The Effect of Selective Occlusal Adjustment on the Disclusion Time Reduction and Symmetry of Occlusal Contacts of the Own Dentition Using Digital Occlusion Analysis in Patients with Temporomandibular Disorders
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design and Population
2.2. The Inclusion and Exclusion Criteria
- Aged 20–50 years old.
- Complete natural dentition comprising at least 28 teeth.
- Presence of chronic muscle-related myofascial pain symptoms consistent with temporomandibular dysfunction.
- Diagnosis of muscle disorders classified as Group I according to the DC/TMD criteria.
- Diagnosis of disk displacement disorders corresponding to Group II of the DC/TMD classification.
- Near-normal occlusal relationships, characterized by preserved contacts between opposing premolars and molars during lateral excursions to both the right and left sides.
- Six months (minimum) of prosthetic treatment of the temporomandibular joint
- Qualification for enameloplasty.
- Temporomandibular joint pain (arthralgia) or degenerative joint disorders, including osteoarthritis and osteoarthrosis, classified as Group III according to the DC/TMD.
- Previous occlusal adjustment therapy.
2.3. Dysfunction Analysis
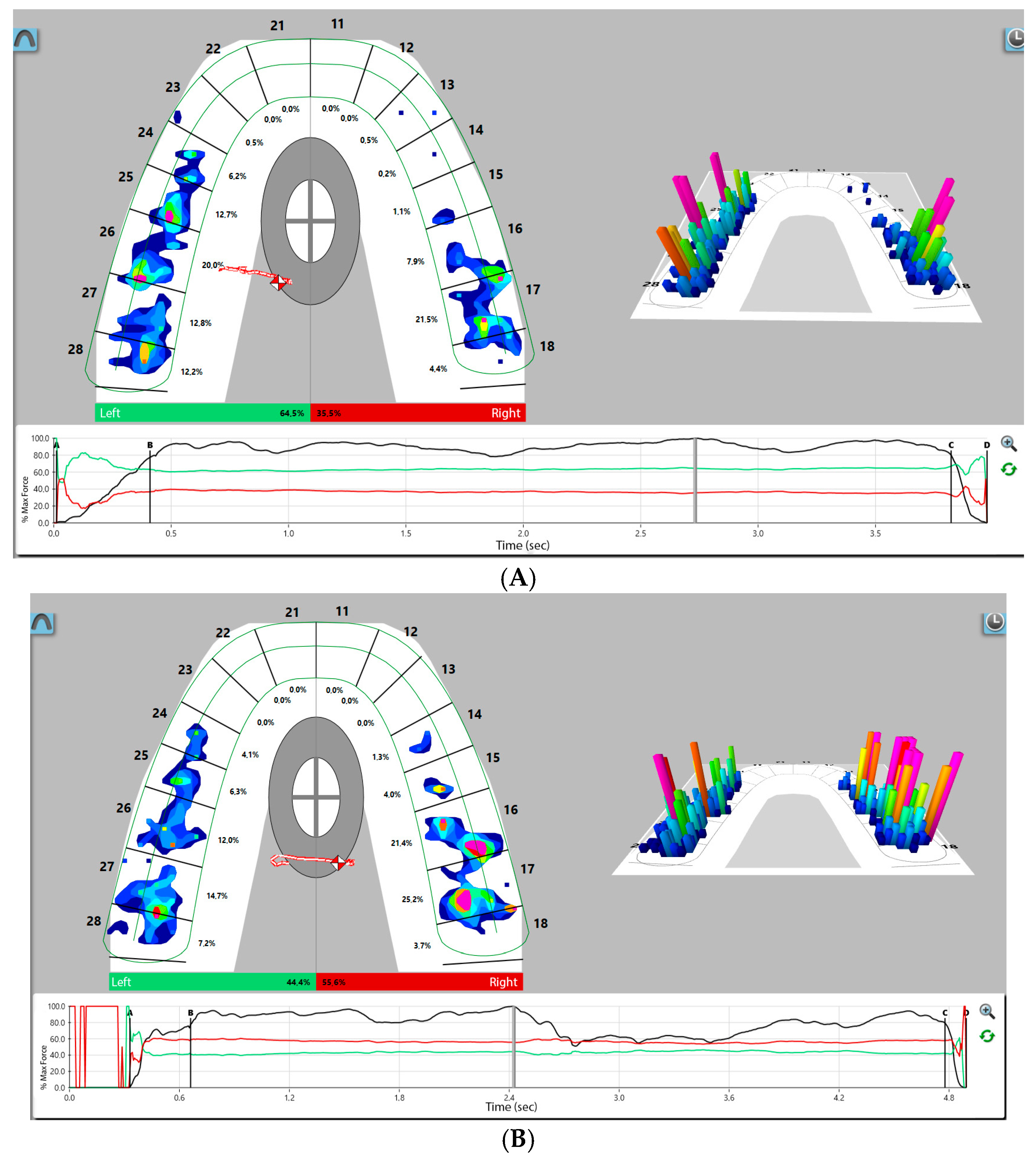
2.4. Digital Occlusal Analysis
2.5. Enameloplasty
2.6. Statistical Analysis
3. Results
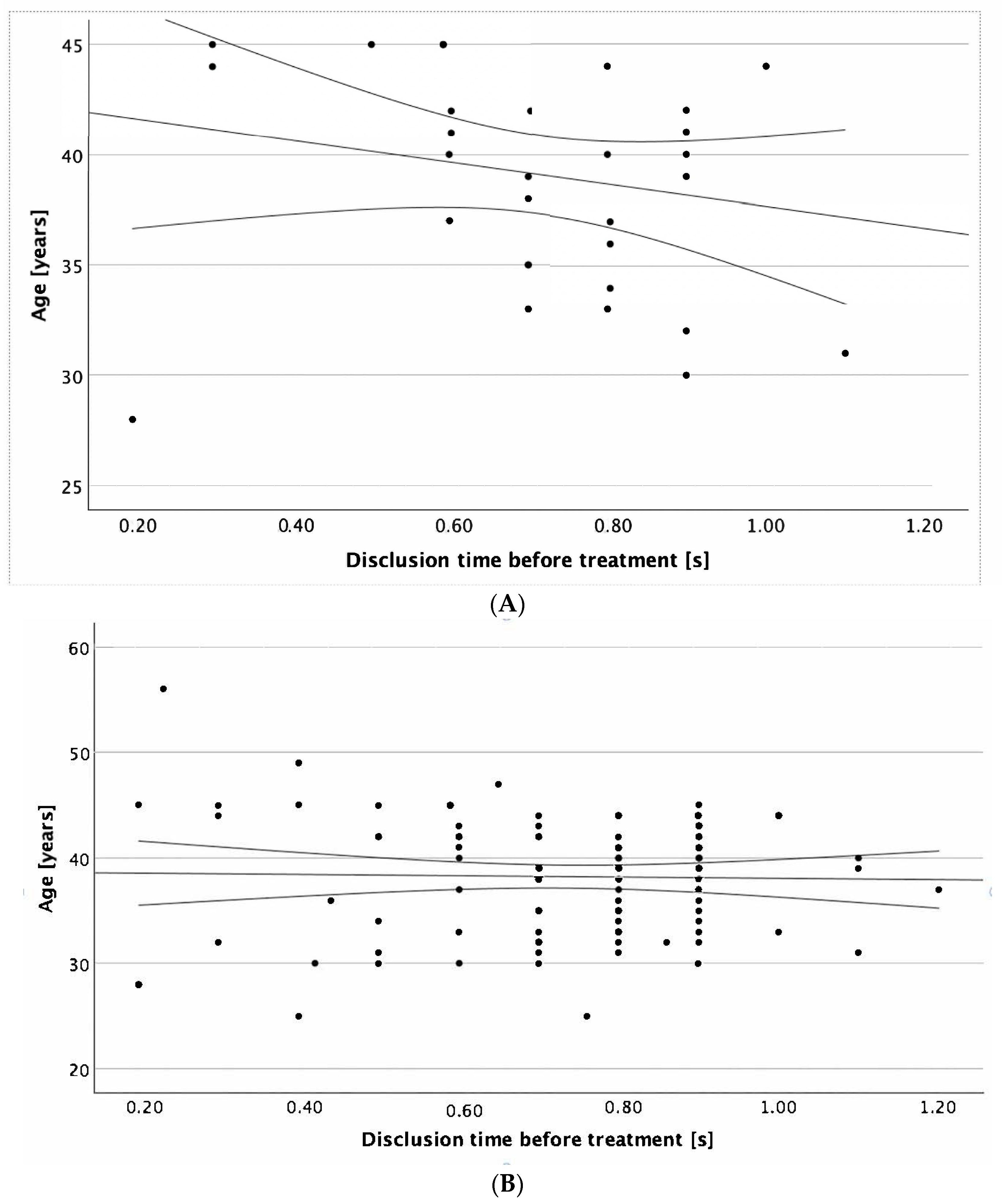
3.1. Demographic and Clinical Characteristics of Subjects
3.2. Clinical Characteristics of Subjects Depending on the Center of the Force
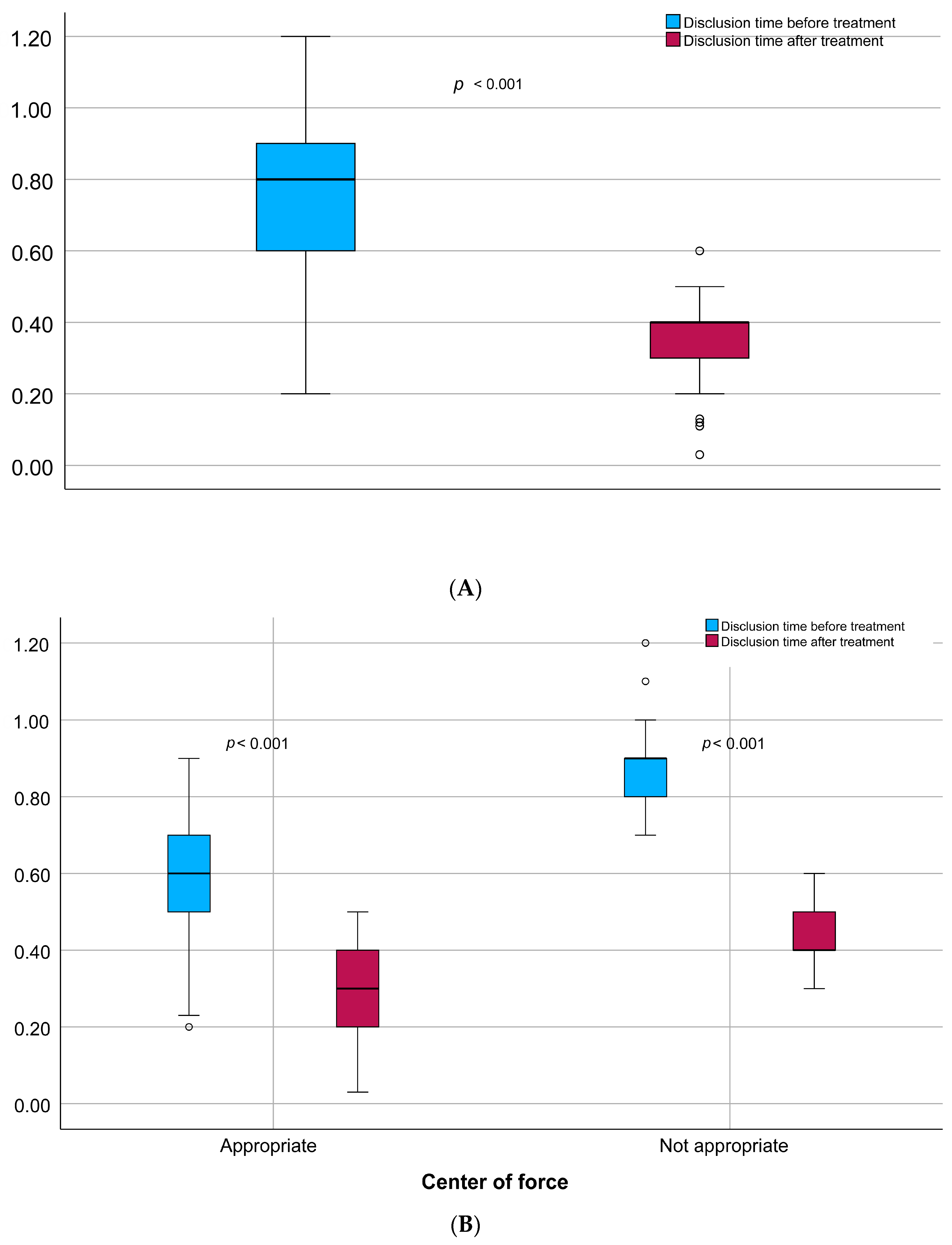
3.3. Disclusion Time Changes Before and After the Enameloplasty
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Madani, A.S.; Nakhaei, M.; Alami, M.; Haghi, H.R.; Moazzami, S.M. Post-insertion posterior single-implant occlusion changes at different intervals: A T-Scan computerized occlusal analysis. J. Contemp. Dent. Pract. 2017, 18, 927–932. [Google Scholar] [CrossRef]
