Comparative Efficacy of Extracorporeal Versus Conventional Cardiopulmonary Resuscitation in Adult Refractory Out-of-Hospital Cardiac Arrest: A Retrospective Study at a Single Center
Abstract
1. Introduction
2. Materials and Methods
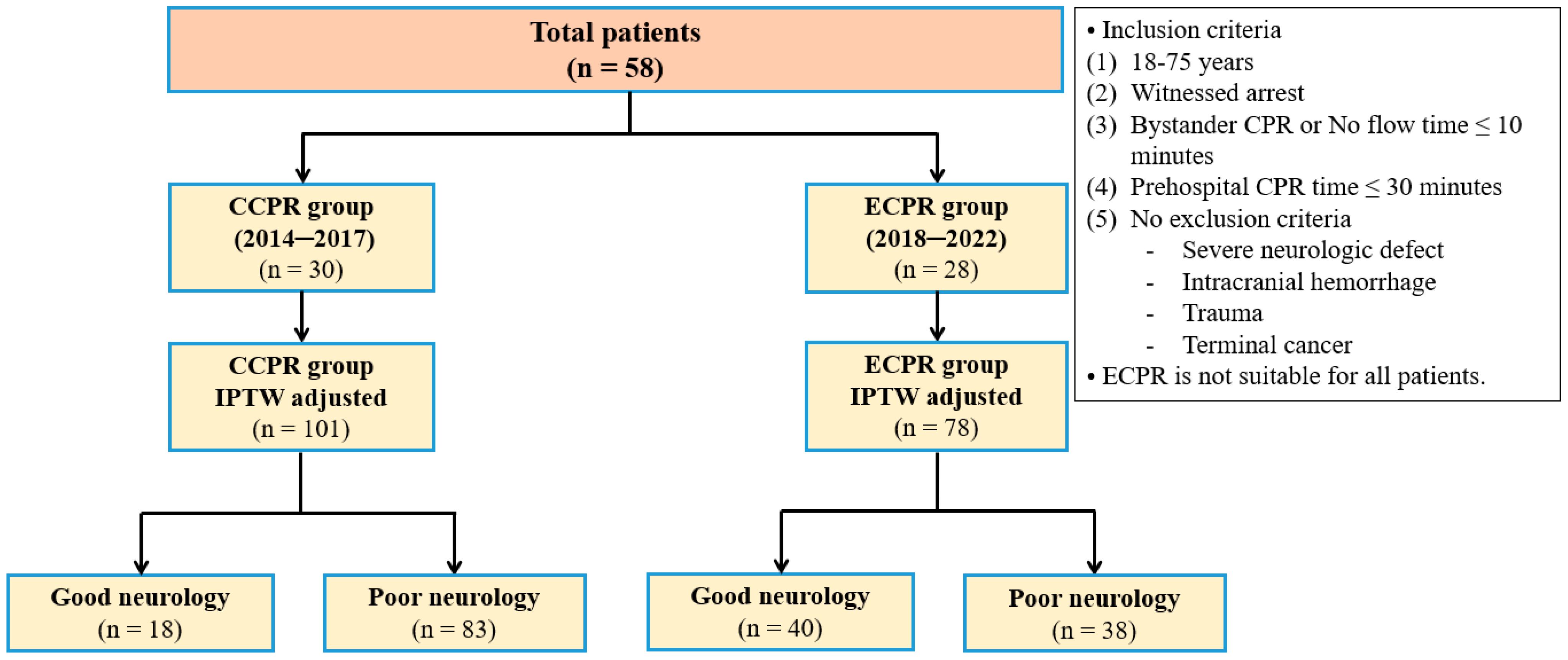
2.1. Study Patients
2.2. Study Outcomes
2.3. Statistical Analysis
3. Results
3.1. Baseline Characteristics of All Patients
3.2. Characteristics of Patients According to Neurological Outcomes
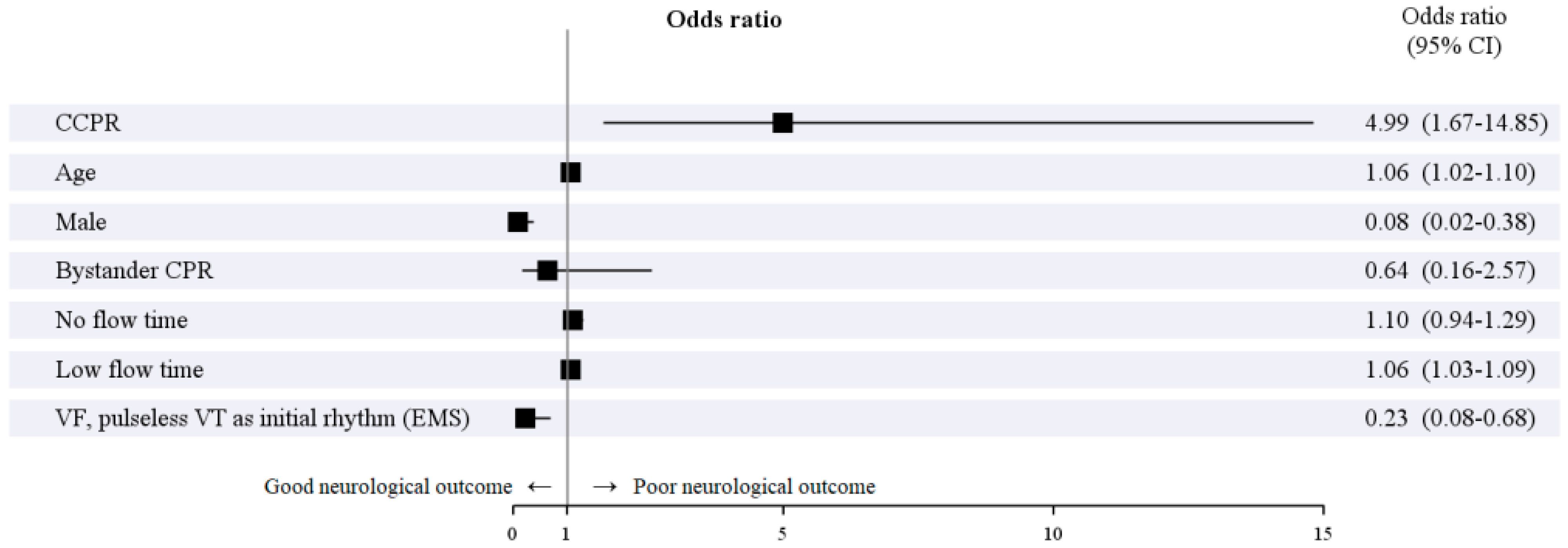
3.3. Impact of ECPR and Predictors of Poor Neurological Outcomes
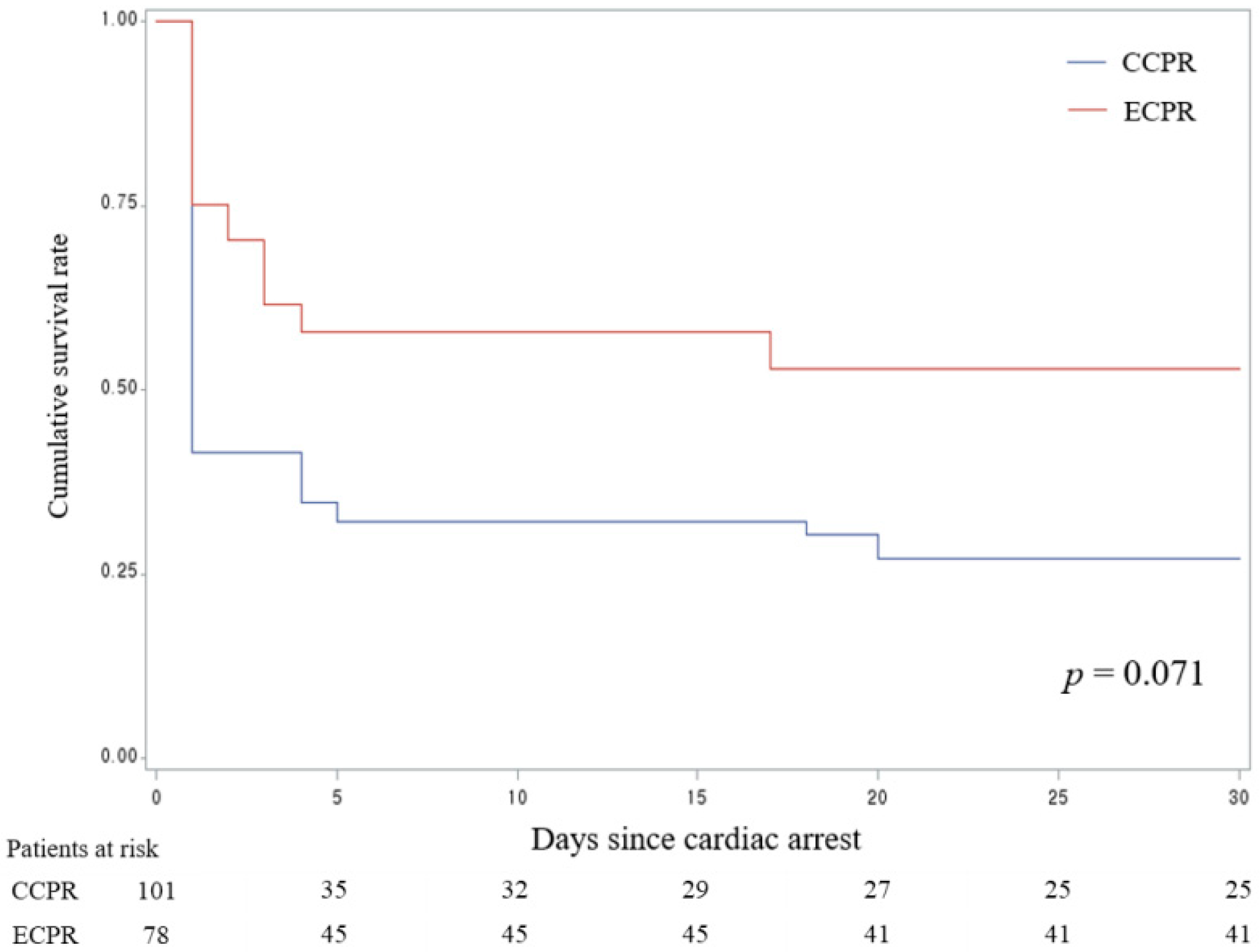
3.4. 30-Day Survival in the ECPR Group Compared with Those in the CCPR Group
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Strömsöe, A.; Svensson, L.; Axelsson, Å.B.; Claesson, A.; Göransson, K.E.; Nordberg, P.; Herlitz, J. Improved outcome in Sweden after out-of-hospital cardiac arrest and possible association with improvements in every link in the chain of survival. Eur. Heart J. 2015, 36, 863–871. [Google Scholar] [CrossRef]
- Gräsner, J.T.; Lefering, R.; Koster, R.W.; Masterson, S.; Böttiger, B.W.; Herlitz, J.; Wnent, J.; Tjelmeland, I.B.; Ortiz, F.R.; Maurer, H.; et al. EuReCa ONE Collaborators. EuReCa ONE-27 Nations, ONE Europe, ONE Registry: A prospective one month analysis of out-of-hospital cardiac arrest outcomes in 27 countries in Europe. Resuscitation 2016, 105, 188–195. [Google Scholar] [CrossRef] [PubMed]
- Panchal, A.R.; Bartos, J.A.; Cabañas, J.G.; Donnino, M.W.; Drennan, I.R.; Hirsch, K.G.; Kudenchuk, P.J.; Kurz, M.C.; Lavonas, E.J.; Morley, P.T.; et al. Part 3: Adult Basic and Advanced Life Support: 2020 American Heart Association Guidelines for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care. Circulation 2020, 142, S366–S468. [Google Scholar] [CrossRef] [PubMed]
- Morales-Cané, I.; Valverde-León, M.D.; Rodríguez-Borrego, M.A. Epinephrine in cardiac arrest: Systematic review and meta-analysis. Rev. Lat.-Am. Enferm. 2016, 24, 2821. [Google Scholar] [CrossRef] [PubMed]
- Bernard, S.A.; Gray, T.W.; Buist, M.D.; Jones, B.M.; Silvester, W.; Gutteridge, G.; Smith, K. Treatment of comatose survivors of out-of-hospital cardiac arrest with induced hypothermia. N. Engl. J. Med. 2002, 346, 557–563. [Google Scholar] [CrossRef]
