 Snellen; however, interventions were performed within days to weeks, not years.
- Boral et al. [22] presented cases of retinal hemorrhage treated surgically using various techniques, showing that earlier intervention yielded superior functional outcomes compared to delayed management.
- Wu et al. [9] demonstrated that early surgical intervention in closed-globe injuries with massive vitreous hemorrhage reduces the risk of PVR and improves retinal survival.
- Lema and Lin [12] identified surgical timing as a key prognostic factor in open-globe injuries with retinal detachment.
3.4. Surgical Strategies and Choice of Tamponade
- Pars plana vitrectomy (PPV): removal of hemorrhagic remnants,
- ILM peeling: reducing traction and promoting retinal integration,
- Endolaser photocoagulation: securing retinal tears and degenerative foci,
- Gas tamponade (SF6, C3F8): applied in localized cases, providing temporary retinal apposition,
3.5. Visual Rehabilitation
- Central and eccentric fixation training,
- Accommodative exercises,
- Adaptation for reading and use of optical aids.
3.6. Clinical and Research Implications
- Should surgical eligibility criteria be more liberal? Traditionally, patients with long-standing hemorrhage were disqualified. This case suggests reconsideration, even after years.
- Which mechanisms underlie preservation of partial retinal functional reserve? Histopathological and experimental studies are needed to clarify the effects of chronic intraocular blood.
- Which tamponade is optimal in chronic cases? The lack of consensus highlights the need for prospective studies.
- Can visual rehabilitation protocols be developed for patients with late visual recovery?
3.7. Discussion Summary
3.8. Limitations
4. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| FA | Fluorescein angiography |
| ILM | Internal limiting membrane |
| IOP | Intraocular pressure |
| OCT | Optical coherence tomography |
| PPV | Pars plana vitrectomy |
| PVR | Proliferative vitreoretinopathy |
| RPE | Retinal pigment epithelium |
| ROS | Reactive oxygen species |
| SF6 | Sulfur hexafluoride (gas tamponade) |
References
- Waters, T.; Vollmer, L.; Sowka, J. Proliferative vitreoretinopathy as a late complication of blunt ocular trauma. Optometry 2008, 79, 197–202. [Google Scholar] [CrossRef] [PubMed]
- Busquets, M.A.; Kim, A.; Busquets, T. Bilateral Giant Retinal Tears Associated with Obsessive-Compulsive Disorder. Ophthalmol. Retin. 2023, 7, 1096. [Google Scholar] [CrossRef] [PubMed]
- Bian, X.; Xu, S.; Song, Y.; Wang, Y.; Zhao, B.; Zhong, Y.; Liu, L.; Hu, Y. Global, national and regional prevalence, and associated factors of ocular trauma: A protocol for systematic review and meta-analysis. Medicine 2020, 99, e21870. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Dogramaci, M.; Erdur, S.K.; Senturk, F. Standardized Classification of Mechanical Ocular Injuries: Efficacy and Shortfalls. Beyoglu Eye J. 2021, 6, 236–242. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Gadde, S.G.K.; Snehith, R.; Jayadev, C.; Poornachandra, B.; Naik, N.K.; Yadav, N.K. Macular tractional retinal detachment: A rare complication of blunt trauma. Indian J. Ophthalmol. 2020, 68, 2602–2604. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Lin, Y.C.; Wang, C.T.; Chen, K.J.; Chou, H.D. Traumatic terson syndrome with a peculiar mass lesion and tractional retinal detachment: A case report. BMC Ophthalmol. 2024, 24, 153. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Wang, Z.G.; Li, P.; Yang, X.M.; Wang, Z.Q.; Zhang, P.R. High BMI, silicone oil tamponade, and recurrent vitreous hemorrhage predict poor visual outcomes after pars plana vitrectomy in proliferative diabetic retinopathy. BMC Ophthalmol. 2025, 25, 148. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Agrawal, R.; Shah, M.; Mireskandari, K. Controversies in ocular trauma classification and management. Int. Ophthalmol. 2013, 33, 49–57. [Google Scholar] [CrossRef]