- Aldowish, A.F.; Alsubaie, M.N.; Alabdulrazzaq, S.S.; Alsaykhan, D.B.; Alamri, A.K.; Alhatem, L.M.; Algoufi, J.F.; Alayed, S.S.; Aljadani, S.S.; Alashjai, A.M.; et al. Occlusion and Its Role in the Long-Term Success of Dental Restorations: A Literature Review. Cureus 2024, 16, e73195. [Google Scholar] [CrossRef]
- Ferrario, V.F.; Serrao, G.; Dellavia, C.; Caruso, E.; Sforza, C. Relationship between the number of occlusal contacts and masticatory muscle activity in healthy young adults. Cranio 2002, 20, 91–98. [Google Scholar] [CrossRef]
- Kerstein, R.B.; Radke, J. Masseter and temporalis excursive hyperactivity decreased by measured anterior guidance development. Cranio 2012, 30, 243–254. [Google Scholar] [CrossRef] [PubMed]
- Kapos, F.P.; Exposto, F.G.; Oyarzo, J.F.; Durham, J. Temporomandibular disorders: A review of current concepts in aetiology, diagnosis and management. Oral Surg. 2020, 13, 321–334. [Google Scholar] [CrossRef] [PubMed]
- Patano, A.; Malcangi, G.; Inchingolo, A.D.; Garofoli, G.; De Leonardis, N.; Azzollini, D.; Latini, G.; Mancini, A.; Carpentiere, V.; Laudadio, C.; et al. Mandibular Crowding: Diagnosis and Management-A Scoping Review. J. Pers. Med. 2023, 13, 774. [Google Scholar] [CrossRef] [PubMed]
- Kerstein, R.B. Reducing chronic masseter and temporalis muscular hyperactivity with computer-guided occlusal adjustments. Compend. Contin. Educ. Dent. 2010, 31, 530–534. [Google Scholar]
- Kerstein, R.B.; Wright, N.R. Electromyographic and computer analyses of patients suffering from chronic myofascial pain-dysfunction syndrome: Before and after treatment with immediate complete anterior guidance development. J. Prosthet. Dent. 1991, 66, 677–686. [Google Scholar] [CrossRef]
- Watanabe, E.K.; Yatani, H.; Kuboki, T.; Matsuka, Y.; Terada, S.; Orsini, M.G.; Yamashita, A. The relationship between signs and symptoms of temporomandibular disorders and bilateral occlusal contact patterns during lateral excursions. J. Oral Rehabil. 1998, 25, 409–415. [Google Scholar] [CrossRef]
