Abstract
Background: Parathyromatosis, an exceptional clinical and pathological entity, involves multiple small nodules of hyper-functional parathyroid tissue scattered throughout the neck and/or mediastinum, in relationship with a prior parathyroidectomy (mostly) or embryologic remnant. Since its first identification in 1975, many aspects of this condition have remained a matter of debate. Objective: We introduce an updated perspective on parathyromatosis covering the main clinical points for everyday practice, from diagnosis to management, as well as the current level of pathogenic understanding. Methods: A narrative review. Results: A total of 22 patients were identified, with the following characteristics: an age range of 33–68 (mean 46.18) years; 4/22 subjects <40 years; female-to-male ratio = 14:8. Of the 22 subjects, 21 had undergone previous parathyroidectomy for primary (n = 14) or secondary (n = 7) hyperparathyroidism. One case was a surgically naïve patient. Analysis of the surgical procedures (seeding circumstances) revealed the following: parathyroid cyst removal, left/right parathyroidectomy; removal of 3.5 parathyroids ± self-transplantation, VATS for mediastinal parathyroid tumours. Parathyroidectomy was accompanied by thyroid surgery (n = 3 patients), specifically hemi-thyroidectomy, partial left-thyroid lobectomy, and partial thyroidectomy. The shortest timeframe from parathyroidectomy to parathyromatosis-related hyperparathyroidism recognition was 1 year, and the longest was 17 years. The highest number of previous surgeries was four. The recognition of parathyromatosis was due to the clinical picture of associated hyperparathyroidism, except for in 2/21 cases with incidental detection. The implant sites coincided with the prior surgical area, but also with unusual locations (clavicle, pleura, mediastinum, sternocleidomastoid muscle and forearm, thyroid). The imaging evaluation included ultrasound plus CT plus 99m-Tc sestamibi scintigraphy, as well as (variable rates) neck MRI, SPECT/CT, 11-Choline PET-CT, Gallium-68 DOTATATE, and 4D CT. Surgery implied serial procedures in some cases (e.g., up to seven). The surgery spectrum largely varied, including not only cervicotomy, but also thoracoscopy, VATS, pericardial adipose tissue excision and thymectomy, etc. Conclusions: Awareness remains a key factor when approaching such an unusual ailment underlying little-understood pathogenic loops, which, if left unrecognized and untreated, might impair patients’ quality of life and the overall parathyroid disease burden.
1. Introduction
Parathyromatosis represents an exceptional clinical and pathological condition characterized by the presence of multiple small nodules of hyper-functional parathyroid tissue scattered throughout the neck and/or mediastinum, which may or may not occur in relationship with a prior parathyroidectomy [1,2,3]. This entity was first described in 1975 by Palmer et al. [4], who identified two different presentations: one in a patient with previous parathyroid surgery, thought to occur due to iatrogenic dissemination and seeding of parathyroid cells during the procedure, and a second disease form in a patient without previous parathyroid removal [4]. It was later hypothesized that in surgically naïve patients, the disease might develop due to scattering of the parathyroid tissue during ontogenesis, the embryological remnants being detected later on during life span, either due to accidental identification via various neck imaging assessments or due to increased parathyroid hormone (PTH)-related hypercalcemia and clinical comorbidities in primary hyperparathyroidism (e.g., cardio-metabolic complications, osteoporosis and fragility fractures, etc.) [5,6,7].
Parathyromatosis caused by surgical exploration/intervention in the cervical region or at the mediastinum is currently considered to be the most common form of the disorder, and leads to recurrent or persistent hyperparathyroidism [8,9,10]. It frequently develops in patients with secondary/tertiary (also named renal) hyperparathyroidism due to chronic kidney disease, as a result of persistent stimuli for parathyroid cells amid a lack of vitamin D activation within the renal cortex [11,12]. Nowadays, the identification of novel cases with respect to congenital parathyroid developmental issues seems to be extremely rare, but estimation of the epidemiologic impact of this condition remains an open matter [10,12].
The main clinical manifestation of parathyromatosis is the presence of hypercalcemia due to excessive PTH secretion, which may lead to the traditional picture of primary hyperparathyroidism (including persistent or recurrent types), as seen in relationship with other benign or malignant parathyroid tumours [13,14,15]. Diagnosis can be challenging considering the infrequent occurrence of the condition, the small size of the parathyroid nodules in this specific instance, the wide dispersion of parathyroid lesions within the neck and mediastinum, and the challenges of differential diagnosis in regard to parathyroid tumours with other histological profiles (e.g., a parathyroid carcinoma) [16,17,18]. From a practical perspective, imaging studies are essential for the localization of hyperactive parathyroid lesions. Ultrasound may reveal hypoechoic, hyper-vascular nodules (which is regarded as a baseline screening tool for parathyroid and thyroid masses), while a 99m-Techentium (Tc) sestamibi scan may show increased uptake [19,20,21].
The management of parathyromatosis is complex and includes both surgical and medical treatment according to a tailored (patient-based) strategy, rather than a guideline-focused approach. Complete resection of the lesions is often difficult, and many cases require multiple surgeries and lifelong monitoring [21,22]. In circumstances where surgery is either not feasible or unable to provide complete remission (or the patient refused the surgery), medical management is employed to achieve long-term control of hypercalcemia and PTH excess-associated comorbidities, using medications such as bisphosphonates or calcimimetics [21,22,23].
Thus, awareness remains the key operating factor in addressing this unusual entity, while many areas, such as pathogenic pathways, early clinical and imaging detection, optimum surgical procedures, true epidemiologic impact, and clear histological definition criteria, remain a matter of debate.
Objective
We aimed to introduce an updated perspective on parathyromatosis covering the main clinical points for everyday practice, from diagnosis to management, as well as the current level of pathogenic understanding.
2. Methods
This was a narrative review. We conducted a PubMed-based search using the keyword “parathyromatosis” and included cases published in the English language from January 2014 to June 2025 reporting parathyromatosis in adults. We excluded cases of pregnancy-related hyperparathyroidism and reports or studies that did not provide clinical characterization of the primary hyperparathyroidism (e.g., histological studies without an endocrine panel including PTH and calcium excess) or did not provide histological confirmation. As a basis for our discussion, we added a novel case in point (a surgery-naïve female who refused parathyroidectomy, and, hence, could only provide an imaging profile of suspected parathyromatosis based on biological confirmation of primary hyperparathyroidism) (Figure 1).
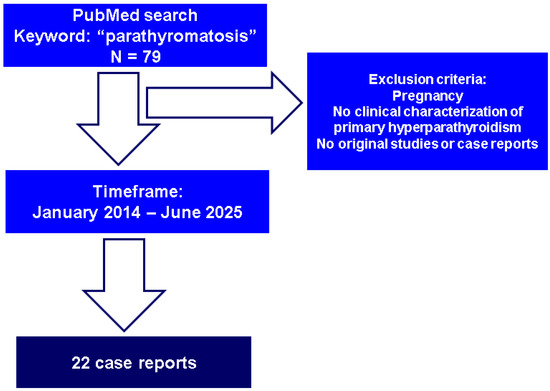
Figure 1.
Flowchart of case-finding strategy.
3. Sample-Focused Analysis of Parathyromatosis
According to our methods, twenty-two case reports [24,25,26,27,28,29,30,31,32,33,34,35,36,37,38,39,40,41,42,43,44,45] of parathyromatosis were identified. The subjects’ ages ranged between 33 and 68 years (mean age of 46.18), and only four individuals were younger than 40. Most patients were females (female-to-male ratio of 14:8). Twenty-one cases occurred in subjects who had undergone previous surgery (parathyroidectomy) either for primary hyperparathyroidism (n = 14) or secondary/renal hyperparathyroidism (n = 7), while one case was detected in a surgically naïve patient [35]. A maximum of three-to-four cases have been published per year (if any) since 2014 [24,25,26,27,28,29,30,31,32,33,34,35,36,37,38,39,40,41,42,43,44,45] (Table 1).

Table 1.
Articles regarding patients diagnosed with parathyromatosis published over the past 10 years (identified according to our methods) [24,25,26,27,28,29,30,31,32,33,34,35,36,37,38,39,40,41,42,43,44,45].
3.1. Parathyromatosis in Prior Surgery Candidates
We identified that most adults diagnosed with parathyromatosis had a history of parathyroid tumour removal and a post-operatory evolution that included further development of the lesion, suggesting intra-surgery seeding as the pathogenic mechanism [24,25,26,27,28,29,30,31,32,33,34,36,37,38,39,40,41,42,43,44,45].
3.1.1. Recurrent Hyperparathyroidism Following Parathyroid Surgery for Primary Hyperparathyroidism
As mentioned, a ratio of 14 to 7 was found with regard to cases of individuals with primary versus renal hyperparathyroidism who were referred for surgery that then became the source of parathyromatosis [24,25,26,27,28,29,30,31,32,33,34,36,37,38,39,40,41,42,43,44,45]. Of note, these are all clinical cases and not experimental models; thus, post-surgery detection of the lesion is circumstantial, and a primary embryologic anomaly cannot be entirely ruled out in these circumstances [35].
Generally, current guidelines recommend parathyroidectomy for patients with primary hyperparathyroidism if they are of a young age (e.g., below the age of 50) or have bone or kidney complications, such as osteoporosis, fragility fractures, high urinary calcium excretion, impaired kidney function, or kidney stones [46,47,48]. This surgical act provides a definitive cure in most patients (90% to 97% of subjects, depending on the study), and this is biochemically reflected in the normalization of serum parathyroid hormone and calcium levels, in addition to an improvement in many traditional complications [49,50,51]. Yet, 5% to 10% (up to one third) of these patients might experience recurrent/persistent hyperparathyroidism-related hypercalcemia [51,52]. If hypercalcemia persists or recurs within six months, the case is classified as persistent hyperparathyroidism, while recurrence of hypercalcemia after more than six months of normal calcium levels is classified as recurrent hyperparathyroidism [51,52,53].
In centres with advanced and high-volume expertise in the field of ortotopic and ectopic parathyroid surgery, the cure rates often exceed 97% and persistent or recurrent hyperparathyroidism due to surgical failure is less common [54,55,56]. Thus, when residual disease due to surgical technique/experience is improbable, the differential diagnosis of post-operatory hypercalcemia (amid parathyroid disease persistence or recurrence) potentially involves a multi-glandular parathyroid disease, (as typically found in multiple endocrine syndromes or synchronous parathyroid adenomas), ectopic parathyroid glands, or spreading of a parathyroid carcinoma [15,57,58,59]. Although a more infrequent cause, parathyromatosis should also be taken into consideration in this spectrum, as parathyroid cells may seed due to the intra-operatory manipulation of parathyroid glands or even due to intra-operatory rupture of a parathyroid adenoma, carcinoma, or cyst [15] (Figure 2).

