Surgical Management of Sacroiliac Joint Dislocations and Crescent Fractures: A Nine-Year Clinical Follow-Up
Abstract
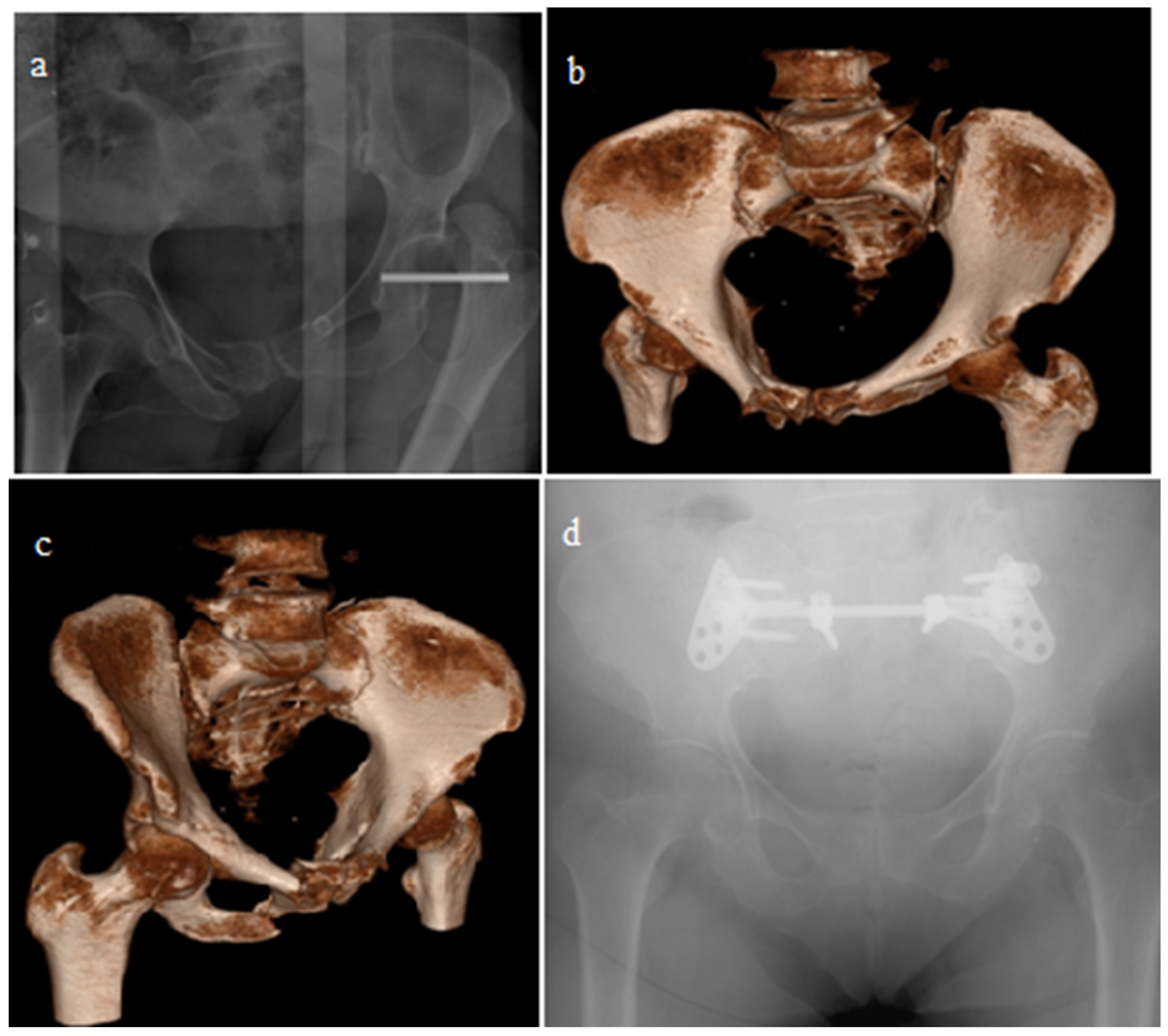
1. Introduction
2. Methods
2.1. Patient Selection
2.2. Evaluation and Treatment of Patients
2.3. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Data Availability Statement
Conflicts of Interest
References
- Köroğlu, M.; Karakaplan, M.; Ergen, E.; Ertem, K.; Çoban, İ.; Köse, H.; Yücel, N.; Bıçakçıoğlu, M.; Özer, A.B.; Özdeş, O.O.; et al. The initial response of a local hospital in the earthquake zone during the 6 February 2023 Kahramanmaraş earthquakes: Injuries and challenges. Acta Orthop. Traumatol. Turc. 2023, 57, 315–321. [Google Scholar] [CrossRef]
- Asik, M.; Basturk, S.; Yazicioglu, O.; Seyhan, F. Fractures of the pelvis: Principles of diagnosis and treatment (new concepts). Acta Orthop. Traumatol. Turc. 1996, 30, 199–205. [Google Scholar]
- Aktas, S.; Sarisaltik, H.; Calpur, O. Pelvis fractures (Consideration of relation between classification and results). Acta Orthop. Traumatol. Turc. 1995, 29, 111–115. [Google Scholar]
- Tile, M. Pelvic fractures: Operative versus nonoperative treatment. Orthop. Clin. North. Am. 1980, 11, 423–464. [Google Scholar] [CrossRef]
- Burgess, A.R.; Eastridge, B.J.; Young, J.W.; Ellison, T.S.; Ellison, P.S., Jr.; Poka, A.; Bathon, G.H.; Brumback, R.J. Pelvic ring disruptions: Effective classification system and treatment protocols. J. Trauma 1990, 30, 848–856. [Google Scholar] [CrossRef]
- Harma, A.; Inan, M.; Ertem, K. Isolated zone III vertical fracture of first sacral vertebra—A case report. Acta Orthop. 2005, 76, 451–452. [Google Scholar] [CrossRef]
- Ansorge, A.; de Foy, M.; Poncet, A.; Gamulin, A. Inter- and intraobserver reliability assessment of the 2018 AO/OTA classification for high-energy pelvic ring injuries: A retrospective study. Orthop. Traumatol. Surg. Res. 2021, 107, 102999. [Google Scholar] [CrossRef]
- Day, A.C.; Kinmont, C.; Bircher, M.D.; Kumar, S. Crescent fracture-dislocation of the sacroiliac joint: A functional classification. J. Bone Joint Surg Br. 2007, 89, 651–658. [Google Scholar] [CrossRef]
- Harma, A.; Inan, M. Acil pelvik eksternal stabilizasyon: Yüksek riskli pelvis kiriklarinda ilk adim [Emergency pelvic external stabilization as the first step treatment in high risk pelvic fractures]. Ulus. Travma Acil Cerrahi Derg. 2004, 10, 115–122. [Google Scholar]
