A Logistic Regression Model for Predicting Osteoporosis Using Alveolar Bone Mineral Density Measured on Intraoral Radiographs Combined with Panoramic Mandibular Cortical Index
Abstract
1. Introduction
2. Materials and Methods
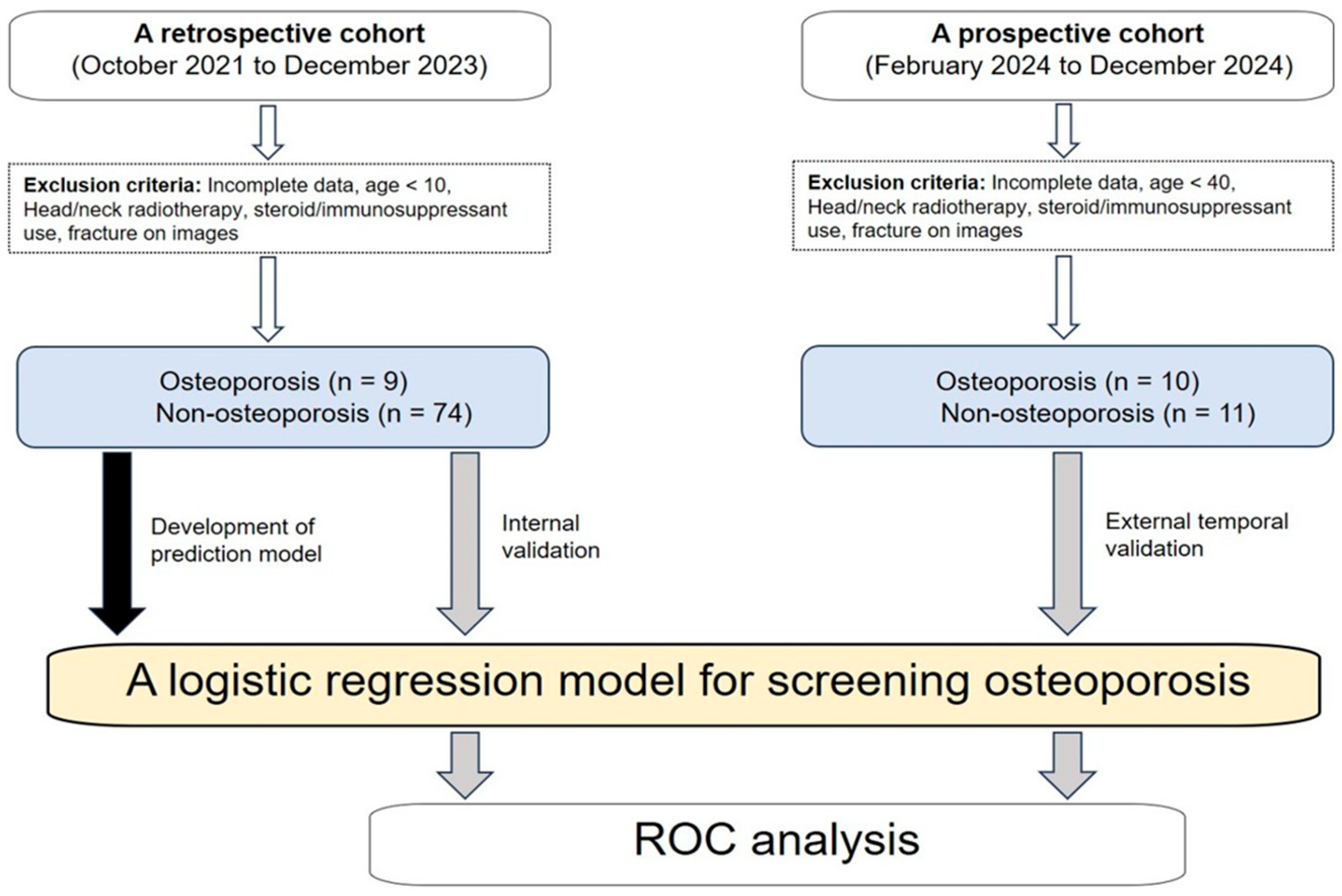
2.1. Study Participants
2.2. Intraoral Radiography and Bone Mineral Density Measurement
2.3. Panoramic Mandibular Cortical Index Evaluation
2.4. Development and Evaluation of a Logistic Regression Model
2.5. Ethical Approval
2.6. Statistical Analysis
3. Results
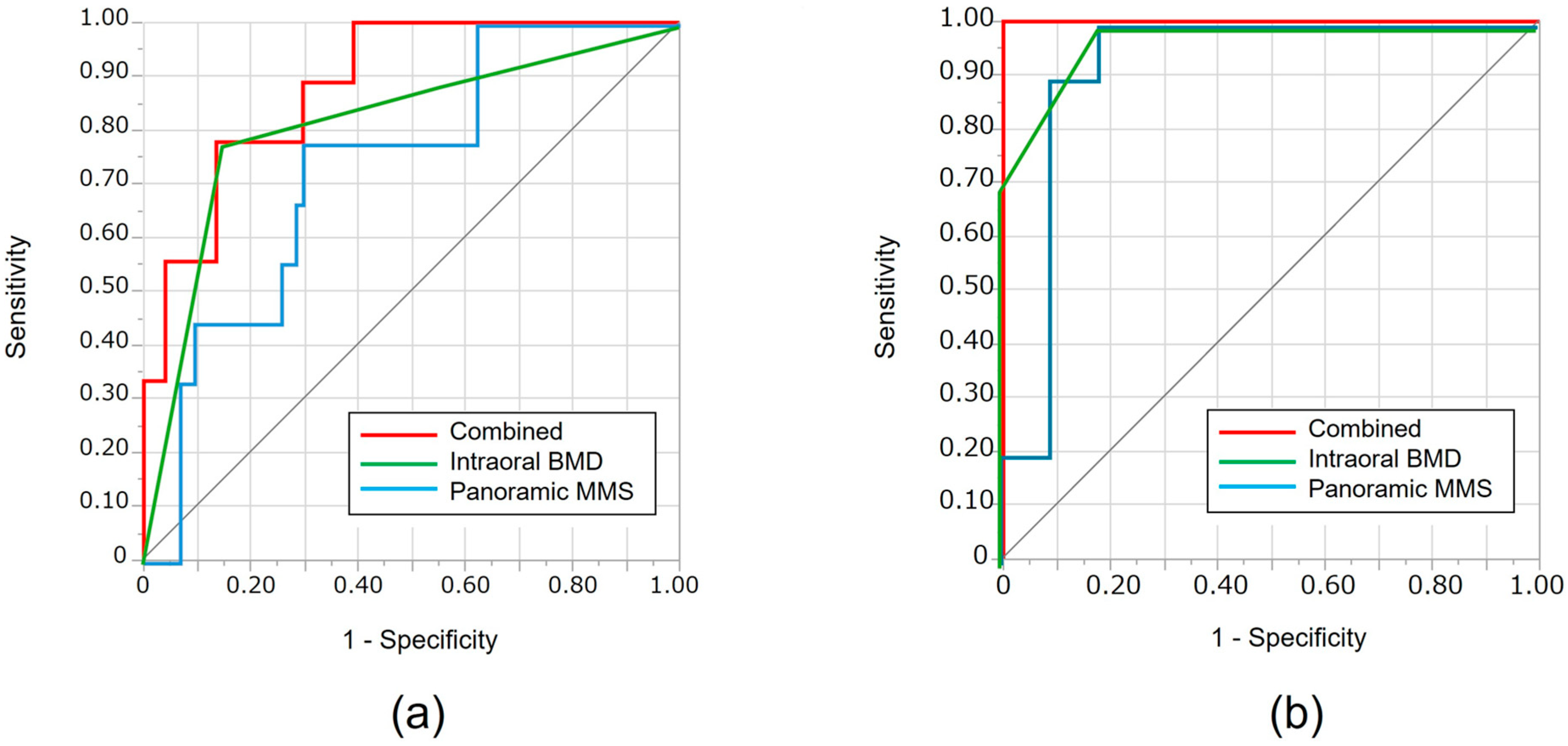
3.1. Internal Validation Using the Training Cohort
3.2. External Validation Using the Temporal Cohort
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| al-BMD | Alveolar Bone Mineral Density |
| AUC | Area Under the Curve |
| BMD | Bone Mineral Density |
| DXA | Dual-energy X-ray Absorptiometry |
| MCI | Mandibular Cortical Index |
| MRONJ | Medication-Related Osteonecrosis of the Jaw |
| ROC | Receiver Operating Characteristic |
| ROI | Region of Interest |
References
- Chongruangsri, N.-n.; Jansisyanont, P.; Chuenchompoonut, V.; Amphansap, T.; Stitkitti, N. Digital Panoramic Radiographic Indices Correlated with BMD Status. J. Dent. Assoc. Thail. 2021, 71, 194–204. Available online: https://www.jdat.org/data/upload/file-20220224121221.pdf (accessed on 15 September 2025).[Green Version]
- Ghasemi, N.; Rokhshad, R.; Zare, Q.; Shobeiri, P.; Schwendicke, F. Artificial intelligence for osteoporosis detection on panoramic radiography: A systematic review and meta analysis. J. Dent. 2025, 156, 105650. [Google Scholar] [CrossRef] [PubMed]
- Kanis, J.A.; Johnell, O.; Oden, A.; Johansson, H.; McCloskey, E. FRAX® and the assessment of fracture probability in men and women from the UK. Osteoporos. Int. 2008, 19, 385–397. [Google Scholar] [CrossRef] [PubMed]
- NIH Consensus Development Panel on Osteoporosis Prevention, Diagnosis, and Therapy. Osteoporosis prevention, diagnosis, and therapy. JAMA 2001, 285, 785–795. [Google Scholar] [CrossRef] [PubMed]