- Metelmann, C.; Metelmann, B.; Kohnen, D.; Brinkrolf, P.; Andelius, L.; Böttiger, B.W.; Burkart, R.; Hahnenkamp, K.; Krammel, M.; Marks, T.; et al. Smartphone-based dispatch of community first responders to out-of-hospital cardiac arrest—Statements from an international consensus conference. Scand. J. Trauma Resusc. Emerg. Med. 2021, 29, 29. [Google Scholar] [CrossRef] [PubMed]
- Kudenchuk, P.J.; Sandroni, C.; Drinhaus, H.R.; Böttiger, B.W.; Cariou, A.; Sunde, K. Breakthrough in cardiac arrest: Reports from the 4th Paris International Conference. Ann. Intensive Care 2015, 5, 22. [Google Scholar] [CrossRef]
- Link, M.S.; Berkow, L.C.; Kudenchuk, P.J.; Halperin, H.R.; Hess, E.P.; Moitra, V.K.; Neumar, R.W.; O’Neil, B.J.; Paxton, J.H.; Silvers, S.M.; et al. Part 7: Adult Advanced Cardiovascular Life Support: 2015 American Heart Association Guidelines Update for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care. Circulation 2015, 132, S444–S464. [Google Scholar] [CrossRef] [PubMed]
- Jones, D.; Daglish, F.M.; Tanner, B.M.; Wilkie, F.J.M. A review of pre-hospital extracorporeal cardiopulmonary resuscitation and its potential application in the North East of England. Int. J. Emerg. Med. 2024, 17, 7. [Google Scholar] [CrossRef]
- Kim, S.J.; Kim, H.J.; Lee, H.Y.; Ahn, H.S.; Lee, S.W. Comparing extracorporeal cardiopulmonary resuscitation with conventional cardiopulmonary resuscitation: A meta-analysis. Resuscitation 2016, 103, 106–116. [Google Scholar] [CrossRef] [PubMed]
- Sakamoto, T.; Morimura, N.; Nagao, K.; Asai, Y.; Yokota, H.; Nara, S.; Hase, M.; Tahara, Y.; Atsumi, T.; SAVE-J Study Group. Extracorporeal cardiopulmonary resuscitation versus conventional cardiopulmonary resuscitation in adults with out-of-hospital cardiac arrest: A prospective observational study. Resuscitation 2014, 85, 762–768. [Google Scholar] [CrossRef]
- Patricio, D.; Peluso, L.; Brasseur, A.; Lheureux, O.; Belliato, M.; Vincent, J.L.; Creteur, J.; Taccone, F.S. Comparison of extracorporeal and conventional cardiopulmonary resuscitation: A retrospective propensity score matched study. Crit. Care 2019, 23, 27. [Google Scholar] [CrossRef]
- Maekawa, K.; Tanno, K.; Hase, M.; Mori, K.; Asai, Y. Extracorporeal cardiopulmonary resuscitation for patients with out-of-hospital cardiac arrest of cardiac origin: A propensity-matched study and predictor analysis. Crit. Care Med. 2013, 41, 1186–1196. [Google Scholar] [CrossRef] [PubMed]
- Yannopoulos, D.; Bartos, J.; Raveendran, G.; Walser, E.; Connett, J.; Murray, T.A.; Collins, G.; Zhang, L.; Kalra, R.; Kosmopoulos, M.; et al. Advanced reperfusion strategies for patients with out-of-hospital cardiac arrest and refractory ventricular fibrillation (ARREST): A phase 2, single centre, open-label, randomised controlled trial. Lancet 2020, 396, 1807–1816. [Google Scholar] [CrossRef]