Figure 2.
Case-finding strategy in patients with recurrent or persistent hyperparathyroidism: among these alternatives, parathyromatosis represents an exceptional finding that should be noted.
Primary hyperparathyroidism in the context of a multi-glandular parathyroid disease is typically associated with genetic syndromes, such as multiple endocrine neoplasia type 1 (MEN1), type 2 (MEN2), and type 4 (MEN4), hyperparathyroidism–jaw tumour syndrome, and familial isolated primary hyperparathyroidism [60,61,62]. The definitive treatment is, again, parathyroidectomy, and it requires a meticulous pre-operative imaging diagnosis in order to establish the number of hyper-functioning glands [63,64,65]. However, parathyroid disease recurrence is high in this instance, and therefore, close lifelong monitoring is mandatory, and sometimes, in the case of genetic conditions, multiple interventions are necessary [66]. For instance, we mention the case study of Sapuppo et al. [27], who illustrated the overlap between parathyromatosis and genetic primary hyperparathyroidism. A 52-year-old woman, who had suffered parathyroidectomy for singe glandular parathyroid disease 16 years prior, developed hyperparathyroidism recurrence for which she underwent three further surgical procedures. Genetic screening revealed a variant in intron 4 (c.655-6C > A) of the MEN1 gene, and a variant in exon 8 of the calcium-sensing receptor (CaSR) gene (c.2549C > G p.Ala850Gly), but no pathogenic variants. Finally, a histological report from the latest surgery also confirmed parathyromatosis [27]. Currently, we do not have enough evidence to more frequently associate this entity with hereditary (syndromic) hyperparathyroidism; parathyromatosis has been listed as a multi-glandular presentation (previously known as parathyroid gland hyperplasia), but the risk of seeding increases with the number of parathyroid surgeries.
Additionally, a parathyroid carcinoma, although rare, represents a complex disease with a high recurrence and mortality rate [67,68,69]. Sometimes, parathyromatosis might mimic a parathyroid malignancy, thus making differential diagnosis crucial, and presenting a challenge for its histological and immunohistochemistry characterization [70,71,72]. Both conditions may present with multiple parathyroid foci dispersed in the soft tissue following parathyroid surgery, as described in the case of Miller et al. [39]. However, intact resection and pathology findings such as vascular invasion strongly suggest a carcinoma over parathyromatosis [73]. In contrast, parathyromatosis usually consists of nested cells forming isles [39], with no trabecular growth [34]. Moreover, parathyroid islets can be surrounded by fibrous tissue, as shown in 2012 by a case study of Aksoy-Altinboga et al. [16]. Overall, recognition of parathyromatosis is often difficult and patients may be misdiagnosed with a parathyroid carcinoma, in spite of benign features supporting parathyromatosis [74].
Another complex presentation is represented by synchronous diagnosis of a parathyroid carcinoma and parathyromatosis, as reported by Yang et al. [36], and Garg et al. [25]. The first was the case of a 46-year-old female who developed recurrent hyperparathyroidism following total parathyroidectomy and self-transplantation. The subject was finally diagnosed with parathyroid carcinoma in association with a subcutaneous nodule of parathyroid cells with no signs of malignancy that were consistent with parathyromatosis [36]. Similarly, Garg et al. [25] described a case of parathyromatosis in a 42-year-old woman with a history of parathyroidectomy for a prior parathyroid carcinoma. One year after the initial procedure, the patient suffered from recurrent hyperparathyroidism. Surgical exploration and histological analysis revealed both a spreading malignancy and parathyromatosis [25]. The intact capsule, vascular invasion, and invasion of the surrounding soft tissue provide essential clues for differentiating parathyroid cancer recurrence/metastasis and post-operatory parathyromatosis. In addition to showing that damage to the capsule during surgery may cause spillage and seeding of the parathyroid tissue, resulting in recurrent hyperparathyroidism, the case reported by Bartoňová et al. [75] in 2018 showed the complicated link between parathyromatosis and a parathyroid carcinoma. Some of the lesions displayed no vascular invasion and no characteristics of malignancy, while others showed a trabecular pattern and vascular invasion consistent with a parathyroid malignancy. Moreover, the initial tumour for which the patient had undergone surgery, thought to be a medullary thyroid carcinoma, was retrospectively classified as a parathyroid carcinoma, while primary parathyromatosis was ruled out [75]. Of note, a retrospective study involving 27 subjects analyzed the histological profile of parathyromatosis (14.8%), atypical adenomas (63%), and parathyroid carcinomas (22.2%), and in parathyromatosis, there was no soft tissue invasion, in contrast with atypical adenomas and carcinomas (0% versus 23% versus 83%, p < 0.01). Other statistically significant differences were the lack of vascular invasion in parathyromatosis versus atypical adenoma versus carcinoma (0% versus 0% versus 33%, p = 0.04), and the lack of metastases (0% versus 6% versus 67%, p < 0.01) [76].
Both ectopic parathyroid glands and parathyromatosis comprise parathyroid chief cells. However, while ectopic parathyroids typically form a single, often encapsulated mass, parathyromatosis presents as a sum/area of multiple micro-nodules without a capsule [16,25,77]. Parathyromatosis may coexist with ectopic parathyroid glands, as suggested by a case report of Li et al. [30] from 2023. This involved a 53-year-old male with a history of parathyroidectomy 17 years prior due to secondary hyperparathyroidism. While lesions in the cervical area identified by neck ultrasound were parathyroid tissue hyperplasia without a capsule, consistent with parathyromatosis, the mediastinal mass showed a well-differentiated nodular hyperplasia suggestive of an ectopic parathyroid tumour. Interestingly, the cervical nodules did not show increased uptake on a 99m-Tc sestamibi scan [30], which, otherwise, remains a pitfall of parathyromatosis recognition in the absence of a histological exam.
3.1.2. Secondary Hyperparathyroidism
As mentioned, the identification of parathyromatosis is feasible, including in cases with renal hyperparathyroidism [24,25,26,27,28,29,30,31,32,33,34,35,36,37,38,39,40,41,42,43,44,45]. Patients with chronic kidney disease frequently experience secondary hyperparathyroidism, characterized by excessive secretion of PTH, as part of the mineral and bone disorder [78,79]. The inability of the kidneys to adequately excrete phosphate and to convert vitamin D to its active form leads to hypocalcaemia and hyperphosphatemia, triggering the parathyroid glands to produce PTH. Changes due to ongoing stimulation of the parathyroid glands cause the glands to become dysfunctional and lead to parathyroid hyperplasia and lower expression of calcium sensing receptors, with eventual autonomisation of the parathyroid glands, which causes persistent elevation of PTH and calcium levels. Parathyroidectomy is often recommended in advanced stages of hyperparathyroidism where medical treatment fails to control the disease [80,81,82,83,84]. Such advanced cases and patients who are being prepared for kidney transplantation are often treated with subtotal or total parathyroidectomy and self-transplantation, usually in the forearm or sternocleidomastoid muscle [85,86,87]. Subtotal parathyroidectomy is also an option; however, most data suggest that the recurrence and persistence of hyperparathyroidism is higher compared to total parathyroidectomy with self-transplantation [87,88]. As found in primary forms, recurrent disease in subjects who have undergone parathyroidectomy for secondary hyperparathyroidism may be caused by ectopic or supernumerary parathyroid glands, for example, but, also by autonomisation of the graft due to persistent stimuli [89,90,91]. Another possible cause is parathyromatosis due to hypersecretion of the seeded parathyroid tissue under the persistence of the initial stimuli [12], and we found seven such cases reported within the timeframe of the search [26,28,29,30,36,38,43] (Table 2).

Table 2.
Case-based sample collected according to our methods: prior surgical history before diagnosis of parathyromatosis (except for ref. [35]) [24,25,26,27,28,29,30,31,32,33,34,35,36,37,38,39,40,41,42,43,44,45].
The analysis of the surgical procedures that led to the consecutive confirmation of parathyromatosis included a parathyroid cyst resection [24], left [25,27,33,37,41,45] and right [27,34,40,42] parathyroidectomy, removal of three and a half parathyroid glands [26], and forearm self-transplantation [28,29,30,36,38,43], as well as video-assisted thoracoscopic (VAS) resection of a mediastinal (ectopic) parathyroid tumour [32]. Of note, the parathyroidectomy was accompanied by thyroid surgery, specifically hemi-thyroidectomy [25], partial left-thyroid lobectomy [31], and partial thyroidectomy [33].
Current knowledge in the field of parathyroid cell seeding does not associate a higher risk with a particular surgical technique, neither is the risk increased if thyroidectomy is simultaneous performed [15,24,25,26,27,28,29,30,31,32,33,34,35,36,37,38,39,40,41,42,43,44,45]. The shortest timeframe from parathyroidectomy until parathyromatosis-related hyperparathyroidism recognition was 1 year, and the longest was 17 years [42]. The highest number of previous parathyroid surgeries was four [27].
3.2. Management Challenges Amid the Diagnosis of Parathyromatosis
Recognition of parathyromatosis was made due to the clinical picture of associated hyperparathyroidism, e.g., bone pain [24,28,29,30,34,35,36,41], kidney stones [24,31], skin itching [30], fatigue [31,41], myalgia [31], muscle weakness [45], chronic constipation [39], polyuria [39], abdominal pain [39,45], nausea [45], and hypercalcemia crisis [25,31,40]. In addition, incidental detection of a malignancy (of colon) in an otherwise asymptomatic patient during a computed tomography scan while the patient was under imagistic surveillance [26], and asymptomatic presentation but with biological confirmation of hyperparathyroidism [42], were found as well. Notably, the majority of these parathyromatosis cases involved recurrent, not persistent, hyperparathyroidism following the initial parathyroid tumour removal [24,25,26,27,28,29,30,31,32,33,34,36,37,38,39,40,41,42,43,44,45].
3.2.1. Detection and Confirmation of Post-Parathyroidectomy Parathyromatosis
Imaging diagnosis plays a crucial role in recognition of the lesion, but in some cases, confirmation was only provided by a histological exam after performing differential diagnosis with other (potential) pathological profiles of parathyroid tumours, including a malignancy. Parathyroid cells may seed all throughout the surgical site, especially in the cervical area. However, parathyromatosis was found in many unusual locations, such as the pleura [32], clavicle [36], and mediastinum [28]. Removal of mediastinal parathyroid adenomas may cause seeding of parathyroid cells in nearby tissues, explaining the location of parathyromatosis in tissues of different histological origin. Such was the case of a 68-year-old male, who was diagnosed with a pleural parathyroid adenoma, after having undergone two mediastinal surgeries for a mediastinal parathyroid adenoma and a mediastinal recurrence [32]. Another possible location is the retrosternal area, requiring thoracoscopy for the removal of hyper-functional tissue [28]. A mediastinal location was also reported by Spillane et al. [26] in a patient with chronic kidney disease who had undergone a subtotal parathyroidectomy 13 years prior [26].
