Deep Learning in Scaphoid Nonunion Treatment
Abstract
1. Introduction
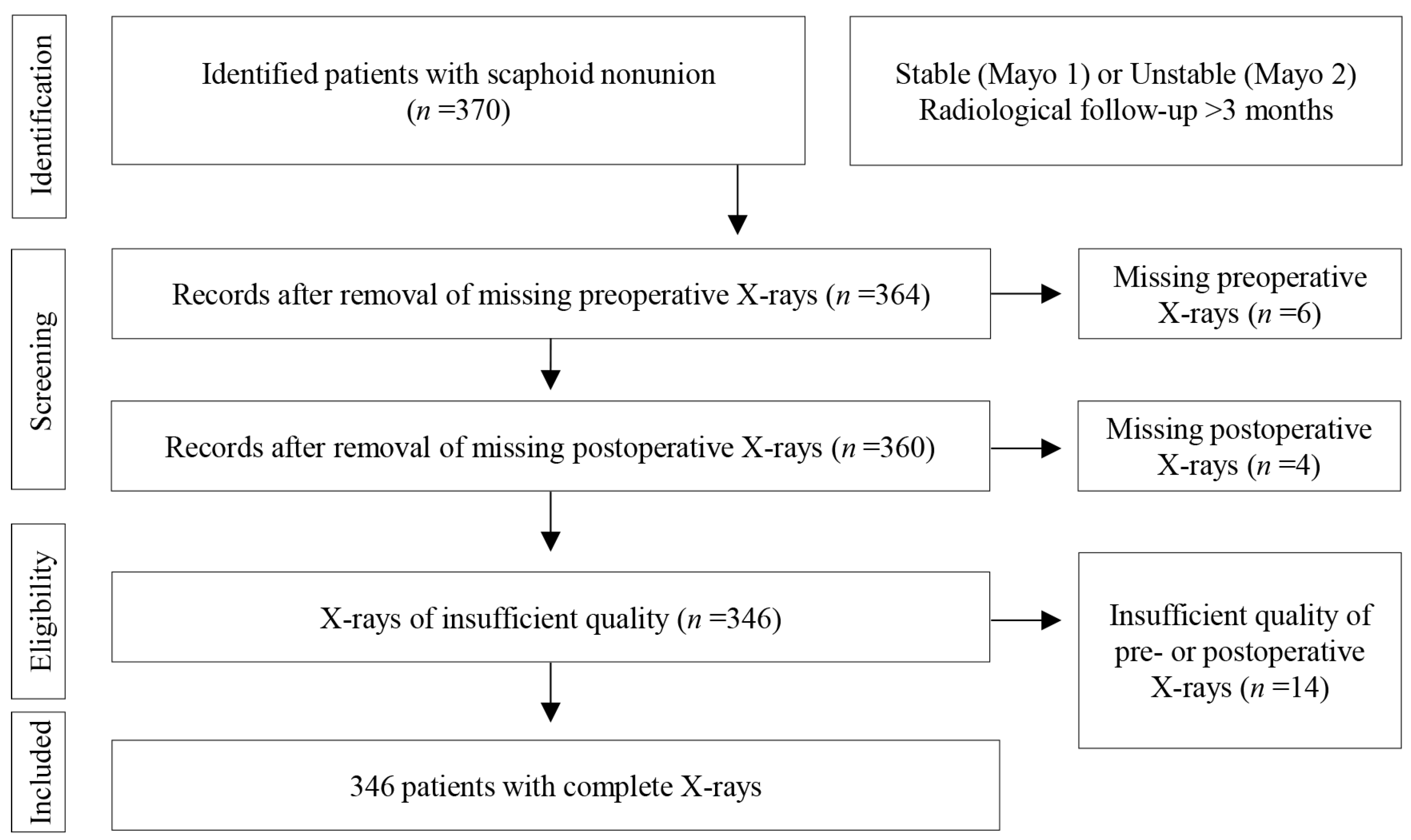
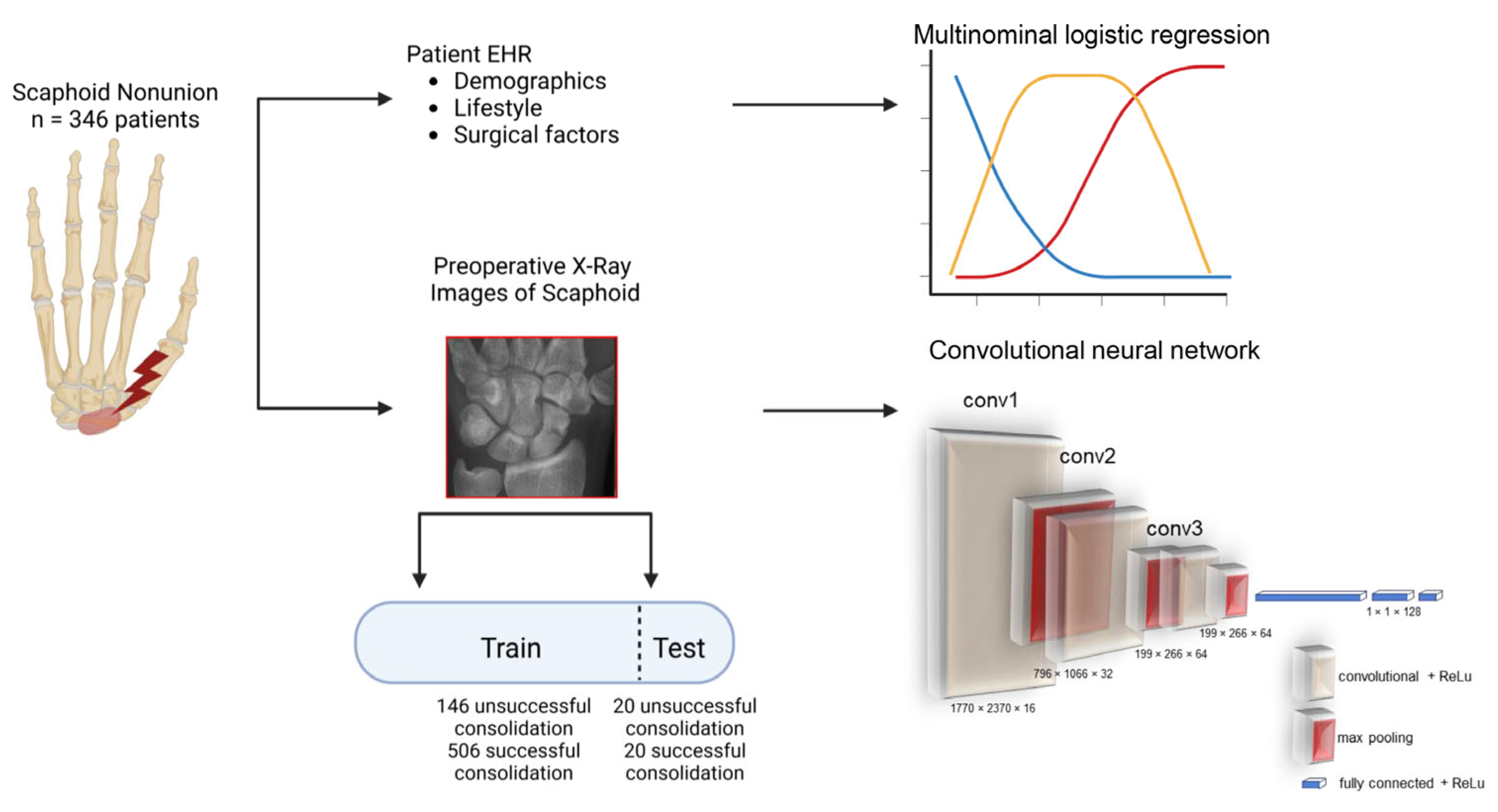
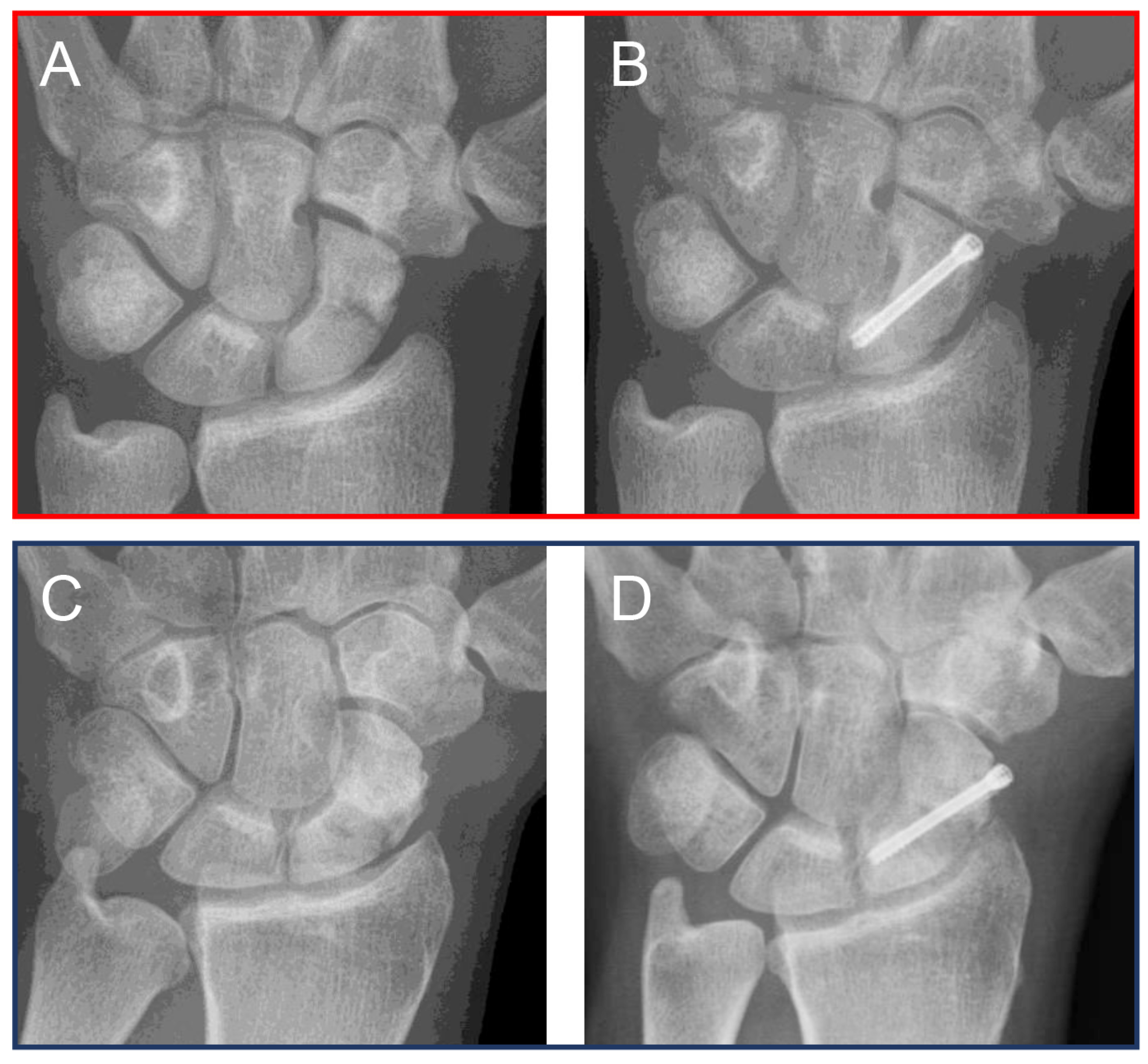
2. Materials and Methods
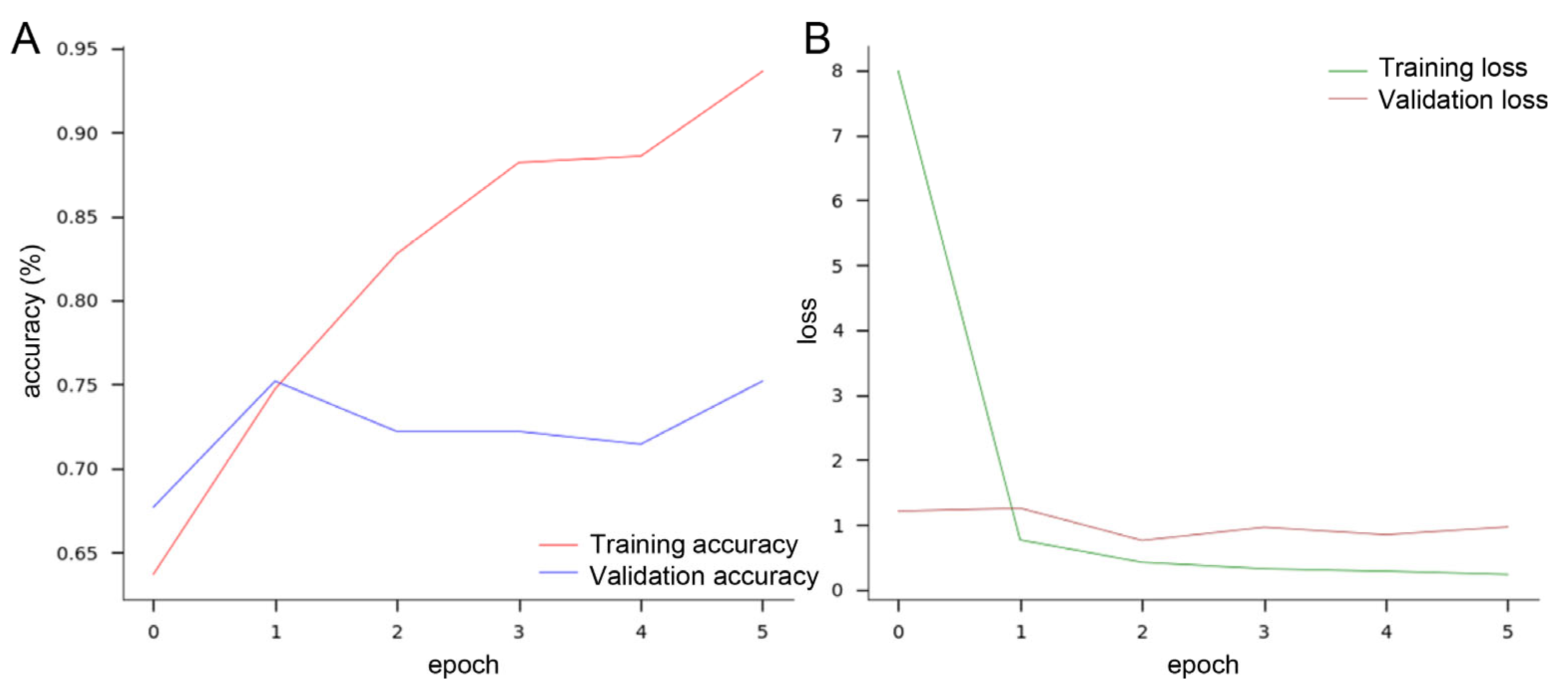
3. Results
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Gray, R.R.L.; Halpern, A.L.; King, S.R.; Anderson, J.E. Scaphoid fracture and nonunion: New directions. J. Hand Surg. Eur. Vol. 2023, 48, 4S–10S. [Google Scholar] [CrossRef] [PubMed]
- Orji, C.; Reghefaoui, M.; Saavedra Palacios, M.S.; Thota, P.; Peresuodei, T.S.; Gill, A.; Hamid, P. Application of Artificial Intelligence and Machine Learning in Diagnosing Scaphoid Fractures: A Systematic Review. Cureus 2023, 15, e47732. [Google Scholar] [CrossRef] [PubMed]
- Wells, M.E.; Nicholson, T.C.; Macias, R.A.; Nesti, L.J.; Dunn, J.C. Incidence of Scaphoid Fractures and Associated Injuries at US Trauma Centers. J. Wrist Surg. 2021, 10, 123–128. [Google Scholar] [CrossRef] [PubMed]
- Duckworth, A.D.; Jenkins, P.J.; Aitken, S.A.; Clement, N.D.; Court-Brown, C.M.; McQueen, M.M. Scaphoid fracture epidemiology. J. Trauma Acute Care Surg. 2012, 72, E41–E45. [Google Scholar] [CrossRef]
- Bäcker, H.C.; Wu, C.H.; Strauch, R.J. Systematic Review of Diagnosis of Clinically Suspected Scaphoid Fractures. J. Wrist Surg. 2020, 9, 81–89. [Google Scholar] [CrossRef]
