Psychological and Behavioral Adjustment in Patients with Non-Traumatic Lower Limb Amputation and Prosthesis: A Mixed-Method Triangulation Study
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design
2.2. Participants
2.3. Instruments
2.3.1. Qualitative Part: Semi-Structured Interviews
- Form A (pre-amputation phase): explored emotional response, treatment adherence, and quality of life following diagnosis of diabetes or vascular disease;
- Form B (post-amputation phase): addressed psychological impact, stump management, body image, and emotional well-being post-surgery;
- Form C (prosthesis use phase): investigated emotional and functional adjustment to prosthesis, autonomy, and self-image at discharge of a rehabilitation program aiming to adapt to prosthesis.
2.3.2. Quantitative Part: Psychometric Assessments
- EuroQol Visual Analogue Scale (EQ-VAS):
- Generalized Anxiety Disorder-7 (GAD-7):
- Patient Health Questionnaire-9 (PHQ-9):
- Antecedents and Self-Efficacy on Adherence (ASonA):
- Body Image Scale (BIS):
- Trinity Amputation and Prosthesis Experience Scales (TAPES):
2.4. Procedure
2.5. Data Analysis
- (a)
- Amputees—Quantitative;
- (b)
- Amputees—Qualitative;
- (c)
- Prosthesis users—Quantitative;
- (d)
- Prosthesis users—Qualitative.
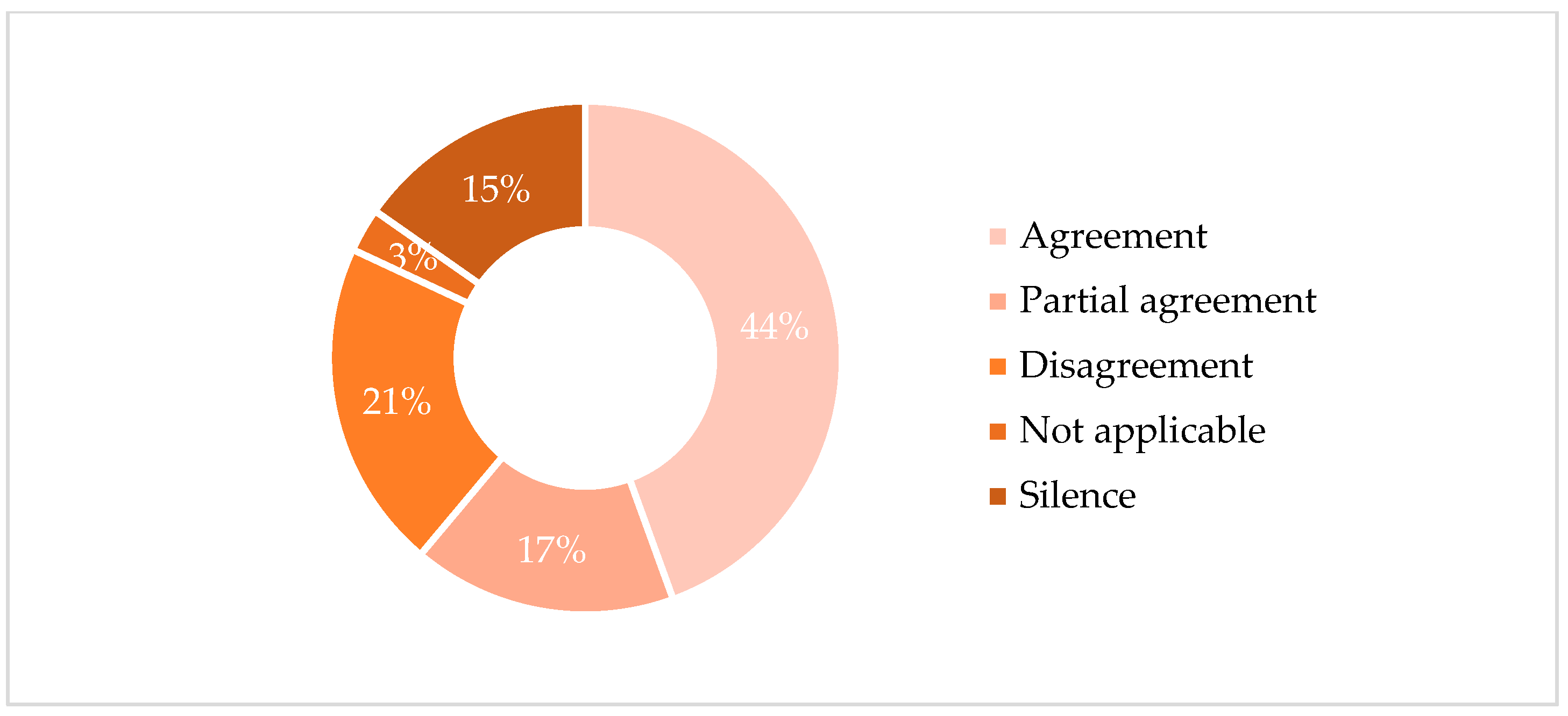
- Agreement is defined as a complete conceptual alignment between the datasets, where both sources address the same construct with consistent interpretations (e.g., both qualitative themes and quantitative results clearly indicated high levels of distress).
- Partial Agreement refers to complementary, but not fully overlapping, findings. This includes cases where one dataset expanded or nuanced the other, or when the alignment was present but not strong or consistent across all participants.
- Disagreement is assigned when findings from different sources directly contradicted each other (e.g., a quantitative score indicating high adherence while the qualitative narrative revealed significant treatment avoidance).
- Silence indicates that a construct emerged in only one of the two datasets, with no mention or measurable data in the other.
- Not Applicable is used when neither dataset contained information related to the construct in question [23].