- Gaudin, R.; Vinayahalingam, S.; van Nistelrooij, N.; Ghanad, I.; Otto, W.; Kewenig, S.; Rendenbach, C.; Alevizakos, V.; Grün, P.; Kofler, F.; et al. AI-powered identification of osteoporosis in dental panoramic radiographs: Addressing methodological flaws in current research. Diagnostics 2024, 14, 2298. [Google Scholar] [CrossRef] [PubMed]
- Kato, C.N.; Tavares, N.P.; Barra, S.G.; Amaral, T.M.; Brasileiro, C.B.; Abreu, L.G.; Mesquita, R.A. Digital panoramic radiography and cone-beam CT as ancillary tools to detect low bone mineral density in post-menopausal women. Dentomaxillofac. Radiol. 2019, 48, 20180254. [Google Scholar] [CrossRef] [PubMed]
- Taguchi, A.; Suei, Y.; Sanada, M.; Ohtsuka, M.; Nakamoto, T.; Sumida, H.; Ohama, K.; Tanimoto, K. Validation of dental panoramic radiography measures for identifying postmenopausal women with spinal osteoporosis. AJR Am. J. Roentgenol. 2004, 183, 1755–1760. [Google Scholar] [CrossRef] [PubMed]
- Geraets, W.G.; Verheij, J.G.; van der Stelt, P.F.; Horner, K.; Lindh, C.; Nicopoulou-Karayianni, K.; Jacobs, R.; Harrison, E.J.; Adams, J.E.; Devlin, H. Prediction of bone mineral density with dental radiographs. Bone 2007, 40, 1217–1221. [Google Scholar] [CrossRef] [PubMed]
- Graham, J. Detecting low bone mineral density from dental radiographs: A mini-review. Clin. Cases Miner. Bone Metab. 2015, 12, 178–182. [Google Scholar] [CrossRef] [PubMed]
- Khadivi, G.; Akhtari, A.; Sharifi, F.; Zargarian, N.; Esmaeili, S.; Ahsaie, M.G.; Shahbazi, S. Diagnostic accuracy of artificial intelligence models in detecting osteoporosis using dental images: A systematic review and meta-analysis. Osteoporos. Int. 2025, 36, 1–19. [Google Scholar] [CrossRef] [PubMed]
- Taguchi, A.; Tanaka, R.; Kakimoto, N.; Morimoto, Y.; Arai, Y.; Hayashi, T.; Kurabayashi, T.; Katsumata, A.; Asaumi, J.; Japanese Society for Oral and Maxillofacial Radiology. Clinical guidelines for the application of panoramic radiographs in screening for osteoporosis. Oral Radiol. 2021, 37, 189–208. [Google Scholar] [CrossRef] [PubMed]
