Emerging Healthcare Trends in Prosthetic Treatment of Hand Osteoarthritis
Abstract
1. Introduction
2. Materials and Methods
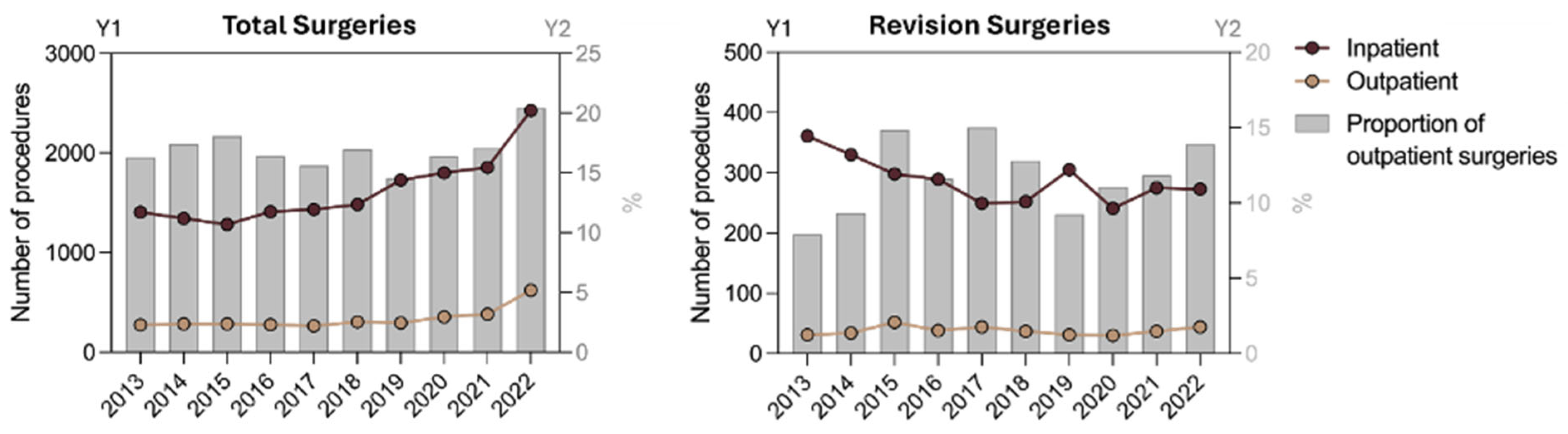
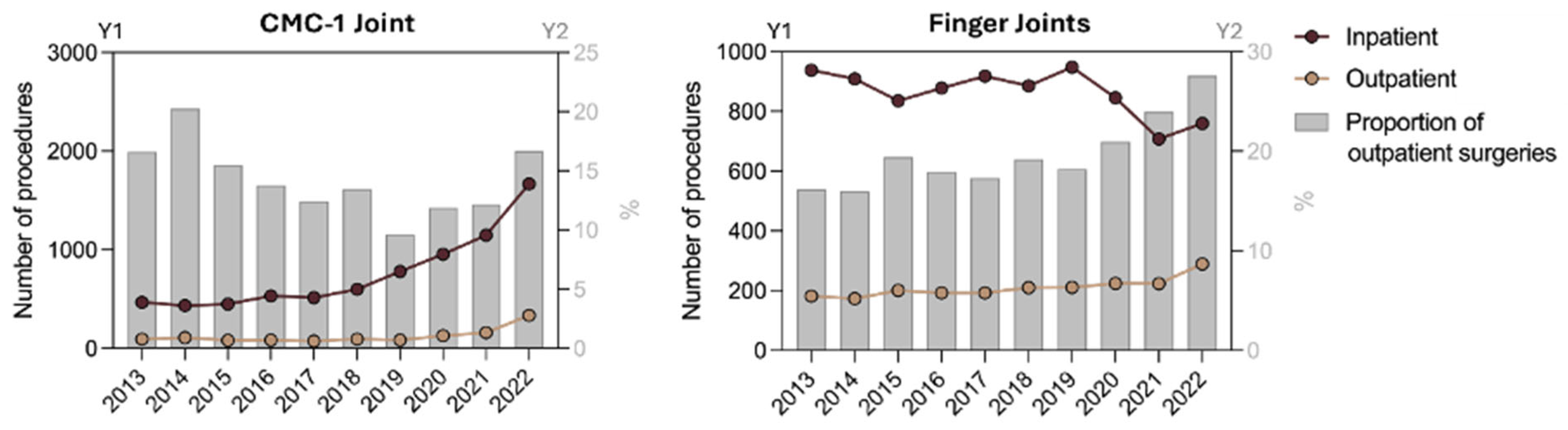
3. Results
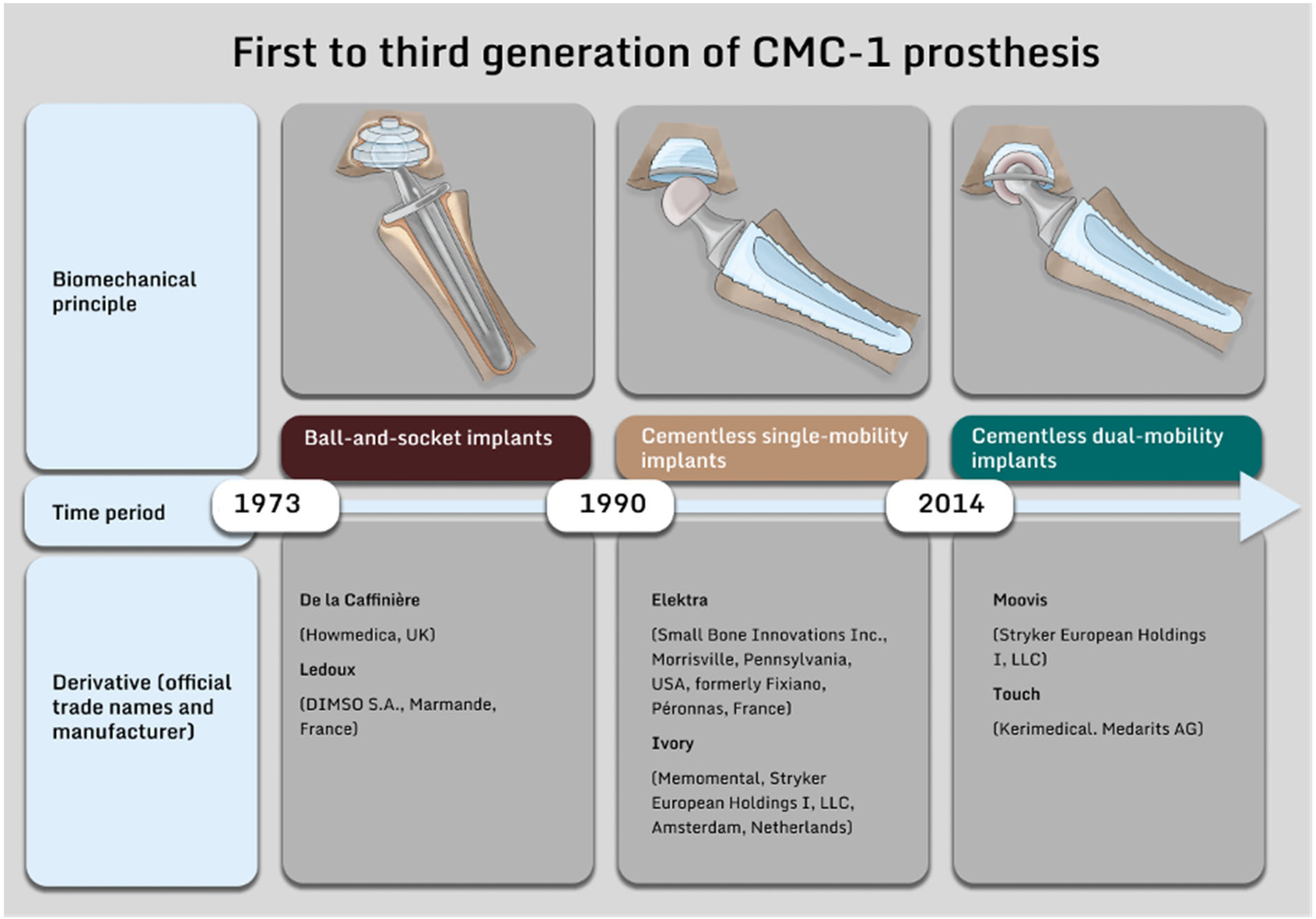
4. Discussion
Increase in Procedures and Shift Towards Outpatient Care
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Krakowski, P.; Krakowski, P.; Rejniak, A.; Rejniak, A.; Sobczyk, J.; Sobczyk, J.; Karpiński, R.; Karpiński, R. Cartilage Integrity: A Review of Mechanical and Frictional Properties and Repair Approaches in Osteoarthritis. Healthcare 2024, 12, 1648. [Google Scholar] [CrossRef]
- Long, H.; Liu, Q.; Yin, H.; Wang, K.; Diao, N.; Zhang, Y.; Lin, J.; Guo, A. Prevalence Trends of Site-Specific Osteoarthritis from 1990 to 2019: Findings from the Global Burden of Disease Study 2019. Arthritis Rheumatol. 2022, 74, 1172–1183. [Google Scholar] [CrossRef]
- Cibere, J.; Sayre, E.; Guermazi, A.; Nicolaou, S.; Kopec, J.; Esdaile, J.; Thorne, A.; Singer, J.; Wong, H. Natural history of cartilage damage and osteoarthritis progression on magnetic resonance imaging in a population-based cohort with knee pain. Osteoarthr. Cartil. 2011, 19, 683–688. [Google Scholar] [CrossRef] [PubMed]
- Johnson, V.L.; Hunter, D.J. The epidemiology of osteoarthritis. Best Pract. Res. Clin. Rheumatol. 2014, 28, 5–15. [Google Scholar] [CrossRef] [PubMed]
- Machrowska, A.; Karpiński, R.; Maciejewski, M.; Jonak, J.; Krakowski, P.; Syta, A. Application of Recurrence Quantification Analysis in the Detection of Osteoarthritis of the Knee with the Use of Vibroarthrography. Adv. Sci. Technol. Res. J. 2024, 18, 19–31. [Google Scholar] [CrossRef]
- Pickrell, B.B.; Eberlin, K.R. Thumb Basal Joint Arthritis. Clin. Plast. Surg. 2019, 46, 407–413. [Google Scholar] [CrossRef]
- Sharma, L. Osteoarthritis of the Knee. N. Engl. J. Med. 2021, 384, 51–59. [Google Scholar] [CrossRef]
- Yao, Q.; Wu, X.; Tao, C.; Gong, W.; Chen, M.; Qu, M.; Zhong, Y.; He, T.; Chen, S.; Xiao, G. Osteoarthritis: Pathogenic signaling pathways and therapeutic targets. Signal Transduct. Target. Ther. 2023, 8, 56. [Google Scholar] [CrossRef]