3. Results
3.1. Sample Characteristics
3.2. Quantitative Data
3.3. Triangulation Data
3.3.1. Comparisons
3.3.2. Key Findings
Acceptance and Adjustment
- Illness acceptance
- Adaptation to the Prosthesis
- Body Image
Adherence
- Pharmacological and Behavioral Adherence
Psychological and Emotional Experience
- Anxiety Symptoms
- Depressive Symptoms
- Quality of Life
Coping and Protective Factors
- Denial
- Optimism
- Family and Social Support
4. Discussion
Strengths, Limitations, and Future Directions
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| LLA | Lower limb amputation |
| PAD | Peripheral artery disease |
| DM | Diabetes mellitus |
| EQ-VAS | EuroQol Visual Analogue Scale |
| GAD-7 | Generalized Anxiety Disorder-7 |
| PHQ-9 | Patient Health Questionnaire-9 |
| ASonA | Antecedents and Self-Efficacy on Adherence |
| BIS | Body Image Scale |
| TAPES | Trinity Amputation and Prosthesis Experience Scales |
Appendix A
| Convergence Category | Amputees Quantitative | Amputees Qualitative | Prosthesis Users Quantitative | Prosthesis Users Qualitative | Agreement |
|---|---|---|---|---|---|
| ACCEPTANCE AND ADJUSTMENT | |||||
| Illness acceptance | Most patients report having accepted their medical condition (ASonA_01: 2.50 ± 1.45; range: 0–4). | Most patients verbally express passive acceptance of their clinical condition. | Most patients report having accepted their medical condition (ASonA_01: 3.00 ± 1.24; range: 0–4). | Most patients verbally express passive acceptance of their clinical condition, although there is positivity related to the hope of functional recovery thanks to the prosthesis. | Agreement: 1 × 3, 2 × 4 (=2) Partial agreement: 1 × 2, 1 × 4, 2 × 3, 3 × 4 (=4) |
| Adaptation to the prosthesis | Silence | Silence | All patients report having adapted to the prosthesis (TAPES_01: 4.57 ± 0.51; range: 4–5). | Almost all patients report having adapted to the prosthesis, although several report physical fatigue and perceiving the prosthesis as a foreign body. | Agreement: 3 × 4 (=1) Silence: 1 × 3; 1 × 4; 2 × 3; 2 × 4 (=4) Not applicable: 1 × 2 (=1) |
| Body image | Several patients report feeling good about the physical changes resulting from their medical condition (BIS: 6.43 ± 6.90; range 0–21). | No difficulties regarding body image are reported, although some mention limb loss and phantom limb. | Several patients report feeling good about the physical changes resulting from their medical condition (BIS: 6.07 ± 8.56; range: 0–25). | Although most patients report feeling good with their prosthesis thanks to the functional recovery obtained, several express fear of others’ judgment and refer to the presence of phantom limb. | Agreement: 1 × 3, 2 × 4 (=2) Partial agreement: 1 × 2, 1 × 4, 2 × 3, 3 × 4 (=4) |
| ADHERENCE | |||||
| Pharmacological adherence | All patients report adhering to medical prescriptions (ASonA_08: 3.57 ± 0.51; range: 0–4). | Most patients say they do not adequately adhere to prescriptions due to forgetfulness and/or lack of perceived benefit. | All patients report adhering to medical prescriptions (ASonA_08: 3.57 ± 0.94; range: 0–4). | All patients express willingness to adhere to medical prescriptions and to perform the recommended physiotherapy to improve their health and gain greater well-being and autonomy. | Agreement: 1 × 3; 1 × 4; 3 × 4 (=3) Disagreement: 1 × 2; 2 × 3; 2 × 4 (=3) |
| Behavioral adherence | All patients report following a healthy lifestyle (ASonA_09: 3.05 ± 1.35; range: 0–4). | Most patients say they do not follow a healthy lifestyle, not limiting food and consuming alcohol or sugary drinks. | All patients report following a healthy lifestyle (ASonA_09: 3.05 ± 1.62; range: 0–4). | All patients express the desire to improve their eating habits and adopt a healthy lifestyle. | Agreement: 1 × 3; 1 × 4; 3 × 4 (=3) Disagreement: 1 × 2; 2 × 3; 2 × 4 (=3) |
| EMOTIONAL EXPERIENCE | |||||
| Anxiety | The sample reports a mild level of anxiety (GAD-07: 4.71 ± 5.40; range: 0–21). | Most patients report moderate anxiety symptoms, mainly related to worries about the future. | The sample reports a mild level of anxiety (GAD-07: 4.29 ± 5.81; range: 0–21). | Although some patients report concerns about returning home, most show positivity, motivation, and hope for recovery. | Agreement: 1 × 3 (=1) Partial agreement: 1 × 4, 3 × 4 (=2) Disagreement: 1 × 2; 2 × 3, 2 × 4 (=3) |
