Edema and Subjective Discomfort After Barbed Stayed Bridge Pharyngoplasty (BSBP)
Abstract
1. Introduction
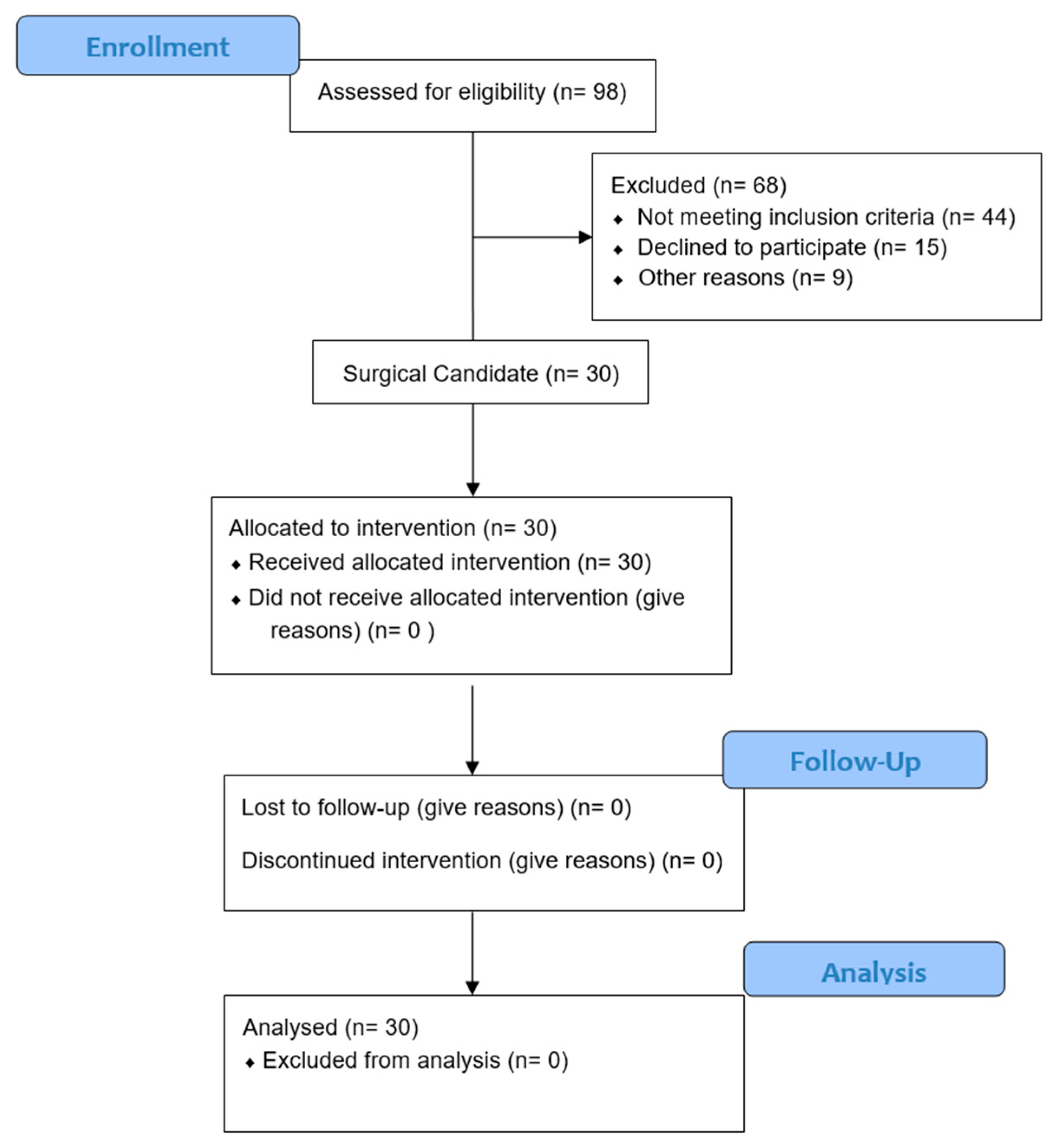
2. Materials and Methods
2.1. Inclusion Criteria
- Age between 30 and 60.
- BMI ≤ 35 kg/m2.
- Moderate OSA patients with AHI > 15 and < 30.
- V1 or 2 concentric/lateral–lateral; O0 or 1; T0; E0.