- Srnec, J.J.; Wagner, E.R.; Rizzo, M. Implant Arthroplasty for Proximal Interphalangeal, Metacarpophalangeal, and Trapeziometacarpal Joint Degeneration. J. Hand Surg. 2017, 42, 817–825. [Google Scholar] [CrossRef]
- Klein, S.M.; Breindl, G.; Koller, M.; Mielenz, M.; Roll, C.; Kinner, B.; Prantl, L. Midterm results after modified Epping procedure for trapeziometacarpal osteoarthritis. Arch. Orthop. Trauma Surg. 2013, 133, 1163–1171. [Google Scholar] [CrossRef]
- Klein, S.M.; Wachter, K.; Koller, M.; Vykoukal, J.; Geis, S.; Dolderer, J.H.; Loibl, M.; Prantl, L. Long-term results after modified Epping procedure for trapeziometacarpal osteoarthritis. Arch. Orthop. Trauma Surg. 2015, 135, 1475–1484. [Google Scholar] [CrossRef] [PubMed]
- Farkash, U.; Sakhnini, M.; Dreyfuss, D.; Tordjman, D.; Rotem, G.; Luria, S. Failure Rate and Early Complications of Thumb Carpometacarpal Joint Replacement—A Multicenter Retrospective Study of Two Modern Implant Designs. J. Clin. Med. 2023, 13, 121. [Google Scholar] [CrossRef] [PubMed]
- Herren, D.B.; Beaulieu, J.-Y.; Calcagni, M.; Erling, C.; Jung, M.; Kaulich, A.; Mühldorfer-Fodor, M.; Papaloïzos, M.; Rosenkranz, A.; Vögelin, E.; et al. Current Trends in the Implantation of the Touch Prosthesis at the Thumb Carpometacarpal Joint: Results of the 1st German-Speaking User Meeting. Handchir. Mikrochir. Plast. Chir. 2024, 56, 201–211. [Google Scholar] [CrossRef]
- Raj, S.; Clay, R.; Ramji, S.; Shaunak, R.; Dadrewalla, A.; Sinha, V.; Shaunak, S. Trapeziectomy versus joint replacement for first carpometacarpal (CMC 1) joint osteoarthritis: A systematic review and meta-analysis. Eur. J. Orthop. Surg. Traumatol. 2022, 32, 1001–1021. [Google Scholar] [CrossRef]
- Weißer, M.; Rosery, H.; Schönfelder, T. Health Economic Aspects. In White Paper on Joint Replacement; Bleß, H.-H., Kip, M., Eds.; Springer: Berlin/Heidelberg, Germany, 2018; pp. 105–119. [Google Scholar] [CrossRef]