| Depression | The entire sample reports a subthreshold level of depression (PHQ-9: 4.07 ± 4.60; range: 0–27). | Most patients report marked low mood due to disappointment about the diagnosis and loss of their health. | The entire sample reports a subthreshold level of depression (PHQ-9: 3.57 ± 4.01; range: 0–27). | Most patients report an improvement in mood following adaptation to the prosthesis and the benefits derived from it. | Agreement: 1 × 3 (=1) Partial agreement: 1 × 4, 3 × 4 (=2) Disagreement: 1 × 2, 2 × 3, 2 × 4 (=3) |
| Quality of life | Most patients perceive themselves to be in good health and to have good quality of life (EQ-VAS: 66.79 ± 21.89; range 20–100). | Almost all patients report experiencing a worsening in their quality of life due to loss of autonomy and increased difficulty performing daily activities. | Most patients perceive themselves to be in good health and to have good quality of life (EQ-VAS: 78.85 ± 17.10; range 50–100). | Almost all patients report an improvement in quality of life thanks to regained autonomy and partial independence. | Agreement: 1 × 3, 1 × 4, 3 × 4 (=3) Disagreement: 1 × 2, 2 × 3, 2 × 4 (=3) |
| Denial | Silence | Almost all patients show emotional detachment and denial of the event, both of the disease diagnosis and the limb amputation. | Silence | Most patients show emotional distance and denial of the impact of their clinical condition, especially regarding the diabetes diagnosis. | Agreement: 2 × 4 (=1) Silence: 1 × 2, 1 × 4, 2 × 3, 3 × 4 (=4) Not applicable: 1 × 3 (=1) |
| Optimism | Most patients consider themselves optimistic about their health (AsonA_10h: 2.57 ± 1.50; range 0–4). | Several patients report positive future expectations about their clinical and functional recovery after amputation. | Most patients consider themselves optimistic about their health (AsonA_10h: 3.00 ± 1.35; range 0–4). | Several patients report being positive about regaining their autonomy and progress with the prosthesis. | Agreement: 1 × 2; 1 × 3; 1 × 4, 2 × 3; 2 × 4; 3 × 4 (=6) |
| PERCEIVED SUPPORT | |||||
| Family | Almost all patients report receiving good support from their family (ASonA_03: 3.43 ± 0.85; range: 0–4). | Several patients report receiving excellent support from their family. | Almost all patients report receiving good support from their family (ASonA_03: 3.21 ± 1.42; range: 0–4). | Almost all patients report receiving excellent support from their family. | Agreement: 1 × 2; 1 × 3; 1 × 4, 2 × 3; 2 × 4; 3 × 4 (=6) |
| Social support | Several patients report receiving fair support from their network of friends (ASonA_04: 1.86 ± 1.46; range: 0–4). | Silence | Several patients report receiving adequate support from their network of friends (ASonA_04: 2.50 ± 1.87; range: 0–4). | Some patients report receiving support from their social network. | Agreement: 1 × 3; 1 × 4; 3 × 4 (=3) Silence: 1 × 2; 2 × 3; 2 × 4 (=3) |
| Total (=72) Agreement (n = 32) Partial Agreement (n = 12) Disagreement (n = 15) Silence (n = 11) Not Applicable (n = 2) | |||||
References
- Markatos, K.; Karamanou, M.; Saranteas, T.; Mavrogenis, A.F. Hallmarks of Amputation Surgery. Int. Orthop. (SICOT) 2019, 43, 493–499. [Google Scholar] [CrossRef] [PubMed]
- Creager, M.A.; Matsushita, K.; Arya, S.; Beckman, J.A.; Duval, S.; Goodney, P.P.; Gutierrez, J.A.T.; Kaufman, J.A.; Joynt Maddox, K.E.; Pollak, A.W.; et al. Reducing Nontraumatic Lower-Extremity Amputations by 20% by 2030: Time to Get to Our Feet: A Policy Statement From the American Heart Association. Circulation 2021, 143, e875–e891. [Google Scholar] [CrossRef]
- Di Giovanni, P.; Scampoli, P.; Meo, F.; Cedrone, F.; D’Addezio, M.; Di Martino, G.; Valente, A.; Romano, F.; Staniscia, T. The Impact of Gender on Diabetes-Related Lower Extremity Amputations: An Italian Regional Analysis on Trends and Predictors. Foot Ankle Surg. 2021, 27, 25–29. [Google Scholar] [CrossRef]
- Lopez-de-Andres, A.; Jimenez-Garcia, R.; Hernandez-Barrera, V.; De Miguel-Diez, J.; De Miguel-Yanes, J.M.; Omaña-Palanco, R.; Carabantes-Alarcon, D. Trends of Non-Traumatic Lower-Extremity Amputation and Type 2 Diabetes: Spain, 2001–2019. J. Clin. Med. 2022, 11, 1246. [Google Scholar] [CrossRef]