- Thumati, P.; Thumati, R.P.; Poovani, S.; Sattur, A.P.; Srinivas, S.; Kerstein, R.B.; Radke, J. A Multi-Center Disclusion Time Reduction (DTR) randomized controlled occlusal adjustment study using occlusal force and timing sensors synchronized with muscle physiology sensors. Sensors 2021, 21, 7804. [Google Scholar] [CrossRef]
- Albagieh, H.; Alomran, I.; Binakresh, A.; Alhatarisha, N.; Almeteb, M.; Khalaf, Y.; Alqublan, A.; Alqahatany, M. Occlusal splints-types and effectiveness in temporomandibular disorder management. Saudi Dent. J. 2023, 35, 70–79. [Google Scholar] [CrossRef]
- Busse, J.W.; Casassus, R.; Carrasco-Labra, A.; Durham, J.; Mock, D.; Zakrzewska, J.M.; Palmer, C.; Samer, C.F.; Coen, M.; Guevremont, B.; et al. Management of chronic pain associated with temporomandibular disorders: A clinical practice guideline. BMJ 2023, 383, e076227. [Google Scholar] [CrossRef]
- Yuan, J.C.; Sukotjo, C. Occlusion for implant-supported xed dental prostheses in partially edentulous patients: A literature review and current concepts. J. Periodontal Implant. Sci. 2013, 43, 51–57. [Google Scholar] [CrossRef] [PubMed]
- Schiffman, E.; Ohrbach, R.; Truelove, E.; Look, J.; Anderson, G.; Goulet, J.-P.; List, T.; Svensson, P.; Gonzalez, Y.; Lobbezoo, F.; et al. Diagnostic Criteria for Temporomandibular Disorders (DC/TMD) for clinical and research applications: Recommendations of the international RDC/TMD Consortium Network* and Orofacial Pain Special Interest Group†. J. Oral Facial Pain Headache 2014, 28, 6–27. [Google Scholar] [CrossRef] [PubMed]
- Osiewicz, M.; Lobbezoo, F.; Loster, B.; Wilkosz, M.; Naeije, M.; Ohrbach, R. Research Diagnostic Criteria for Temporomandibular Disorders (RDC/TMD)—The Polish version of a dual-axis system for the diagnosis of TMD.*RDC/TMD Form. J. Stoma. 2013, 66, 576–649. [Google Scholar] [CrossRef]
- Thumati, P. The influence of immediate complete anterior guidance development technique on subjective symptoms in Myofascial pain patients: Verified using digital analysis of occlusion (Tek-scan) for analysing occlusion: A 3 years clinical observation. J. Indian Prosthodont. Soc. 2015, 15, 218–223. [Google Scholar] [CrossRef]