- Clementson, M.; Björkman, A.; Thomsen, N.O.B. Acute scaphoid fractures: Guidelines for diagnosis and treatment. EFORT Open Rev. 2020, 5, 96–103. [Google Scholar] [CrossRef]
- Kraus, M.; Anteby, R.; Konen, E.; Eshed, I.; Klang, E. Artificial intelligence for X-ray scaphoid fracture detection: A systematic review and diagnostic test accuracy meta-analysis. Eur. Radiol. 2024, 34, 4341–4351. [Google Scholar] [CrossRef]
- Balci, A.; Basara, I.; Çekdemir, E.Y.; Tetik, F.; Aktaş, G.; Acarer, A.; Özaksoy, D. Wrist fractures: Sensitivity of radiography, prevalence, and patterns in MDCT. Emerg. Radiol. 2015, 22, 251–256. [Google Scholar] [CrossRef]
- Welling, R.D.; Jacobson, J.A.; Jamadar, D.A.; Chong, S.; Caoili, E.M.; Jebson, P.J.L. MDCT and radiography of wrist fractures: Radiographic sensitivity and fracture patterns. AJR Am. J. Roentgenol. 2008, 190, 10–16. [Google Scholar] [CrossRef]
- Hendrix, N.; Hendrix, W.; van Dijke, K.; Maresch, B.; Maas, M.; Bollen, S.; Scholtens, A.; de Jonge, M.; Ong, L.-L.S.; van Ginneken, B.; et al. Musculoskeletal radiologist-level performance by using deep learning for detection of scaphoid fractures on conventional multi-view radiographs of hand and wrist. Eur. Radiol. 2023, 33, 1575–1588. [Google Scholar] [CrossRef]