- Lombardo, F.L.; Maggini, M.; De Bellis, A.; Seghieri, G.; Anichini, R. Lower Extremity Amputations in Persons with and without Diabetes in Italy: 2001–2010. PLoS ONE 2014, 9, e86405. [Google Scholar] [CrossRef]
- Al Agha, R.; Muneer, H.; Alqaseer, A. Major Lower Limb Amputation: Causes, Characteristics and Complications. Bahrain Med. Bull. 2017, 39, 159–161. [Google Scholar] [CrossRef]
- Al-Rubeaan, K.; Al Derwish, M.; Ouizi, S.; Youssef, A.M.; Subhani, S.N.; Ibrahim, H.M.; Alamri, B.N. Diabetic Foot Complications and Their Risk Factors from a Large Retrospective Cohort Study. PLoS ONE 2015, 10, e0124446. [Google Scholar] [CrossRef]
- Soyoye, D.O.; Abiodun, O.O.; Ikem, R.T.; Kolawole, B.A.; Akintomide, A.O. Diabetes and Peripheral Artery Disease: A Review. World J. Diabetes 2021, 12, 827–838. [Google Scholar] [CrossRef] [PubMed]
- Jeffcoate, W.; Game, F.; Morbach, S.; Narres, M.; Van Acker, K.; Icks, A. Assessing Data on the Incidence of Lower Limb Amputation in Diabetes. Diabetologia 2021, 64, 1442–1446. [Google Scholar] [CrossRef]
- Margolis, D.J.; Malay, D.S.; Hoffstad, O.J.; Leonard, C.E.; MaCurdy, T.; López de Nava, K.; Tan, Y.; Molina, T.; Siegel, K.L. Incidence of Diabetic Foot Ulcer and Lower Extremity Amputation among Medicare Beneficiaries, 2006 to 2008; Agency for Healthcare Research and Quality (US): Rockville, MD, USA, 2011. [Google Scholar]
- Tao, G.-L.; Zheng, L.-S.; Wang, Z.-Y.; Xu, Y.-P.; Zhong, X.-G.; Wang, H.; Zhang, X.-S. Clinical Characteristics and Risk Factors of Diabetic Foot Ulcers with PAD. Eur. Rev. Med. Pharmacol. Sci. 2023, 27, 11412–11420. [Google Scholar] [CrossRef] [PubMed]
- Chimen, M.; Kennedy, A.; Nirantharakumar, K.; Pang, T.T.; Andrews, R.; Narendran, P. What Are the Health Benefits of Physical Activity in Type 1 Diabetes Mellitus? A Literature Review. Diabetologia 2012, 55, 542–551. [Google Scholar] [CrossRef]
- Zhang, Y.; Pan, X.-F.; Chen, J.; Xia, L.; Cao, A.; Zhang, Y.; Wang, J.; Li, H.; Yang, K.; Guo, K.; et al. Combined Lifestyle Factors and Risk of Incident Type 2 Diabetes and Prognosis among Individuals with Type 2 Diabetes: A Systematic Review and Meta-Analysis of Prospective Cohort Studies. Diabetologia 2020, 63, 21–33. [Google Scholar] [CrossRef]
- Jeon, B.; Choi, H.J.; Kang, J.S.; Tak, M.S.; Park, E.S. Comparison of Five Systems of Classification of Diabetic Foot Ulcers and Predictive Factors for Amputation. Int. Wound J. 2017, 14, 537–545. [Google Scholar] [CrossRef] [PubMed]
- Ramstrand, S.; Carlberg, M.; Jarl, G.; Johannesson, A.; Hiyoshi, A.; Jansson, S. Exploring Potential Risk Factors for Lower Limb Amputation in People with Diabetes—A National Observational Cohort Study in Sweden. J. Foot Ankle Res. 2024, 17, e70005. [Google Scholar] [CrossRef]
- Jiang, S.; Zhu, Z.; Liao, G.; Huang, Y.; Li, L.; Zeng, K. Relationship Between Medication Literacy and Beliefs Among Persons with Type 2 Diabetes Mellitus in Guangdong, China. Patient Prefer. Adherence 2023, 17, 2039–2050. [Google Scholar] [CrossRef]
- Yoo, J.E.; Lee, D.; Kim, B.; Chang, W.H.; Jin, S.-M.; Han, K.; Shin, D.W. Increased Risk of Type 2 Diabetes after Traumatic Amputation: A Nationwide Retrospective Cohort Study. Front. Endocrinol. 2025, 15, 1437860. [Google Scholar] [CrossRef] [PubMed]
- Şimsek, N.; Öztürk, G.K.; Nahya, Z.N. The Mental Health of Individuals With Post-Traumatic Lower Limb Amputation: A Qualitative Study. J. Patient Exp. 2020, 7, 1665–1670. [Google Scholar] [CrossRef]
- Calabrese, L.; Maffoni, M.; Torlaschi, V.; Pierobon, A. What Is Hidden behind Amputation? Quanti-Qualitative Systematic Review on Psychological Adjustment and Quality of Life in Lower Limb Amputees for Non-Traumatic Reasons. Healthcare 2023, 11, 1661. [Google Scholar] [CrossRef]
- Senra, H.; Oliveira, R.A.; Leal, I.; Vieira, C. Beyond the Body Image: A Qualitative Study on How Adults Experience Lower Limb Amputation. Clin. Rehabil. 2012, 26, 180–191. [Google Scholar] [CrossRef] [PubMed]
- Pedras, S.; Vilhena, E.; Carvalho, R.; Pereira, M.G. Psychosocial Adjustment to a Lower Limb Amputation Ten Months after Surgery. Rehabil. Psychol. 2018, 63, 418–430. [Google Scholar] [CrossRef]