Parathyroid cells may also seed in the pre-tracheal area. For example, a 60-year-old man with normocalcemic recurrent hyperparathyroidism and a history of partial thyroidectomy, upper-left parathyroidectomy, and surgical removal of a retrosternal parathyroid adenoma was diagnosed with parathyromatosis via identification of a pre-tracheal nodule, anterior to the cricoid, using 18F-Fluorocholine positron emission tomography/computed tomography (PET-CT). A pathology report following surgical removal identified islets of parathyroid tissue, confirming the diagnosis of parathyromatosis [33]. Another particular circumstance involves auto-transplantation performed for secondary hyperparathyroidism in patients with chronic kidney failure. Some patients develop parathyromatosis at the implantation site, as shown in the case of a 53-year-old female who underwent total parathyroidectomy with self-transplantation in the left arm and later developed parathyromatosis both subcutaneously in the sternocleidomastoid muscle, in the left clavicle head, and in the forearm, where the graft was implanted [36].
While most cases of post-surgery parathyromatosis occur after classical surgical approaches, Aggarwal et al. [41] reported a case in relationship with an endoscopic procedure. Two years after an endoscopic left superior parathyroidectomy, a 57-year-old male developed recurrent hyperparathyroidism. Localization failed on both ultrasound and a 99m-Tc sestamibi scan. Surgical exploration revealed numerous nodules on the thyroid surface and in the left-central compartment of the neck [41]. A similar report of parathyromatosis along the endoscopic tract wall following endoscopic parathyroidectomy was reported by Sharma et al. [44]. Other procedures, such as percutaneous ethanol injection therapy (PEIT), have also been linked to parathyromatosis, as was the case of a 51-year-old female who developed cervical and pulmonary parathyromatosis following six rounds of PEIT and total parathyroidectomy with auto-transplantation [43].
Another challenge is distinguishing between different types of parathyroid lesions, including ectopic glands, remnant parathyroids, and parathyromatosis. In support of this claim, Cao et al. [38] reported the case of a 61-year-old female who developed recurrent hyperparathyroidism following surgical removal of three parathyroid glands and auto-transplantation. Hyperparathyroidism persisted despite the removal of the graft and PEIT. Single-photon-emission computed tomography (SPECT/CT) revealed multiple foci in the neck and the patient underwent further surgery for the removal of both small nodules beneath the platysma muscle, consistent with parathyromatosis, and a remnant left inferior parathyroid gland [38].
Identifying parathyromatosis pre-operatively can be difficult, as in some cases, ultrasound, computed tomography, and even a 99m-Tc sestamibi scan may fail to reveal any lesion [40]. An alternative used by Wei et al. [40] was four-dimensional CT (4D CT), which managed to identify an area of high signal enhancement that corresponded with small foci in the right thyroid lobe, consistent with parathyromatosis [40].
To conclude, imaging diagnosis was based (at the moment of parathyromatosis suspicion/confirmation) on using ultrasound plus computed tomography plus 99m-Tc sestamibi scintigraphy [24,27,29,31,32,34,35,43], in addition to there being various rates of utilization of the following techniques: neck magnetic resonance imaging [31], SPECT/CT [24,25,29,30,36,38], 11-Choline PET-CT [25,26,33,44], Gallium-68 DOTATATE [27], and 4D CT [36,40,42]. Notably, the high rate of non-diagnosis (mostly in relationship with the small lesion size and low clinical index of suspicion) upon imaging assessment might necessitate the use of multiple methods in order to avoid an exploratory surgery (Table 3).

Table 3.
Imaging evaluation and pathological findings in patients with parathyromatosis [24,25,26,27,28,29,30,31,32,33,34,35,36,37,38,39,40,41,42,43,44,45].
3.2.2. Parathyroidectomy and Medical Therapy for Parathyromatosis
Surgical management of parathyromatosis is frequently challenging as patients often undergo multiple procedures in order to control the disease [24]. In addition to the removal of hyperactive lesions, medical therapy with bisphosphonates and cinacalcet might help [31]. For instance, the case of a 38-year-old female, who had suffered seven surgical procedures in the span of twenty years after the intraoperative rupture of a parathyroid cyst, is highly illustrative of the complex surgical approach needed for these patients [24]. A similar case of a 68-year-old woman, who suffered four unsuccessful surgical attempts for parathyromatosis and remained hypercalcemic and symptomatic in spite of treatment with bisphosphonates and cinacalcet, also reflects the difficulties faced in managing this condition [45].
In cases where both surgical and conventional medical treatment with bisphosphonates and cinacalcet fail, denosumab might be a rescue drug. For instance, Tzotzas et al. [31] reported the case of a patient with parathyromatosis and uncontrolled hypercalcemia, despite having had multiple neck explorations over the course of 18 years, as well as medical management with bisphosphonates and cinacalcet. The patient became normocalcemic following a combined regime with monthly denosumab and cinacalcet [31].
Interestingly, another treatment applied in one patient with parathyromatosis was lanreotide (a somatostatin analogue which is commonly used in neuroendocrine neoplasia [92,93]), together with cinacalcet and vitamin D, which led to an initial reduction in PTH and calcium levels, with subsequent relapse [27]. Some studies supported the use of somatostatin analogues for severe primary hyperparathyroidism in patients with MEN1 [94], considering the expression of somatostatin receptors on parathyroid cells in this syndrome [95]. However, the case reported by Sapuppo et al. [27] was the only report of lanreotide applied for parathyromatosis [27].
Furthermore, surgery implied a higher number of procedures in some cases (e.g., up to seven [24]). The techniques used included not only cervicotomy, but also thoracoscopy [28,30,43,44]; VATS [32]; pericardial adipose tissue excision and thymectomy [35]; excision of a subcutaneous nodule, associated with right inferior and left inferior clavicle head resection [36]; neck exploration revealing nodules covering the left thyroid lobe [39]; right hemi-thyroidectomy and central-compartment neck dissection [40]; neck exploration with left hemi-thyroidectomy and excision of multiple nodules in the left-side neck compartment [41]; and neck exploration and bilateral neck exploration with subtotal parathyroidectomy and cervical thymectomy [42].
The dramatic scenario of surgery for parathyromatosis that requires a highly skilled surgical team is correlated with difficulty in predicting the outcome after a first intervention. Considering the low rate of success in such surgeries, their combination with medical treatment, particularly with bisphosphonates, cinacalcet, denosumab, and even lanreotide, is mandatory (Table 4).

Table 4.
Case-focused analysis of surgical management of parathyromatosis, either associated or not with medical therapy, as well as post-operative outcomes [24,25,26,27,28,29,30,31,32,33,34,35,36,37,38,39,40,41,42,43,44,45].
3.3. Parathyromatosis in Patients Without a Surgical History
Parathyromatosis in subjects who do not have an associated surgical history is extremely rare. During the past decade, only two such cases have reported, according to our investigation [35,42]. One of the cases was a 58-year-old female diagnosed with primary hyperparathyroidism, without any identified neck lesions. Computed tomography and 99m-Tc sestamibi parathyroid scintigraphy both confirmed a retrosternal lesion. After surgical removal of the pericardial adipose tissue and thymus, histological analysis revealed multiple foci of parathyroid tissue all throughout the pericardial adipose tissue [35]. Another report analyzed, in retrospect, the specimen from the initial surgery of a patient who developed parathyromatosis following parathyroidectomy. The authors reported microscopic glandular nests outside the parathyroid capsule indicating possible parathyromatosis from the very start (in addition to the post-surgery presentation) [42].
4. Discussion
Overall, parathyromatosis displays a low level of statistical evidence, with most patients being prior surgery candidates [24,25,26,27,28,29,30,31,32,33,34,36,37,38,39,40,41,42,43,44,45]. Its pathogenic background is not completely understood, neither with respect to the post-operative seeding and development of the parathyroid tissue, nor with respect to an even rarer presentation in surgery-naïve patients who present (most probably) embryologic remnants [35,42]. In addition to the two patients that we identified, previous data also show a limited number of similar reports. For instance, we mention a case of parathyromatosis in a subject with secondary hyperparathyroidism due to chronic renal failure, without a history of surgery. The 36-year-old female underwent surgical exploration of the neck in the context of secondary hyperparathyroidism and had 3.5 parathyroid glands and an ectopic thyroid nodule in the thymus removed. Pathology revealed both hyperplasia of the parathyroid glands and the presence of parathyroid cells in the ectopic thyroid nodule, suggesting parathyromatosis [96]. Three more cases have been reported upon first description of parathyromatosis [4,5]. Palmer et al. [4] described a patient who, in addition to a multi-glandular disease, had nodules of hyper-functioning parathyroid tissue in the fibro-adipose tissue of the neck [4]. Two other cases of parathyroid nests in the cervical and mediastinal fibro-adipose tissue in 22-year-old and 49-year-old males with primary hyperparathyroidism have also been described [5].
We add a novel report of a surgery-naïve adult who refused parathyroidectomy for newly detected parathyroid nodules. This was a 59-year-old female admitted for longstanding hypercalcemia due to primary hyperparathyroidism and discordant imaging results over the years. The patient underwent spontaneous menopause at the age of 45. Her medical history included hypertension, dyslipidaemia, and impaired fasting glucose. She had been diagnosed with primary hyperparathyroidism and osteoporosis seven years prior. She received weekly alendronate (with stationary bone mineral density and no incidental fragility fracture during surveillance) and refused exploratory surgery (Table A1). At current admission, biological confirmation of primary hyperparathyroidism was re-performed. (Table A2) A parathyroid nodule was newly detected on ultrasound (on the right), and another on a 99m-Tc pertechnetate and sestamibi scintigraphy scan (on the left), while contrast-enhanced computed tomography identified five parathyroid micro-nodules (on both anterior cervical sites), suggestive of parathyromatosis. The patient refused parathyroidectomy; thus, no additional localization tool was applied, and the medical therapy was switched to an annual zoledronate injection to prevent further bone loss and hypercalcemia, in addition to mandatory close follow-up (Figure A1) This scenario of parathyromatosis suspicion based on imaging exploration should be backed up by histological analysis of the lesions, since otherwise, no clear criteria can be applied yet. Awareness might help overall hyperparathyroidism management in daily practice.