- Ko, S.; Pareek, A.; Du Ro, H.; Lu, Y.; Camp, C.L.; Martin, R.K.; Krych, A.J. Artificial intelligence in orthopedics: Three strategies for deep learning with orthopedic specific imaging. Knee Surg. Sports Traumatol. Arthrosc. 2022, 30, 758–761. [Google Scholar] [CrossRef] [PubMed]
- Bidyuk, P.; Gozhyj, A.; Kalinina, I.; Vysotska, V.; Vasilev, M.; Malets, R. Forecasting Nonlinear Nonstationary Processes in Machine Learning Task. In Proceedings of the 2020 IEEE Third International Conference on Data Stream Mining & Processing (DSMP), Lviv, Ukraine, 21–25 August 2020; IEEE: Piscataway, NJ, USA, 2020; pp. 28–32, ISBN 978-1-7281-3214-3. [Google Scholar]
- Goodacre, S. Using clinical risk models to predict outcomes: What are we predicting and why? Emerg. Med. J. 2023, 40, 728–730. [Google Scholar] [CrossRef]
- He, Y.; Liu, N.; Yang, J.; Hong, Y.; Ni, H.; Zhang, Z. Comparison of artificial intelligence and logistic regression models for mortality prediction in acute respiratory distress syndrome: A systematic review and meta-analysis. Intensive Care Med. Exp. 2025, 13, 23. [Google Scholar] [CrossRef] [PubMed]
- Germann, C.; Meyer, A.N.; Staib, M.; Sutter, R.; Fritz, B. Performance of a deep convolutional neural network for MRI-based vertebral body measurements and insufficiency fracture detection. Eur. Radiol. 2023, 33, 3188–3199. [Google Scholar] [CrossRef]