- Taccone, F.S.; Minini, A.; Avalli, L.; Alm-Kruse, K.; Annoni, F.; Bougouin, W.; Burrell, A.; Cariou, A.; Coppalini, G.; Grunau, B.; et al. Impact of extracorporeal cardiopulmonary resuscitation on neurological prognosis and survival in adult patients after cardiac arrest: An individual pooled patient data meta-analysis. Resuscitation 2024, 202, 110357. [Google Scholar] [CrossRef] [PubMed]
- Choi, D.S.; Kim, T.; Ro, Y.S.; Ahn, K.O.; Lee, E.J.; Hwang, S.S.; Song, S.W.; Song, K.J.; Shin, S.D. Extracorporeal life support and survival after out-of-hospital cardiac arrest in a nationwide registry: A propensity score-matched analysis. Resuscitation 2016, 99, 26–32. [Google Scholar] [CrossRef] [PubMed]
- Twohig, C.J.; Singer, B.; Grier, G.; Finney, S.J. A systematic literature review and meta-analysis of the effectiveness of extracorporeal-CPR versus conventional-CPR for adult patients in cardiac arrest. J. Intensive Care Soc. 2019, 20, 347–357. [Google Scholar] [CrossRef] [PubMed]
- Ahn, C.; Kim, W.; Cho, Y.; Choi, K.S.; Jang, B.H.; Lim, T.H. Efficacy of extracorporeal cardiopulmonary resuscitation compared to conventional cardiopulmonary resuscitation for adult cardiac arrest patients: A systematic review and meta-analysis. Sci. Rep. 2016, 23, 34208. [Google Scholar] [CrossRef]
- Wang, J.Y.; Chen, Y.; Dong, R.; Li, S.; Peng, J.; Hu, X.; Jiang, W.; Wang, C.; Weng, L.; Du, B. Extracorporeal vs. conventional CPR for out-of-hospital cardiac arrest: A systematic review and meta-analysis. Am. J. Emerg. Med. 2024, 80, 185–193. [Google Scholar] [CrossRef] [PubMed]
- Reddy, S.; Garcia, S.; Hostetter, L.J.; Finch, A.S.; Bellolio, F.; Guru, P.; Gerberi, D.J.; Smischney, N.J. Extracorporeal-CPR versus conventional-CPR for adult patients in out of hospital cardiac arrest- Systematic review and meta-analysis. J. Intensive Care Med. 2025, 40, 207–217. [Google Scholar] [CrossRef] [PubMed]
- Pagura, L.; Fabris, E.; Rakar, S.; Gabrielli, M.; Mazzaro, E.; Sinagra, G.; Stolfo, D. Does extracorporeal cardiopulmonary resuscitation improve survival with favorable neurological outcome in out-of-hospital cardiac arrest? A systematic review and meta-analysis. J. Crit. Care 2024, 84, 154882. [Google Scholar] [CrossRef] [PubMed]