On theoretical ground, it has been hypothesized that this phenomenon has an embryological origin and may occur due to remnant nests of parathyroid cells in the fibro-adipose tissue of the neck during ontogenesis [4,5,35,97]. The pathogenic process, however, remains unclear. The development of the parathyroid glands begins with the endodermal germ layer, specifically from the third and fourth pharyngeal pouches. The third pharyngeal pouch gives rise to the inferior parathyroid glands, while the fourth pharyngeal pouch forms the superior parathyroid glands. Parathyroid ontogenesis involves differentiation, separation from the thymus, and migration [98,99,100]. While the exact mechanisms underlying parathyroid organogenesis are incompletely understood, they gravitate around the Gcm2 gene, which is involved in parathyroid cell differentiation and in the expression of the PTH gene [99,100,101,102,103].
More recent data also provides insight into the metabolomic profile of parathyroid adenomas, suggesting the possible role of chronic inflammation provoked by infiltration of myeloid cells, fibroblasts, macrophages, and endothelial cells, as found in other endocrine and non-endocrine ailments [104,105,106]. Furthermore, parathyroid adenoma cells have shown high expression of histone-lysine N-methyltransferase 2A [106], increased glucose uptake, high lipid biosynthesis, increased expression of 3-phosphoglycerate dehydrogenase and glucose-6-phosphate dehydrogenase, and cytochrome C expression [105]. Whether genetic factors such as Gcm2 gene or different metabolic stimuli such as inflammation or oxidative stress play a role in the development of parathyromatosis in surgically naïve individuals (either in addition to a traditional parathyroid adenoma growth or not) remains to be explored.
Another area of discussion remains the applicability of fine-needle aspiration in the parathyroid tissue with regard to parathyromatosis recognition. Parathyroid fine-needle aspiration is a procedure used for pre-operative diagnosis of parathyroid tumours in certain centres, but not routinely. Its use remains controversial due to its possible complications, including tumour seeding [107,108], as there have been reports of cutaneous tumour seeding along the aspiration track and cutaneous spread [109,110]. A retrospective study by Balbaloglu et al. [111] explored the hypothesis of parathyromatosis following this procedure in a retrospective analysis of 87 patients (90.8% females) who underwent the aspiration with PTH washout due to inconclusive imaging results. However, no case of parathyromatosis was identified in this cohort [111].
Alternatively, a less accepted theory involves the fact that parathyromatosis may be a low-grade parathyroid malignancy, as suggested by its rapid recurrence and spread over different foci [37].
Another aspect that needs to be explored is whether the mechanisms behind glandular proliferation involved in the development of other endocrine tumours could be involved in parathyromatosis, too. Most endocrine proliferations start with a trigger followed by chronic stimulation. For instance, Thyroid Stimulating Hormone (TSH) elevation due to iodine deficiency stimulates the proliferation of follicular cells of the thyroid [112]. Another factor may be chronic inflammation, which may inhibit thyroid hormone synthesis, leading to TSH elevation [113]. Similarly, chronic stress and inflammation leading to Adrenocorticotropic Hormone (ACTH) secretion stimulates the adrenal cortex, contributing to the formation of adrenal nodules [114,115]. Apart from triggers generating chronic stimulation, other contributing factors are genetic stimuli, such as GNAS, PRKAR1A, PRKACA, PRKACB, PDE8B, and PDE11A variants in the case of adrenal tumours [116]. While initially, cellular proliferation is subordinated to feedback mechanisms, eventually, the tissue may become autonomous, as found in the case of toxic goitre or adrenal nodules with mild autonomous cortisol secretion [117,118]. Henceforth, mechanisms such as stimulation by triggers, including hypocalcemia, as well as genetic and epigenetic factors (e.g., chronic inflammation and of feedback alterations), should be explored as possible mechanisms underlying parathyromatosis development.
The limitations of the present work involve its narrative design based on a single database search. Regarding the topic of parathyromatosis, in regard to which there is still a low level of statistical evidence, further genetic studies and molecular biology research are needed to clarify the pathogenic loops in parathyromatosis tissue, as well as experimental cell models. The clinical perspective needs to integrate a suitable case-finding strategy and refined histological analysis. Management should include a multidisciplinary team: multilayered methods of imaging evaluation and a skilled surgeon, in addition to medical team to control hypercalcemia and PTH excess-related complications across the life span if surgery is unsuccessful.
On a personal note, we highlight an even larger topic which is open for exploration: the phenomenon of iatrogenic parathyromatosis, which may be compared to post-cesarean seeding in the abdominal wall and cesarean scarring of endometrial cells that remain hormonally active throughout the reproductive years (post-cesarean endometriosis versus post-parathyroidectomy parathyromatosis). Similarly, multiple theories have been proposed to explain the association between an adult’s personal background and the surgical act that allows cell implantation and growth, involving a particular reaction of local metalloproteinases, cytokines, collagen tissue, and even vascular response [119,120,121]. Whether a similar molecular and histological model can be applied to parathyromatosis is yet to be discovered. Until then, it mostly remains an enigmatic entity, with many cases underdiagnosed or unrecognized.
5. Conclusions
Parathyromatosis is an exceptional and complex disease that can either develop as a result of recurrent/persistent hyperparathyroidism following parathyroid (±thyroid) surgery, or develop in surgically naïve patients. Its diagnosis is challenging due to discordant imaging results and inconclusive 99m-Tc sestamibi scintigraphy due the small size and scattered character of the micro-nodules. The condition’s management often demands an intensive multidisciplinary approach with repeated surgery and medical management, which may still be suboptimal, as many cases remain hypercalcemic. While parathyromatosis in surgically naïve patients is an exceptional finding, the cases reported so far reflect similar diagnosis and treatment challenges. The mechanisms underlying this condition are still unknown, but most theories gravitate towards the hypothesis of embryological anomalies. Notably, differential diagnosis with parathyroid carcinoma is crucial. Even though both conditions can cause recurrent primary hyperparathyroidism and present with multiple tumours, often located in the cervical and mediastinal areas, as well as the lungs, parathyromatosis differs histologically through the absence of vascular invasion and low mitotic activity. Further research should focus on the risk factors of developing parathyromatosis and identifying the best tailored approach for the management of individuals suffering from parathyromatosis.
Author Contributions
Conceptualization, A.-M.G., C.N. and M.C.; methodology, A.-M.G. and M.C.; software, A.-M.G., C.N. and M.C.; validation, A.-M.G., C.N. and M.C.; formal analysis, A.-M.G., C.N. and M.C.; investigation, A.-M.G., C.N. and M.C.; resources, A.-M.G., C.N. and M.C.; data curation, A.-M.G., C.N. and M.C.; writing—original draft preparation, A.-M.G.; writing—review and editing, M.C.; visualization, A.-M.G., C.N. and M.C.; supervision, M.C.; project administration, M.C.; funding acquisition, M.C. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
The Ethical Committee of “Dr. Carol Davila” Central Military University Emergency Hospital approved the case data collection (number 664 from 31 January 2024).
Informed Consent Statement
Patient consent was waived due to retrospective data collection.
Data Availability Statement
Not applicable.
Acknowledgments
This is part of a PhD research project belonging to the PhD Doctoral School of “Carola Davila” University of Medicine and Pharmacy, entitled “Primary hyperparathyroidism: cardio-metabolic, osseous and surgical aspects” (number 28374 from 2 October 2023). We thank the medical team involved in this case.
Conflicts of Interest
The authors declare no conflicts of interest.
Abbreviations
The following abbreviations are used in this manuscript:
| AT | auto-transplantation |
| ACTH | Adrenocorticotropic Hormone |
| BMD | bone mineral density |
| CaSR | calcium-sensing receptor |
| CKD | chronic kidney disease |
| CT | computed tomography |
| 4D CT | four-dimensional computed tomography |
| DXA | Dual-Energy X-Ray Absorptiometry |
| F | female |
| FNAC | fine-needle aspiration cytology |
| HPTH | hyperparathyroidism |
| MEN | multiple endocrine neoplasia |
| M | male |
| mo | month |
| MRI | magnetic resonance imaging |
| NA | not available |
| PTH | parathyroid hormone |
| PHPT | primary hyperparathyroidism |
| PTx | parathyroidectomy |
| PC | parathyroid carcinoma |
| PET-CT | positron emission tomography–computed tomography |
| PEIT | percutaneous ethanol injection therapy |
| P1NP | procollagen type 1 N-terminal propeptide |
| SHPT | secondary hyperparathyroidism |
| SPECT | single-photon-emission computed tomography |
| Tc | Technetium |
| TSH | Thyroid Stimulating Hormone |
| VATS | video-assisted thoracoscopy |
| y | years |
Appendix A

Table A1.
Central Dual-Energy X-Ray Absorptiometry (DXA) results in an osteoporotic menopausal female with primary hyperparathyroidism.
Table A1.
Central Dual-Energy X-Ray Absorptiometry (DXA) results in an osteoporotic menopausal female with primary hyperparathyroidism.
| Age (Years) | 53 | 54 | 56 | 57 | 58 | 59 | |
|---|---|---|---|---|---|---|---|
| Lumbar | BMD | 0.718 | 0.771 | 0.829 | 0.797 | 0.826 | 0.841 |
| T-score | −3.0 | −2.3 | −2.0 | −2.3 | −2.0 | −1.9 | |
| Z-score | −2.1 | −1.3 | −0.8 | −1.0 | −0.7 | −0.5 | |
| Femoral neck | BMD | 0.599 | 0.650 | 0.622 | 0.613 | 0.628 | 0.603 |
| T-score | −2.2 | −1.7 | −2.0 | −2.1 | −2.0 | −2.2 | |
| Z-score | −1.2 | −0.7 | −0.9 | −0.9 | −0.8 | −1.0 | |
| Total hip | BMD | 0.680 | 0.732 | 0.744 | 0.714 | 0.729 | 0.712 |
| T-score | −2.0 | −1.6 | −1.6 | −1.9 | −1.7 | −1.9 | |
| Z-score | −1.4 | −1.0 | −0.9 | −1.0 | −0.9 | −1.0 | |
| 1/3 distal radius | BMD | NA | 0.560 | 0.548 | 0.559 | 0.544 | 0.549 |
| T-score | NA | −2.2 | −2.4 | −2.2 | −2.5 | −2.4 | |
| Z-score | NA | −1.3 | −1.4 | −1.1 | −1.3 | −1.2 | |
Abbreviations: BMD = bone mineral density, NA = not available

Table A2.
Mineral metabolism assays in a 59-year-old female with primary hyperparathyroidism.
Table A2.