- Thumati, P.; Manwani, R.; Mahantshetty, M. The effect of reduced disclusion time in the treatment of myofascial pain dysfunction syndrome using immediate complete anterior guidance development protocol monitored by digital analysis of occlusion. Cranio 2014, 32, 289–299. [Google Scholar] [CrossRef]
- Kerstein, R.B.; Chapman, R.; Klein, M. A comparison of ICAGD immediate complete anterior guidance development to mock ICAGD for symptom reductions in chronic myofascial pain dysfunction patients. Cranio 1997, 15, 21–37. [Google Scholar] [CrossRef]
- Thumati, P.; Poovani, S.; Ayinala, A. A retrospective five-year survey on the treatment outcome of disclusion time reduction (DTR) therapy in treating temporomandibular dysfunction patients. Cranio 2023, 41, 494–500. [Google Scholar] [CrossRef]
- Revuru, P.; Mc, S.S. Influence of disclusion time reduction on changes in posterior implant prosthesis occlusion and its association with crestal bone loss: A clinical study. J. Prosthet. Dent. 2025, 133, 1024.e1–1024.e11. [Google Scholar] [CrossRef]
- Abutayyem, H.; Annamma, L.M.; Desai, V.B.; Alam, M.K. Evaluation of occlusal bite force distribution by T-Scan in orthodontic patients with different occlusal characteristics: A cross sectional-observational study. BMC Oral Health 2023, 23, 888. [Google Scholar] [CrossRef] [PubMed]
- Kerstein, R.B.; Radke, J. The effect of Disclusion Time reduction on maximal clench muscle activity levels. Cranio 2006, 24, 156–165. [Google Scholar] [CrossRef]
- Carey, J.P.; Craig, M.; Kerstein, R.B.; Radke, J. Determining a relationship between applied occlusal load and articulating paper mark area. Open Dent. J. 2007, 1, 1–7. [Google Scholar] [CrossRef]
- Chaithanya, R.; Sajjan, S.; Raju, A.V.R. A study of change in occlusal contacts and force dynamics after xed prosthetic treatment and after equilibration—Using Tekscan III. J Indian Prosthodont. Soc. 2019, 19, 9–19. [Google Scholar] [CrossRef]