- Duerinckx, J.; Verstreken, F. Total joint replacement for osteoarthritis of the carpometacarpal joint of the thumb: Why and how? EFORT Open Rev. 2022, 7, 349–355. [Google Scholar] [CrossRef] [PubMed]
- Patel, N.P.; Elali, F.; Coban, D.; Changoor, S.; Shah, N.V.; Sinha, K.; Hwang, K.; Faloon, M.; Paulino, C.B.; Emami, A. The 5-factor modified Frailty Index (mFI-5) predicts adverse outcomes after elective Anterior Lumbar Interbody Fusion (ALIF). N. Am. Spine Soc. J. 2023, 13, 100189. [Google Scholar] [CrossRef] [PubMed]
- Classen, S. Ambulantisierung—Über den Tellerrand hinaus gedacht—Chancen und Risiken in Hinblick auf die knappen Ressourcen: Mensch—Umwelt—Energie. Gefasschirurgie 2023, 28, 127–130. [Google Scholar] [CrossRef]
- Tillmanns, H.; Jäckel, D. Entwicklung der Ambulantisierung. In Krankenhaus-Report 2024; Klauber, J., Wasem, J., Beivers, A., Mostert, C., Scheller-Kreinsen, D., Eds.; Springer: Berlin/Heidelberg, Germany, 2024; pp. 225–268. [Google Scholar] [CrossRef]
- Nyszkiewicz, R.; Becker, K.; Engelhardt, T.O.; Hakimi, M.; Lautenbach, M.; Millrose, M.; Mühldorfer-Fodor, M.; Obladen, A.; van Schoonhoven, J. Konsensusempfehlung—Empfehlungen der Deutschen Gesellschaft für Handchirurgie zur ambulanten Leistungserbringung handchirurgischer Operationen. Handchir. Mikrochir. Plast. Chir. 2020, 52, 244–248. [Google Scholar] [CrossRef]
- Dengler, R.; Kron, F. Ambulantisierung und Vergütungssystematik im deutschen Gesundheitssystem: Eine Bestandaufnahme und kritische Analyse der aktuellen Reformvorhaben der Bundesregierung. In Wege zum neuen Gesundheitssystem—“Change by Design” oder “Change by Disaster”? Cassens, M., Städter, T., Eds.; Springer: Wiesbaden, Germany, 2023; pp. 129–146. [Google Scholar] [CrossRef]
- Nisar, A.; Shah, Z.; Pendse, A.; Chakrabarti, I. Day Case Total Joint Arthroplasty in the Hand: Results in a District General Hospital. J. Hand Surg. 2009, 34, 367–370. [Google Scholar] [CrossRef]
- Buta, M.G. The unseen face of resource rationalization in medical practice. Med. Pharm. Rep. 2024, 97, 99–103. [Google Scholar] [CrossRef]