- Jeon, S.J.; Yun, J.P.; Yeom, H.G.; Shin, W.S.; Lee, J.H.; Jeong, S.H.; Seo, M.S. Deep-learning for predicting C-shaped canals in mandibular second molars on panoramic radiographs. Dento Maxillo Fac. Radiol. 2021, 50, 20200513. [Google Scholar] [CrossRef] [PubMed]
- Calciolari, E.; Donos, N.; Park, J.C.; Petrie, A.; Mardas, N. Panoramic measures for oral bone mass in detecting osteoporosis: A systematic review and meta-analysis. J. Dent. Res. 2015, 94, 17S–27S. [Google Scholar] [CrossRef] [PubMed]
- Savic Pavicin, I.; Dumancic, J.; Jukic, T.; Badel, T.; Badanjak, A. Digital orthopantomograms in osteoporosis detection: Mandibular density and mandibular radiographic indices as skeletal BMD predictors. Dento Maxillo Fac. Radiol. 2014, 43, 20130366. [Google Scholar] [CrossRef] [PubMed]
- Horner, K.; Devlin, H.; Alsop, C.W.; Hodgkinson, I.M.; Adams, J.E. Mandibular bone mineral density as a predictor of skeletal osteoporosis. Br. J. Radiol. 1996, 69, 1019–1025. [Google Scholar] [CrossRef] [PubMed]
- Nakamoto, T.; Hatsuta, S.; Yagi, S.; Verdonschot, R.G.; Taguchi, A.; Kakimoto, N. Computer-aided diagnosis system for osteoporosis based on quantitative evaluation of mandibular lower border porosity using panoramic radiographs. Dento Maxillo Fac. Radiol. 2020, 49, 20190481. [Google Scholar] [CrossRef] [PubMed]
- Tarighatnia, A.; Amanzadeh, M.; Hamedan, M.; Mohammadnia, A.; Nader, N.D. Deep learning-based evaluation of panoramic radiographs for osteoporosis screening: A systematic review and meta-analysis. BMC Med. Imaging 2025, 25, 86. [Google Scholar] [CrossRef] [PubMed]
- Katsumata, A.; Kohinata, K.; Esaki, Y.; Kawai, M. Variance of radiographical alveolar bone mineral density by the anatomical morphology of mandibular bone. Heliyon 2022, 8, e11507. [Google Scholar] [CrossRef] [PubMed]
- Oohashi, M.; Mizuhashi, F.; Sugawara, Y.; Saegusa, H.; Katsumata, A.; Ogura, I. Computer-assisted measurement of radiographical alveolar bone density using intraoral radiographs Preliminary study on comparison between men and women in young adults. J. Oral Maxillofac. Radiol. 2020, 8, 1–4. [Google Scholar] [CrossRef]
