Review and First Study of a Single-Port Robot in Pelvic Traumatology
Abstract
1. Introduction
2. Materials and Methods
2.1. Patient Demographics
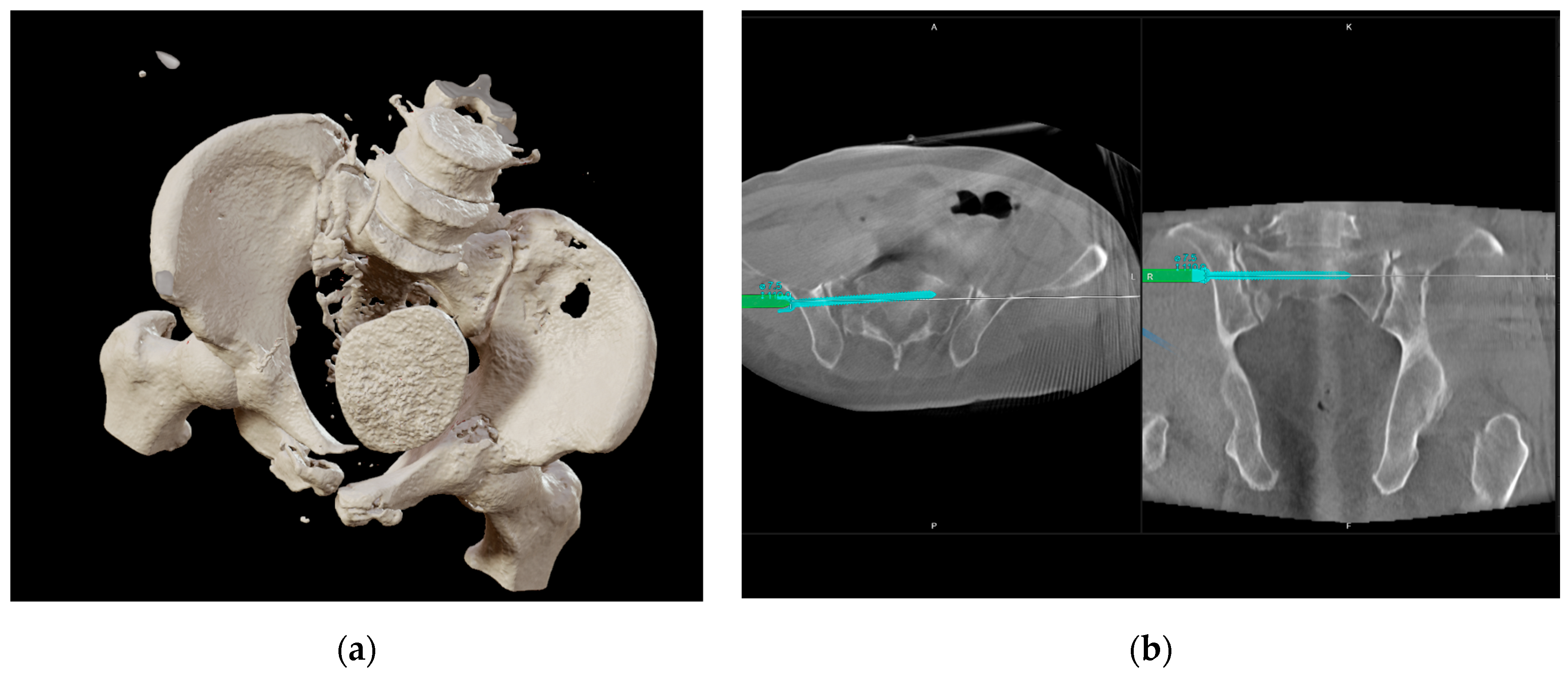
2.2. Injury Details and Initial Treatment
2.3. Indication
3. Results
3.1. Literature Review
3.2. Intervention
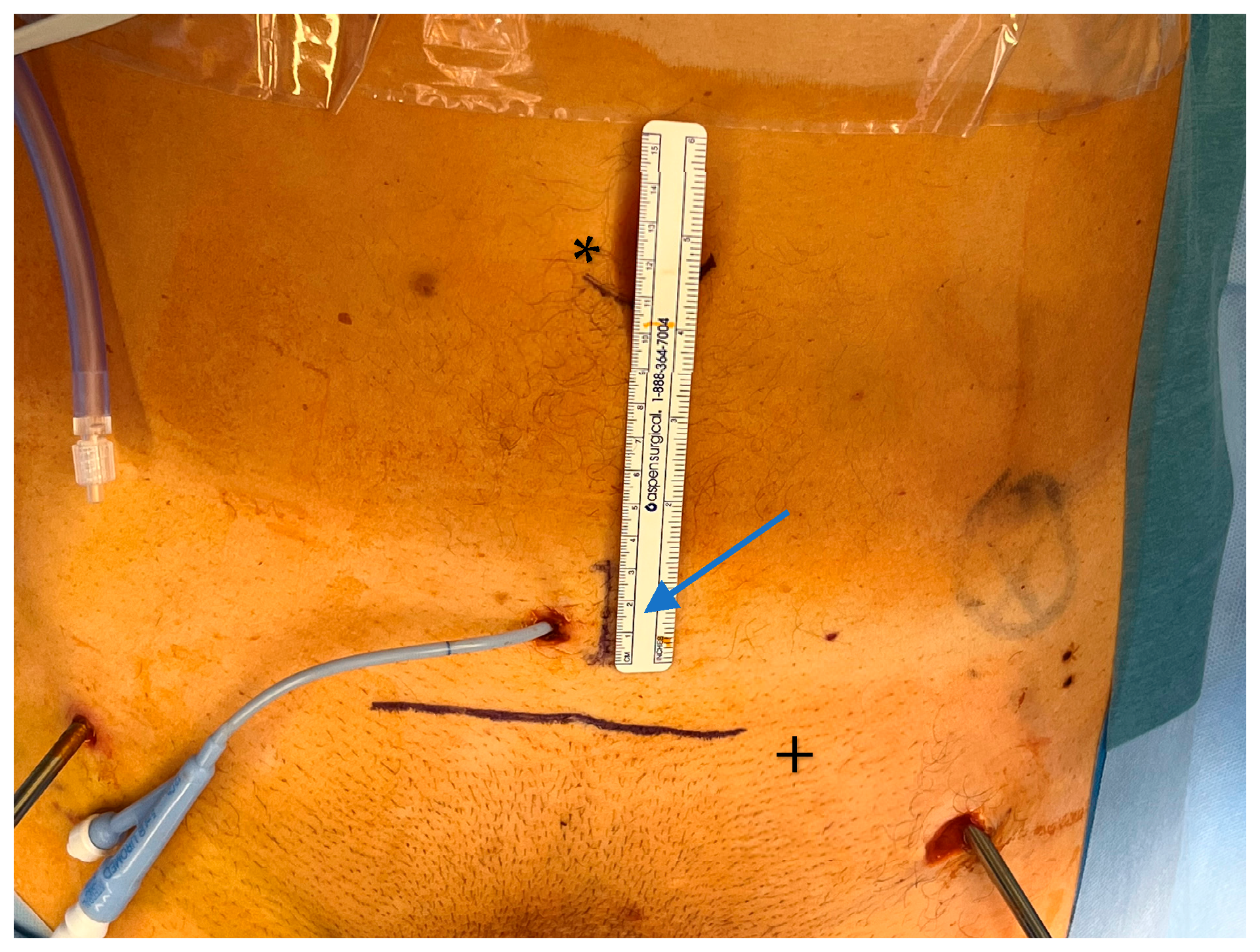
3.3. Approach
3.4. Urethral Repair
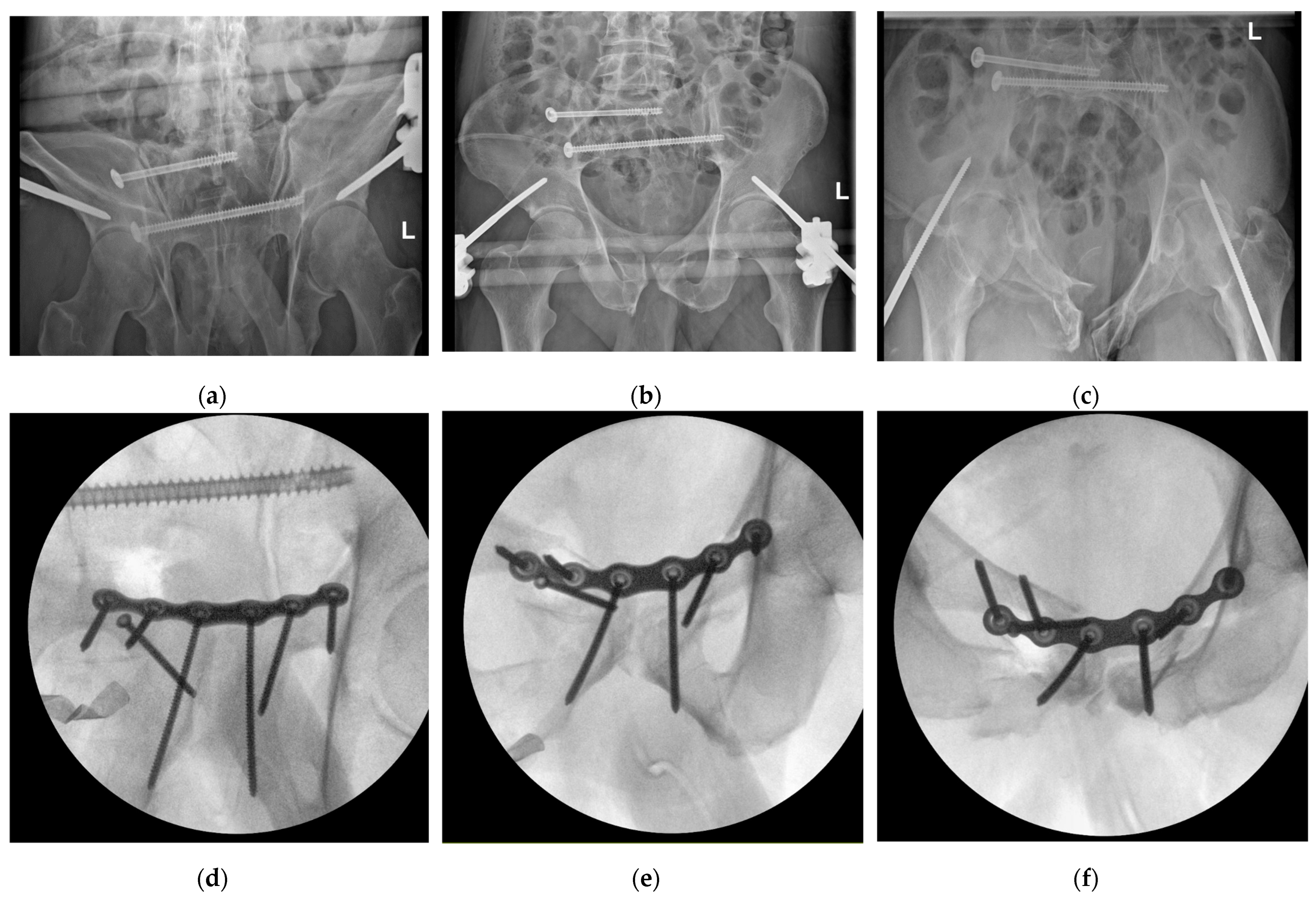
3.5. Fracture Repositioning and Osteosynthesis
3.6. Outcomes
4. Discussion
4.1. Literature Review
4.2. Interdisciplinary Approach
4.3. Fracture Treatment
4.4. Limitations and Need for Development
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Zhao, C.; Wang, Y.; Wu, X.; Zhu, G.; Shi, S. Design and Evaluation of an Intelligent Reduction Robot System for the Minimally Invasive Reduction in Pelvic Fractures. J. Orthop. Surg. Res. 2022, 17, 205. [Google Scholar] [CrossRef]
- Binder, J.; Kramer, W. Telerobotic Minimally Invasive Procedures in Urology--Laparoscopic Radical Prostatectomy. Surg. Technol. Int. 2002, 10, 45–48. [Google Scholar]
- Moschovas, M.C.; Bhat, S.; Sandri, M.; Rogers, T.; Onol, F.; Mazzone, E.; Roof, S.; Mottrie, A.; Patel, V. Comparing the Approach to Radical Prostatectomy Using the Multiport Da Vinci Xi and Da Vinci Sp Robots: A Propensity Score Analysis of Perioperative Outcomes. Eur. Urol. 2021, 79, 393–404. [Google Scholar] [CrossRef]
- Seon, K.E.; Lee, Y.J.; Lee, J.Y.; Nam, E.J.; Kim, S.; Kim, Y.T.; Kim, S.W. Initial Experience with the Da Vinci Sp Robot-Assisted Surgical Staging of Endometrial Cancer: A Retrospective Comparison with Conventional Laparotomy. J. Robot. Surg. 2023, 17, 2889–2898. [Google Scholar] [CrossRef] [PubMed]