- Friedman Tongue grade I–II–III.
- Lingual tonsil hypertrophy > 1.
2.2. Exclusion Criteria
- Age < 30 and > 60.
- BMI < 35 kg/m2.
- AHI > 15/h and > 30 h.
- VOTE is different from V1 or 2 concentric/laterolateral; O0 or 1; T0; E0.
- Patients who need a multilevel approach.
- Friedman Tongue grade IV.
- Lingual tonsil hypertrophy > I.
2.3. Surgical Technique: Barbed Stayed Bridge Pharyngoplasty (BSBP)
2.4. Post-Surgery Evaluation
2.5. Statistical Analysis
3. Results
4. Discussion
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| OSA | Obstructive Sleep Apnea |
| CPAP | Continuous Positive Airway Pressure |
| BRP | Barbed Reposition Pharyngoplasty |
| BSBP | Barbed Stayed Bridge Pharyngoplasty |
| PPM | Palatopharyngeal Muscle |
| PGM | Palatoglossal Muscle |
| HSAT | Home Sleep Apnea Testing |
| AHI | Apnea–Hypopnea Index |
| AASM | American Academy of Sleep Medicine |
| DISE | Drug-Induced Sleep Endoscopy |
| VOTE | Velum, Oropharynx, Tongue, Epiglottis (classification system for airway collapse) |
| IV | Intravenous |
| VAS | Visual Analog Scale |
| PPOPS | Palatal Postoperative Problems Score |
| ODI | Oxygen Desaturation Index |
| t90% | Percentage of Time with Oxygen Saturation <90% |
| LPW | Lateral Pharyngeal Wall |
| OSAS | Obstructive Sleep Apnea Syndrome |
| LAUP | Laser-Assisted Uvulopalatoplasty |
| NSAIDs | Non-Steroidal Anti-Inflammatory Drugs |
References
- Gottlieb, D.J.; Punjabi, N.M. Diagnosis and Management of Obstructive Sleep Apnea: A Review. JAMA 2020, 323, 1389–1400. [Google Scholar] [CrossRef]