- Billig, J.I.; Nasser, J.S.; Chung, K.C. National Prevalence of Complications and Cost of Small Joint Arthroplasty for Hand Osteoarthritis and Post-Traumatic Arthritis. J. Hand Surg. 2020, 45, 553.e1–553.e12. [Google Scholar] [CrossRef] [PubMed]
- Wachtl, S.W.; Guggenheim, P.R.; Sennwald, G.R. Cemented and non-cemented replacements of the trapeziometacarpal joint. J. Bone Jt. Surgery. Br. Vol. 1998, 80, 121–125. [Google Scholar] [CrossRef]
- Tchurukdichian, A.; Guillier, D.; Moris, V.; See, L.-A.; Macheboeuf, Y. Results of 110 IVORY® prostheses for trapeziometacarpal osteoarthritis with a minimum follow-up of 10 years. J. Hand Surg. 2020, 45, 458–464. [Google Scholar] [CrossRef]
- Tchurukdichian, A.; Gerenton, B.; Moris, V.; See, L.-A.; Stivala, A.; Guillier, D. Outcomes of Double-Mobility Prosthesis in Trapeziometacarpal Joint Arthritis with a Minimal 3 Years of Follow-Up: An Advantage for Implant Stability. HAND 2021, 16, 368–374. [Google Scholar] [CrossRef] [PubMed]
- Liukkonen, R.; Karjalainen, V.-L.; Kvist, R.; Vaajala, M.; Ponkilainen, V.; Karjalainen, T. Total joint arthroplasty for thumb carpometacarpal joint osteoarthritis: A systematic review and meta-analysis of randomized controlled trials. Acta Orthop. 2024, 95, 325–332. [Google Scholar] [CrossRef] [PubMed]
- Borgers, A.; Verstreken, A.; Vanhees, M.; Verstreken, F. Primary endoprosthetic replacement of the arthritic CMC-1 joint. Oper. Orthopadie Traumatol. 2021, 33, 228–244. [Google Scholar] [CrossRef]
- Erne, H.; Scheiber, C.; Schmauss, D.; Loew, S.; Cerny, M.; Ehrl, D.; Schmauss, V.; Machens, H.-G.; Muhl, P. Total Endoprosthesis Versus Lundborg´s Resection Arthroplasty for the Treatment of Trapeziometacarpal Joint Osteoarthritis. Plast. Reconstr. Surg. Glob. Open 2018, 6, e1737. [Google Scholar] [CrossRef]
- Chung, K.C.; Pushman, A.G. Current Concepts in the Management of the Rheumatoid Hand. J. Hand Surg. 2011, 36, 736–747. [Google Scholar] [CrossRef]

| OPS-Codes | OPS Group |
|---|---|
| 5-824.a | Thumb carpometacarpal joint prosthesis |
