Ultrasound Assessment of Breech Engagement: Breech Progression Angle and Prediction of External Cephalic Version Success
Abstract
1. Introduction
2. Materials and Methods
2.1. Participants
2.2. Ultrasound Assessment
2.3. ECV Procedure
2.4. Statistical Analysis
3. Results
3.1. Association Between BPA and ECV Outcome
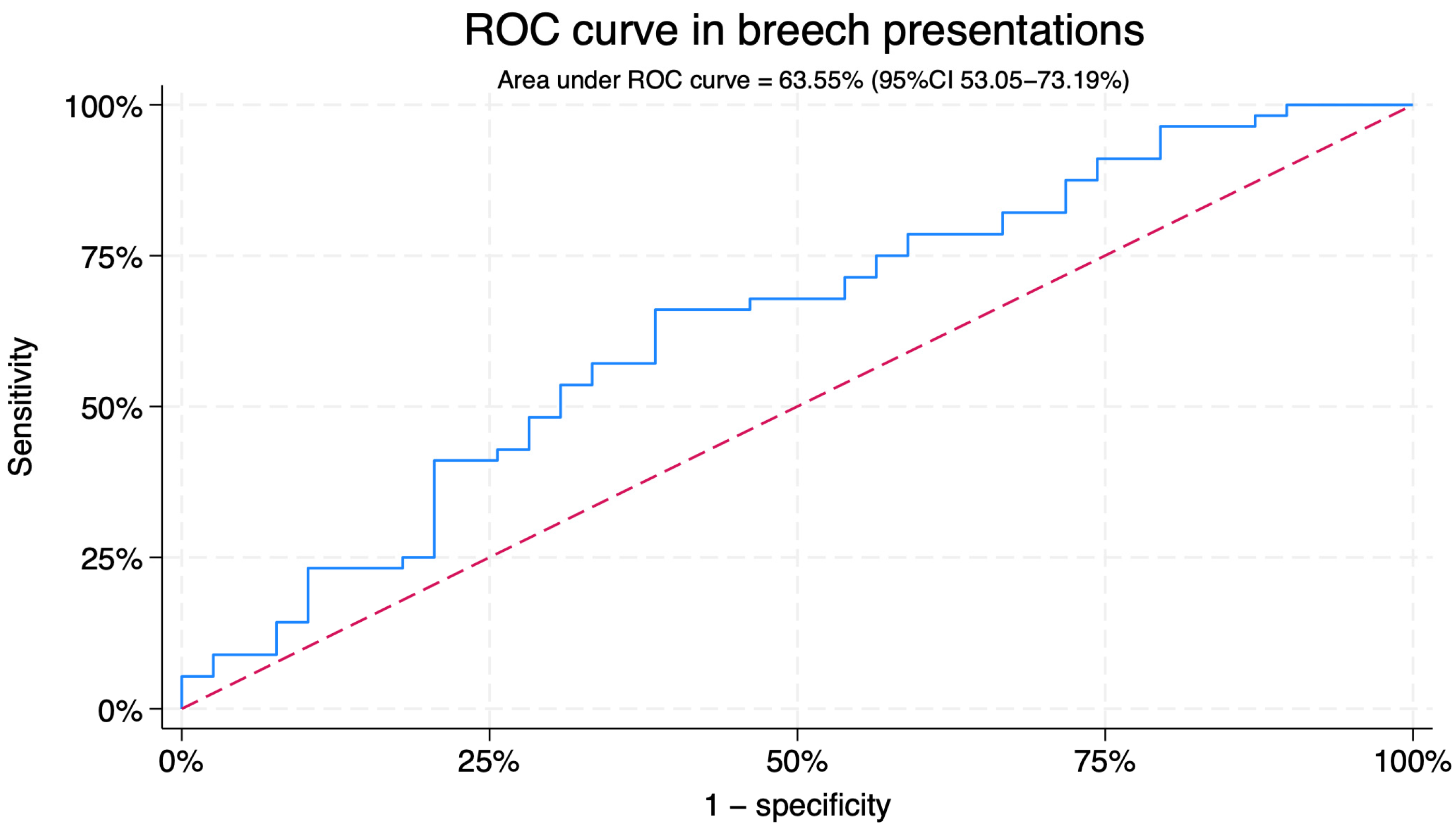
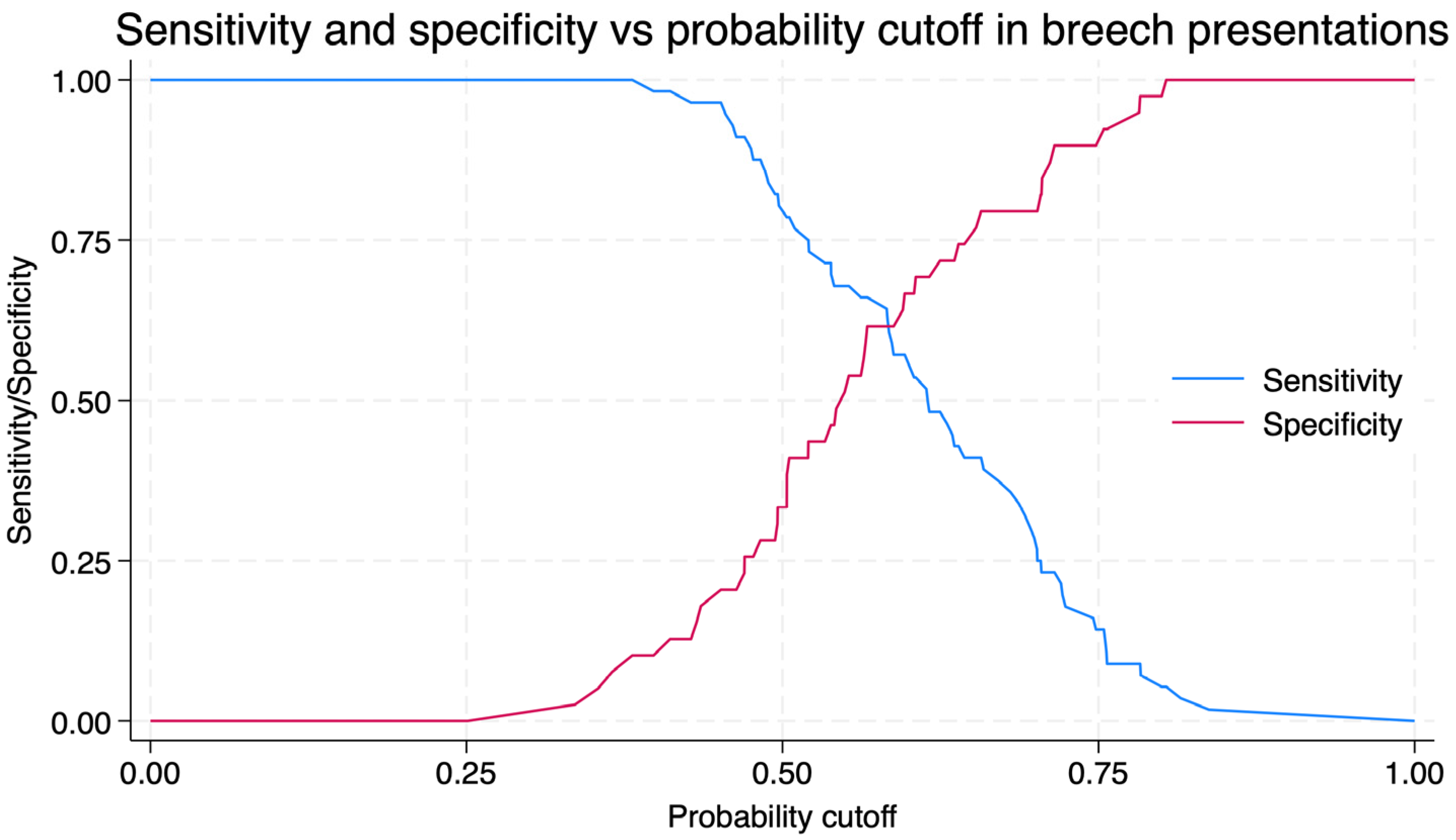
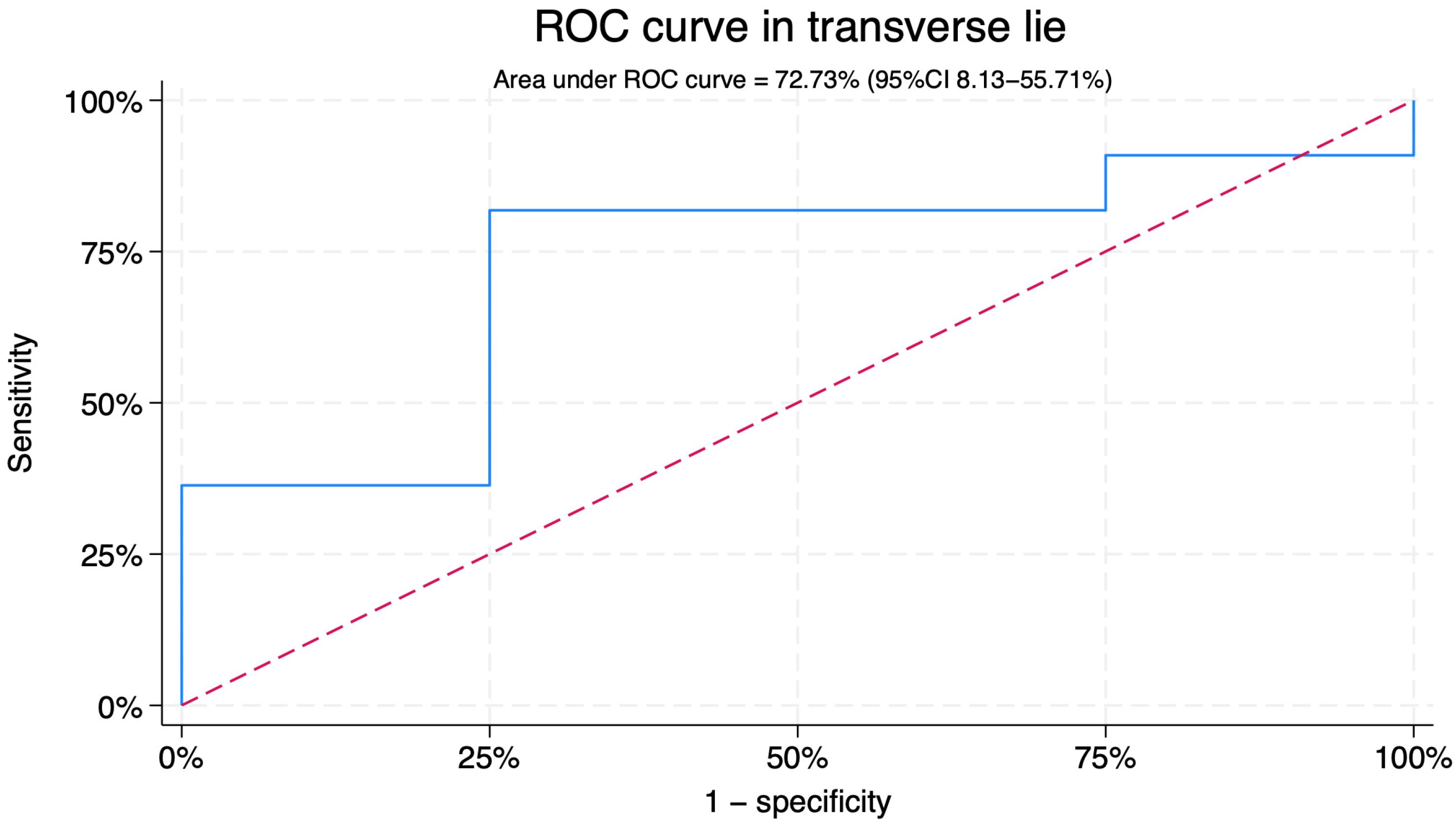