Mineral metabolism assays in a 59-year-old female with primary hyperparathyroidism.
| Parameter (Unit) | Pre-Admission | On Admission | Normal Range |
|---|---|---|---|
| Serum total calcium (mg/dL) | 11.16 | 10.6 | 8.4–10.2 |
| Serum ionized calcium (mg/dL) ** | 4.56 | 4.32 | 3.9–4.9 |
| Phosphorus (mg/dL) | NA | 2.8 | 2.3–4.7 |
| Total proteins (g/dL) ** | 8.1 | 8.1 | 6.4–8.6 |
| PTH (pg/mL) * | 109 | 64.62 | 17.3–74.1 |
| 25-hydroxyvitamin D (ng/mL) | 31.4 (>30) | 31.8 | 20–100 |
| 24-h urinary calcium (mg/24 h) | 0.42 | 0.36 | 0.07–0.3 |
| Alkaline phosphatase (U/L) | NA | 74 | 38 –105 |
| Osteocalcin (ng/mL) | NA | 17.92 | 15–46 |
| CrossLaps (ng/mL) | NA | 0.49 | 0.33–0.782 |
| P1NP (ng/mL) | NA | 116.5 | 20.25–76.31 |
Abbreviations: NA = not available; P1NP = procollagen type 1 N-terminal propeptide; PTH = parathyroid hormone; * PTH normal ranges: 11–67 pg/mL; ** ionized calcium formula of calculation = (6 × serum total calcium (mg/dL) − total proteins (g/dL)/3)/(total proteins (g/dL) + 6).
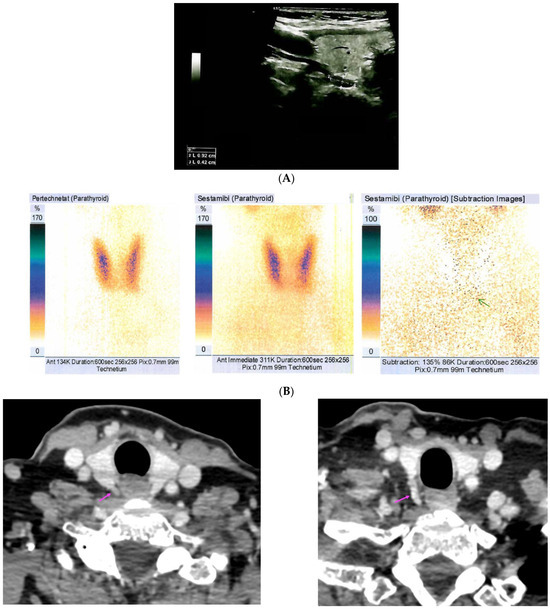
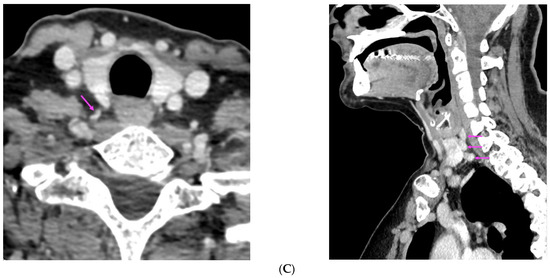
Figure A1.
Imaging evaluation of the neck parathyroid tissue. (A) Neck ultrasound shows a right inferior parathyroid nodule of 0.92 by 0.42 cm (dotted white lines) behind the right thyroid lobe; (B) Dual-phase 99m-Tc pertechnetate and sestamibi scintigraphy scan shows a tracer uptake (subtraction image) inferior to the left thyroid lobe, suggestive for parathyroid tissue (green arrow). (C) Computed tomography identified three parathyroid micro-nodules distributed in a layered pattern, located in the right latero-cervical, para-tracheal, and para-oesophageal areas (of 0.22 by 0.61 by 0.69 cm, of 0.34 by 0.65 by 0.6 cm, respectively, of 0.35 by 1.12 by 1.33 cm), and two small left parathyroid glands (of less than 1 cm largest diameter for each); (pink arrows).
References
- Baloch, Z.W.; LiVolsi, V.A. Pathology of the parathyroid glands in hyperparathyroidism. Semin. Diagn. Pathol. 2013, 30, 165–177. [Google Scholar] [CrossRef] [PubMed]
- Twig, B.A.; van Dalen, T.; Vroonhoven, T.J.M.V.V.; Consten, E.C.J. Recurrent hyperparathyroidism caused by benign neoplastic seeding: Two cases of parathyromatosis and a review of the literature. Acta Chir. Belg. 2013, 113, 228–232. [Google Scholar] [CrossRef] [PubMed]
- Carsote, M.; Paduraru, D.N.; Nica, A.E.; Valea, A. Parathyroidectomy: Is vitamin D a player for a good outcome? J. Med. Life 2016, 9, 348–352. [Google Scholar] [PubMed]
- Palmer, J.A.; Brown, W.A.; Kerr, W.H.; Rosen, I.B.; Watters, N.A. The surgical aspects of hyperparathyroidism. Arch. Surg. 1975, 110, 1004–1007. [Google Scholar] [CrossRef]
- Reddick, R.; Costa, J.; Marx, S. Parathyroid hyperplasia and parathyromatosis. Lancet 1977, 1, 549. [Google Scholar] [CrossRef]
- Pipernea, R.; Popa, F.-L.; Ciortea, V.-M.; Irsay, L.; Ungur, R.A.; Pintea, A.L.; Iliescu, M.-G.; Cipăian, R.-C.; Stanciu, M. The role of rehabilitation and anabolic treatment in severe osteoporosis associated with significant vitamin D deficiency-case report. Balneo PRM Res. J. 2023, 14, 539. [Google Scholar] [CrossRef]
- Nica, S.; Sionel, R.; Măciucă, R.; Csutak, O.; Cimponeriu, D.; Ciobica, M.L.; Nica, M.I.; Chelu, I.; Radu, I.; Toma, M. Gender-Dependent Associations Between Digit Ratio and Genetic Polymorphisms, BMI, and Reproductive Factors. Rom. J. Mil. Med. 2025, 128, 78–86. [Google Scholar] [CrossRef]
- Hage, M.P.; Salti, I.; Fuleihan, G.E.-H. Parathyromatosis: A rare yet problematic etiology of recurrent and persistent hyperparathyroidism. Metabolism 2012, 61, 762–775. [Google Scholar] [CrossRef]
- Alnajmi, R.A.; Ali, D.S.; Khan, A.A. Persistence and Recurrence of Primary Hyperparathyroidism. Best Pract. Res. Clin. Endocrinol. Metab. 2025, 39, 101986. [Google Scholar] [CrossRef]
- Guerin, C.; Paladino, N.C.; Lowery, A.; Castinetti, F.; Taieb, D.; Sebag, F. Persistent and recurrent hyperparathyroidism. Updates Surg. 2017, 69, 161–169. [Google Scholar] [CrossRef]
- Popa, F.L.; Boicean, L.C.; Iliescu, M.G.; Stanciu, M. The importance of association between sex steroids deficiency, reduction of bone mineral density and falling risk in men with implications in medical rehabilitation. Balneo PRM Res. J. 2021, 12, 318–322. [Google Scholar] [CrossRef]
- Matsuoka, S.; Tominaga, Y.; Sato, T.; Uno, N.; Goto, N.; Katayama, A.; Uchida, K.; Tsuzuki, T. Recurrent renal hyperparathyroidism caused by parathyromatosis. World J. Surg. 2007, 31, 299–305. [Google Scholar] [CrossRef] [PubMed]
- Haciyanli, S.G.; Acar, N.; Gür, E.; Çelik, S.; Karaıslı, S.; Dilek, O.; Haciyanli, M. Severe hypercalcaemia of primary hyperparathyroidism: Could giant adenoma be the real culprit rather than carcinoma? Ann. R. Coll. Surg. Engl. 2020, 102, 363–368. [Google Scholar] [CrossRef] [PubMed]
- Dumitru, N.; Carsote, M.; Cocolos, A.; Petrova, E.; Olaru, M.; Dumitrache, C.; Ghemigian, A. The Link Between Bone Osteocalcin and Energy Metabolism in a Group of Postmenopausal Women. Curr. Health Sci. J. 2019, 45, 47–51. [Google Scholar] [CrossRef]
- Ladsous, M.; Deguelte, S.; Hindié, E.; Caiazzo, R.; Delemer, B. Chapter 15: Recurrent or persistent primary hyperparathyroidism, parathyromatosis. Ann. Endocrinol. 2025, 86, 101704. [Google Scholar] [CrossRef]
- Aksoy-Altinboga, A.; Akder Sari, A.; Rezanko, T.; Haciyanli, M.; Orgen Calli, A. Parathyromatosis: Critical diagnosis regarding surgery and pathologic evaluation. Korean J. Pathol. 2012, 46, 197–200. [Google Scholar] [CrossRef]
- Mitrica, M.; Vasiliu, O.; Plesa, A.; Sirbu, O.M. Multinodular and vacuolating neuronal tumor. Rom. J. Mil. Med. 2025, 128, 10–16. [Google Scholar] [CrossRef]
- Fernandez-Ranvier, G.G.; Khanafshar, E.; Jensen, K.; Zarnegar, R.; Lee, J.; Kebebew, E.; Duh, Q.; Clark, O.H. Parathyroid carcinoma, atypical parathyroid adenoma, or parathyromatosis? Cancer 2007, 110, 255–264. [Google Scholar] [CrossRef]
- Valea, A.; Carsote, M.; Moldovan, C.; Georgescu, C. Chronic autoimmune thyroiditis and obesity. Arch. Balk. Med. Union 2018, 53, 64–69. [Google Scholar]
- Tublin, M.E.; Yim, J.H.; Carty, S.E. Recurrent hyperparathyroidism secondary to parathyromatosis: Clinical and imaging findings. J. Ultrasound Med. 2007, 26, 847–851. [Google Scholar] [CrossRef]
- Pinnamaneni, N.; Shankar, P.R.; Muthukrishnan, A. (99m)Tc MIBI SPECT findings in parathyromatosis—A rare entity causing recurrent hyperparathyroidism. Clin. Nucl. Med. 2013, 38, e443–e445. [Google Scholar] [CrossRef]
- Vellanki, P.; Lange, K.; Elaraj, D.; Kopp, P.A.; El Muayed, M. Denosumab for management of parathyroid carcinoma-mediated hypercalcemia. J. Clin. Endocrinol. Metab. 2014, 99, 387–390. [Google Scholar] [CrossRef] [PubMed]
- Daphnis, E.; Stylianou, K.; Katsipi, I.; Stratigis, S.; Karamitopoulou, E.; Karkavitsas, N.; Kyriazis, J. Parathyromatosis and the challenge of treatment. Am. J. Kidney Dis. 2006, 48, 502–505. [Google Scholar] [CrossRef]
- Bashantoof, S.K.; Alramadhan, M.A.; Alawadh, M.H.; Samaih, N.A.B.; Alshammari, R.A.; Aodah, A. Intractable Parathyromatosis despite extensive surgical interventions: A case report with literature review. Int. J. Surg. Case Rep. 2024, 114, 109172. [Google Scholar] [CrossRef]
- Garg, Y.; Vaishnav, M.S.; Garg, N.; Muniraj, K.; Srikanta, S. Parathyroid Carcinoma Complicated by Parathyromatosis and Refractory Hypercalcemia. Cureus 2024, 16, e72584. [Google Scholar] [CrossRef]
- Spillane, C.; Calpin, G.; Singh, S.; O’Reilly, K.; Hehir, C.; Hill, A.; Magee, C.; Barrett, H. A case of mediastinal hyperparathyromatosis. J. Surg. Case Rep. 2024, 2024, rjad735. [Google Scholar] [CrossRef]