- Sigua-Rodriguez, E.A.; da Costa Ribeiro, R.; de Brito, A.C.R.; Alvarez-Pinzon, N.; de Albergaria-Barbosa, J.R. Bisphosphonate-related osteonecrosis of the jaw: A review of the literature. Int. J. Dent. 2014, 2014, 192320. [Google Scholar] [CrossRef] [PubMed]
- Shin, J.W.; Kim, J.E.; Huh, K.H.; Yi, W.J.; Heo, M.S.; Lee, S.S.; Choi, S.C. Radiological manifestations and clinical findings of patients with oncologic and osteoporotic medication-related osteonecrosis of the jaw. Sci. Rep. 2024, 14, 8744. [Google Scholar] [CrossRef] [PubMed]
- Alam, T.; AlShahrani, I.; Assiri, K.I.; Almoammar, S.; Togoo, R.A.; Luqman, M. Evaluation of clinical and radiographic parameters as dental indicators for postmenopausal osteoporosis. Oral Health Prev. Dent. 2020, 18, 499–504. [Google Scholar] [CrossRef] [PubMed]
- Osanai, H.; Kuroiwa, H.; Yamada, S.; Sugino, N.; Nakamoto, T.; Ohtsuka, M.; Suei, Y.; Kakimoto, N.; Taguchi, A. Screening ability of dental students to detect osteoporosis on dental panoramic radiographs. Osteoporos. Sarcopenia 2024, 10, 145–150. [Google Scholar] [CrossRef] [PubMed]
- Kubo, R.; Yoshida, R.; Baba-Tajiri, R.; Nakamura-Yamada, H.; Miyahara, T.; Ooyama, T.; Inoue, J.; Hirosue, A.; Kawahara, K.; Nakamoto, M.; et al. Differences in alveolar bone mineral density by tooth type in female osteoporotic patients treated with bisphosphonates. Oral Sci. Int. 2025, 22, e1285. [Google Scholar] [CrossRef]
- Heuchert, J.; Kozieł, S.; Spinek, A.E. Radiomorphometric indices of the mandible as indicators of decreased bone mineral density and osteoporosis—Meta-analysis and systematic review. Osteoporos. Int. 2024, 35, 401–412. [Google Scholar] [CrossRef]
- Nakamoto, T.; Taguchi, A.; Kakimoto, N. Osteoporosis screening support system from panoramic radiographs using deep learning by convolutional neural network. Dento Maxillo Fac. Radiol. 2022, 51, 20220135. [Google Scholar] [CrossRef] [PubMed]