- Bulstra, A.E.J. A Machine Learning Algorithm to Estimate the Probability of a True Scaphoid Fracture After Wrist Trauma. J. Hand Surg. Am. 2022, 47, 709–718. [Google Scholar] [CrossRef]
- Singh, A.; Ardakani, A.A.; Loh, H.W.; Anamika, P.V.; Acharya, U.R.; Kamath, S.; Bhat, A.K. Automated detection of scaphoid fractures using deep neural networks in radiographs. Eng. Appl. Artif. Intell. 2023, 122, 106165. [Google Scholar] [CrossRef]
- Yoon, A.P.; Chung, W.T.; Wang, C.-W.; Kuo, C.-F.; Lin, C.; Chung, K.C. Can a Deep Learning Algorithm Improve Detection of Occult Scaphoid Fractures in Plain Radiographs? A Clinical Validation Study. Clin. Orthop. Relat. Res. 2023, 481, 1828–1835. [Google Scholar] [CrossRef]
- Yoon, A.P.; Lee, Y.-L.; Kane, R.L.; Kuo, C.-F.; Lin, C.; Chung, K.C. Development and Validation of a Deep Learning Model Using Convolutional Neural Networks to Identify Scaphoid Fractures in Radiographs. JAMA Netw. Open 2021, 4, e216096. [Google Scholar] [CrossRef]
- Machrowska, A.; Karpiński, R.; Maciejewski, M.; Jonak, J.; Krakowski, P.; Syta, A. Multi-Scale Analysis of Knee Joint Acoustic Signals for Cartilage Degeneration Assessment. Sensors 2025, 25, 706. [Google Scholar] [CrossRef]