- Bergen, N.; Labonté, R. “Everything Is Perfect, and We Have No Problems”: Detecting and Limiting Social Desirability Bias in Qualitative Research. Qual. Health Res. 2020, 30, 783–792. [Google Scholar] [CrossRef] [PubMed]
- Tonkin-Crine, S.; Anthierens, S.; Hood, K.; Yardley, L.; Cals, J.W.L.; Francis, N.A.; Coenen, S.; Van Der Velden, A.W.; Godycki-Cwirko, M.; Llor, C.; et al. Discrepancies between Qualitative and Quantitative Evaluation of Randomised Controlled Trial Results: Achieving Clarity through Mixed Methods Triangulation. Implement. Sci 2015, 11, 66. [Google Scholar] [CrossRef] [PubMed]
- Östlund, U.; Kidd, L.; Wengström, Y.; Rowa-Dewar, N. Combining qualitative and quantitative research within mixed method research designs: A methodological review. Int. J. Nurs. Stud. 2011, 48, 369–383. [Google Scholar] [CrossRef]
- Jones, A.; Bugge, C. Improving understanding and rigour through triangulation: An exemplar based on patient participation in interaction. J. Adv. Nurs. 2006, 55, 612–621. [Google Scholar] [CrossRef]
- Foderaro, G.; Isella, V.; Mazzone, A.; Biglia, E.; Di Gangi, M.; Pasotti, F.; Sansotera, F.; Grobberio, M.; Raimondi, V.; Mapelli, C.; et al. Brand New Norms for a Good Old Test: Northern Italy Normative Study of MiniMental State Examination. Neurol. Sci. 2022, 43, 3053–3063. [Google Scholar] [CrossRef]
- DiMatteo, M.R.; Haskard-Zolnierek, K.B.; Martin, L.R. Improving Patient Adherence: A Three-Factor Model to Guide Practice. Health Psychol. Rev. 2012, 6, 74–91. [Google Scholar] [CrossRef]
- Rabin, R.; Charro, F.D. EQ-SD: A Measure of Health Status from the EuroQol Group. Ann. Med. 2001, 33, 337–343. [Google Scholar] [CrossRef]
- Savoia, E.; Fantini, M.P.; Pandolfi, P.P.; Dallolio, L.; Collina, N. Assessing the Construct Validity of the Italian Version of the EQ-5D: Preliminary Results from a Cross-Sectional Study in North Italy. Health Qual. Life Outcomes 2006, 4, 47. [Google Scholar] [CrossRef]
- Spitzer, R.L.; Kroenke, K.; Williams, J.B.W.; Löwe, B. A Brief Measure for Assessing Generalized Anxiety Disorder: The GAD-7. Arch. Intern. Med. 2006, 166, 1092. [Google Scholar] [CrossRef] [PubMed]
- Kroenke, K.; Spitzer, R.L.; Williams, J.B.W. The PHQ-9: Validity of a Brief Depression Severity Measure. J. Gen. Intern. Med. 2001, 16, 606–613. [Google Scholar] [CrossRef] [PubMed]
- Zanatta, F.; Nissanova, E.; Świątoniowska-Lonc, N.; Pierobon, A.; Callegari, G.; Olmetti, F.; Felicetti, G.; Karniej, P.; Polański, J.; Giardini, A.; et al. Psychosocial Predictors of Self-Efficacy Related to Self-Reported Adherence in Older Chronic Patients Dealing with Hypertension: A European Study. Patient Prefer. Adherence 2020, 14, 1709–1718. [Google Scholar] [CrossRef]
- Cheli, S.; Agostini, A.; Herd-Smith, A.; Caligiani, L.; Martella, F.; Fioretto, L. The Italian version of Body Image Scale Reliability and Sensitivity in a sample of breast cancer patients. Psicoter. Cogn. Comport. 2016, 22, 65–79. [Google Scholar]
- Annunziata, M.A.; Muzzatti, B.; Bomben, F.; Flaiban, C.; Piccinin, M.; Solfrini, V. A Contribution to the Validation of the Italian Version of the Body Image Scale (BIS). BMC Cancer 2018, 18, 1222. [Google Scholar] [CrossRef]
- Gallagher, P.; MacLachlan, M. Development and Psychometric Evaluation of the Trinity Amputation and Prosthesis Experience Scales (TAPES). Rehabil. Psychol. 2000, 45, 130–154. [Google Scholar] [CrossRef]
- Desmond, D.M.; MacLachlan, M. Factor Structure of the Trinity Amputation and Prosthesis Experience Scales (TAPES) with Individuals with Acquired Upper Limb Amputations. Am. J. Phys. Med. Rehabil. 2005, 84, 506–513. [Google Scholar] [CrossRef]
- Thorne, S.; Kirkham, S.R.; MacDonald-Emes, J. Interpretive Description: A Noncategorical Qualitative Alternative for Developing Nursing Knowledge. Res. Nurs. Health 1997, 20, 169–177. [Google Scholar] [CrossRef]
- Lee, J.J.; Thorne, S. Interpretive Description: A Rigorous Approach to Qualitative Research in the Applied Disciplines. In The SAGE Handbook of Qualitative Research in the Asian Context; SAGE Publications Ltd.: London, UK, 2022; pp. 308–324. ISBN 978-1-5297-7962-2. [Google Scholar]
- Farmer, T.; Robinson, K.; Elliott, S.J.; Eyles, J. Developing and Implementing a Triangulation Protocol for Qualitative Health Research. Qual. Health Res. 2006, 16, 377–394. [Google Scholar] [CrossRef] [PubMed]