- Ono, R.; Katsumata, A.; Fujikawa, Y.; Takahira, E.; Yamamoto, T.; Kanamura, N. Sex differences and age-related changes in the mandibular alveolar bone mineral density using a computer-aided measurement system for intraoral radiography. Sci. Rep. 2024, 14, 7386. [Google Scholar] [CrossRef] [PubMed]
- Kinalski, M.A.; Boscato, N.; Damian, M.F. The accuracy of panoramic radiography as a screening of bone mineral density in women: A systematic review. Dento Maxillo Fac. Radiol. 2020, 49, 20190149. [Google Scholar] [CrossRef] [PubMed]


| Characteristics | Training (Internal Validation) Cohort (n = 83) | External (Temporal) Validation Cohort (n = 21) | |||||
|---|---|---|---|---|---|---|---|
| Osteoporosis (n = 9) | Non-Osteoporosis (n = 74) | p Value | Osteoporosis (n = 10) | Non-Osteoporosis (n = 11) | p Value | ||
| Sex | Female | 8 | 46 | 0.150 | 9 | 8 | 0.59 |
| Male | 1 | 28 | 1 | 3 | |||
| Age (years) | Mean ± SD | 75.4 ± 10.8 | 51.9 ± 22.4 | 0.010 | 76.1 ± 8.3 | 54.2 ± 11.1 | 0.022 |
| al- BMD (mg/cm2) | Mean ± SD | 858.5 ± 179.4 | 1016.6 ± 232.3 | 0.032 | 773.2 ± 192.7 | 1204.6 ± 295.6 | 0.019 |
| MCI | class 1 and 2 | 2 | 63 | 0.003 | 3 | 11 | <0.001 |
| class 3 | 7 | 11 | 7 | 0 | |||
| History of steroid use | Present | 1 | 2 | 0.29 | 0 | 0 | <0.001 |
| Absent | 8 | 72 | 10 | 11 | |||
| Diabetes | Present | 0 | 4 | 1.00 | 1 | 0 | 0.48 |
| Absent | 9 | 70 | 9 | 11 | |||
| History of malignant tumors | Present | 1 | 3 | 0.37 | 0 | 2 | 0.48 |
| Absent | 8 | 71 | 10 | 9 | |||
| Thyroid disease | Present | 0 | 6 | 1.00 | 1 | 3 | 0.59 |
| (Graves’ disease, hypothyroidism, chronic thyroiditis) | Absent | 9 | 68 | 9 | 8 | ||
| Training (Internal Validation) Cohort (n = 83) | External (Temporal) Validation Cohort (n = 21) | |||||
|---|---|---|---|---|---|---|
| al-BMD Alone | MCI Alone | Combined Model | al-BMD Alone | MCI Alone | Combined Model | |
| Cutoff value | 884.8 | Class 2 | 0.23 | 1067.1 | Class 2 | 0.13 |
| AUC | 0.74 | 0.82 | 0.88 | 0.92 | 0.97 | 1.00 |
| Sensitivity | 0.78 | 0.78 | 0.87 | 0.82 | 1.00 | 1.00 |
| Specificity | 0.70 | 0.85 | 0.78 | 1.00 | 0.82 | 1.00 |