- Casale, M.; Moffa, A.; Giorgi, L.; Sabatino, L.; Pierri, M.; Lugo, R.; Baptista, P.; Rinaldi, V. No-Cutting Remodelling Intra-Pharyngeal Surgery Can Avoid CPAP in Selected OSA Patients: Myth or Reality? Eur. Arch. Oto-Rhino-Laryngol. 2022, 279, 5039–5045. [Google Scholar] [CrossRef]
- Saenwandee, P.; Neruntarat, C.; Saengthong, P.; Wiriyaamornchai, P.; Khuancharee, K.; Sirisomboonwech, S.; Chuoykwamdee, N. Barbed Pharyngoplasty for Obstructive Sleep Apnea: A Meta-Analysis. Am. J. Otolaryngol. 2022, 43, 103306. [Google Scholar] [CrossRef]
- Maniaci, A.; Di Luca, M.; Lechien, J.R.; Iannella, G.; Grillo, C.; Grillo, C.M.; Merlino, F.; Calvo-Henriquez, C.; De Vito, A.; Magliulo, G.; et al. Lateral Pharyngoplasty vs. Traditional Uvulopalatopharyngoplasty for Patients with OSA: Systematic Review and Meta-Analysis. Sleep Breath. 2022, 26, 1539–1550. [Google Scholar] [CrossRef]
- Vicini, C.; Hendawy, E.; Campanini, A.; Eesa, M.; Bahgat, A.; AlGhamdi, S.; Meccariello, G.; DeVito, A.; Montevecchi, F.; Mantovani, M. Barbed Reposition Pharyngoplasty (BRP) for OSAHS: A Feasibility, Safety, Efficacy and Teachability Pilot Study. “We Are on the Giant’s Shoulders”. Eur. Arch. Oto-Rhino-Laryngol. 2015, 272, 3065–3070. [Google Scholar] [CrossRef]
- Vicini, C.; Salamanca, F.; Iannella, G. Barbed Pharyngoplasty and Sleep Disordered Breathing, 1st ed.; Springer: Cham, Switzerland, 2022. [Google Scholar]
- Magliulo, G.; Iannella, G.; Casale, M.; Vicini, C.; Pace, A. Barbed Stayed Bridge Pharyngoplasty (BSBP). Laryngoscope 2024, 134, 3853–3855. [Google Scholar] [CrossRef]