- Sonneville, R.; Schmidt, M. Extracorporeal cardiopulmonary resuscitation for adults with refractory out-of-hospital cardiac arrest. Circulation 2020, 141, 887–890. [Google Scholar] [CrossRef] [PubMed]
- Grossestreuer, A.V.; Abella, B.S.; Sheak, K.R.; Cinousis, M.J.; Perman, S.M.; Leary, M.; Wiebe, D.J.; Gaieski, D.F. Inter-rater reliability of post-arrest cerebral performance category (CPC) scores. Resuscitation 2016, 109, 21–24. [Google Scholar] [CrossRef]
- Robins, J.M.; Hernán, M.A.; Brumback, B. Marginal structural models and causal inference in epidemiology. Epidemiology 2000, 11, 550–560. [Google Scholar] [CrossRef]
- Shin, Y.S.; Kim, Y.J.; Ryoo, S.M.; Sohn, C.H.; Ahn, S.; Seo, D.W.; Kim, W.Y. Promising candidates for extracorporeal cardiopulmonary resuscitation for out-of-hospital cardiac arrest. Sci. Rep. 2020, 10, 22180. [Google Scholar] [CrossRef]
- Schober, A.; Sterz, F.; Herkner, H.; Wallmueller, C.; Weiser, C.; Hubner, P.; Testori, C. Emergency extracorporeal life support and ongoing resuscitation: A retrospective comparison for refractory out-of-hospital cardiac arrest. Emerg. Med. J. 2017, 34, 277–281. [Google Scholar] [CrossRef] [PubMed]
- Alm-Kruse, K.; Sørensen, G.; Osbakk, S.A.; Sunde, K.; Bendz, B.; Andersen, G.; Fiane, A.; Hagen, O.A.; Kramer-Johansen, J. Outcome in refractory out-of-hospital cardiac arrest before and after implementation of an ECPR protocol. Resuscitation 2021, 162, 35–42. [Google Scholar] [CrossRef]
- Suverein, M.M.; Delnoij, T.S.R.; Lorusso, R.; Brandon Bravo Bruinsma, G.J.; Otterspoor, L.; Elzo Kraemer, C.V.; Vlaar, A.P.J.; van der Heijden, J.J.; Scholten, E.; den Uil, C.; et al. Early Extracorporeal CPR for Refractory Out-of-Hospital Cardiac Arrest. N. Engl. J. Med. 2023, 388, 299–309. [Google Scholar] [CrossRef] [PubMed]
- Pozzi, M.; Armoiry, X.; Achana, F.; Koffel, C.; Pavlakovic, I.; Lavigne, F.; Fellahi, J.L.; Obadia, J.F. Extracorporeal Life Support for Refractory Cardiac Arrest: A 10-Year Comparative Analysis. Ann. Thorac. Surg. 2019, 107, 809–816. [Google Scholar] [CrossRef] [PubMed]
- Chen, Y.S.; Lin, J.W.; Yu, H.Y.; Ko, W.J.; Jerng, J.S.; Chang, W.T.; Chen, W.J.; Huang, S.C.; Chi, N.H.; Wang, C.H.; et al. Cardiopulmonary resuscitation with assisted extracorporeal life-support versus conventional cardiopulmonary resuscitation in adults with in-hospital cardiac arrest: An observational study and propensity analysis. Lancet 2008, 372, 554–561. [Google Scholar] [CrossRef]