- Abdelrahman, H.; El-Menyar, A.; Keil, H.; Alhammoud, A.; Ghouri, S.I.; Babikir, E.; Asim, M.; Muenzberg, M.; Al-Thani, H. Patterns, Management, and Outcomes of Traumatic Pelvic Fracture: Insights from a Multicenter Study. J. Orthop. Surg. Res. 2020, 15, 249. [Google Scholar] [CrossRef] [PubMed]
- Dabetic, U.; Grupkovic, J.; Zagorac, S.; Aleksandric, D.; Bogosavljevic, N.; Tulic, G. Advances in Managing Pelvic Fractures in Polytrauma: A Comprehensive Review. J. Clin. Med. 2025, 14, 1492. [Google Scholar] [CrossRef]
- Yu, Y.H.; Hsu, Y.H.; Chou, Y.C.; Liu, C.H.; Tseng, I.C.; Chen, I.J. Three-Year Functional Outcome after Open Pelvic Fracture Treatment: A Retrospective Case Series from a Level I Trauma Center. Eur. J. Orthop. Surg. Traumatol. 2023, 33, 937–945. [Google Scholar] [CrossRef] [PubMed]
- Küper, M.A.; Trulson, A.; Johannink, J.; Hirt, B.; Leis, A.; Hoßfeld, M.; Histing, T.; Herath, S.C.; Amend, B. Robotic-Assisted Plate Osteosynthesis of the Anterior Pelvic Ring and Acetabulum: An Anatomical Feasibility Study. J. Robot. Surg. 2022, 16, 1401–1407. [Google Scholar] [CrossRef]
- Ge, Y.; Zhao, C.; Wang, Y.; Wu, X. Robot-Assisted Autonomous Reduction of a Displaced Pelvic Fracture: A Case Report and Brief Literature Review. J. Clin. Med. 2022, 11, 1598. [Google Scholar] [CrossRef]
- Peng, Y.; Zhang, W.; Zhang, G.; Wang, X.; Zhang, S.; Ma, X.; Tang, P.; Zhang, L. Using the Starr Frame and Da Vinci Surgery System for Pelvic Fracture and Sacral Nerve Injury. J. Orthop. Surg. Res. 2019, 14, 29. [Google Scholar] [CrossRef]