- Harma, A.; Inan, M. Surgical management of transforaminal sacral fractures. Int. Orthop. 2005, 29, 333–337. [Google Scholar] [CrossRef]
- Peng, C.; Yuan, B.; Wang, J.; Liu, H.; Wang, D. Treating sacroiliac joint dislocation through percutaneous sacroiliac screw fixation with the aid of 2 fluoroscopes: A novel technique. Quant Imaging Med Surg. 2021, 11, 2076–2084. [Google Scholar] [CrossRef]
- Chen, W.; Pan, Z.; Chen, J. Biomechanical research on anterior double-plate fixation for vertically unstable sacroiliac dislocations. Orthop Surg. 2009, 1, 127–131. [Google Scholar] [CrossRef]
- Wu, T.; Su, K.; Zhang, Y.Z.; Yang, Z.Y.; Li, H.J.; Han, Y.T. Biomechanical comparison of three kinds of fixation in fracture-dislocation of the sacroiliac joint. Technol. Health Care 2019, 27, 89–99. [Google Scholar] [CrossRef]
- Menon, K.V.; Suresh, S.S.; Kalyanasundaram, S.; Varughese, J. Crescent fractures of the pelvis treated by open reduction and internal fixation: A critique of Day’s guidelines. Eur. J. Orthop. Surg. Traumatol. 2017, 27, 1089–1095. [Google Scholar] [CrossRef]
- Ye, K.; Tang, J.; Shen, L.; An, Z. Open reduction and internal fixation of crescent fracture-dislocation: Anterior or posterior approach? Arch. Orthop. Trauma Surg. 2024, 144, 1269–1279. [Google Scholar] [CrossRef]
- Zong, Z.; Chen, S.; Jia, M.; Shen, Y.; Hua, X.; Liu, D. Posterior iliac crescent fracture-dislocation: Is it only rotationally unstable? Orthopedics 2014, 37, e435–e440. [Google Scholar] [CrossRef]
- Li, M.; Huang, D.; Yan, H.; Li, H.; Wang, L.; Dong, J. Cannulated iliac screw fixation combined with reconstruction plate fixation for Day type II crescent pelvic fractures. J. Int. Med. Res. 2020, 48, 0300060519896120. [Google Scholar]
- Calafi, L.A.; Routt, M.L. Posterior iliac crescent fracture-dislocation: What morphological variations are amenable to iliosacral screw fixation? Injury 2013, 44, 194–198. [Google Scholar] [CrossRef]
- Griffin, D.R.; Starr, A.J.; Reinert, C.M.; Jones, A.L.; Whitlock, S. Vertically unstable pelvic fractures fixed with percutaneous iliosacral screws: Does posterior injury pattern predict fixation failure? J. Orthop. Trauma 2003, 17, 399–405. [Google Scholar]
- Mardanpour, K.; Rahbar, M. The outcome of surgically treated traumatic unstable pelvic fractures by open reduction and internal fixation. J. Inj. Violence Res. 2013, 5, 77. [Google Scholar] [CrossRef]