- Shin, T.G.; Jo, I.J.; Sim, M.S.; Song, Y.B.; Yang, J.H.; Hahn, J.Y.; Choi, S.H.; Gwon, H.C.; Jeon, E.S.; Sung, K.; et al. Two-year survival and neurological outcome of in-hospital cardiac arrest patients rescued by extracorporeal cardiopulmonary resuscitation. Int. J. Cardiol. 2013, 168, 3424–3430. [Google Scholar] [CrossRef] [PubMed]
- Shoji, K.; Ohbe, H.; Kudo, D.; Tanikawa, A.; Kobayashi, M.; Aoki, M.; Hamaguchi, T.; Nagashima, F.; Inoue, A.; Hifumi, T.; et al. Low-flow time and outcomes in out-of-hospital cardiac arrest patients treated with extracorporeal cardiopulmonary resuscitation. Am. J. Emerg. Med. 2024, 75, 37–41. [Google Scholar] [CrossRef]
- Kandori, K.; Okada, Y.; Okada, A.; Nakajima, S.; Okada, N.; Matsuyama, T.; Kitamura, T.; Narumiya, H.; Iizuka, R. Association between cardiac rhythm conversion and neurological outcome among cardiac arrest patients with initial shockable rhythm: A nationwide prospective study in Japan. Eur. Heart J. Acute Cardiovasc. Care 2021, 10, 119–126. [Google Scholar] [CrossRef]
- Daou, O.; Winiszewski, H.; Besch, G.; Pili-Floury, S.; Belon, F.; Guillon, B.; Marx, T.; Chocron, S.; Capellier, G.; Perrotti, A.; et al. Initial pH and shockable rhythm are associated with favorable neurological outcome in cardiac arrest patients resuscitated with extracorporeal cardiopulmonary resuscitation. J. Thorac. Dis. 2020, 12, 849–857. [Google Scholar] [CrossRef] [PubMed]
- Kishimori, T.; Matsuyama, T.; Kiyohara, K.; Kitamura, T.; Shida, H.; Kiguchi, T.; Nishiyama, C.; Kobayashi, D.; Okabayashi, S.; Shimamoto, T.; et al. Prehospital cardiopulmonary resuscitation duration and neurological outcome after adult out-of-hospital cardiac arrest by location of arrest. Eur. Heart J. Acute Cardiovasc. Care 2020, 9, S90–S99. [Google Scholar] [CrossRef]
- Kiyohara, K.; Nishiyama, C.; Kitamura, T.; Matsuyama, T.; Sado, J.; Shimamoto, T.; Kobayashi, D.; Kiguchi, T.; Okabayashi, S.; Kawamura, T.; et al. The association between public access defibrillation and outcome in witnessed out-of-hospital cardiac arrest with shockable rhythm. Resuscitation 2019, 140, 93–97. [Google Scholar] [CrossRef] [PubMed]
- Park, J.H.; Song, K.J.; Shin, S.D.; Hong, K.J. Does second EMS unit response time affect outcomes of OHCA in multi-tiered system? A nationwide observational study. Am. J. Emerg. Med. 2021, 42, 161–167. [Google Scholar] [CrossRef]