- Schuijt, H.J.; Hundersmarck, D.; Smeeing, D.P.J.; van der Velde, D.; Weaver, M.J. Robot-Assisted Fracture Fixation in Orthopaedic Trauma Surgery: A Systematic Review. OTA Int. 2021, 4, e153. [Google Scholar] [CrossRef] [PubMed]
- Wu, Z.; Dai, Y.; Zeng, Y. Intelligent Robot-Assisted Fracture Reduction System for the Treatment of Unstable Pelvic Fractures. J. Orthop. Surg. Res. 2024, 19, 271. [Google Scholar] [CrossRef] [PubMed]
- Zhu, H.Z.; Li, D.G.; Li, Y.F.; Xu, W.Y.; Chen, G. A Systematic Review and Meta-Analysis Comparing Robotic-Assisted Percutaneous Screw Fixation and Conventional Surgical Techniques for Acetabular Fractures. J. Robot. Surg. 2024, 19, 17. [Google Scholar] [CrossRef]
- Hu, R.; Longo, U.G.; Pittman, J.; Nazarian, A. Robotic Innovations in Orthopedics: A Growing Landscape, Challenges, and Implications for Care. Osteology 2025, 5, 13. [Google Scholar] [CrossRef]
- Yuk, F.J.; Carr, M.T.; Schupper, A.J.; Lin, J.; Tadros, R.; Wiklund, P.; Sfakianos, J.; Steinberger, J. Da Vinci Meets Globus Excelsius Gps: A Totally Robotic Minimally Invasive Anterior and Posterior Lumbar Fusion. World Neurosurg. 2023, 180, 29–35. [Google Scholar] [CrossRef]
- Kabir, K.; von Rundstedt, F.C.; Roos, J.; Gathen, M. Robotic-Assisted Plate Fixation of the Anterior Acetabulum—Clinical Description of a New Technique. J. Orthop. Surg. Res. 2024, 19, 253. [Google Scholar] [CrossRef]
- Baumgarten, A.S.; Heinsimer, K.; Wiegand, L. Robotic Posterior Urethroplasty after Complete Urethral Transection During Abdominal Perineal Resection. Int. Braz. J. Urol. 2021, 47, 210. [Google Scholar]