- Mu, L.; Chen, J.; Nyirenda, T.; Li, J.; Sobotka, S.; Benson, B.; Sanders, I. Morphometric and Immunohistochemical Characteristics of the Adult Human Soft Palate Muscles. J. Histochem. Cytochem. 2022, 70, 225–236. [Google Scholar] [CrossRef] [PubMed]
- Kapur, V.K.; Auckley, D.H.; Chowdhuri, S.; Kuhlmann, D.C.; Mehra, R.; Ramar, K.; Harrod, C.G. Clinical Practice Guideline for Diagnostic Testing for Adult Obstructive Sleep Apnea: An American Academy of Sleep Medicine Clinical Practice Guideline. J. Clin. Sleep Med. 2017, 13, 479–504. [Google Scholar] [CrossRef] [PubMed]
- Friedman, M.; Salapatas, A.M.; Bonzelaar, L.B. Updated Friedman Staging System for Obstructive Sleep Apnea. Adv. Otorhinolaryngol. 2017, 80, 41–48. [Google Scholar] [CrossRef]
- De Vito, A.; Carrasco Llatas, M.; Ravesloot, M.J.; Kotecha, B.; De Vries, N.; Hamans, E.; Maurer, J.; Bosi, M.; Blumen, M.; Heiser, C.; et al. European Position Paper on Drug-Induced Sleep Endoscopy: 2017 Update. Clin. Otolaryngol. 2018, 43, 1541–1552. [Google Scholar] [CrossRef] [PubMed]
- Haefeli, M.; Elfering, A. Pain Assessment. Eur. Spine J. 2006, 15 (Suppl. S1), S17–S24. [Google Scholar] [CrossRef]
- Williamson, A.; Hoggart, B. Pain: A Review of Three Commonly Used Pain Rating Scales. J. Clin. Nurs. 2005, 14, 798–804. [Google Scholar] [CrossRef]
- Ezzat, A.E.M.; El-Shenawy, H.M.; El-Begermy, M.M.; Eid, M.I.; Akel, M.M.; Abbas, A.Y. The Effectiveness of Low-Level Laser on Postoperative Pain and Edema in Secondary Palatal Operation. Int. J. Pediatr. Otorhinolaryngol. 2016, 89, 183–186. [Google Scholar] [CrossRef] [PubMed]