- Yeung, L.; Chen, T.L.; Kuo, Y.H.; Chao, A.N.; Wu, W.C.; Chen, K.J.; Hwang, Y.S.; Chen, Y.; Lai, C.C. Severe vitreous hemorrhage associated with closed-globe injury. Graefes Arch. Clin. Exp. Ophthalmol. 2006, 244, 52–57. [Google Scholar] [CrossRef] [PubMed]
- Chen, K.J.; Sun, M.H.; Sun, C.C.; Wang, N.K.; Hou, C.H.; Wu, A.L.; Wu, W.C.; Lai, C.C. Traumatic Maculopathy with Massive Subretinal Hemorrhage after Closed-Globe Injuries: Associated Findings, Management, and Visual Outcomes. Ophthalmol. Retin. 2019, 3, 53–60. [Google Scholar] [CrossRef] [PubMed]
- Quiroz-Reyes, M.A.; Quiroz-Gonzalez, E.A.; Quiroz-Gonzalez, M.A.; Lima-Gómez, V. Early versus Delayed Vitrectomy for Open Globe Injuries: A Systematic Review and Meta-Analysis. Clin. Ophthalmol. 2024, 18, 1889–1900. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Lema, G.M.C.; Lin, H.; Yoganathan, P. Prognostic indicators of visual acuity after open-globe injury and retinal detachment repair. Retina 2016, 36, 687–694. [Google Scholar] [CrossRef]
- Ulianova, N.; Sidak-Petretska, O.; Bondar, N. Outcomes of vitrectomy for chorioretinitis sclopetaria following blast-related ocular trauma. Int. J. Retin. Vitr. 2025, 11, 49. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Jabłoński, M.; Winiarczyk, M.; Biela, K.; Bieliński, P.; Jasielska, M.; Batalia, J.; Mackiewicz, J. Open Globe Injury (OGI) with a Presence of an Intraocular Foreign Body (IOFB)-Epidemiology, Management, and Risk Factors in Long Term Follow-Up. J. Clin. Med. 2022, 12, 190. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Lee, S.; Kim, J. Rhegmatogenous Retinal Detachment with Giant Retinal Tear: Case Series and Literature Review. J. Clin. Med. 2024, 13, 4690. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Glatt, H.; Machemer, R. Experimental subretinal hemorrhage in rabbits. Am. J. Ophthalmol. 1982, 94, 762–773. [Google Scholar] [CrossRef]
- Hope, G.M.; Dawson, W.W.; Engel, H.M. Subretinal blood induces retinal degeneration in cats. Investig. Ophthalmol. Vis. Sci. 1992, 33, 2894–2901. [Google Scholar]
- Toth, C.A.; Morse, L.S.; Hjelmeland, L.M.; Landers, M.B., 3rd. Fibrin directs early retinal damage after experimental subretinal hemorrhage. Arch. Ophthalmol. 1991, 109, 723–729. [Google Scholar] [CrossRef] [PubMed]
- Znaor, L.; Medic, A.; Binder, S.; Vucinovic, A.; Marin Lovric, J.; Puljak, L. Pars plana vitrectomy versus scleral buckling for repairing simple rhegmatogenous retinal detachments. Cochrane Database Syst. Rev. 2019, 3, CD009562. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Arroyo, J.G.; Yang, L.; Bula, D.; Chen, D.F. Photoreceptor apoptosis in human retinal detachment. Am. J. Ophthalmol. 2005, 139, 605–610. [Google Scholar] [CrossRef] [PubMed]
- Almeida, D.R.P.; Khan, M.S.; Engelbert, M.; Kapusta, M.A.; Chow, D.R. Timing of surgery for traumatic macular holes and associated retinal detachment: Visual outcomes. Retina 2017, 37, 1071–1077. [Google Scholar] [CrossRef]
- Boral, S.K.; Agarwal, D.; Das, A.; Chakraborty, D.; Mandal, S. Real-world outcomes and complications of different surgical approaches for significant submacular haemorrhages. Indian J. Ophthalmol. 2023, 71, 2045–2052. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Smith, J.M.; Steel, D.H. Anti-vascular endothelial growth factor for prevention of postoperative vitreous cavity haemorrhage after vitrectomy for proliferative diabetic retinopathy. Cochrane Database Syst. Rev. 2015, 2015, CD008214, Update in Cochrane Database Syst. Rev. 2023, 5, CD008214. https://doi.org/10.1002/14651858.CD008214.pub4. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Shaikh, N.; Srishti, R.; Khanum, A.; Thirumalesh, M.B.; Dave, V.; Arora, A.; Bansal, R.; Surve, A.; Azad, S.; Kumar, V. Vitreous hemorrhage—Causes, diagnosis, and management. Indian J. Ophthalmol. 