- Bosson, N.; Kaji, A.H.; Fang, A.; Thomas, J.L.; French, W.J.; Shavelle, D.; Niemann, J.T. Sex Differences in Survival From Out-of-Hospital Cardiac Arrest in the Era of Regionalized Systems and Advanced Post-Resuscitation Care. J. Am. Heart Assoc. 2016, 5, e004131. [Google Scholar] [CrossRef] [PubMed]
- Ng, Y.Y.; Wah, W.; Liu, N.; Zhou, S.A.; Ho, A.F.; Pek, P.P.; Shin, S.D.; Tanaka, H.; Khunkhlai, N.; Lin, C.H.; et al. Associations between gender and cardiac arrest outcomes in Pan-Asian out-of-hospital cardiac arrest patients. Resuscitation 2016, 102, 116–121. [Google Scholar] [CrossRef] [PubMed]
- Karlsson, V.; Dankiewicz, J.; Nielsen, N.; Kern, K.B.; Mooney, M.R.; Riker, R.R.; Rubertsson, S.; Seder, D.B.; Stammet, P.; Sunde, K.; et al. Association of gender to outcome after out-of-hospital cardiac arrest—A report from the International Cardiac Arrest Registry. Crit. Care 2015, 19, 182. [Google Scholar] [CrossRef] [PubMed]
- Goto, T.; Morita, S.; Kitamura, T.; Natsukawa, T.; Sawano, H.; Hayashi, Y.; Kai, T. Impact of extracorporeal cardiopulmonary resuscitation on outcomes of elderly patients who had out-of-hospital cardiac arrests: A single-centre retrospective analysis. BMJ Open 2018, 8, e019811. [Google Scholar] [CrossRef] [PubMed]
- Lunz, D.; Calabrò, L.; Belliato, M.; Contri, E.; Broman, L.M.; Scandroglio, A.M.; Patricio, D.; Malfertheiner, M.; Creteur, J.; Philipp, A.; et al. Extracorporeal membrane oxygenation for refractory cardiac arrest: A retrospective multicenter study. Intensive Care Med. 2020, 46, 973–982. [Google Scholar] [CrossRef]

| Overall Cohort | IPTW | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Total Patients (n = 58) | ECPR Group (n = 28) | CCPR Group (n = 30) | p Value | SMD | Total Patients (n =179) | ECPR Group (n = 78) | CCPR Group (n = 101) | p Value | SMD | |
| Age, median (IQR) (yr) | 58.0 (50.0–68.0) | 55.5 (48.0–65.0) | 58.5 (53.0–68.0) | 0.121 | −0.486 | 58.0 (50.0–69.0) | 54.0 (39.0–65.0) | 66.0 (55.0–72.0) | 0.001 | −0.531 |
| Male, n (%) | 46 (79.3) | 25 (83.3) | 21 (75.0) | 0.525 | −0.206 | 142 (79.3) | 53 (67.1) | 89 (88.1) | 0.001 | −0.521 |
| Pre-arrest co-morbidities, n (%) | ||||||||||
| Coronary artery disease | 12 (20.7) | 6 (21.4) | 6 (20.0) | >0.999 | - | 30 (16.8) | 11 (14.1) | 19 (18.8) | 0.461 | - |
| Arrythmia | 7 (12.1) | 3 (10.7) | 4 (13.3) | >0.999 | - | 21 (11.7) | 10 (12.8) | 11 (10.9) | 0.778 | - |
| Heart failure | 6 (10.3) | 3 (10.7) | 3 (10.0) | >0.999 | - | 15 (8.4) | 6 (7.7) | 9 (8.9) | 0.622 | - |
| Hypertension | 23 (39.7) | 10 (35.7) | 13 (43.3) | 0.600 | - | 66 (36.9) | 24 (30.8) | 42 (41.6) | 0.146 | - |