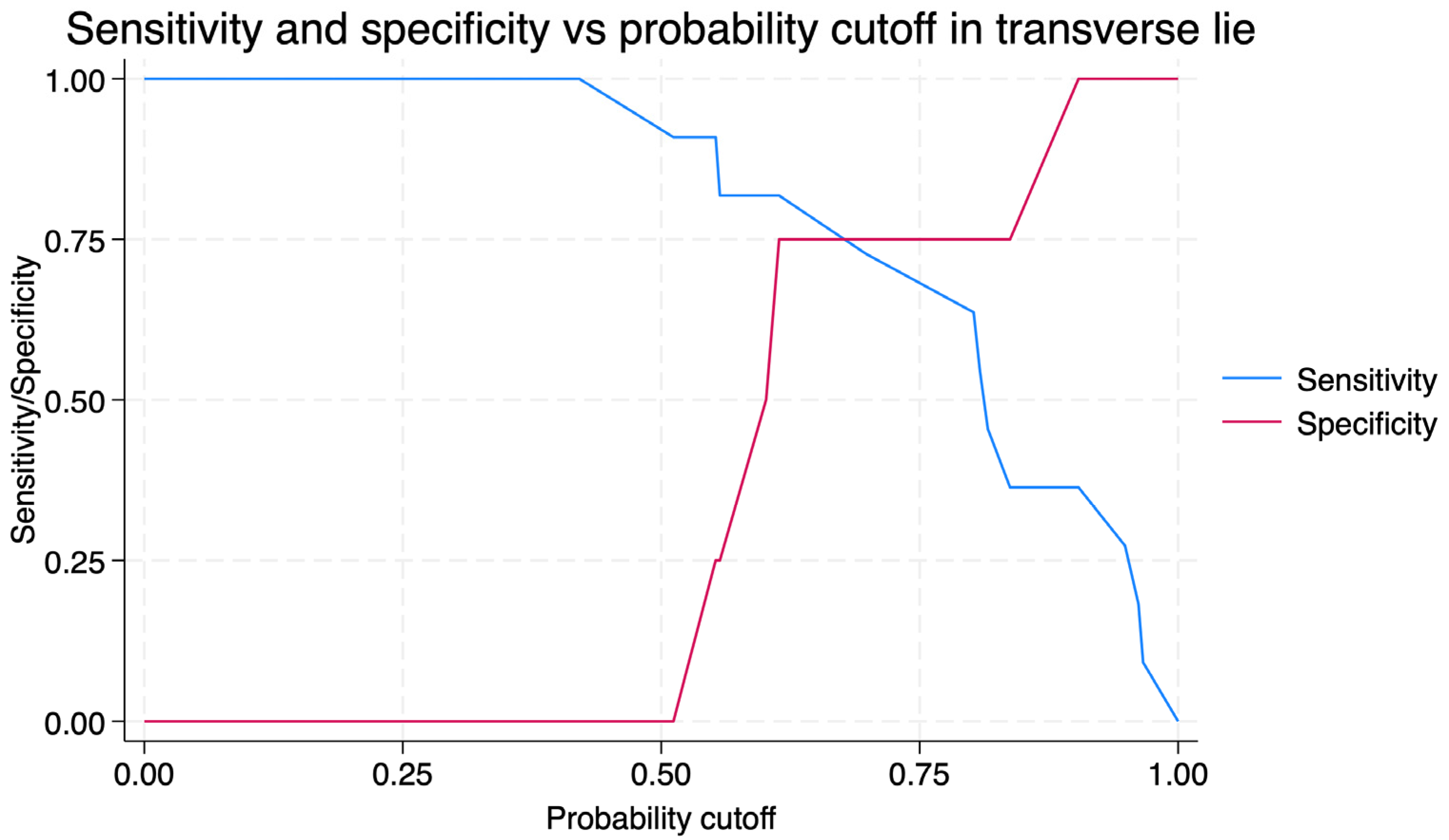
3.2. Predictive Performance of BPA
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Hughey, M.J. Fetal Position during Pregnancy. Am. J. Obstet. Gynecol. 1985, 153, 885–886. [Google Scholar] [CrossRef]
- World Health Organization WHO Recommendations Non-Clinical Interventions to Reduce Unnecessary Caesarean Sections; World Health Organization: Geneva, Switzerland, 2018; ISBN 978-92-4-155033-8.