| Accuracy | 0.71 | 0.86 | 0.86 | 0.91 | 0.91 | 1.00 |
| Multivariate Analysis | ||
|---|---|---|
| Variable | OR (95% CI) | p-Value |
| Age | 0.033 (5.078 × 10−5–29.9) | 0.21 |
| al-BMD values from intraoral radiographs | 10.3 (3.69–15.8) | 0.014 |
| MCI from panoramic radiographs | 0.10 (0.0064–9.81) | 0.033 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Okubo, S.; Miyabe, S.; Kise, Y.; Kuwada, T.; Hirukawa, A.; Gotoh, K.; Katsumata, A.; Shibata, N.; Morotomi, T.; Okada, S.; et al. A Logistic Regression Model for Predicting Osteoporosis Using Alveolar Bone Mineral Density Measured on Intraoral Radiographs Combined with Panoramic Mandibular Cortical Index. J. Clin. Med. 2025, 14, 7198. https://doi.org/10.3390/jcm14207198
Okubo S, Miyabe S, Kise Y, Kuwada T, Hirukawa A, Gotoh K, Katsumata A, Shibata N, Morotomi T, Okada S, et al. A Logistic Regression Model for Predicting Osteoporosis Using Alveolar Bone Mineral Density Measured on Intraoral Radiographs Combined with Panoramic Mandibular Cortical Index. Journal of Clinical Medicine. 2025; 14(20):7198. https://doi.org/10.3390/jcm14207198
Chicago/Turabian StyleOkubo, Satoshi, Satoru Miyabe, Yoshitaka Kise, Tsutomu Kuwada, Akiko Hirukawa, Kenichi Gotoh, Akitoshi Katsumata, Naoki Shibata, Takahiko Morotomi, Soma Okada, and et al. 2025. "A Logistic Regression Model for Predicting Osteoporosis Using Alveolar Bone Mineral Density Measured on Intraoral Radiographs Combined with Panoramic Mandibular Cortical Index" Journal of Clinical Medicine 14, no. 20: 7198. https://doi.org/10.3390/jcm14207198
APA StyleOkubo, S., Miyabe, S., Kise, Y., Kuwada, T., Hirukawa, A., Gotoh, K., Katsumata, A., Shibata, N., Morotomi, T., Okada, S., Watanabe, S., Nagao, T., Ariji, E., & Goto, M. (2025). A Logistic Regression Model for Predicting Osteoporosis Using Alveolar Bone Mineral Density Measured on Intraoral Radiographs Combined with Panoramic Mandibular Cortical Index. Journal of Clinical Medicine, 14(20), 7198. https://doi.org/10.3390/jcm14207198