- Rana, K.; Chimoriya, R. A Guide to a Mixed-Methods Approach to Healthcare Research. Encyclopedia 2025, 5, 51. [Google Scholar] [CrossRef]
- Smajic, E.; Avdic, D.; Pasic, A.; Prcic, A.; Stancic, M. Mixed Methodology of Scientific Research in Healthcare. Acta Inform. Medica 2022, 30, 57. [Google Scholar] [CrossRef]
- Telford, K.; Kralik, D.; Koch, T. Acceptance and Denial: Implications for People Adapting to Chronic Illness: Literature Review. J. Adv. Nurs. 2006, 55, 457–464. [Google Scholar] [CrossRef]
- Dekker, J.; De Groot, V. Psychological Adjustment to Chronic Disease and Rehabilitation—an Exploration. Disabil. Rehabil. 2018, 40, 116–120. [Google Scholar] [CrossRef]
- Nugent, K.; Joshi, A.; Viana, R.; Payne, M.W.; Unger, J.; Hunter, S.W. How Has Body Image Been Evaluated among People with Lower Limb Loss? A Scoping Review. Disabil. Rehabil. 2025, 47, 33–46. [Google Scholar] [CrossRef]
- Leventhal, H.; Phillips, L.A.; Burns, E. The Common-Sense Model of Self-Regulation (CSM): A Dynamic Framework for Understanding Illness Self-Management. J. Behav. Med. 2016, 39, 935–946. [Google Scholar] [CrossRef] [PubMed]
- Luza, L.P.; Ferreira, E.G.; Minsky, R.C.; Pires, G.K.W.; Da Silva, R. Psychosocial and Physical Adjustments and Prosthesis Satisfaction in Amputees: A Systematic Review of Observational Studies. Disabil. Rehabil. Assist. Technol. 2020, 15, 582–589. [Google Scholar] [CrossRef] [PubMed]
- Fundarò, C.; Casale, R.; Maestri, R.; Traversoni, S.; Colombo, R.; Salvini, S.; Ferretti, C.; Bartolo, M.; Buonocore, M.; Giardini, A. Technology Assisted Rehabilitation Patient Perception Questionnaire (TARPP-Q): Development and Implementation of an Instrument to Evaluate Patients’ Perception during Training. J. NeuroEng. Rehabil. 2023, 20, 35. [Google Scholar] [CrossRef]
- Prochaska, J.O.; DiClemente, C.C. Stages and Processes of Self-Change of Smoking: Toward an Integrative Model of Change. J. Consult. Clin. Psychol. 1983, 51, 390–395. [Google Scholar] [CrossRef] [PubMed]
- Horgan, O.; MacLachlan, M. Psychosocial Adjustment to Lower-Limb Amputation: A Review. Disabil. Rehabil. 2004, 26, 837–850. [Google Scholar] [CrossRef]
- Kizilkurt, O.K. Quality of Life after Lower Extremity Amputation Due to Diabetic Foot Ulcer: The Role of Prosthesis-Related Factors, Body Image, Self-Esteem, and Coping Styles. Dusunen Adam J. Psychiatry Neurol. Sci. 2020, 33, 109–119. [Google Scholar] [CrossRef]
- Murray, C.D.; Forshaw, M.J. The Experience of Amputation and Prosthesis Use for Adults: A Metasynthesis. Disabil. Rehabil. 2013, 35, 1133–1142. [Google Scholar] [CrossRef]
- Østlie, K.; Magnus, P.; Skjeldal, O.H.; Garfelt, B.; Tambs, K. Mental Health and Satisfaction with Life among Upper Limb Amputees: A Norwegian Population-Based Survey Comparing Adult Acquired Major Upper Limb Amputees with a Control Group. Disabil. Rehabil. 2011, 33, 1594–1607. [Google Scholar] [CrossRef]
- Makai, G.; Rátvai, E.; Veszely, J.; Pethes, B.; Kiss, E.C. Resilience in Patients with Diabetes-Related Lower Limb Amputation. Open Psychol. J. 2019, 12, 34–39. [Google Scholar] [CrossRef]
- Livneh, H. The Use of Generic Avoidant Coping Scales for Psychosocial Adaptation to Chronic Illness and Disability: A Systematic Review. Health Psychol. Open 2019, 6, 2055102919891396. [Google Scholar] [CrossRef] [PubMed]
- Rodrigues, D.; Carvalho, L.; Pinto, C. Lower-Limb Amputees and Family Caregivers: Challenges, Needs, and Strategies for Empowerment—A Qualitative Study. Nurs. Rep. 2025, 15, 166. [Google Scholar] [CrossRef] [PubMed]
| Amputees | Prosthesis Users | |||
|---|---|---|---|---|
| Variable | N | % | N | % |
| Age | ||||
| ≤60 years | 3 | 21.4% | 5 | 35.7% |
| 61–70 years | 6 | 42.9% | 8 | 57.1% |
| 71–80 years | 4 | 28.6% | 1 | 7.1% |
| ≥80 years | 1 | 7.1% | 0 | 0% |
| Gender | ||||
| Male | 12 | 85.7% | 14 | 100% |
| Female | 2 | 14.3% | 0 | 0% |
| Education level | ||||
| Primary school | 4 | 28.6% | 4 | 28.6% |
| Lower secondary school | 6 | 42.9% | 5 | 35.7% |
| High school diploma | 3 | 21.4% | 5 | 35.7% |
| University degree | 1 | 71.1% | 0 | 0% |
| Postgraduate degree | 0 | 0% | 0 | 0% |
| Employment status | ||||
| Retired | 7 | 50.0% | 9 | 64.3% |
| Unemployed | 1 | 7.1% | 1 | 7.1% |
| Employed | 6 | 42.9% | 4 | 28.6% |
| Marital status | ||||
| Single | 6 | 42.9% | 6 | 42.9% |