- Modica, D.M.; Lorusso, F.; Presti, G.; Fasola, S.; Gallina, S. Our Assessment Using Palate Postoperative Problems Score (PPOPS): Tool for the Evaluation of Results in Palatal Surgery Techniques. Indian J. Otolaryngol. Head Neck Surg. 2019, 71 (Suppl. S1), 766–770. [Google Scholar] [CrossRef]
- Iannella, G.; Vallicelli, B.; Magliulo, G.; Cammaroto, G.; Meccariello, G.; De Vito, A.; Greco, A.; Pelucchi, S.; Sgarzani, R.; Corso, R.M.; et al. Long-Term Subjective Outcomes of Barbed Reposition Pharyngoplasty for Obstructive Sleep Apnea Syndrome Treatment. Int. J. Environ. Res. Public Health 2020, 17, 1542. [Google Scholar] [CrossRef] [PubMed]
- Wischhusen, J.; Qureshi, U.; Camacho, M. Laser-Assisted Uvulopalatoplasty (LAUP) Complications and Side Effects: A Systematic Review. Nat. Sci. Sleep 2019, 11, 59–67. [Google Scholar] [CrossRef]
- Schwab, R.J.; Pasirstein, M.; Pierson, R.; Mackley, A.; Hachadoorian, R.; Arens, R.; Maislin, G.; Pack, A.I. Identification of Upper Airway Anatomic Risk Factors for Obstructive Sleep Apnea with Volumetric Magnetic Resonance Imaging. Am. J. Respir. Crit. Care Med. 2003, 168, 522–530. [Google Scholar] [CrossRef] [PubMed]
- Schwab, R.J.; Lin, T.C.; Wiemken, A.S.; Tang, S.H.; Schwab, A.; Keenan, B.T. Effect of Neck-Bending on Upper Airway Caliber and Surrounding Soft Tissues in Controls and Apneics. Medrxiv 2025, 19, 2025.06.05.25329072. [Google Scholar] [CrossRef]
- Li, H.Y. Palatal Surgery for Obstructive Sleep Apnea: From Ablation to Reconstruction. Sleep Med. Clin. 2019, 14, 51–58. [Google Scholar] [CrossRef]