- Leveillee, R.J.; Williams, S.K. Role of Robotics for Ureteral Pelvic Junction Obstruction and Ureteral Pathology. Curr. Opin. Urol. 2009, 19, 81–88. [Google Scholar] [CrossRef] [PubMed]
- Kim, S.; Buckley, J.C. Robotic Lower Urinary Tract Reconstruction. Urol. Clin. N. Am. 2021, 48, 103–112. [Google Scholar] [CrossRef]
- Chavali, J.S.; Adriana, M.; Pedraza, N.A.; Soputro, R.R.-C.; Mikesell, C.D.; Kaouk, J. Single-Port Extraperitoneal Vs. Multiport Transperitoneal Robot-Assisted Radical Prostatectomy: A Propensity Score-Matched Analysis. Cancers 2024, 16, 2994. [Google Scholar] [CrossRef]
- Tracey, A.T.; Eun, D.D.; Stifelman, M.D.; Hemal, A.K.; Stein, R.J.; Mottrie, A.; Cadeddu, J.A.; Stolzenburg, J.U.; Berger, A.K.; Buffi, N.; et al. Robotic-Assisted Laparoscopic Repair of Ureteral Injury: An Evidence-Based Review of Techniques and Outcomes. Minerva Urol. Nefrol. 2018, 70, 231–241. [Google Scholar] [CrossRef]
- Metzger, F.; Höch, A.; Herath, S.C.; Buschbeck, S.; Huber, S.F.; Schweigkofler, U.; Society Working Group on Pelvic Fractures of the German Trauma. Hemorrhage Control in Pelvic Ring Injuries: The Role of Pccds and Other Acute Measures in Germany. Eur. J. Trauma. Emerg. Surg. 2025, 51, 159. [Google Scholar] [CrossRef]
- Kabir, K.; Lingohr, P.; Jaenisch, M.; Hackenberg, R.K.; Sommer, N.; Ossendorff, R.; Welle, K.; Gathen, M. Total Endoscopic Anterior Pelvic Approach (Tapa)—A New Approach to the Internal Fixation of the Symphysis. Injury 2022, 53, 802–808. [Google Scholar] [CrossRef] [PubMed]