- Kim, Y.; Oh, T.J.; Misch, C.E.; Wang, H.L. Occlusal considerations in implant therapy: Clinical guidelines with biomechanical rationale. Clin. Oral Implant. Res. 2005, 16, 26–35. [Google Scholar] [CrossRef]
- Qadeer, S.; Ozcan, M.; Edelhoff, D.; van Pelt, H. Accuracy, reliability and clinical implications of static compared to quanti able occlusal indicators. Eur. J. Prosthodont. Restor. Dent. 2021, 31, 130–141. [Google Scholar]
| Gender, n (%) [Female] | 73 (68.9%) |
| Center of force, n (%) [Appropriate] | 49 (46.2%) |
| Premature occlusal contacts, n (%) [Yes] | 75 (70.8%) |
| Age, IQR (95%CI) [years] | 39 (33; 43) |
| Disclusion time before treatment, IQR (95%CI) [s] | 0.80 (0.60; 0.90) |
| Disclusion time after treatment, IQR (95%CI) [s] | 0.40 (0.30; 0.40) |
| Disclusion time difference before-after, IQR (95%CI) [s] | 0.40 (0.20; 0.50) |
| Right site, IQR (95%CI) | 51.50 (44.07; 57.64) |
| Left site, IQR (95%CI) | 48.50 (42.36; 55.93) |
| Site difference right–left, IQR (95%CI) | 3.00 (−11.86; 15.28) |
| Maximal bite force, IQR (95%CI) [N] | 90.13 (84.58; 95.11) |
| Occlusion time before treatment IQR (95%CI) [s] | 0.35 (0.26; 0.42) |
| Occlusion time after treatment, IQR (95%CI) [s] | 0.35 (0.28; 0.42) |
| Occlusion time difference before-after, IQR (95%CI) [s] | −0.02 (−0.08; 0.08) |
| Center of the Force | p-Value | ||
|---|---|---|---|
| Appropriate n = 49 | Not Appropriate n = 57 | ||
| Gender, n (%) [Female] | 30 (61.2%) | 43 (75.4%) | 0.142 |
| Age, IQR (95%CI) [years] | 39 (33; 44) | 39 (33; 42) | 0.489 |
| Disclusion time before treatment, IQR (95%CI) [s] | 0.60 (0.50; 0.70) | 0.90 (0.80; 0.90) | <0.001 |
| Disclusion time after treatment, IQR (95%CI) [s] | 0.30 (0.20; 0.40) | 0.40 (0.40; 0.50) | <0.001 |
| Disclusion time difference before-after, IQR (95%CI) [s] | 0.29 (0.19; 0.39) | 0.40 (0.40; 0.50) | <0.001 |
| Right site, IQR (95%CI) | 50.86 (46.93; 54.07) | 57.64 (40.64; 61.50) | 0.437 |
| Left site, IQR (95%CI) | 49.14 (45.93; 53.07) | 42.36 (38.50; 59.36) | 0.437 |