- Rashwan, M.S.; Montevecchi, F.; Cammaroto, G.; el Deen, M.B.; Iskander, N.; El Hennawi, D.; El Tabbakh, M.; Meccariello, G.; Gobbi, R.; Stomeo, F.; et al. Evolution of Soft Palate Surgery Techniques for Obstructive Sleep Apnea Patients: A Comparative Study for Single-Level Palatal Surgeries. Clin. Otolaryngol. 2018, 43, 584–590. [Google Scholar] [CrossRef]
- Cammaroto, G.; Bettini, P.; Meccariello, G.; Cannavicci, A.; Iannella, G.; Stringa, L.M.; Visconti, I.C.; Ciorba, A.; Bianchini, C.; Pelucchi, S.; et al. Barbed Repositioning Pharyngoplasty: Tips and Tricks. Otolaryngol.-Head Neck Surg. 2024, 170, 1204–1207. [Google Scholar] [CrossRef] [PubMed]

| Time 0 | Time 1 | p-Value | |
|---|---|---|---|
| AHI | 23.4 (2.1) 23.4 (21.8; 25.4) | 7.2 (2.6) 6.8 (4.9; 8.0) | <0.001 |
| ODI | 21.0 (4.1) 21.9 (16.4; 22.8) | 6.5 (2.1) 6.2 (5.1; 7.1) | <0.001 |
| ESS | 5.1 (3.4) 4 (3; 8) | 3.5 (2.5) 3 (1; 6) | <0.001 |
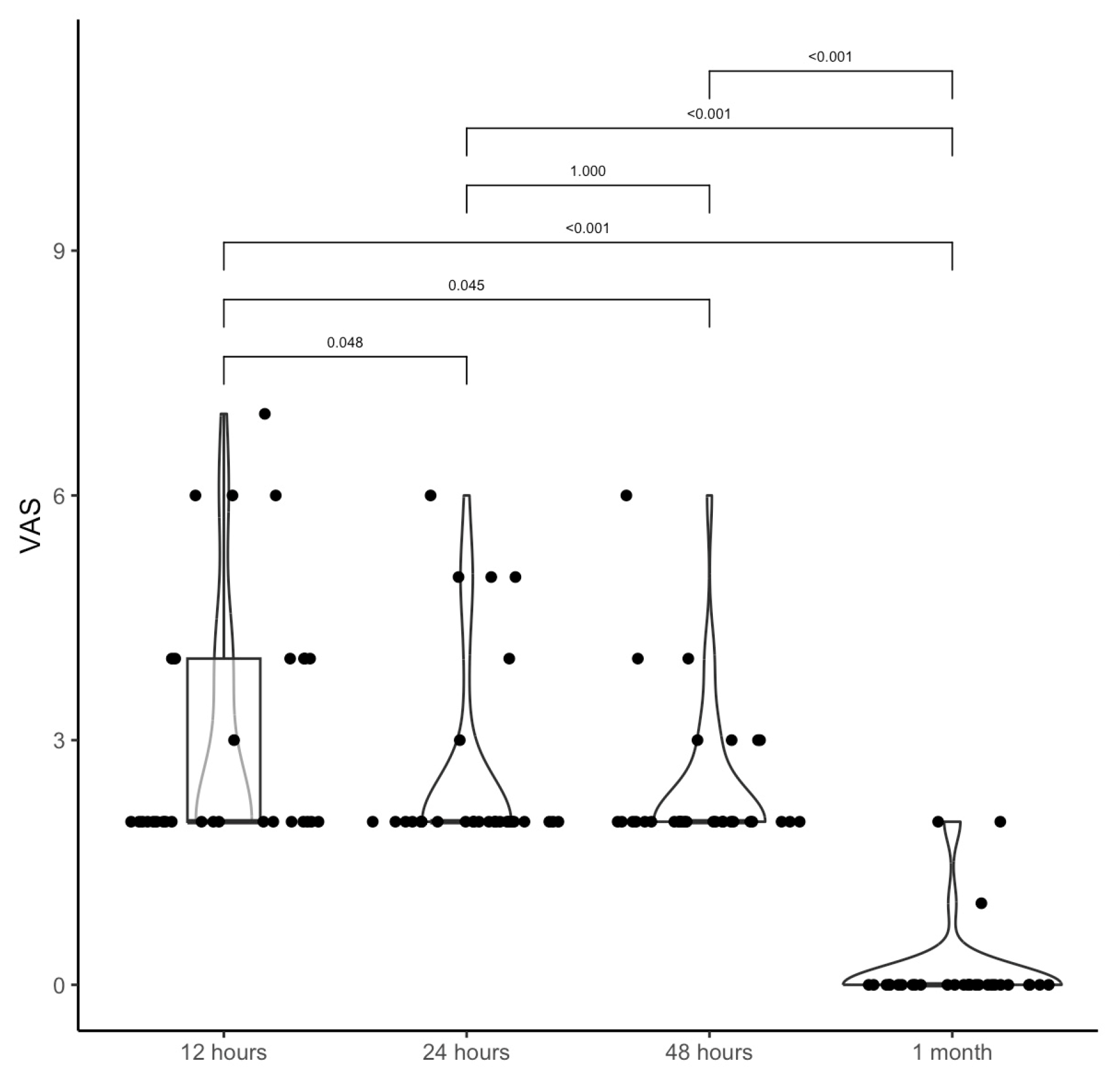
| 12 h | 24 h | 48 h | 1 Month |
|---|---|---|---|
| VAS→3.0 (1.5) | 2.5 (1.2) | 2.4 (0.9) | 0.2 (0.5) |
| 2 (2; 4) | 2 (2; 2) | 2 (2; 2) | 0 (0; 0) |
| p | |||
| 12 h | 24 h | 0.048 | |
| 12 h | 48 h | 0.045 | |
| 12 h | 1 month | <0.001 | |
| 24 h | 48 h | 1.000 | |
| 24 h | 1 month | <0.001 | |
| 48 h | 1 month | <0.001 |
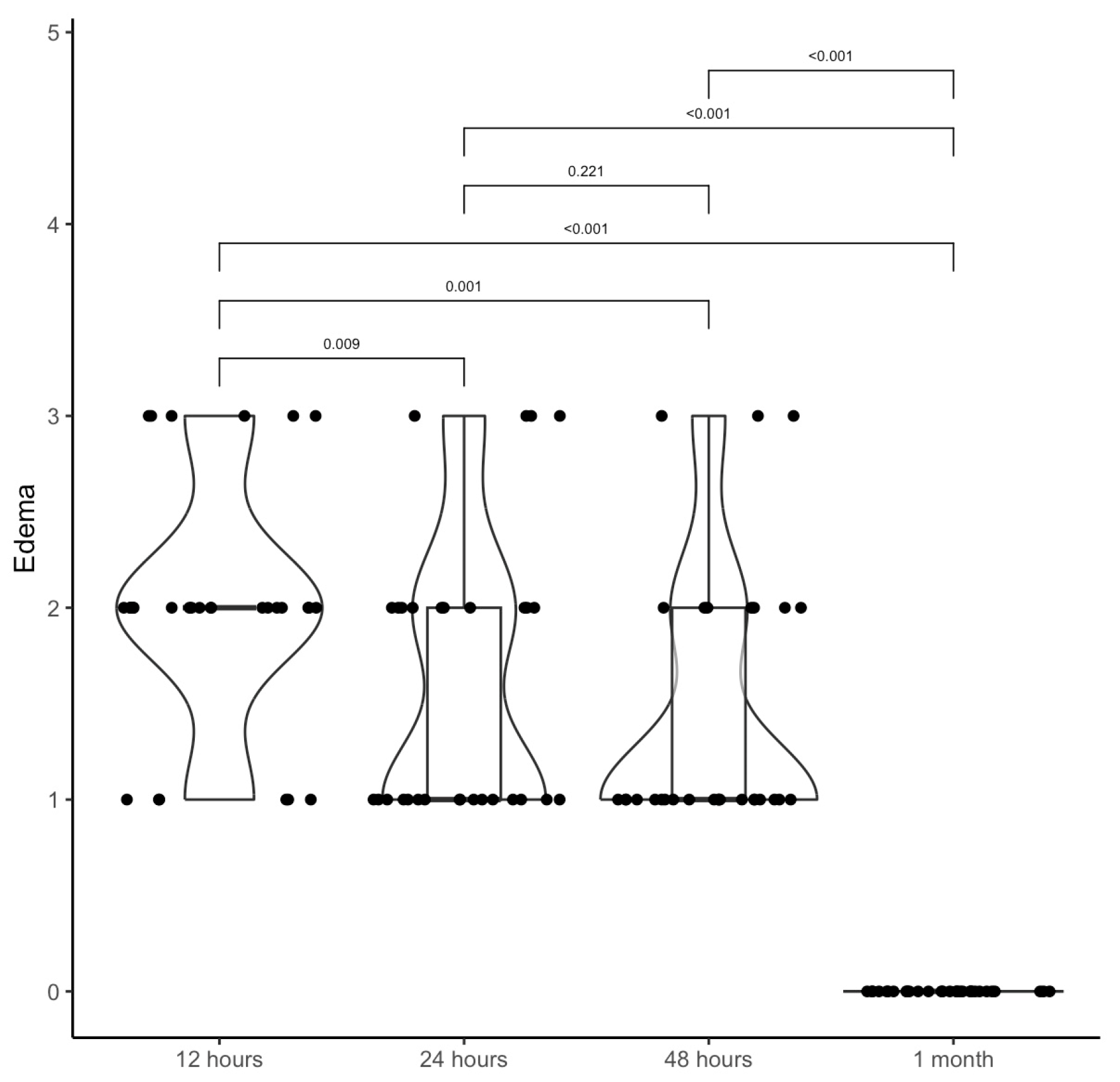
| 12 h | 24 h | 48 h | 1 Month |
|---|---|---|---|
| Edema→2.0 (0.6) | 1.6 (0.7) | 1.4 (0.7) | 0.0 (0.0) |
| 2 (2; 2) | 1 (1; 2) | 1 (1; 2) | 0 (0; 0) |
| p | |||
| 12 h | 24 h | 0.009 | |
| 12 h | 48 h | 0.001 | |
| 12 h | 1 month | <0.001 | |
| 24 h | 48 h | 0.221 | |
| 24 h | 1 month | <0.001 | |
| 48 h | 1 month | <0.001 |
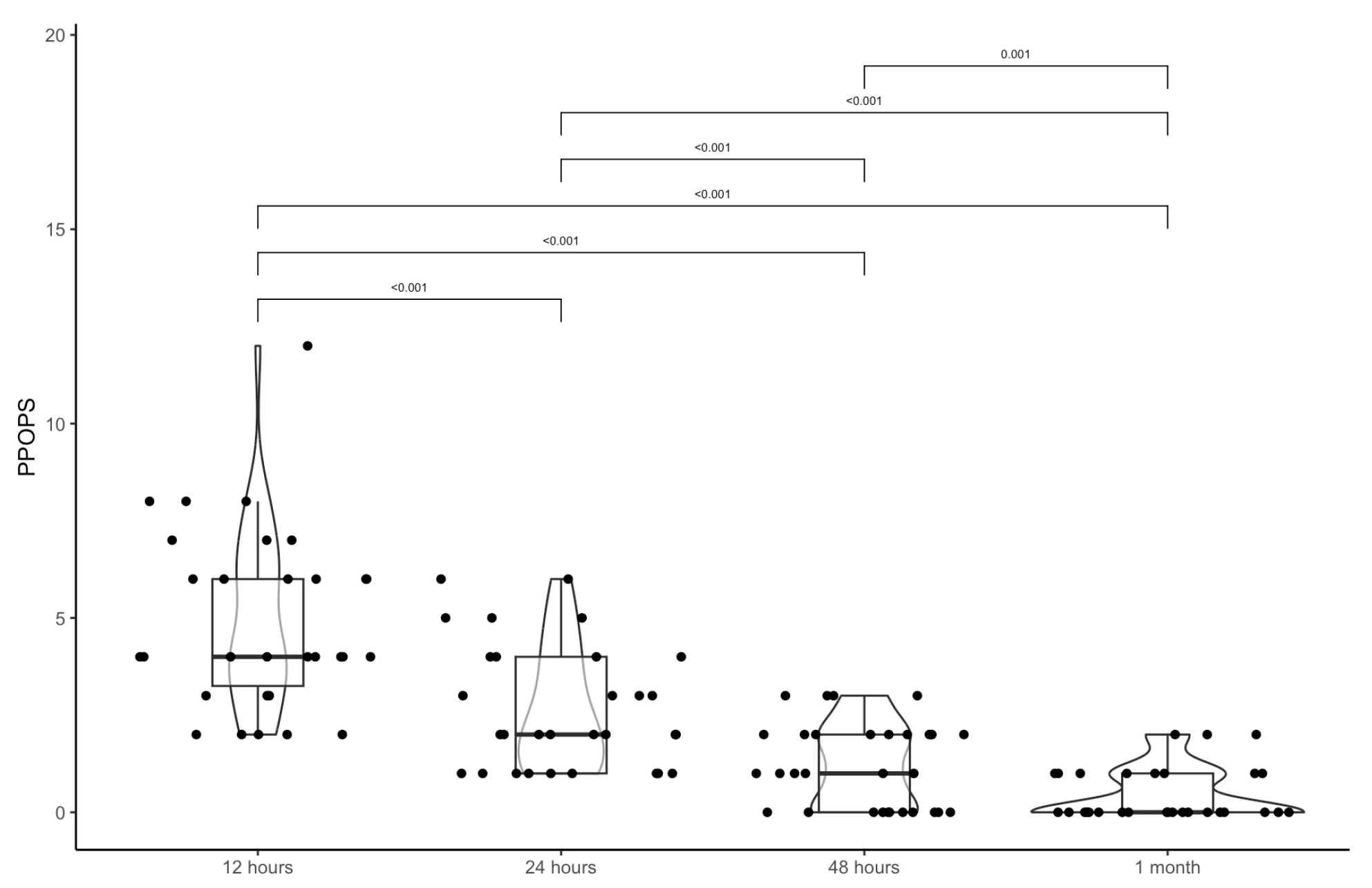
| 12 h | 24 h | 48 h | 1 Month |
|---|---|---|---|