- Sapuppo, G.; Giusti, M.A.; Aricò, D.; Masucci, R.; Tavarelli, M.; Russo, M.; Pellegriti, G. Recurrent parathyromatosis in a patient with concomitant MEN1 and CASR gene alterations: Clinical management of a case report and literature review. Front. Endocrinol. 2023, 14, 1108278. [Google Scholar] [CrossRef]
- Saleh, T.; Alaswad, M.; Otry, A.; Saleh, W. Retrosternal parathyromatosis in a patient with prior total parathyroidectomy. J. Surg. Case Rep. 2023, 2023, rjad256. [Google Scholar] [CrossRef]
- Yang, J.; Lu, X.; Zhou, P.; Liu, H.; Wang, J.; Su, X. Recurrence hyperparathyroidism caused by synchronous parathyroid carcinoma and parathyromatosis in a patient with long-term hemodialysis. BMC Nephrol. 2023, 24, 293. [Google Scholar] [CrossRef]
- Li, L.; He, C.; Cheng, G.; Cao, J.; Wang, C.; Tang, Y.; Zhang, W. Recurrent renal secondary hyperparathyroidism caused by supernumerary mediastinal parathyroid gland and parathyromatosis: A case report. Front. Surg. 2023, 10, 1135596. [Google Scholar] [CrossRef]
- Tzotzas, T.; Goropoulos, A.; Karras, S.; Terzaki, A.; Siolos, A.; Doumas, A.; Zaramboukas, T.; Tigas, S. Effective long-term management of parathyromatosis-related refractory hypercalcemia with a combination of denosumab and cinacalcet treatment. Hormones 2022, 21, 171–176. [Google Scholar] [CrossRef]
- Kaur, J.; Drake, T. Ectopic Pleural Parathyroid Adenoma Causing Recurrent Primary Hyperparathyroidism. Cureus 2022, 14, e25101. [Google Scholar] [CrossRef] [PubMed]
- Latgé, A.; Averous, G.; Helali, M.; Bachellier, P.; Imperiale, A. Parathyromatosis: A challenging cause of recurrent primary hyperparathyroidism. QJM 2022, 115, 235–236. [Google Scholar] [CrossRef] [PubMed]
- Ilyicheva, E.A.; Bersenev, G.A. Parathyromatosis as a cause of recurrence primary hyperparathyroidism: A case report. Int. J. Surg. Case Rep. 2021, 80, 105689. [Google Scholar] [CrossRef] [PubMed]
- Altin, O.; Sari, R. Pericardial Type 1 Parathyromatosis: A very rare cause of primary hyperparathyroidism. Acta Endocrinol. 2020, 16, 505–507. [Google Scholar] [CrossRef]
- Yang, J.; Zhang, J.; Liu, N.-H.; Liu, H.; Dong, M.J. Persistent secondary hyperparathyroidism caused by parathyromatosis and supernumerary parathyroid glands in a patient on haemodialysis. BMC Nephrol. 2020, 21, 257. [Google Scholar] [CrossRef]
- Haciyanli, M.; Karaisli, S.; Gucek Haciyanli, S.; Atasever, A.; Arikan Etit, D.; Gur, E.O.; Acar, T. Parathyromatosis: A very rare cause of recurrent primary hyperparathyroidism-case report and review of the literature. Ann. R. Coll. Surg. Engl. 2019, 101, e178–e183. [Google Scholar] [CrossRef]
- Cao, H.; Zeng, M.; Fang, H.; Tang, L.; Liu, W. Parathyromatosis type 2 detected by 99mTc-MIBI SPECT/CT. Gland. Surg. 2019, 8, 806–809. [Google Scholar] [CrossRef]
- Miller, M.J.; Agrawal, N.; Katz, G.; Ogilvie, J.; Melamed, J. Parathyromatosis with a papillary architecture. Histopathology 2019, 75, 598–602. [Google Scholar] [CrossRef]
- Wei, A.E.; Garrett, M.R.; Gupta, A. Parathyromatois: A rare case of recurrent hyperparathyroidism localized by four-dimensional computed tomography. AACE Clin. Case Rep. 2019, 5, e384–e387. [Google Scholar] [CrossRef]
- Aggarwal, A.; Wadhwa, R.; Aggarwal, V. Parathyromatosis Following Endoscopic Parathyroid Surgery: A Rare Occurrence. Indian J. Endocrinol. Metab. 2017, 21, 641–642. [Google Scholar] [CrossRef]
- Jain, M.; Krasne, D.L.; Singer, F.R.; Giuliano, A.E. Recurrent primary hyperparathyroidism due to Type 1 parathyromatosis. Endocrine 2017, 55, 643–650. [Google Scholar] [CrossRef]
- Nakamura, M.; Tanaka, K.; Fujii, T. Hyperparathyroidism caused by distant pulmonary lesions and parathyromatosis after ethanol injection/parathyroidectomy for secondary hyperparathyroidism. Hemodial. Int. 2017, 21, E45–E49. [Google Scholar] [CrossRef] [PubMed]
- Sharma, S.; Dey, P.; Gude, G.; Saikia, U.N. Parathyromatosis-A rare occurrence along the endoscopic tract detected on fine needle aspiration cytology. Diagn. Cytopathol. 2016, 44, 1125–1127. [Google Scholar] [CrossRef]
- Scorza, A.B.; Moore, A.G.; Terry, M.; Bricker, L.A. Secondary parathyromatosis in a patient with normal kidney function: Review of diagnostic modalities and approaches to management. Endocr. Pract. 2014, 20, e4–e7. [Google Scholar] [CrossRef]
- Bilezikian, J.P.; Khan, A.A.; Silverberg, S.J.; Fuleihan, G.E.-H.; Marcocci, C.; Minisola, S.; Perrier, N.; Sitges-Serra, A.; Thakker, R.V.; Guyatt, G.; et al. Evaluation and Management of Primary Hyperparathyroidism: Summary Statement and Guidelines from the Fifth International Workshop. J. Bone Miner. Res. 2022, 37, 2293–2314. [Google Scholar] [CrossRef]
- Wilhelm, S.M.; Wang, T.S.; Ruan, D.T.; Lee, J.A.; Asa, S.L.; Duh, Q.-Y.; Doherty, G.M.; Herrera, M.F.; Pasieka, J.L.; Perrier, N.D.; et al. The American Association of Endocrine Surgeons Guidelines for Definitive Management of Primary Hyperparathyroidism. JAMA Surg. 2016, 151, 959–968. [Google Scholar] [CrossRef]
- Frey, S.; Mosbah, H.; Donatini, G.; Brunaud, L.; Chabre, O.; Vezzosi, D. Chapter 9: Indications for the treatment of primary hyperparathyroidism. Ann. Endocrinol. 2025, 86, 101698. [Google Scholar] [CrossRef]
- Manea, M.M.; Dragos, D.; Ghenu, M.I.; Enache, I.I.; Stoican, I.C.; Ciulavu, C.; Vasiliu, O.; Sirbu, C.A.; Tuta, S. The Neurocardiogenic Impact of Ischemic Stroke: Intricacies of Cardiac Enzymes and the Vegetative System. Rom. J. Mil. Med. 2025, 128, 36–42. [Google Scholar] [CrossRef]
- Pappachan, J.M.; Lahart, I.M.; Viswanath, A.K.; Borumandi, F.; Sodi, R.; Metzendorf, M.-I.; Bongaerts, B. Parathyroidectomy for adults with primary hyperparathyroidism. Cochrane Database Syst. Rev. 2023, 3, CD013035. [Google Scholar] [CrossRef]
- Ünlü, M.T.; Aygun, N.; Kostek, M.; Caliskan, O.; Uludag, M. The relationship between postoperative parathormone suppression and surgical cure in primary hyperparathyroidism. Front. Endocrinol. 2025, 16, 1629719. [Google Scholar] [CrossRef]
- Uludag, M.; Unlu, M.T.; Kostek, M.; Caliskan, O.; Aygun, N.; Isgor, A. Persistent and Recurrent Primary Hyperparathyroidism: Etiological Factors and Pre-Operative Evaluation. Sisli Etfal Hastan Tip Bul. 2023, 57, 1–17. [Google Scholar] [CrossRef]
- Shires, C.B.; Parsons, A.; Dewan, K.; Sebelik, M. Controversies in thyroid and parathyroid surgery. Am. J. Otolaryngol. 2025, 46, 104703. [Google Scholar] [CrossRef] [PubMed]
- Udelsman, R.; Lin, Z.; Donovan, P. The superiority of minimally invasive parathyroidectomy based on 1650 consecutive patients with primary hyperparathyroidism. Ann. Surg. 2011, 253, 585–591. [Google Scholar] [CrossRef] [PubMed]
- Chen, H.; Wang, T.S.; Yen, T.W.F.; Doffek, K.; Krzywda, E.; Schaefer, S.; Sippel, R.S.; Wilson, S.D. Operative failures after parathyroidectomy for hyperparathyroidism: The influence of surgical volume. Ann. Surg. 2010, 252, 691–695. [Google Scholar] [CrossRef]
- Lenschow, C.; Pistorius, R.; Meir, M.; Schlegel, N. Parathyroid glands and their anatomical positional variations: Preoperative diagnostics and surgical planning. Chirurgie 2025. [Google Scholar] [CrossRef]
- Anghel, D.; Ciobica, L.M.; Negru, M.M.; Jurcut, C.; Otlocan, L.; Coca, A. Bone mineral density and vitamin D levels in patients with rheumatoid arthritis. Osteoporos. Int. 2017, 28 (Suppl. S1), S435–S436. [Google Scholar]
- Vasiliu, O. Impact of SGLT2 inhibitors on metabolic status in patients with psychiatric disorders undergoing treatment with second-generation antipsychotics (Review). Exp. Ther. Med. 2023, 25, 125. [Google Scholar] [CrossRef]
- Htoo, S.T.; Cusano, N.E. Management of Primary Hyperparathyroidism: Historical and Contemporary Perspectives. Endocr. Pract. 2025. [Google Scholar] [CrossRef]