- Jatoi, A.; Sahito, B.; Kumar, D.; Rajput, N.H.; Ali, M. Fixation of Crescent Pelvic Fracture in a Tertiary Care Hospital: A Steep Learning Curve. Cureus 2019, 11, e5614. [Google Scholar] [CrossRef]
- Fan, X.H.; Zhen, P.; Gao, M.X.; Wang, J.J.; Xue, Y.; Li, M.; Deng, X.W.; Li, X.S. Characteristics of treating dislocation and fracture of sacroiliac joint through anterior and posterior approches. Zhongguo Gu Shang 2013, 26, 1048–1051. [Google Scholar]
- Li, C.L. Clinical comparative analysis on unstable pelvic fractures in the treatment with percutaneous sacroiliac screws and sacroiliac joint anterior plate fixation. Eur. Rev. Med. Pharmacol. Sci. 2014, 18, 2704–2708. [Google Scholar]
- Zhang, R.; Yin, Y.; Li, S.; Hou, Z.; Jin, L.; Zhang, Y. Percutaneous sacroiliac screw versus anterior plating for sacroiliac joint disruption: A retrospective cohort study. Int. J. Surg. 2018, 50, 11–16. [Google Scholar] [CrossRef]
- Shui, X.; Ying, X.; Mao, C.; Feng, Y.; Chen, L.; Kong, J.; Guo, X.; Wang, G. Percutaneous Screw Fixation of Crescent Fracture-Dislocation of the Sacroiliac Joint. Orthopedics 2015, 38, e976–e982. [Google Scholar] [CrossRef]
- Gu, R.; Huang, W.; Yang, L.; Liu, H.; Xie, K.; Huang, Z. Comparisons of front plate, percutaneous sacroiliac screws, and sacroiliac anterior papilionaceous plate in fixation of unstable pelvic fractures. Medicine 2017, 96, e7775. [Google Scholar] [CrossRef]
- Khaled, S.A.; Soliman, O.; Wahed, M.A. Functional outcome of unstable pelvic ring injuries after iliosacral screw fixation: Single versus two screw fixation. Eur. J. Trauma Emerg. Surg. 2015, 41, 387–392. [Google Scholar]
- Routt, M.L.C. Iliosacral screw fixation: Early complications of the percutaneous technique. J. Orthop. Trauma 1997, 11, 584–589. [Google Scholar] [CrossRef]
- Andrés-Peiró, J.V.; Piedra-Calle, C.A.; Blasco-Casado, F.; García-Albó, E.; Tomàs-Hernández, J.; Selga-Marsà, J.; García-Sánchez, Y.; de Delás-Vigo, M.D.A.; Teixidor-Serra, J. Insertion of S1 iliosacral screws in the computed tomography room: An alternative to improve safety in the percutaneous management of posterior pelvic ring injuries. Rev. Esp. Cir. Ortop. Traumatol. 2024, 68, T253–T261. [Google Scholar] [CrossRef]
- Collinge, C.; Coons, D.; Aschenbrenner, J. Risks to the superior gluteal neurovascular bundle during percutaneous iliosacral screw insertion: An anatomical cadaver study. J. Orthop. Trauma 2005, 19, 96–101. [Google Scholar] [CrossRef]