| PPOPS→4.9 (2.3) | 2.7 (1.6) | 1.2 (1.1) | 0.5 (0.7) |
| 4 (3.2; 6) | 2 (1; 4) | 1 (0; 2) | 0 (0; 1) |
| p | |||
| 12 h | 24 h | <0.001 | |
| 12 h | 48 h | <0.001 | |
| 12 h | 1 month | <0.001 | |
| 24 h | 48 h | <0.001 | |
| 24 h | 1 month | <0.001 | |
| 48 h | 1 month | 0.001 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Pace, A.; Iannella, G.; Maniaci, A.; Cocuzza, S.; Moffa, A.; Alunni Fegatelli, D.; Manno, A.; De Virgilio, A.; Casale, M.; Magliulo, G. Edema and Subjective Discomfort After Barbed Stayed Bridge Pharyngoplasty (BSBP). J. Clin. Med. 2025, 14, 7402. https://doi.org/10.3390/jcm14207402
Pace A, Iannella G, Maniaci A, Cocuzza S, Moffa A, Alunni Fegatelli D, Manno A, De Virgilio A, Casale M, Magliulo G. Edema and Subjective Discomfort After Barbed Stayed Bridge Pharyngoplasty (BSBP). Journal of Clinical Medicine. 2025; 14(20):7402. https://doi.org/10.3390/jcm14207402
Chicago/Turabian StylePace, Annalisa, Giannicola Iannella, Antonino Maniaci, Salvatore Cocuzza, Antonio Moffa, Danilo Alunni Fegatelli, Alessandra Manno, Armando De Virgilio, Manuele Casale, and Giuseppe Magliulo. 2025. "Edema and Subjective Discomfort After Barbed Stayed Bridge Pharyngoplasty (BSBP)" Journal of Clinical Medicine 14, no. 20: 7402. https://doi.org/10.3390/jcm14207402
APA StylePace, A., Iannella, G., Maniaci, A., Cocuzza, S., Moffa, A., Alunni Fegatelli, D., Manno, A., De Virgilio, A., Casale, M., & Magliulo, G. (2025). Edema and Subjective Discomfort After Barbed Stayed Bridge Pharyngoplasty (BSBP). Journal of Clinical Medicine, 14(20), 7402. https://doi.org/10.3390/jcm14207402