| Married | 5 | 14.3% | 5 | 35.7% |
| Separated | 2 | 28.6% | 2 | 14.3% |
| Widowed | 1 | 14.3% | 1 | 7.1% |
| Living situation | ||||
| Alone | 6 | 42.9% | 3 | 21.4% |
| With spouse/partner | 2 | 14.3% | 4 | 28.6% |
| With partner and sons and daughters | 4 | 28.6% | 1 | 7.1% |
| With sons and daughters | 0 | 0% | 1 | 7.1% |
| With other relatives | 2 | 14.3% | 5 | 35.7% |
| Caregiver | ||||
| Spouse | 3 | 21.4% | 3 | 21.4% |
| Son/daughter | 5 | 35.7% | 2 | 14.3% |
| Parent | 1 | 7.1% | 2 | 14.3% |
| Other family member | 4 | 28.6% | 4 | 28.6% |
| Non-family member | 1 | 7.1% | 1 | 7.1% |
| None | 0 | 0% | 2 | 14.3% |
| Level of amputation | ||||
| Foot amputation | 4 | 28.6% | 0 | 0% |
| Transtibial amputation | 4 | 28.6% | 14 | 100% |
| Transfemoral amputation | 6 | 42.9% | 0 | 0% |
| Comorbidities | ||||
| Type 2 diabetes mellitus | 11 | 78.6% | 8 | 57.1% |
| Peripheral arterial disease (PAD) | 0 | 0% | 1 | 7.1% |
| Diabetes + PAD | 2 | 14.3% | 5 | 35.7% |
| Other | 1 | 7.1% | 0 | 0% |
| Smoking | ||||
| No | 4 | 28.6% | 5 | 35.7% |
| Yes | 2 | 14.3% | 4 | 28.6% |
| In the past | 8 | 57.1% | 5 | 35.7% |
| Alcohol | ||||
| No | 7 | 50.0% | 8 | 57.1% |
| Yes | 5 | 35.7% | 3 | 21.4% |
| In the past | 2 | 14.3% | 3 | 21.4% |
| (a) | ||||||||||||
| Asymmetry | Shapiro-Wilk | |||||||||||
| N | Missing | Average | IF | Median | SD | Minimum | Maximum | Asymmetry | IF | W | p | |
| Age | 14 | 0 | 66.64 | 2.47 | 65.50 | 9.24 | 51 | 82 | −0.116 | 0.597 | 0.969 | 0.857 |
| Weight | 14 | 0 | 71.64 | 3.82 | 73.00 | 14.31 | 48.0 | 95.0 | −0.387 | 0.597 | 0.924 | 0.248 |
| Height | 14 | 0 | 168.64 | 2.01 | 166.00 | 7.52 | 160 | 180 | 0.474 | 0.597 | 0.884 | 0.066 |
| BMI | 14 | 0 | 25.16 | 1.14 | 26.32 | 4.27 | 18.6 | 30.1 | −0.415 | 0.597 | 0.885 | 0.069 |
| Education | 14 | 0 | 9.50 | 1.27 | 8.00 | 4.77 | 5 | 23 | 1.898 | 0.597 | 0.759 | 0.002 |
| Gender | 14 | 0 | 1.143 | 0.0971 | 1.000 | 0.363 | 1 | 2 | 2.295 | 0.597 | 0.428 | <0.001 |
| Working status | 14 | 0 | 2.571 | 0.5105 | 1.500 | 1.910 | 1 | 7 | 0.954 | 0.597 | 0.769 | 0.002 |
| Marital status | 14 | 0 | 1.857 | 0.2537 | 2.000 | 0.949 | 1 | 4 | 0.951 | 0.597 | 0.824 | 0.010 |
| Living condition | 14 | 0 | 2.286 | 0.3841 | 2.000 | 1.437 | 1 | 5 | 0.866 | 0.597 | 0.813 | 0.007 |
| Caregiver | 14 | 0 | 2.714 | 0.3982 | 2.000 | 1.490 | 1 | 6 | 0.734 | 0.597 | 0.880 | 0.058 |
| Comorbidities | 14 | 0 | 1.500 | 0.2724 | 1.000 | 1.019 | 1 | 4 | 1.781 | 0.597 | 0.552 | <0.001 |
| Smoke | 14 | 0 | 1.286 | 0.2442 | 2.000 | 0.914 | 0 | 2 | −0.662 | 0.597 | 0.703 | <0.001 |
| Alcohol | 14 | 0 | 0.714 | 0.2442 | 0.500 | 0.914 | 0 | 3 | 1.368 | 0.597 | 0.767 | 0.002 |
| (b) | ||||||||||||
| Asymmetry | Shapiro-Wilk | |||||||||||
| N | Missing | Average | IF | Median | SD | Minimum | Maximum | Asymmetry | IF | W | p | |
| Age | 14 | 0 | 61.50 | 1.851 | 61.50 | 6.93 | 50 | 71 | −0.379 | 0.597 | 0.944 | 0.476 |
| Weight | 14 | 0 | 77.86 | 2.783 | 79.00 | 10.41 | 60.0 | 99 | 0.142 | 0.597 | 0.957 | 0.666 |
| Height | 14 | 0 | 174.57 | 1.889 | 174.00 | 7.07 | 161 | 185 | −0.237 | 0.597 | 0.970 | 0.874 |
| BMI | 14 | 0 | 25.73 | 1.293 | 25.45 | 4.84 | 18.9 | 35.9 | 0.687 | 0.597 | 0.954 | 0.616 |
| Education | 14 | 0 | 8.86 | 0.776 | 8.00 | 2.91 | 5 | 13 | 0.209 | 0.597 | 0.864 | 0.034 |
| Gender | 14 | 0 | 1.000 | 0.0000 | 1.00 | 0.000 | 1 | 1 | Nan | 0.597 | Nan | Nan |
| Working status | 14 | 0 | 1.929 | 0.3701 | 1.00 | 1.385 | 1 | 4 | 0.9580 | 0.597 | 0.633 | <0.001 |
| Marital status | 14 | 0 | 1.857 | 0.2537 | 2.00 | 0.949 | 1 | 4 | 0.9507 | 0.597 | 0.824 | 0.010 |
| Living condition | 14 | 0 | 3.071 | 0.4504 | 2.50 | 1.685 | 1 | 5 | 0.0953 | 0.597 | 0.817 | 0.008 |
| Caregiver | 14 | 0 | 3.500 | 0.5522 | 3.50 | 2.066 | 1 | 7 | 0.4883 | 0.597 | 0.902 | 0.121 |
| Comorbidities | 14 | 0 | 1.786 | 0.2606 | 1.00 | 0.975 | 1 | 3 | 0.4921 | 0.597 | 0.675 | <0.001 |
| Smoke | 14 | 0 | 1.000 | 0.2344 | 1.00 | 0.877 | 0 | 2 | 0.0000 | 0.597 | 0.792 | 0.004 |
| Alcohol | 14 | 0 | 0.643 | 0.2250 | 0.00 | 0.842 | 0 | 2 | 0.8287 | 0.597 | 0.724 | <0.001 |
| Variable | Test | p-Value | Effect Size/Association |
|---|---|---|---|
| Age | U = 63.0 | 0.113 | r = −0.357 |
| Weight | U = 73.0 | 0.259 | r = 0.255 |
| Height | U = 54.0 | 0.045 * | r = 0.449 |
| BMI | U = 96.0 | 0.946 | r = 0.020 |