| 5-824.9 | Finger joint prosthesis |
| 5-824.90 | 1 finger joint prosthesis |
| 5-824.91 | 2 finger joint prostheses |
| 5-824.92 | 3 finger joint prostheses |
| 5-824.93 | 4 finger joint prostheses |
| 5-825.c | Removal of a finger joint prosthesis |
| 5-825.d | Replacement of a thumb carpometacarpal joint prosthesis |
| 5-825.e | Removal of a thumb carpometacarpal joint prosthesis |
| 5-825.6 | Replacement of a finger joint prosthesis |
| Total n | Outpatient (%) | Inpatient (%) | p | ||
|---|---|---|---|---|---|
| Number of procedures | 22,752 | 3715 (16.3) | 19,037 (83.7) | <0.001 | |
| Prosthesis implantation | All | 19,501 | 3337 (17.1) | 16,164 (82.8) | <0.001 |
| CMC-1 | 8782 | 1241 (14.1) | 7541 (85.7) | <0.001 | |
| Finger | 10,719 | 2096 (19.6) | 8623 (80.4) | <0.001 | |
| Revision surgeries | 3251 | 378 (11.6) | 2873 (88.4) | <0.001 | |
| All | IR | IRR | 95% CI | p | ||
|---|---|---|---|---|---|---|
| Year | 2013 | 2022 | ||||
| Number of procedures | 2.56 | 3.99 | 1.56 | 1.47 to 1.64 | <0.001 | |
| Prostheses | All | 2.08 | 3.61 | 1.74 | 1.64 to 1.85 | <0.001 |
| CMC-1 | 0.69 | 2.37 | 3.42 | 3.12 to 3.76 | <0.001 | |
| Finger | 1.39 | 1.24 | 0.90 | 0.82 to 0.98 | 0.0111 | |
| Revisions | 0.49 | 0.38 | 0.77 | 0.67 to 0.90 | <0.001 | |
| Outpatient | IR | IRR | 95% CI | p | ||
| Year | 2013 | 2022 | ||||
| Number of procedures | 0.38 | 0.79 | 2.09 | 1.83 to 2.40 | <0.001 | |
| Prostheses | All | 0.34 | 0.74 | 2.18 | 1.89 to 2.51 | <0.001 |
| CMC-1 | 0.12 | 0.40 | 3.44 | 2.73 to 4.33 | <0.001 | |
| Finger | 0.22 | 0.34 | 1.53 | 1.27 to 1.84 | <0.001 | |
| Revisions | 0.04 | 0.05 | 1.36 | 0.86 to 2.15 | 0.1892 | |
| Inpatient | IR | IRR | 95% CI | p | ||
| Year | 2013 | 2022 | ||||
| Number of procedures | 2.19 | 3.20 | 1.46 | 1.38 to 1.55 | <0.001 | |
| Protheses | All | 1.74 | 2.88 | 1.65 | 1.55 to 1.77 | <0.001 |
| CMC-1 | 0.58 | 1.98 | 3.42 | 3.08 to 3.79 | <0.001 | |
| Finger | 1.16 | 0.90 | 0.77 | 0.70 to 0.85 | <0.001 | |
| Revisions | 0.45 | 0.32 | 0.72 | 0.62 to 0.85 | <0.001 | |
| All | IR 1 and AAIR | IRR | 95% CI | p | ||