- Mahmoodi, S.; Sharif, B.S.; Chester, E.G.; Owen, J.P.; Lee, R. Skeletal growth estimation using radiographic image processing and analysis. IEEE Trans. Inf. Technol. Biomed. 2000, 4, 292–297. [Google Scholar] [CrossRef]
- Lee, J.; Chung, S.W. Deep Learning for Orthopedic Disease Based on Medical Image Analysis: Present and Future. Appl. Sci. 2022, 12, 681. [Google Scholar] [CrossRef]
- Li, C.; Peng, Z.; Zhou, Y.; Ruan, M.; Su, Y.-Y.; Liu, S.; Meng, X.-H.; Xu, Y.-Q. The progress in the classification and treatment of scaphoid nonunion. Surgeon 2022, 20, e231–e235. [Google Scholar] [CrossRef] [PubMed]
- Unay, K.; Gokcen, B.; Ozkan, K.; Poyanli, O.; Eceviz, E. Examination tests predictive of bone injury in patients with clinically suspected occult scaphoid fracture. Injury 2009, 40, 1265–1268. [Google Scholar] [CrossRef] [PubMed]
- Hayes, D.S.; Cush, C.; El Koussaify, J.; Manzar, S.; Klena, J.C.; Grandizio, L.C. Defining Nonunion for Metacarpal Fractures: A Systematic Review. J. Hand Surg. Glob. Online 2023, 5, 677–681. [Google Scholar] [CrossRef]
- Medtronic Sofamor Danek, Inc. INFUSE® Bone Graft Important Medical Information; Food and Drug Administration: Silver Spring, MD, USA, 2007. Available online: https://www.accessdata.fda.gov/cdrh_docs/pdf/p000054c.pdf (accessed on 22 February 2025).