- Lauricella, E.; Chaoul, N.; D’aNgelo, G.; Giglio, A.; Cafiero, C.; Porta, C.; Palmirotta, R. Neuroendocrine Tumors: Germline Genetics and Hereditary Syndromes. Curr. Treat. Options Oncol. 2025, 26, 55–71. [Google Scholar] [CrossRef]
- Balachandra, S.; Fazendin, J.; Chen, H. Complex Primary Hyperparathyroidism: Hereditary and Recurrent Disease. Surg. Clin. N. Am. 2024, 104, 811–823. [Google Scholar] [CrossRef] [PubMed]
- Brandi, M.L.; Pieterman, C.R.C.; English, K.A.; Lines, K.E.; Shariq, O.A.; Marini, F.; Cuny, T.; Lewis, M.A.; Stratakis, C.A.; Perrier, N.D.; et al. Multiple endocrine neoplasia type 1 (MEN1): Recommendations and guidelines for best practice. Lancet Diabetes Endocrinol. 2025, 13, 699–721. [Google Scholar] [CrossRef] [PubMed]
- Ruggeri, R.M.; Benevento, E.; De Cicco, F.; Grossrubatscher, E.M.; Hasballa, I.; Tarsitano, M.G.; Centello, R.; Isidori, A.M.; Colao, A.; Pellegata, N.S.; et al. Multiple endocrine neoplasia type 4 (MEN4): A thorough update on the latest and least known men syndrome. Endocrine 2023, 82, 480–490. [Google Scholar] [CrossRef] [PubMed]
- Cristina, E.V.; Alberto, F. Management of familial hyperparathyroidism syndromes: MEN1, MEN2, MEN4, HPT-Jaw tumour, Familial isolated hyperparathyroidism, FHH, and neonatal severe hyperparathyroidism. Best Pccat. Res. Clin. Endocrinol. Metab. 2018, 32, 861–875. [Google Scholar] [CrossRef] [PubMed]
- Gioia, A.; Nappi, C.J.; Socin, M.; Vallon, G.; Naviglio, S.; Bernardi, S.; Boscarelli, A.; Dobrinja, C. Primary Hyperparathyroidism: A Case Series, Patient-Centered Approach to Diagnosis and Management Review. Ann. Ital. Chir. 2025, 96, 878–893. [Google Scholar] [CrossRef]
- Al-Salameh, A.; Haissaguerre, M.; Tresallet, C.; Kuczma, P.; Marciniak, C.; Cardot-Bauters, C. Chapter 6: Syndromic primary hyperparathyroidism. Ann. Endocrinol. 2025, 86, 101695. [Google Scholar] [CrossRef]
- Magnabosco, F.F.; Brescia, M.D.G.; Nascimento Júnior, C.P.; Massoni Neto, L.M.; Arap, S.S.; de Castro Junior, G.; Ledesma, F.L.; Ferreira Alves, V.A.; Kowalski, L.P.; Martin, R.M.; et al. Time to Recurrence as a Prognostic Factor in Parathyroid Carcinoma. J. Endocr. Soc. 2023, 7, bvad067. [Google Scholar] [CrossRef]
- Traini, E.; Lanzafame, A.; Carnassale, G.; Daloiso, G.; Borghesan, N.; Sanchez, A.M.; Mattia, A. Synchronous Multiple Parathyroid Carcinoma: A Challenging Diagnosis Influencing Optimal Primary Treatment-A Literature Review to Guide Clinical Decision-Making. J. Clin. Med. 2025, 14, 5228. [Google Scholar] [CrossRef]
- Simescu, R.; Piciu, A.; Muntean, V.; Mester, A.; Leucuta, D.C.; Piciu, D. Diagnostic and Surgical Challenges in Parathyroid Neoplasia: An Extensive Analysis of a Single Endocrine Surgery Center Cohort of Patients. Cancers 2025, 17, 1783. [Google Scholar] [CrossRef]
- Jentus, M.M.; Corver, W.E.; Snel, M.; van Haalen, F.M.; van Wezel, T.; Ruano, D.; Kapiteijn, E.; Crobach, S.; Appelman-Dijkstra, N.M.; Schepers, A.; et al. Diagnosing the silent: The molecular landscape of non-functional parathyroid carcinoma. Virchows Arch. 2025. [Google Scholar] [CrossRef]
- Yu, Z.; Zhou, J.; Xie, X.; Li, X.; Gié, M.-L.M.; Bouvet, M.; Manyalich-Blasi, M.; Wu, Y. Potential higher malignancy of nonfunctional parathyroid carcinoma: A case series study. Gland. Surg. 2025, 14, 947–957. [Google Scholar] [CrossRef]
- Fuenzalida, L.; Indo, S.; Contreras, H.R.; Rappoport, D.; Cabané, P. Basic-Clinical Analysis of Parathyroid Cancer. Biomedicines 2025, 13, 687. [Google Scholar] [CrossRef]
- Gubbiotti, M.; Livolsi, V.A. Late Recurrence of Hyperparathyroidism: Parathyromatosis or Recurrent Parathyroid Carcinoma? Mayo Clin. Proc. 2022, 97, 2161–2163. [Google Scholar] [CrossRef]
- Kaszczewska, M.; Popow, M.; Chudziński, W.; Kaszczewska, J.; Bogdańska, M.; Podgórska, J.; Czarniecka, A.; Gałązka, Z. A Woman with a 27-Year History of Hyperparathyroidism and Hypercalcemia Who Was Diagnosed with Low-Grade Parathyroid Carcinoma. Am. J. Case Rep. 2021, 22, e930301. [Google Scholar] [CrossRef] [PubMed]
- Bartoňová, L.; Campr, V.; Chmelová, R.; Taudy, M.; Kodet, R. Nonfunctioning parathyroid carcinoma associated with parathyromatosis. A case report. Cesk. Patol. 2018, 54, 37–42. [Google Scholar] [PubMed]
- Schulte, J.J.; Pease, G.; Taxy, J.B.; Hall, C.; Cipriani, N.A. Distinguishing Parathyromatosis, Atypical Parathyroid Adenomas, and Parathyroid Carcinomas Utilizing Histologic and Clinical Features. Head Neck Pathol. 2021, 15, 727–736. [Google Scholar] [CrossRef] [PubMed]
- Sato, S.; Kitahara, A.; Koike, T.; Hashimoto, T.; Ohashi, R.; Motoi, N.; Tsuchida, M. Resection of a large ectopic parathyroid adenoma: A case report. Int. J. Surg. Case Rep. 2016, 23, 8–11. [Google Scholar] [CrossRef][Green Version]
- Kidney Disease: Improving Global Outcomes (KDIGO) CKD-MBD Update Work Group. KDIGO 2017 Clinical Practice Guideline Update for the Diagnosis, Evaluation, Prevention, and Treatment of Chronic Kidney Disease-Mineral and Bone Disorder (CKD-MBD). Kidney Int. Suppl. 2017, 7, 1–59. [Google Scholar] [CrossRef]
- Bellorin-Font, E.; Rojas, E.; Martin, K.J. Bone Disease in Chronic Kidney Disease and Kidney Transplant. Nutrients 2022, 15, 167. [Google Scholar] [CrossRef]
- Magagnoli, L.; Ciceri, P.; Cozzolino, M. Secondary hyperparathyroidism in chronic kidney disease: Pathophysiology, current treatments and investigational drugs. Expert Opin. Investig. Drugs 2024, 33, 775–789. [Google Scholar] [CrossRef]
- Zhang, L.-X.; Zhang, B.; Liu, X.-Y.; Wang, Z.-M.; Qi, P.; Zhang, T.-Y.; Zhang, Q. Advances in the treatment of secondary and tertiary hyperparathyroidism. Front. Endocrinol. 2022, 13, 1059828. [Google Scholar] [CrossRef]
- Hu, L.; Napoletano, A.; Provenzano, M.; Garofalo, C.; Bini, C.; Comai, G.; La Manna, G. Mineral Bone Disorders in Kidney Disease Patients: The Ever-Current Topic. Int. J. Mol. Sci. 2022, 23, 12223. [Google Scholar] [CrossRef]
- Tsai, S.-H.; Kan, W.-C.; Jhen, R.-N.; Chang, Y.-M.; Kao, J.-L.; Lai, H.-Y.; Liou, H.-H.; Shiao, C.-C. Secondary hyperparathyroidism in chronic kidney disease: A narrative review focus on therapeutic strategy. Clin. Med. 2024, 24, 100238. [Google Scholar] [CrossRef]
- Stack, B.C. Secondary Hyperparathyroidism. Otolaryngol. Clin. N. Am. 2024, 57, 99–110. [Google Scholar] [CrossRef] [PubMed]
- Dream, S.; Kuo, L.E.M.; Kuo, J.H.; Sprague, S.M.D.; Nwariaku, F.E.; Wolf, M.M.; Olson, J.A.J.; Moe, S.M.; Lindeman, B.M.; Chen, H. The American Association of Endocrine Surgeons Guidelines for the Definitive Surgical Management of Secondary and Tertiary Renal Hyperparathyroidism. Ann. Surg. 2022, 276, e141–e176. [Google Scholar] [CrossRef] [PubMed]
- Sari, R.; Yabanoglu, H.; Hargura, A.; Kus, M.; Arer, I.M. Outcomes of Total Parathyroidectomy with Autotransplantation versus Subtotal Parathyroidectomy Techniques for Secondary Hyperparathyroidism in Chronic Renal Failure. J. Coll. Physicians Surg. Pak. 2020, 30, 18–22. [Google Scholar] [CrossRef] [PubMed]
- Zmijewski, P.V.; Staloff, J.A.; Wozniak, M.J.; Mazzaglia, P.J. Subtotal Parathyroidectomy vs Total Parathyroidectomy with Autotransplantation for Secondary Hyperparathyroidism in Dialysis Patients: Short- and Long-Term Outcomes. J. Am. Coll. Surg. 2019, 228, 831–838. [Google Scholar] [CrossRef]
- Hiramitsu, T.; Hasegawa, Y.; Futamura, K.; Okada, M.; Goto, N.; Narumi, S.; Watarai, Y.; Tominaga, Y.; Ichimori, T. Treatment for secondary hyperparathyroidism focusing on parathyroidectomy. Front. Endocrinol. 2023, 14, 1169793. [Google Scholar] [CrossRef]
- Reitz, R.J.; Dreimiller, A.; Khil, A.; Horwitz, E.; McHenry, C.R. Ectopic and supernumerary parathyroid glands in patients with refractory renal hyperparathyroidism. Surgery 2021, 169, 513–518. [Google Scholar] [CrossRef]