| Diabetes mellitus | 14 (24.1) | 9 (32.1) | 5 (16.7) | 0.224 | - | 35 (19.6) | 18 (23.1) | 17 (16.8) | 0.304 | - |
| Stroke | 3 (5.2) | 0 (0) | 3 (10.0) | 0.238 | - | 19 (10.6) | 0 (0) | 19 (18.8) | <0.001 | - |
| Lung disease | 1 (1.7) | 0 (0) | 1 (3.3) | >0.999 | - | 3 (1.7) | 0 (0) | 3 (3.0) | 0.136 | - |
| Chronic renal disease | 4 (6.9) | 3 (10.7) | 1 (3.3) | 0.345 | - | 8(4.5) | 5(6.4) | 3 (3.0) | 0.423 | - |
| Liver cirrhosis | 2 (3.5) | 0 (0) | 2 (6.7) | 0.492 | - | 5 (2.8) | 0 (0) | 5 (5.0) | 0.060 | - |
| OHCA circumstances, n (%) | ||||||||||
| Witness status | ||||||||||
| By EMS personnel | 10 (17.2) | 5 (17.9) | 5 (16.7) | >0.999 | - | 24 (13.4) | 10 (12.8) | 14 (13.9) | 0.852 | - |
| By Layperson | 48 (82.8) | 23 (82.1) | 25 (83.3) | >0.999 | - | 155 (86.6) | 68 (87.2) | 87 (86.1) | 0.852 | - |
| Bystander CPR | 35 (60.3) | 18 (64.3) | 17 (56.7) | 0.600 | 0.156 | 98 (54.8) | 49 (62.8) | 48 (47.5) | 0.043 | 0.311 |
| First documented arrest rhythm (EMS) | ||||||||||
| VF/pulseless VT | 32 (55.2) | 20 (71.4) | 12 (40.0) | 0.020 | 0.667 | 89 (49.7) | 65 (83.3) | 24 (23.8) | <0.001 | 1.485 |
| PEA | 12 (20.7) | 5 (17.9) | 7 (23.3) | 0.749 | - | 27 (15.1) | 9 (11.5) | 18 (17.8) | 0.291 | - |
| Asystole | 14 (24.1) | 3 (10.7) | 11 (36.7) | 0.031 | - | 63 (35.2) | 4 (5.1) | 60 (59.4) | <0.001 | - |
| First documented arrest rhythm (ER) | ||||||||||
| VF/pulseless VT | 21 (36.2) | 18 (64.3) | 3 (10.0) | <0.001 | - | 57 (31.8) | 52 (66.7) | 9 (8.9) | <0.001 | - |
| PEA | 17 (29.3) | 8 (28.6) | 9 (30.0) | >0.999 | - | 44 (24.6) | 20 (25.6) | 24 (23.8) | 0.733 | - |
| Asystole | 20 (34.5) | 2 (7.1) | 18 (60.0) | <0.001 | - | 78 (43.6) | 6 (7.7) | 72 (71.3) | <0.001 | - |
| Time from collapse to CPR termination, median (IQR) (min) | ||||||||||
| No flow time | 1.0 (0.0–5.0) | 0.0 (0.0–8.0) | 3.5 (1.0–5.0) | 0.167 | 0.021 | 2.0 (0.0–5.0) | 0.0 (0.0–6.0) | 3.0 (0.0–5.0) | 0.967 | 0.007 |
| Low flow time * | 45.5 (32.0–57.0) | 45.5 (33.5–63.5) | 45.5 (30.0–57.0) | 0.581 | 0.276 | 44.0 (31.0–57.0) | 47.0 (34.0–68.0) | 43.0 (30.0–57.0) | 0.074 | 0.287 |
| Pre-hospital CPR time | 20.0 (11.0–27.0) | 18.5 (11.0–30.0) | 20.5 (11.0–26.0) | 0.732 | - | 19.0 (11.0–26.0) | 18.0 (12.0–30.0) | 20.0 (11.0–24.0) | 0.268 | - |
| In-hospital CPR time | 28.5 (12.0–34.0) | 30.0 (15.0–33.5) | 23.5 (12.0–35.0) | 0.508 | - | 27.0 (12.0–34.0) | 30.0 (11.0–34.0) | 23.0 (12.0–34.0) | 0.173 | - |