- Zura, R.; Xiong, Z.; Einhorn, T.; Watson, J.T.; Ostrum, R.F.; Prayson, M.J.; Della Rocca, G.J.; Mehta, S.; McKinley, T.; Wang, Z.; et al. Epidemiology of Fracture Nonunion in 18 Human Bones. JAMA Surg. 2016, 151, e162775. [Google Scholar] [CrossRef]
- Strauch, R.J. Scapholunate advanced collapse and scaphoid nonunion advanced collapse arthritis--update on evaluation and treatment. J. Hand Surg. Am. 2011, 36, 729–735. [Google Scholar] [CrossRef]
- Filan, S.L.; Herbert, T.J. Herbert screw fixation of scaphoid fractures. J. Bone Jt. Surg. Br. 1996, 78, 519–529. [Google Scholar] [CrossRef]
- Slade, J.F.; Geissler, W.B.; Gutow, A.P.; Merrell, G.A. Percutaneous internal fixation of selected scaphoid nonunions with an arthroscopically assisted dorsal approach. J. Bone Jt. Surg. Am. 2003, 85 (Suppl. S4), 20–32. [Google Scholar] [CrossRef]
- Slade, J.F.; Dodds, S.D. Minimally invasive management of scaphoid nonunions. Clin. Orthop. Relat. Res. 2006, 445, 108–119. [Google Scholar] [CrossRef]
- Sharma, S. Artificial intelligence for fracture diagnosis in orthopedic X-rays: Current developments and future potential. SICOT J. 2023, 9, 21. [Google Scholar] [CrossRef]
- Cohen, M.; Puntonet, J.; Sanchez, J.; Kierszbaum, E.; Crema, M.; Soyer, P.; Dion, E. Artificial intelligence vs. radiologist: Accuracy of wrist fracture detection on radiographs. Eur. Radiol. 2023, 33, 3974–3983. [Google Scholar] [CrossRef] [PubMed]
- Langerhuizen, D.W.G.; Bulstra, A.E.J.; Janssen, S.J.; Ring, D.; Kerkhoffs, G.M.M.J.; Jaarsma, R.L.; Doornberg, J.N. Is Deep Learning On Par with Human Observers for Detection of Radiographically Visible and Occult Fractures of the Scaphoid? Clin. Orthop. Relat. Res. 2020, 478, 2653–2659. [Google Scholar] [CrossRef] [PubMed]
- Hendrix, N.; Scholten, E.; Vernhout, B.; Bruijnen, S.; Maresch, B.; de Jong, M.; Diepstraten, S.; Bollen, S.; Schalekamp, S.; de Rooij, M.; et al. Development and Validation of a Convolutional Neural Network for Automated Detection of Scaphoid Fractures on Conventional Radiographs. Radiol. Artif. Intell. 2021, 3, e200260. [Google Scholar] [CrossRef] [PubMed]
- Chung, S.W.; Han, S.S.; Lee, J.W.; Oh, K.-S.; Kim, N.R.; Yoon, J.P.; Kim, J.Y.; Moon, S.H.; Kwon, J.; Lee, H.-J.; et al. Automated detection and classification of the proximal humerus fracture by using deep learning algorithm. Acta Orthop. 2018, 89, 468–473. [Google Scholar] [CrossRef]
- Gulshan, V.; Peng, L.; Coram, M.; Stumpe, M.C.; Wu, D.; Narayanaswamy, A.; Venugopalan, S.; Widner, K.; Madams, T.; Cuadros, J.; et al. Development and Validation of a Deep Learning Algorithm for Detection of Diabetic Retinopathy in Retinal Fundus Photographs. JAMA 2016, 316, 2402–2410. [Google Scholar] [CrossRef]
- Zargari Khuzani, A.; Heidari, M.; Shariati, S.A. COVID-Classifier: An automated machine learning model to assist in the diagnosis of COVID-19 infection in chest X-ray images. Sci. Rep. 2021, 11, 9887. [Google Scholar] [CrossRef]