- Bousbaa, H.; Ouahidi, M.; Louaste, J.; Bennani, M.; Cherrad, T.; Jezzari, H.; Kasmaoui, E.H. Percutaneous iliosacral screw fixation in unstable pelvic fractures. Pan Afr. Med. J. 2017, 27, 244. [Google Scholar]
- Javidmehr, S.; Golbakhsh, M.R.; Siavashi, B.; Talebian, P.; Dehnokhalaji, M.; Zehtab, M.J.; Bozorgmanesh, M. A New Modified Method for Inserting Iliosacral Screw versus the Conventional Method. Asian Spine J. 2018, 12, 119–125. [Google Scholar] [CrossRef]
- Tang, C.H.; Yao, G.W.; Wang, L.; Tu, H.L.; Luo, W. Minimally invasive internal fixation of pelvic ring for type C pelvic fracture. Zhongguo Gu Shang 2017, 30, 660–663. [Google Scholar] [PubMed]
- Peng, K.T.; Li, Y.Y.; Hsu, W.H.; Yang, J.T.; Hsu, C.H.; Huang, T.J. Intraoperative computed tomography with integrated navigation in percutaneous iliosacral screwing. Injury 2013, 44, 203–208. [Google Scholar] [CrossRef] [PubMed]
- Solyom, A.; Moldovan, F.; Moldovan, L.; Strnad, G.; Fodor, P. Clinical Workflow Algorithm for Preoperative Planning, Reduction and Stabilization of Complex Acetabular Fractures with the Support of Three-Dimensional Technologies. J. Clin. Med. 2024, 13, 3891. [Google Scholar] [CrossRef] [PubMed]
- Wu, X.B.; Wang, J.Q.; Zhao, C.P.; Sun, X.; Shi, Y.; Zhang, Z.A.; Li, Y.N.; Wang, M.Y. Printed three-dimensional anatomic templates for virtual preoperative planning before reconstruction of old pelvic injuries: Initial results. Chin. Med. J. 2015, 128, 477–482. [Google Scholar]
- Wu, K.; Bai, X.; Li, S. A new individually designed 3D printing guide plate-assisted internal fixator (INFIX) surgery for the treatment of pelvic fractures. J. Orthop. Surg. Res. 2025, 20, 770. [Google Scholar] [CrossRef]



| Pain at Rest Pain with Activity Limping | None | Mild | Moderate | Severe | Continually |
|---|---|---|---|---|---|
| Score | 1 | 2 | 3 | 4 | 5 |
| Treatment satisfaction | Very satisfied | Satisfied | Satisfied, sometimes restrictive | Not satisfied, no activity restrictions | Not satisfied, have activity restrictions |
| Score | 1 | 2 | 3 | 4 | 5 |
| n | % | |
|---|---|---|
| Gender | ||
| Male | 74 | 67.3 |
| Female | 36 | 32.7 |
| Etiology of Injury | ||
| In-vehicle traffic accident | 39 | 33.45 |
| Non-vehicle traffic accident | 31 | 28.2 |
| Fall from a height | 22 | 20 |
| Other | 18 | 16.4 |
| Additional orthopedic injury | ||
| Positive | 53 | 48.2 |
| None | 57 | 51.8 |
| Additional injuries | ||
| Positive | 45 | 40.9 |
| None | 65 | 59.1 |
| Fracture Classification (OTA) | ||