| Total epinephrine dose, median (IQR) (mg) | 9.5 (4.0–12.0) | 10.0 (4.5–11.5) | 7.5 (4.0–12.0) | 0.691 | - | 7.0 (4.0–11.0) | 10.0 (3.0–11.0) | 6.0 (5.0–11.0) | 0.928 | - |
| Laboratory finding (Initial), median (IQR) | ||||||||||
| Lactate (mmol/L) (n = 56) | 11.0 (7.0–14.6) | 11.0 (6.8–14.9) | 11.0 (7.2–14.6) | >0.999 | - | 10.9 (6.9–15.0) | 10.2 (6.9–15.6) | 10.9 (7.1–15.0) | 0.780 | - |
| pH (n = 56) | 7.0 (6.9–7.2) | 7.0 (6.9–7.1) | 7.1 (6.9–7.2) | 0.352 | - | 7.0 (6.9–7.2) | 7.0 (6.9–7.1) | 7.1 (7.0–7.2) | 0.442 | - |
| Troponin I (ng/mL) (n = 44) | 0.1 (0.0–0.5) | 0.3 (0.1–0.9) | 0.1 (0.0–0.1) | 0.023 | - | 0.1 (0.0–0.4) | 0.3 (0.1–0.8) | 0.0 (0.0–0.1) | 0.082 | - |
| Hospital stay, median (IQR) (day) | 4.0 (1.0–16.0) | 4.5 (1.5–17.0) | 2.5 (1.0–15.0) | 0.215 | - | 4.0 (1.0–16.0) | 8.0 (2.0–17.0) | 1.0 (1.0–13.0) | 0.368 | - |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lee, J.; Jeong, Y.H.; Kim, Y.J.; Cho, Y.; Oh, J.; Jang, H.J.; Shin, Y.; Kim, J.E.; Kim, H.J.; Cho, Y.H.; et al. Comparative Efficacy of Extracorporeal Versus Conventional Cardiopulmonary Resuscitation in Adult Refractory Out-of-Hospital Cardiac Arrest: A Retrospective Study at a Single Center. J. Clin. Med. 2025, 14, 513. https://doi.org/10.3390/jcm14020513
Lee J, Jeong YH, Kim YJ, Cho Y, Oh J, Jang HJ, Shin Y, Kim JE, Kim HJ, Cho YH, et al. Comparative Efficacy of Extracorporeal Versus Conventional Cardiopulmonary Resuscitation in Adult Refractory Out-of-Hospital Cardiac Arrest: A Retrospective Study at a Single Center. Journal of Clinical Medicine. 2025; 14(2):513. https://doi.org/10.3390/jcm14020513
Chicago/Turabian StyleLee, Juncheol, Yong Ho Jeong, Yun Jin Kim, Yongil Cho, Jaehoon Oh, Hyo Jun Jang, Yonghoon Shin, Ji Eon Kim, Hee Jung Kim, Yang Hyun Cho, and et al. 2025. "Comparative Efficacy of Extracorporeal Versus Conventional Cardiopulmonary Resuscitation in Adult Refractory Out-of-Hospital Cardiac Arrest: A Retrospective Study at a Single Center" Journal of Clinical Medicine 14, no. 2: 513. https://doi.org/10.3390/jcm14020513
APA StyleLee, J., Jeong, Y. H., Kim, Y. J., Cho, Y., Oh, J., Jang, H. J., Shin, Y., Kim, J. E., Kim, H. J., Cho, Y. H., Jung, J. S., & Lee, J. H. (2025). Comparative Efficacy of Extracorporeal Versus Conventional Cardiopulmonary Resuscitation in Adult Refractory Out-of-Hospital Cardiac Arrest: A Retrospective Study at a Single Center. Journal of Clinical Medicine, 14(2), 513. https://doi.org/10.3390/jcm14020513