- Kuper, M.A.; Stockle, U.; Stuby, F.; Trulson, A. Clinical Experience with the New Easy (Endoscopic Approach to the Symphysis) Preparation Technique for Injuries of the Anterior Pelvic Ring. Z. Orthop. Unf. 2023, 161, 211–217. [Google Scholar] [CrossRef]
- Kuper, M.A.; Trulson, A.; Trulson, I.M.; Minarski, C.; Grunwald, L.; Gonser, C.; Bahrs, C.; Hirt, B.; Stockle, U.; Stuby, F.M. Easy (Endoscopic Approach to the Symphysis): A New Minimally Invasive Approach for the Plate Osteosynthesis of the Symphysis and the Anterior Pelvic Ring-a Cadaver Study and First Clinical Results. Eur. J. Trauma Emerg. Surg. 2019, 45, 745–755. [Google Scholar] [CrossRef]
- Hoskins, W.; Bucknill, A.; Wong, J.; Britton, E.; Judson, R.; Gumm, K.; Santos, R.; Sheehy, R.; Griffin, X. A Prospective Case Series for a Minimally Invasive Internal Fixation Device for Anterior Pelvic Ring Fractures. J. Orthop. Surg. Res. 2016, 11, 135. [Google Scholar] [CrossRef]
- Omran, K.; Nady, A.; Ali, A.H.A.; Khamies, M.S. Anterior Minimal Invasive Internal Fixator Versus Open Plating in Treatment of Unstable Pelvic Ring Injuries. Arch. Orthop. Trauma Surg. 2025, 145, 282. [Google Scholar] [CrossRef]
- Lodde, M.F.; Katthagen, J.C.; Schopper, C.O.; Zderic, I.; Richards, R.G.; Gueorguiev, B.; Raschke, M.J.; Hartensuer, R. Is Anterior Plating Superior to the Bilateral Use of Retrograde Transpubic Screws for Treatment of Straddle Pelvic Ring Fractures? A Biomechanical Investigation. J. Clin. Med. 2021, 10, 5049. [Google Scholar] [CrossRef]