- Impey, L.; Pandit, M. Tocolysis for Repeat External Cephalic Version in Breech Presentation at Term: A Randomized, Double-Blind, Placebo-Controlled Trial. Obstet. Gynecol. Surv. 2005, 60, 629–630. [Google Scholar] [CrossRef]
- Sánchez-Romero, J.; López-Pérez, J.; Flores-Muñoz, A.B.; Méndez-Martínez, M.J.; Araico-Rodríguez, F.; Mendiola-Olivares, J.; Blanco-Carnero, J.E.; Falcón-Araña, L.; Nieto-Díaz, A.; Sánchez-Ferrer, M.L. Sedation with Propofol plus Paracetamol in External Cephalic Version: An Observational Study. JCM 2022, 11, 489. [Google Scholar] [CrossRef] [PubMed]
- Magro-Malosso, E.R.; Saccone, G.; Di Tommaso, M.; Mele, M.; Berghella, V. Neuraxial Analgesia to Increase the Success Rate of External Cephalic Version: A Systematic Review and Meta-Analysis of Randomized Controlled Trials. Am. J. Obstet. Gynecol. 2016, 215, 276–286. [Google Scholar] [CrossRef]
- Cillard, L.; Verhaeghe, C.; Spiers, A.; Madzou, S.; Descamps, P.; Legendre, G.; Corroenne, R. External Cephalic Version: Predictors for Success. J. Gynecol. Obstet. Hum. Reprod. 2021, 50, 102165. [Google Scholar] [CrossRef] [PubMed]
- Kok, M.; Cnossen, J.; Gravendeel, L.; Van Der Post, J.A.; Mol, B.W. Ultrasound Factors to Predict the Outcome of External Cephalic Version: A Meta-analysis. Ultrasound Obs. Gyne 2009, 33, 76–84. [Google Scholar] [CrossRef]
- Lau, T.K.; Lo, K.W.; Wan, D.; Rogers, M.S. Predictors of Successful External Cephalic Version at Term: A Prospective Study. Br. J. Obstet. Gynaecol. 1997, 104, 798–802. [Google Scholar] [CrossRef]
- Wong, W.M.; Lao, T.T.; Liu, K.L. Predicting the Success of External Cephalic Version with a Scoring System. A Prospective, Two-Phase Study. J. Reprod. Med. 2000, 45, 201–206. [Google Scholar]
- Hutton, E.K.; Simioni, J.C.; Thabane, L. Predictors of Success of External Cephalic Version and Cephalic Presentation at Birth among 1253 Women with Non-Cephalic Presentation Using Logistic Regression and Classification Tree Analyses. Acta Obstet. Gynecol. Scand. 2017, 96, 1012–1020. [Google Scholar] [CrossRef]
- Barbera, A.F.; Pombar, X.; Perugino, G.; Lezotte, D.C.; Hobbins, J.C. A New Method to Assess Fetal Head Descent in Labor with Transperineal Ultrasound. Ultrasound Obs. Gyne 2009, 33, 313–319. [Google Scholar] [CrossRef]
- Youssef, A.; Brunelli, E.; Azzarone, C.; Di Donna, G.; Casadio, P.; Pilu, G. Fetal Head Progression and Regression on Maternal Pushing at Term and Labor Outcome. Ultrasound Obs. Gyne 2021, 58, 105–110. [Google Scholar] [CrossRef]
- Molina, F.S.; Terra, R.; Carrillo, M.P.; Puertas, A.; Nicolaides, K.H. What Is the Most Reliable Ultrasound Parameter for Assessment of Fetal Head Descent? Ultrasound Obs. Gyne 2010, 36, 493–499. [Google Scholar] [CrossRef]
- Usman, S.; Hanidu, A.; Kovalenko, M.; Hassan, W.A.; Lees, C. The Sonopartogram. Am. J. Obstet. Gynecol. 2023, 228, S997–S1016. [Google Scholar] [CrossRef] [PubMed]
- Youssef, A.; Brunelli, E.; Fiorentini, M.; Lenzi, J.; Pilu, G.; El-Balat, A. Breech Progression Angle: New Feasible and Reliable Transperineal Ultrasound Parameter for Assessment of Fetal Breech Descent in Birth Canal. Ultrasound Obs. Gyne 2021, 58, 609–615. [Google Scholar] [CrossRef]