| Site difference right–left, IQR (95%CI) | 1.72 (−6.14; 8.14) | 15.28 (−18.72; 23.00) | 0.437 |
| Maximal bite force, IQR (95%CI) [N] | 90.59 (85.70; 94.52) | 88.21 (83.73; 96.07) | 0.470 |
| Occlusion time before treatment IQR (95%CI) [s] | 0.32 (0.23; 0.43) | 0.36 (0.30; 0.42) | 0.20 |
| Occlusion time after treatment, IQR (95%CI) [s] | 0.34 (0.27; 0.41) | 0.35 (0.28; 0.44) | 0.329 |
| Occlusion time difference before-after, IQR (95%CI) [s] | −0.03 (−0.07; 0.07) | 0.01 (−0.08; 0.08) | 0.676 |
| Premature occlusal contacts, n (%) [Yes] | 18 (36.7%) | 57 (100%) | <0.001 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Maga, W.; Schönborn, M.; Pihut, M. The Effect of Selective Occlusal Adjustment on the Disclusion Time Reduction and Symmetry of Occlusal Contacts of the Own Dentition Using Digital Occlusion Analysis in Patients with Temporomandibular Disorders. J. Clin. Med. 2025, 14, 7007. https://doi.org/10.3390/jcm14197007
Maga W, Schönborn M, Pihut M. The Effect of Selective Occlusal Adjustment on the Disclusion Time Reduction and Symmetry of Occlusal Contacts of the Own Dentition Using Digital Occlusion Analysis in Patients with Temporomandibular Disorders. Journal of Clinical Medicine. 2025; 14(19):7007. https://doi.org/10.3390/jcm14197007
Chicago/Turabian StyleMaga, Wojciech, Martyna Schönborn, and Małgorzata Pihut. 2025. "The Effect of Selective Occlusal Adjustment on the Disclusion Time Reduction and Symmetry of Occlusal Contacts of the Own Dentition Using Digital Occlusion Analysis in Patients with Temporomandibular Disorders" Journal of Clinical Medicine 14, no. 19: 7007. https://doi.org/10.3390/jcm14197007
APA StyleMaga, W., Schönborn, M., & Pihut, M. (2025). The Effect of Selective Occlusal Adjustment on the Disclusion Time Reduction and Symmetry of Occlusal Contacts of the Own Dentition Using Digital Occlusion Analysis in Patients with Temporomandibular Disorders. Journal of Clinical Medicine, 14(19), 7007. https://doi.org/10.3390/jcm14197007