- Kwak, S.; Fishman, E.K. Ectopic mediastinal parathyroid: A case report of recurrent secondary hyperparathyroidism. Radiol. Case Rep. 2023, 18, 2229–2231. [Google Scholar] [CrossRef]
- Lentsch, E.J.; Withrow, K.P.; Ackermann, D.; Bumpous, J.M. Parathyromatosis and recurrent hyperparathyroidism. Arch. Otolaryngol. Head Neck Surg. 2003, 129, 894–896. [Google Scholar] [CrossRef] [PubMed]
- Haimi, M.; Yang, J.W.; Kremer, R. Refractory hypercalcemia caused by parathyroid-hormone-related peptide secretion from a metastatic pancreatic neuroendocrine tumor: A case report. J. Med. Case Rep. 2025, 19, 54. [Google Scholar] [CrossRef] [PubMed]
- Vitale, G.; Gaudenzi, G.; Oldani, M.; Pandozzi, C.; Filice, A.; Jaafar, S.; Barrea, L.; Colao, A.; Faggiano, A.; Nike Group. Nutritional status and gastroenteropancreatic neuroendocrine neoplasms: Lights and shadows with a clinical guide from the NIKE Group. Rev. Endocr. Metab. Disord. 2025, 26, 161–174. [Google Scholar] [CrossRef] [PubMed]
- Faggiano, A.; Tavares, L.B.; Tauchmanova, L.; Milone, F.; Mansueto, G.; Ramundo, V.; De Caro, M.L.D.B.; Lombardi, G.; De Rosa, G.; Colao, A. Effect of treatment with depot somatostatin analogue octreotide on primary hyperparathyroidism (PHP) in multiple endocrine neoplasia type 1 (MEN1) patients. Clin. Endocrinol. 2008, 69, 756–762. [Google Scholar] [CrossRef]
- Storvall, S.; Leijon, H.; Ryhänen, E.; Louhimo, J.; Haglund, C.; Schalin-Jäntti, C.; Arola, J. Somatostatin receptor expression in parathyroid neoplasms. Endocr. Connect. 2019, 8, 1213–1223. [Google Scholar] [CrossRef]
- Lee, P.C.; Mateo, R.B.; Clarke, M.R.; Brown, M.L.; Carty, S.E. Parathyromatosis: A cause for recurrent hyperparathyroidism. Endocr. Pract. 2001, 7, 189–192. [Google Scholar] [CrossRef]
- Carsote, M.; Valea, A.; Dumitru, N.; Terzea, D.; Petrova, E.; Albu, S.; Buruiana, A.; Ghemigian, A. Metastases in daily endocrine practice. Arch. Balk. Med. Union 2016, 51, 476–480. [Google Scholar]
- Kamenicky, P.; Mirallie, E.; Hindie, E.; Vantyghem, M.-C.; Brunaud, L. Chapter 0: Introduction to the consensus on primary hyperparathyroidism from the French Society of Endocrinology, French speaking Association of Endocrine Surgery and French Society of Nuclear Medicine. Ann. Endocrinol. 2025, 86, 101689. [Google Scholar] [CrossRef]
- Wang, X.; Liang, Y.; Zhu, Z.; Li, W.; Shi, B.; Deng, Y.; Li, C.; Sha, O. Fn1 Regulates the Third Pharyngeal Pouch Patterning and Morphogenesis. J. Dent. Res. 2022, 101, 1082–1091. [Google Scholar] [CrossRef]
- Valea, A.; Ghervan, C.; Morar, A.; Pop, D.D.; Carsote, M.; Albu, S.E.; Georgescu, C.E.; Chiorean, A. Hashimoto’s thyroiditis and breast cancer: Coincidence or correlation? Arch. Balk. Med. Union 2016, 51, 129–132. [Google Scholar]
- Peissig, K.; Condie, B.G.; Manley, N.R. Embryology of the Parathyroid Glands. Endocrinol. Metab. Clin. N. Am. 2018, 47, 733–742. [Google Scholar] [CrossRef]
- Parvari, R.; Diaz, G.A.; Hershkovitz, E. Parathyroid development and the role of tubulin chaperone E. Horm. Res. 2007, 67, 12–21. [Google Scholar] [CrossRef] [PubMed]
- Zajac, J.D.; Danks, J.A. The development of the parathyroid gland: From fish to human. Curr. Opin. Nephrol. Hypertens. 2008, 17, 353–356. [Google Scholar] [CrossRef] [PubMed]
- Vasiliu, O. Therapeutic management of atypical antipsychotic-related metabolic dysfunctions using GLP-1 receptor agonists: A systematic review. Exper. Ther. Med. 2023, 26, 355. [Google Scholar] [CrossRef] [PubMed]
- di Masi, A.; Leboffe, L.; Sodo, A.; Tabacco, G.; Cesareo, R.; Sbroscia, M.; Giovannoni, I.; Taffon, C.; Crucitti, P.; Longo, F.; et al. Metabolic profile of human parathyroid adenoma. Endocrine 2020, 67, 699–707. [Google Scholar] [CrossRef]
- Xu, Q.; La, T.; Ye, K.; Wang, L.; Wang, S.; Hu, Y.; Teng, L.; Yan, L.; Li, J.; Zhang, Z.; et al. KMT2A and chronic inflammation as potential drivers of sporadic parathyroid adenoma. Clin. Transl. Med. 2024, 14, e1734. [Google Scholar] [CrossRef]
- Klein, P.; Alsleibi, S.; Cohen, O.; Ilany, J.; Hemi, R.; Barhod, E.; Vered, I.; Winder, O.; Avior, G.; Tripto-Shklonik, L. Parathyroid fine-needle aspiration with parathyroid hormone washout as a preoperative localisation of parathyroid adenoma-A retrospective study. Clin. Endocrinol. 2023, 99, 246–252. [Google Scholar] [CrossRef]
- Kendrick, M.L.; Charboneau, J.W.; Curlee, K.J.; Van Heerden, J.A.; Farley, D.R. Risk of parathyromatosis after fine-needle aspiration. Am. Surg. 2001, 67, 290–293; discussion 293–294. [Google Scholar] [CrossRef]
- Agarwal, G.; Dhingra, S.; Mishra, S.K.; Krishnani, N. Implantation of parathyroid carcinoma along fine needle aspiration track. Langenbecks Arch. Surg. 2006, 391, 623–626. [Google Scholar] [CrossRef]
- Spinelli, C.; Bonadio, A.G.; Berti, P.; Materazzi, G.; Miccoli, P. Cutaneous spreading of parathyroid carcinoma after fine needle aspiration cytology. J. Endocrinol. Investig. 2000, 23, 255–257. [Google Scholar] [CrossRef]
- Balbaloglu, H.; Deniz, O.; Ozaydin, R.Y.; Tasdoven, I.; Karadeniz Cakmak, G. Parathyroid fine needle aspiration with PTH washout: Can it lead to parathyroid cell seeding in primary hyperparathyroidism? Medicine 2024, 103, e37754. [Google Scholar] [CrossRef]
- Lou, X.; Wang, X.; Wang, Z.; Mao, G.; Zhu, W.; Wang, Y.; Pan, X.; Chen, Z.; Mo, Z. The Effect of Iodine Status on the Risk of Thyroid Nodules: A Cross-Sectional Study in Zhejiang, China. Int. J. Endocrinol. 2020, 2020, 3760375. [Google Scholar] [CrossRef] [PubMed]
- Li, Z.; Huang, Y.; Chen, X.; Wei, C.; Yang, P.; Xu, W. The Effect of Inflammation on the Formation of Thyroid Nodules. Int. J. Endocrinol. 2020, 2020, 9827349. [Google Scholar] [CrossRef] [PubMed]
- Choromańska, B.; Myśliwiec, P.; Kozłowski, T.; Łuba, M.; Wojskowicz, P.; Dadan, J.; Myśliwiec, H.; Choromańska, K.; Makarewicz, K.; Zalewska, A.; et al. Cross-Talk Between Nitrosative Stress, Inflammation and Hypoxia-Inducible Factor in Patients with Adrenal Masses. J. Inflamm. Res. 2021, 14, 6317–6330. [Google Scholar] [CrossRef] [PubMed]
- Herrera-Martínez, A.D.; Román, Á.R.; Corrales, E.P.; Idrobo, C.; Ramírez, P.P.; Rojas, P.M.; Lázaro, C.R.; Araujo-Castro, M. Adrenal incidentalomas, cortisol secretion and cancer: Is there a real crosstalk? Front. Endocrinol. 2024, 14, 1335202. [Google Scholar] [CrossRef]
- Pitsava, G.; Stratakis, C.A. Genetic Alterations in Benign Adrenal Tumors. Biomedicines 2022, 10, 1041. [Google Scholar] [CrossRef]
- Wiersinga, W.M.; Poppe, K.G.; Effraimidis, G. Hyperthyroidism: Aetiology, pathogenesis, diagnosis, management, complications, and prognosis. Lancet Diabetes Endocrinol. 2023, 11, 282–298. [Google Scholar] [CrossRef]
- Prete, A.; Bancos, I. Mild autonomous cortisol secretion: Pathophysiology, comorbidities and management approaches. Nat. Rev. Endocrinol. 2024, 20, 460–473. [Google Scholar] [CrossRef]
- Hasan, A.; Deyab, A.; Monazea, K.; Salem, A.; Futooh, Z.; Mostafa, M.A.; Youssef, A.; Nasr, M.; Omar, N.; Rabaan, A.A.; et al. Clinico-pathological assessment of surgically removed abdominal wall endometriomas following cesarean section. Ann. Med. Surg. 2021, 62, 219–224. [Google Scholar] [CrossRef]
- Yıldırım, D.; Tatar, C.; Doğan, O.; Hut, A.; Dönmez, T.; Akıncı, M.; Toptaş, M.; Bayık, R.N. Post-cesarean scar endometriosis. Turk. J. Obstet. Gynecol. 2018, 15, 33–38. [Google Scholar] [CrossRef]
- Touleimat, S.; Darwish, B.; Vassilieff, M.; Stochino Loi, E.; Hennetier, C.; Roman, H. Abdominal wall endometriosis following cesarean section: A study of the growth rate of parietal endometriosis implants. Minerva Ginecol. 2017, 69, 440–446. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).