- Rasheed, J.; Hameed, A.A.; Djeddi, C.; Jamil, A.; Al-Turjman, F. A machine learning-based framework for diagnosis of COVID-19 from chest X-ray images. Interdiscip. Sci. 2021, 13, 103–117. [Google Scholar] [CrossRef]
- Erkoc, M.F.; Ulutas, H.; Sahin, M.E. Intervertebral Cervical Disc Intensity (IVCDI) Detection and Classification on MRI Scans Using Deep Learning Methods. Int. J. Imaging Syst. Technol. 2024, 34, e23174. [Google Scholar] [CrossRef]
- Dong, S.; Wang, P.; Abbas, K. A survey on deep learning and its applications. Comput. Sci. Rev. 2021, 40, 100379. [Google Scholar] [CrossRef]
- Rachunek-Medved, K.; Illg, C.; Einzmann, A.; Kolbenschlag, J.; Daigeler, A.; Medved, F. Postoperative scaphoid alignment, smoking, and avascular necrosis mostly influence union rate after scaphoid reconstruction: Results from a retrospective single center study involving 370 patients. J. Plast. Reconstr. Aesthet. Surg. 2023, 87, 430–439. [Google Scholar] [CrossRef]
- Joseph, V.R. Optimal ratio for data splitting. Stat. Anal. 2022, 15, 531–538. [Google Scholar] [CrossRef]
- Brown, A.; Tomasev, N.; Freyberg, J.; Liu, Y.; Karthikesalingam, A.; Schrouff, J. Detecting shortcut learning for fair medical AI using shortcut testing. Nat. Commun. 2023, 14, 4314. [Google Scholar] [CrossRef] [PubMed]
- Busfield, T. Image Classification with TensorFlow; Analytics Vidhya: Gurugram, India, 2020; Available online: https://medium.com/analytics-vidhya/image-classification-with-tensorflow-2a406bdfe0c1 (accessed on 2 January 2025).
- Heidsieck, D.S.P.; ten Berg, P.W.L.; Schep, N.W.L.; Strackee, S.D. Factors Associated with Patient Delay in Scaphoid Nonunions. J. Hand Microsurg. 2015, 7, 300–305. [Google Scholar] [CrossRef] [PubMed]
- Grewal, R.; Suh, N.; MacDermid, J.C. The Missed Scaphoid Fracture-Outcomes of Delayed Cast Treatment. J. Wrist Surg. 2015, 4, 278–283. [Google Scholar] [CrossRef] [PubMed]
- Ritter, K.; Giachino, A.A. The treatment of pseudoarthrosis of the scaphoid by bone grafting and three methods of internal fixation. Can. J. Surg. 2000, 43, 118–124. [Google Scholar]
- Ayalon, O.; Rettig, S.A.; Tedesco, L.J. Bone Graft and Fixation Options in the Surgical Management of Scaphoid Nonunion. J. Am. Acad. Orthop. Surg. 2024, 24, 510. [Google Scholar] [CrossRef]
- Shapiro, L.M.; Schultz, E.A.; Welch, J.; Zhuang, T.; Kamal, R.N. MRI for Scaphoid Nonunion: Utilization Rates, Factors Associated with Utilization, and Subsequent Vascularized Bone Graft Use. J. Hand Surg. Am. 2024, 50, 182–187. [Google Scholar] [CrossRef]
- Bagley, S.C.; White, H.; Golomb, B.A. Logistic regression in the medical literature: Standards for use and reporting, with particular attention to one medical domain. J. Clin. Epidemiol. 2001, 54, 979–985. [Google Scholar] [CrossRef]
- Liew, B.X.W.; Kovacs, F.M.; Rügamer, D.; Royuela, A. Machine learning versus logistic regression for prognostic modelling in individuals with non-specific neck pain. Eur. Spine J. 2022, 31, 2082–2091. [Google Scholar] [CrossRef]