- Fidalgo, A.M.; Aquise, A.; Molina, F.S.; Youssef, A.; González-Vanegas, O.; Brunelli, E.; Cataneo, I.; Segata, M.; Cuerva, M.J.; Rolle, V.; et al. Reproducibility of Breech Progression Angle: Standardization of Transperineal Measurements and Development of Image-Based Checklist for Quality Control. Diagnostics 2025, 15, 1757. [Google Scholar] [CrossRef]
- Sánchez-Romero, J.; Falcón-Araña, L.; Blanco-Carnero, J.E.; García-Ferreira, J.; Herrera-Giménez, J.; Fuentes-García, D.; Araico-Rodríguez, F.; Gallego-Pozuelo, R.M.; Nieto-Díaz, A.; De Paco-Matallana, C. Randomized Clinical Trial of the Use of Propofol as a Sedative Agent versus Spinal Analgesia with Bupivacaine in External Cephalic Version (PropoSpinECV): Study Protocol for a Randomized Clinical Trial. Trials 2025, 26, 398. [Google Scholar] [CrossRef]
- Zweig, M.H.; Campbell, G. Receiver-Operating Characteristic (ROC) Plots: A Fundamental Evaluation Tool in Clinical Medicine. Clin. Chem. 1993, 39, 561–577. [Google Scholar] [CrossRef]
- Ghi, T.; Maroni, E.; Youssef, A.; Morselli-Labate, A.M.; Paccapelo, A.; Montaguti, E.; Rizzo, N.; Pilu, G. Sonographic Pattern of Fetal Head Descent: Relationship with Duration of Active Second Stage of Labor and Occiput Position at Delivery. Ultrasound Obs. Gyne. 2014, 44, 82–89. [Google Scholar] [CrossRef] [PubMed]
- Burgos, J.; Melchor, J.C.; Pijoán, J.I.; Cobos, P.; Fernández-Llebrez, L.; Martínez-Astorquiza, T. A Prospective Study of the Factors Associated with the Success Rate of External Cephalic Version for Breech Presentation at Term. Int. J. Gynecol. Obstet. 2011, 112, 48–51. [Google Scholar] [CrossRef] [PubMed]
- Correia Costa, S.; Raposo, M.I.; Machado, A.P.; Ramalho, C.; Ayres-de-Campos, D.; Montenegro, N. External Cephalic Version: Predictors of Success and Influence on Caesarean Rates. Eur. J. Obstet. Gynecol. Reprod. Biol. 2021, 256, 211–214. [Google Scholar] [CrossRef]
- Dong, T.; Chen, X.; Zhao, B.; Jiang, Y.; Chen, Y.; Lv, M.; Pu, Y.; Chen, G.; Xu, J.; Luo, Q. Development of Prediction Models for Successful External Cephalic Version and Delivery Outcome. Arch. Gynecol. Obstet. 2022, 305, 63–75. [Google Scholar] [CrossRef] [PubMed]
- Velzel, J.; De Hundt, M.; Mulder, F.M.; Molkenboer, J.F.M.; Van Der Post, J.A.M.; Mol, B.W.; Kok, M. Prediction Models for Successful External Cephalic Version: A Systematic Review. Eur. J. Obstet. Gynecol. Reprod. Biol. 2015, 195, 160–167. [Google Scholar] [CrossRef] [PubMed]
- Melo, P.; Georgiou, E.; Hedditch, A.; Ellaway, P.; Impey, L. External Cephalic Version at Term: A Cohort Study of 18 Years’ Experience. BJOG 2019, 126, 493–499. [Google Scholar] [CrossRef] [PubMed]

| Variable | Breech n = 100 | Transverse Lie n = 17 | p |
|---|---|---|---|
| Age (years) | 32.5 (28.6–36.6) | 37.3 (34–41.1) | 0.001 |
| Gestational age at ECV (weeks) | 37.6 (37.1–37.7) | 37.1 (37–37.7) | 0.894 |
| BMI (kg/m2) | 27 (24.3–30.4) | 27.8 (26.8–33.3) | 0.184 |
| Nulliparity | 62 (62%) | 8 (47.1%) | 0.245 |