| Years of education | U = 98.0 | 1.000 | r = 0.000 |
| MMSE | U = 85.0 | 0.551 | r = 0.133 |
| EQ-VAS | U = 69.0 | 0.187 | r = 0.296 |
| GAD-7 | U = 87.0 | 0.625 | r = −0.112 |
| PHQ-9 | U = 90.0 | 0.726 | r = −0.082 |
| BIS | U = 87.5 | 0.641 | r = −0.107 |
| Gender | χ2(1) = 2.15; Fisher = 0.481 | 0.142 | C = 0.267; Tau-b = −0.277 |
| Working status | χ2(3) = 1.36; Fisher = 0.838 | 0.715 | C = 0.215; Tau-b = −0.163 |
| Marital status | χ2(3) = 0.00; Fisher = 1.000 | 1.000 | C = 0.000; Tau-b = 0.00 |
| Living condition | χ2(4) = 5.75; Fisher = 0.244 | 0.218 | C = 0.413; Tau-b = 0.216 |
| Caregiver | χ2(5) = 3.62; Fisher = 0.732 | 0.605 | C = 0.338; Tau-b = 0.163 |
| Smoking | χ2(2) = 1.47; Fisher = 0.623 | 0.479 | C = 0.223; Tau-b = −0.163 |
| Alcohol | χ2(2) = 0.77; Fisher = 0.775 | 0.682 | C = 0.163; Tau-b = −0.023 |
| (a) | ||||||||||||
| Descriptive | ||||||||||||
| Shapiro-Wilk | ||||||||||||
| N | Missing | Average | IF | Median | SD | Minimum | Maximum | W | p | |||
| MMSE | 14 | 0 | 28.500 | 0.3593 | 29.000 | 1.345 | 26 | 30 | 0.889 | 0.078 | ||
| EQ-VAS | 14 | 0 | 66.786 | 5.8509 | 65.000 | 21.892 | 20 | 100 | 0.968 | 0.846 | ||
| GAD-7 | 14 | 0 | 4.714 | 1.4428 | 4.000 | 5.398 | 0 | 17 | 0.763 | 0.002 | ||
| PHQ-9 | 14 | 0 | 4.071 | 1.2291 | 3.500 | 4.599 | 0 | 17 | 0.812 | 0.007 | ||
| PID-5-BF | 14 | 0 | 0.514 | 0.0924 | 0.540 | 0.346 | 0.00 | 1.32 | 0.959 | 0.710 | ||
| Adhenrence ASonA | 14 | 0 | 56.429 | 3.6969 | 58.500 | 13.833 | 37 | 76 | 0.911 | 0.162 | ||
| Self efficacy ASonA | 14 | 0 | 18.357 | 1.1222 | 19.500 | 4.199 | 10 | 24 | 0.950 | 0.554 | ||
| Affect ASonA | 14 | 0 | 22.143 | 2.2795 | 24.500 | 8.529 | 5 | 32 | 0.920 | 0.221 | ||
| Total ASonA | 14 | 0 | 96.929 | 6.2075 | 102.500 | 23.226 | 65 | 132 | 0.921 | 0.229 | ||
| BIS | 14 | 0 | 6.429 | 1.8448 | 4.500 | 6.903 | 0 | 21 | 0.855 | 0.026 | ||
| (b) | ||||||||||||
| Descriptive | ||||||||||||
| Asymmetry | Shapiro-Wilk | |||||||||||
| N | Missing | Average | IF | Median | SD | Minimum | Maximum | Asymmetry | IF | W | p | |
| MMSE | 14 | 0 | 28.79 | 0.366 | 29.00 | 1.37 | 26 | 30 | −1.232 | 0.597 | 0.796 | 0.004 |
| EQ-VAS | 14 | 0 | 80.36 | 4.643 | 80.00 | 17.37 | 50 | 100 | −0.468 | 0.597 | 0.893 | 0.091 |
| GAD-7 | 14 | 0 | 4.29 | 1.553 | 1.50 | 5.81 | 0 | 19 | 1.518 | 0.597 | 0.776 | 0.003 |
| PHQ-9 | 14 | 0 | 3.57 | 1.073 | 2.50 | 4.01 | 0 | 13 | 1.383 | 0.597 | 0.813 | 0.007 |
| Total BIS | 14 | 0 | 6.07 | 2.288 | 2.00 | 8.56 | 0 | 25 | 1.557 | 0.597 | 0.724 | <0.001 |
| Total TAPES psychosocial adjustment | 14 | 0 | 55.00 | 1.627 | 55.00 | 6.09 | 45 | 70 | 0.980 | 0.597 | 0.930 | 0.308 |
| Total TAPES Prostheses Satisfection | 14 | 0 | 35.21 | 2.640 | 35.50 | 9.88 | 10 | 49 | −1.045 | 0.597 | 0.917 | 0.198 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Maffoni, M.; Casati, A.; Tambussi, C.; Torlaschi, V.; Baldini, M.; Dragoni, R.; Fundarò, C.; Bagnara, L.; Ferretti, C.; Pierobon, A. Psychological and Behavioral Adjustment in Patients with Non-Traumatic Lower Limb Amputation and Prosthesis: A Mixed-Method Triangulation Study. J. Clin. Med. 2025, 14, 6973. https://doi.org/10.3390/jcm14196973
Maffoni M, Casati A, Tambussi C, Torlaschi V, Baldini M, Dragoni R, Fundarò C, Bagnara L, Ferretti C, Pierobon A. Psychological and Behavioral Adjustment in Patients with Non-Traumatic Lower Limb Amputation and Prosthesis: A Mixed-Method Triangulation Study. Journal of Clinical Medicine. 2025; 14(19):6973. https://doi.org/10.3390/jcm14196973
Chicago/Turabian StyleMaffoni, Marina, Alessandra Casati, Clara Tambussi, Valeria Torlaschi, Marco Baldini, Roberto Dragoni, Cira Fundarò, Laura Bagnara, Chiara Ferretti, and Antonia Pierobon. 2025. "Psychological and Behavioral Adjustment in Patients with Non-Traumatic Lower Limb Amputation and Prosthesis: A Mixed-Method Triangulation Study" Journal of Clinical Medicine 14, no. 19: 6973. https://doi.org/10.3390/jcm14196973
APA StyleMaffoni, M., Casati, A., Tambussi, C., Torlaschi, V., Baldini, M., Dragoni, R., Fundarò, C., Bagnara, L., Ferretti, C., & Pierobon, A. (2025). Psychological and Behavioral Adjustment in Patients with Non-Traumatic Lower Limb Amputation and Prosthesis: A Mixed-Method Triangulation Study. Journal of Clinical Medicine, 14(19), 6973. https://doi.org/10.3390/jcm14196973