- Schuind, F.; Haentjens, P.; van Innis, F.; Vander Maren, C.; Garcia-Elias, M.; Sennwald, G. Prognostic factors in the treatment of carpal scaphoid nonunions. J. Hand Surg. Am. 1999, 24, 761–776. [Google Scholar] [CrossRef]
- Leister, I.; Haider, T.; Vogel, M.; Vastmans, J.; Langthaler, P.; Mattiassich, G.; Christ, A.; Etschmaier, M.; Eijkenboom, A.; Burghuber, J.; et al. A Predictive Model to Identify Treatment-related Risk Factors for Odontoid Fracture Nonunion Using Machine Learning. Spine 2023, 48, 164–171. [Google Scholar] [CrossRef] [PubMed]
- Takahashi, S.; Terai, H.; Hoshino, M.; Tsujio, T.; Kato, M.; Toyoda, H.; Suzuki, A.; Tamai, K.; Yabu, A.; Nakamura, H. Machine-learning-based approach for nonunion prediction following osteoporotic vertebral fractures. Eur. Spine J. 2023, 32, 3788–3796. [Google Scholar] [CrossRef] [PubMed]
- Hofer, I.S.; Burns, M.; Kendale, S.; Wanderer, J.P. Realistically Integrating Machine Learning into clinical practice: A road map of opportunities, challenges, and a potential future. Anesth. Analg. 2020, 130, 1115–1118. [Google Scholar] [CrossRef] [PubMed]
- Naik, N.; Hameed, B.M.Z.; Shetty, D.K.; Swain, D.; Shah, M.; Paul, R.; Aggarwal, K.; Ibrahim, S.; Patil, V.; Smriti, K.; et al. Legal and Ethical Consideration in Artificial Intelligence in Healthcare: Who Takes Responsibility? Front. Surg. 2022, 9, 862322. [Google Scholar] [CrossRef]
| Successful Operation (n = 263) | Unsuccessful Operation (n = 83) | p-Value | |
|---|---|---|---|
| Age (yrs) [mean, ±SD] | 34.6 ± 12.0 | 32.9 ± 10.3 | 0.25 1 |
| Sex (female) [n, %] | 26, 9.9% | 5, 6.0% | 0.38 2 |
| Side (right) [n, %] | 127, 48.3% | 40, 48.2% | >0.99 2 |
| Smoking status (yes) [n, %] | 61, 23.2% | 38, 45.8% | 0.0001 (***) 2 |
| AVN intraop. (yes) [n, %] | 27, 11.6% | 21, 36.8% | <0.0001 (****) 2 |
| Grafts used [n, %) | |||
| Non-vascularized | 191, 72.6% | 57, 68.7% | 0.49 2 |
| Vascularized, pedicled | 59, 22.4% | 23, 27.7% | 0.37 2 |
| Vascularized, free | 11, 4.2% | 3, 3.6% | >0.99 2 |
| None | 2, 0.8% | 0, 0% | >0.99 2 |
| Features | Coefficients |
|---|---|
| AVN intraop. (yes) | −0.50 |
| Smoking | −0.15 |
| Age | 0.01 |
| Sex | 0.00 |
| Side | 0.00 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Tümen, L.; Medved, F.; Rachunek-Medved, K.; Han, Y.; Saul, D. Deep Learning in Scaphoid Nonunion Treatment. J. Clin. Med. 2025, 14, 1850. https://doi.org/10.3390/jcm14061850
Tümen L, Medved F, Rachunek-Medved K, Han Y, Saul D. Deep Learning in Scaphoid Nonunion Treatment. Journal of Clinical Medicine. 2025; 14(6):1850. https://doi.org/10.3390/jcm14061850
Chicago/Turabian StyleTümen, Leyla, Fabian Medved, Katarzyna Rachunek-Medved, Yeaeun Han, and Dominik Saul. 2025. "Deep Learning in Scaphoid Nonunion Treatment" Journal of Clinical Medicine 14, no. 6: 1850. https://doi.org/10.3390/jcm14061850
APA StyleTümen, L., Medved, F., Rachunek-Medved, K., Han, Y., & Saul, D. (2025). Deep Learning in Scaphoid Nonunion Treatment. Journal of Clinical Medicine, 14(6), 1850. https://doi.org/10.3390/jcm14061850