2023, 71, 28–38. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Picard, E.; Daruich, A.; Youale, J.; Courtois, Y.; Behar-Cohen, F. From Rust to Quantum Biology: The Role of Iron in Retina Physiopathology. Cells 2020, 9, 705. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Di Fazio, N.; Delogu, G.; Morena, D.; Cipolloni, L.; Scopetti, M.; Mazzilli, S.; Frati, P.; Fineschi, V. New Insights into the Diagnosis and Age Determination of Retinal Hemorrhages from Abusive Head Trauma: A Systematic Review. Diagnostics 2023, 13, 1722. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Colcombe, J.; Mundae, R.; Kaiser, A.; Bijon, J.; Modi, Y. Retinal Findings and Cardiovascular Risk: Prognostic Conditions, Novel Biomarkers, and Emerging Image Analysis Techniques. J. Pers. Med. 2023, 13, 1564. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Mayer, C.S.; Reznicek, L.; Baur, I.D.; Khoramnia, R. Open Globe Injuries: Classifications and Prognostic Factors for Functional Outcome. Diagnostics 2021, 11, 1851. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Cui, X.; Buonfiglio, F.; Pfeiffer, N.; Gericke, A. Aging in Ocular Blood Vessels: Molecular Insights and the Role of Oxidative Stress. Biomedicines 2024, 12, 817. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Confalonieri, F.; Ferraro, V.; Barone, G.; Di Maria, A.; Petrovski, B.É.; Vallejo Garcia, J.L.; Randazzo, A.; Vinciguerra, P.; Lumi, X.; Petrovski, G. Outcomes in the Treatment of Subretinal Macular Hemorrhage Secondary to Age-Related Macular Degeneration: A Systematic Review. J. Clin. Med. 2024, 13, 367. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Lendzioszek, M.; Bryl, A.; Poppe, E.; Zorena, K.; Mrugacz, M. Retinal Vein Occlusion-Background Knowledge and Foreground Knowledge Prospects-A Review. J. Clin. Med. 2024, 13, 3950. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Tripepi, D.; Jalil, A.; Ally, N.; Buzzi, M.; Moussa, G.; Rothschild, P.R.; Rossi, T.; Ferrara, M.; Romano, M.R. The Role of Subretinal Injection in Ophthalmic Surgery: Therapeutic Agent Delivery and Other Indications. Int. J. Mol. Sci. 2023, 24, 10535. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Siwik, P.; Chudoba, T.; Cisiecki, S. Retinal Displacement Following Vitrectomy for Rhegmatogenous Retinal Detachment: A Systematic Review of Surgical Techniques, Tamponade Agents, and Outcomes. J. Clin. Med. 2025, 14, 250. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Confalonieri, F.; Josifovska, N.; Boix-Lemonche, G.; Stene-Johansen, I.; Bragadottir, R.; Lumi, X.; Petrovski, G. Vitreous Substitutes from Bench to the Operating Room in a Translational Approach: Review and Future Endeavors in Vitreoretinal Surgery. Int. J. Mol. Sci. 2023, 24, 3342. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Shettigar, M.P.; Dave, V.P.; Chou, H.D.; Fung, A.; Iguban, E.; March de Ribot, F.; Zabala, C.; Hsieh, Y.T.; Lalwani, G. Vitreous substitutes and tamponades—A review of types, applications, and future directions. Indian J. Ophthalmol. 2024, 72, 1102–1111. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Luboń, W.; Luboń, M.; Rokicki, W. Should Chronic Subretinal Hemorrhage Be Treated Surgically? J. Clin. Med. 2025, 14, 7411. https://doi.org/10.3390/jcm14207411
Luboń W, Luboń M, Rokicki W. Should Chronic Subretinal Hemorrhage Be Treated Surgically? Journal of Clinical Medicine. 2025; 14(20):7411. https://doi.org/10.3390/jcm14207411
Chicago/Turabian StyleLuboń, Wojciech, Małgorzata Luboń, and Wojciech Rokicki. 2025. "Should Chronic Subretinal Hemorrhage Be Treated Surgically?" Journal of Clinical Medicine 14, no. 20: 7411. https://doi.org/10.3390/jcm14207411
APA StyleLuboń, W., Luboń, M., & Rokicki, W. (2025). Should Chronic Subretinal Hemorrhage Be Treated Surgically? Journal of Clinical Medicine, 14(20), 7411. https://doi.org/10.3390/jcm14207411