| B1 | 3 | 27 |
| B2 | 56 | 50.9 |
| B3 | 11 | 10 |
| C1 | 21 | 19.1 |
| C2 | 10 | 9.1 |
| C3 | 9 | 8.2 |
| Sacroiliac joint surgery | ||
| Closed reduction + ISS | 59 | 48.7 |
| Open reduction + Anterior PS | 36 | 29.75 |
| Open reduction + Posterior PS | 15 | 12.4 |
| Open reduction + ISS | 11 | 9.1 |
| Complications | 13 | 11.8 |
| Wound infection | ||
| Superficial | 3 | 2.7 |
| Deep | 2 | 1.8 |
| Neurological deficit | 7 | 6.36 |
| Reflex sympathetic dystrophy | 1 | 0.9 |
| Open Reduction + PS n = 51 | Closed Reduction + ISS n = 59 | Open Reduction + ISS n = 11 | p Value | |
|---|---|---|---|---|
| Excellent | 24 (47.06%) | 25 (42.37%) | 8 (72.7%) | 0.204 |
| Good/Fair/Poor | 27(52.94%) | 34 (57.63%) | 3 (27.3%) |
| Excellent | Good | Fair/Poor | p Value | |
|---|---|---|---|---|
| Open reduction+ PS Anterior approach (n = 36) | 19 (52.8%) | 14 (38.9%) | 3 (8.3%) | 0.204 |
| Open reduction +PS Posterior approach (n = 15) | 5 (33.3%) | 8 (53.3%) | 2 (13.3%) | |
| Open reduction+ PS Anterior approach (n = 36) | 19 (52.8%) | 14 (38.9%) | 3 (8.3%) | 0.135 |
| Closed reduction +ISS (n = 59) | 25 (42.4%) | 24 (40.7%) | 10 (16.95%) | |
| Open reduction +PS Posterior approach (n = 15) | 5 (33.3%) | 8 (53.3%) | 2 (13.3%) | 0.880 |
| Closed reduction +ISS (n = 59) | 25 (42.4%) | 24 (40.7%) | 10 (16.95%) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Özdeş, H.U.; Köroğlu, M.; Çoban, İ.; Harma, A.; Aslantürk, O. Surgical Management of Sacroiliac Joint Dislocations and Crescent Fractures: A Nine-Year Clinical Follow-Up. J. Clin. Med. 2025, 14, 7139. https://doi.org/10.3390/jcm14207139
Özdeş HU, Köroğlu M, Çoban İ, Harma A, Aslantürk O. Surgical Management of Sacroiliac Joint Dislocations and Crescent Fractures: A Nine-Year Clinical Follow-Up. Journal of Clinical Medicine. 2025; 14(20):7139. https://doi.org/10.3390/jcm14207139
Chicago/Turabian StyleÖzdeş, Hüseyin Utku, Muhammed Köroğlu, İdris Çoban, Ahmet Harma, and Okan Aslantürk. 2025. "Surgical Management of Sacroiliac Joint Dislocations and Crescent Fractures: A Nine-Year Clinical Follow-Up" Journal of Clinical Medicine 14, no. 20: 7139. https://doi.org/10.3390/jcm14207139
APA StyleÖzdeş, H. U., Köroğlu, M., Çoban, İ., Harma, A., & Aslantürk, O. (2025). Surgical Management of Sacroiliac Joint Dislocations and Crescent Fractures: A Nine-Year Clinical Follow-Up. Journal of Clinical Medicine, 14(20), 7139. https://doi.org/10.3390/jcm14207139