| Previous CS | 5 (5%) | 2 (11.8%) | 0.277 |
| Estimated Fetal Weight (grams) | 3002 (2782–3188) | 2922 (2839–3092) | 0.818 |
| AF Pocket (mm) | 50 (42–64.5) | 49 (41–65) | 0.919 |
| AF Index (mm) | 154 (125–182) | 155 (137–185) | 0.416 |
| Placenta position | 0.440 | ||
| Anterior | 41 (41%) | 9 (52.9%) | |
| Posterior | 40 (40%) | 7 (41.2%) | |
| Uterine fundus | 6 (6%) | 1 (5.88%) | |
| Lateral wall | 13 (13%) | 0 | |
| Fetal position | <0.001 | ||
| Transverse lie | 0 | 17 (100%) | |
| Frank Breech | 80 (80%) | 0 | |
| Complete breech | 16 (16%) | 0 | |
| Footling breech | 4 (4%) | 0 | |
| Analgesia | 0.032 | ||
| Propofol | 69 (69%) | 16 (94.1%) | |
| Spinal anesthesia | 31 (31%) | 1 (5.88%) | |
| Breech Progression Angle (°) | 87.2 (76.7–95) | 70.2 (54.4–81.5) | <0.001 |
| Variables | Breech | Transverse Lie | ||||||
|---|---|---|---|---|---|---|---|---|
| crudeOR (95%CI) | p | aOR (95%CI) | p | crudeOR (95%CI) | p | aOR (95%CI) | p | |
| Breech Progression Angle (°) | 0.95 (0.92–0.99) | 0.018 | 0.95 (0.91–0.99) | 0.015 | 1.08 (0.97–1.20) | 0.181 | 1.06 (0.94–1.19) | 0.358 |
| Age (years) | 0.99 (0.92–1.07) | 0.828 | 1.32 (0.92–1.89) | 0.126 | ||||
| BMI (kg/m2) | 1.03 (0.93–1.13) | 0.623 | 0.80 (0.57–1.14) | 0.221 | ||||
| Nulliparity | 0.67 (0.27–1.64) | 0.379 | 0.56 (0.01–21.74) | 0.759 | ||||
| Propofol | 1.07 (0.42–2.72) | 0.886 | 1.00 | 1.00 | ||||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Sánchez-Romero, J.; Gallego-Pozuelo, R.M.; Ortuño-Hernández, C.; Martínez-Zarco, A.; Barroso-Linares, R.; Araico-Rodríguez, F.; Blanco-Carnero, J.E.; Nieto-Díaz, A.; de Paco-Matallana, C. Ultrasound Assessment of Breech Engagement: Breech Progression Angle and Prediction of External Cephalic Version Success. J. Clin. Med. 2025, 14, 7179. https://doi.org/10.3390/jcm14207179
Sánchez-Romero J, Gallego-Pozuelo RM, Ortuño-Hernández C, Martínez-Zarco A, Barroso-Linares R, Araico-Rodríguez F, Blanco-Carnero JE, Nieto-Díaz A, de Paco-Matallana C. Ultrasound Assessment of Breech Engagement: Breech Progression Angle and Prediction of External Cephalic Version Success. Journal of Clinical Medicine. 2025; 14(20):7179. https://doi.org/10.3390/jcm14207179
Chicago/Turabian StyleSánchez-Romero, Javier, Rosa María Gallego-Pozuelo, Cristina Ortuño-Hernández, Ana Martínez-Zarco, Rocío Barroso-Linares, Fernando Araico-Rodríguez, José Eliseo Blanco-Carnero, Aníbal Nieto-Díaz, and Catalina de Paco-Matallana. 2025. "Ultrasound Assessment of Breech Engagement: Breech Progression Angle and Prediction of External Cephalic Version Success" Journal of Clinical Medicine 14, no. 20: 7179. https://doi.org/10.3390/jcm14207179
APA StyleSánchez-Romero, J., Gallego-Pozuelo, R. M., Ortuño-Hernández, C., Martínez-Zarco, A., Barroso-Linares, R., Araico-Rodríguez, F., Blanco-Carnero, J. E., Nieto-Díaz, A., & de Paco-Matallana, C. (2025). Ultrasound Assessment of Breech Engagement: Breech Progression Angle and Prediction of External Cephalic Version Success. Journal of Clinical Medicine, 14(20), 7179. https://doi.org/10.3390/jcm14207179