- Lodde, M.F.; Katthagen, J.C.; Schopper, C.O.; Zderic, I.; Richards, G.; Gueorguiev, B.; Raschke, M.J.; Hartensuer, R. Biomechanical Comparison of Five Fixation Techniques for Unstable Fragility Fractures of the Pelvic Ring. J. Clin. Med. 2021, 10, 2326. [Google Scholar] [CrossRef] [PubMed]
- Yoon, Y.C.; Parry, J.A.; Mauffrey, C. Comparative Study on Anterior Pelvic Plating and Pubic Ramus Screw Fixation for Straddle Fracture: A Matched-Pair Outcome Analysis. Int. Orthop. 2024, 48, 3217–3225. [Google Scholar] [CrossRef] [PubMed]
- Li, J.; He, L.; Xia, C.; Zhu, M.; Zhang, W.; Huang, H. Comparison of the Mippo Technique and the Modified Stoppa Approach in the Treatment of Unstable Anterior Pelvic Ring Injuries: A Retrospective Cohort Study. BMC Musculoskelet. Disord. 2024, 25, 873. [Google Scholar] [CrossRef] [PubMed]



Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Rogenhofer, S.; Hartensuer, R. Review and First Study of a Single-Port Robot in Pelvic Traumatology. J. Clin. Med. 2025, 14, 6920. https://doi.org/10.3390/jcm14196920
Rogenhofer S, Hartensuer R. Review and First Study of a Single-Port Robot in Pelvic Traumatology. Journal of Clinical Medicine. 2025; 14(19):6920. https://doi.org/10.3390/jcm14196920
Chicago/Turabian StyleRogenhofer, Sebastian, and René Hartensuer. 2025. "Review and First Study of a Single-Port Robot in Pelvic Traumatology" Journal of Clinical Medicine 14, no. 19: 6920. https://doi.org/10.3390/jcm14196920
APA StyleRogenhofer, S., & Hartensuer, R. (2025). Review and First Study of a Single-Port Robot in Pelvic Traumatology. Journal of Clinical Medicine, 14(19), 6920. https://doi.org/10.3390/jcm14196920