|---|---|---|---|---|---|---|
| 2013 | 2022 | |||||
| Finger prostheses | All | 1.39 1 | 1.24 1 | 0.90 | 0.82 to 0.98 | 0.0111 |
| 40–59 | 1.18 | 1.15 | 0.98 | 0.83 to 1.15 | 0.7853 | |
| 60–79 | 4.35 | 3.50 | 0.81 | 0.73 to 0.89 | <0.001 | |
| Outpatient | IR 1 and AAIR | IRR | 95% CI | p | ||
| 2013 | 2022 | |||||
| Finger prostheses | All | 0.22 1 | 0.34 1 | 1.53 | 1.27 to 1.84 | <0.001 |
| 40–59 | 0.16 | 0.29 | 1.82 | 1.23 to 2.71 | 0.0026 | |
| 60–79 | 0.75 | 1.01 | 1.35 | 1.08 to 1.69 | 0.0076 | |
| Inpatient | IR 1 and AAIR | IRR | 95% CI | p | ||
| 2013 | 2022 | |||||
| Finger prostheses | All | 1.16 1 | 0.90 1 | 0.77 | 0.70 to 0.85 | <0.001 |
| 40–59 | 1.02 | 0.87 | 0.85 | 0.70 to 1.02 | 0.0791 | |
| 60–79 | 3.60 | 2.49 | 0.69 | 0.61 to 0.78 | <0.001 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Siegmund, A.M.; Ruewe, M.; Szymski, D.; Loucas, R.; Oliinyk, D.; Pagani, A.; Ecklmaier, C.; Geis, S.; Anker, A.M.; Prantl, L.; et al. Emerging Healthcare Trends in Prosthetic Treatment of Hand Osteoarthritis. J. Clin. Med. 2025, 14, 573. https://doi.org/10.3390/jcm14020573
Siegmund AM, Ruewe M, Szymski D, Loucas R, Oliinyk D, Pagani A, Ecklmaier C, Geis S, Anker AM, Prantl L, et al. Emerging Healthcare Trends in Prosthetic Treatment of Hand Osteoarthritis. Journal of Clinical Medicine. 2025; 14(2):573. https://doi.org/10.3390/jcm14020573
Chicago/Turabian StyleSiegmund, Andreas M., Marc Ruewe, Dominik Szymski, Rafael Loucas, Dmytro Oliinyk, Andrea Pagani, Cassandra Ecklmaier, Sebastian Geis, Alexandra M. Anker, Lukas Prantl, and et al. 2025. "Emerging Healthcare Trends in Prosthetic Treatment of Hand Osteoarthritis" Journal of Clinical Medicine 14, no. 2: 573. https://doi.org/10.3390/jcm14020573
APA StyleSiegmund, A. M., Ruewe, M., Szymski, D., Loucas, R., Oliinyk, D., Pagani, A., Ecklmaier, C., Geis, S., Anker, A. M., Prantl, L., & Klein, S. M. (2025). Emerging Healthcare Trends in Prosthetic Treatment of Hand Osteoarthritis. Journal of Clinical Medicine, 14(2), 573. https://doi.org/10.3390/jcm14020573









