A Systematic Review and Meta-Analysis of Preoperative Characteristics and Postoperative Outcomes in Patients Undergoing Endoscopic Spine Surgery: Part I Endoscopic Microdiscectomy
Abstract
1. Introduction
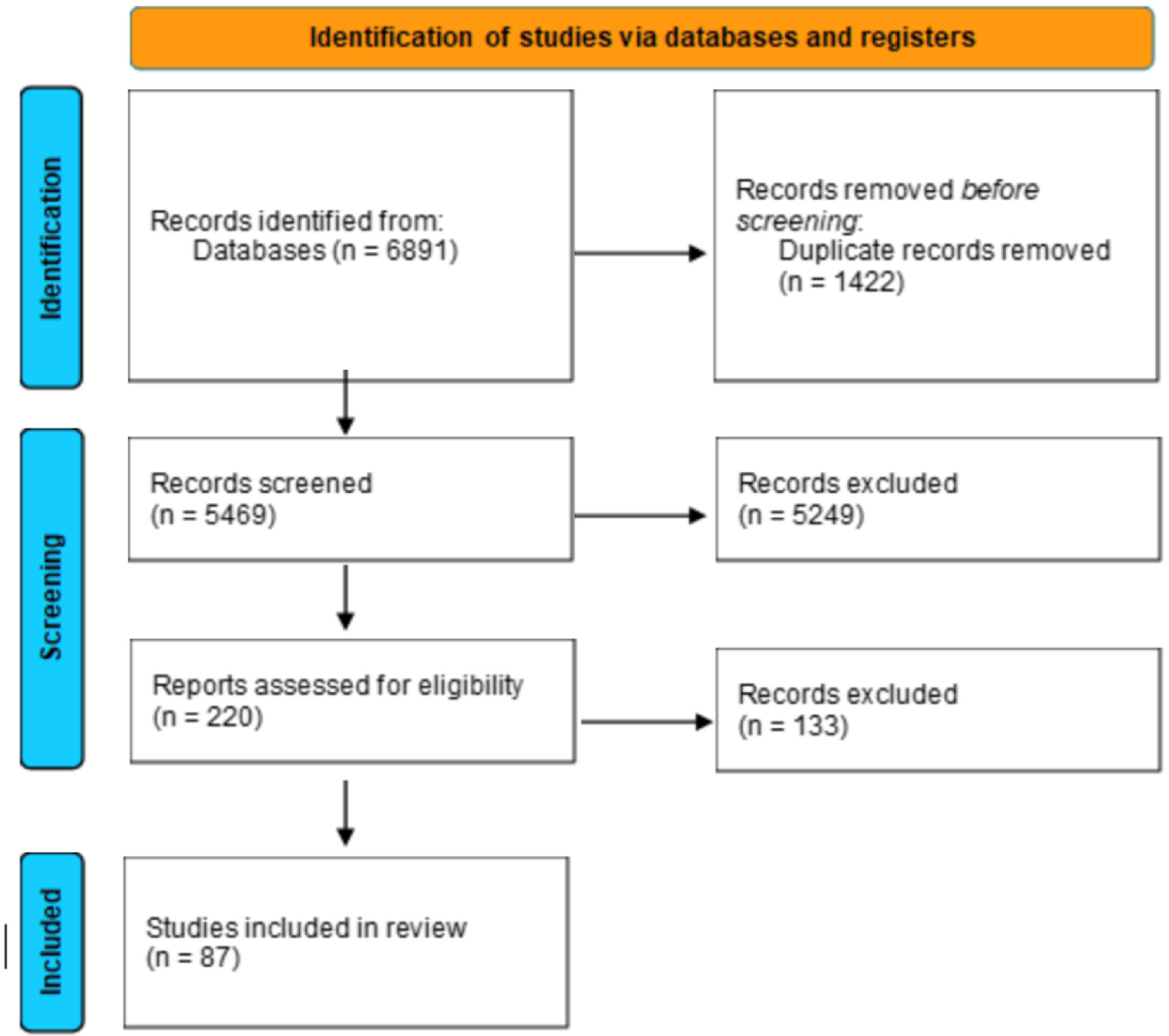
2. Materials and Methods
2.1. Summary
2.2. Data Source and Literature Searches
2.3. Study Eligibility and Selection
2.4. Data Abstraction and Synthesis
2.5. Assessment of Risk of Bias
2.6. Analytical Plan
3. Results
3.1. Pre-Operative Demographic and Clinical Data
3.2. Postoperative Outcomes and Complication Rates
3.3. MIS vs. Endoscopic Diskectomy
3.4. FELD: Interlaminar vs. Transforaminal
3.5. FELD and BELD
4. Discussion
5. Limitations
6. Conclusions
Author Contributions
Funding
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| PRISMA | Preferred Reporting Items for Systematic Reviews and Meta-Analyses |
| FELD | Full Endoscopic Lumbar Discectomy |
| BELD | Biportal Endoscopic Lumbar Discectomy |
| ELMD | Endoscopic Lumbar Microdiscectomy |
| MIS | Minimally Invasive Spine Surgery |
| VAS | Visual Analog Scale |
| BMI | Body Mass Index |
References
- Hincapié, C.A.; Kroismayr, D.; Hofstetter, L.; Kurmann, A.; Cancelliere, C.; Raja Rampersaud, Y.; Boyle, E.; Tomlinson, G.A.; Jadad, A.R.; Hartvigsen, J.; et al. Incidence of and risk factors for lumbar disc herniation with radiculopathy in adults: A systematic review. Eur. Spine J. 2025, 34, 263–294. [Google Scholar] [CrossRef]
- Zielinska, N.; Podgórski, M.; Haładaj, R.; Polguj, M.; Olewnik, Ł. Risk Factors of Intervertebral Disc Pathology-A Point of View Formerly and Today-A Review. J. Clin. Med. 2021, 10, 409. [Google Scholar] [CrossRef]
- Woolf, S.H.; Schoomaker, H. Life Expectancy and Mortality Rates in the United States, 1959-2017. Jama 2019, 322, 1996–2016. [Google Scholar] [CrossRef]
- Li, M.; Gong, W.; Wang, S.; Li, Z. Trends in body mass index, overweight and obesity among adults in the USA, the NHANES from 2003 to 2018: A repeat cross-sectional survey. BMJ Open 2022, 12, e065425. [Google Scholar] [CrossRef]
- Shriver, M.F.; Xie, J.J.; Tye, E.Y.; Rosenbaum, B.P.; Kshettry, V.R.; Benzel, E.C.; Mroz, T.E. Lumbar microdiscectomy complication rates: A systematic review and meta-analysis. Neurosurg. Focus FOC 2015, 39, E6. [Google Scholar] [CrossRef] [PubMed]
- Aiyer, R.; Noori, S.; Schirripa, F.; Schirripa, M.; Jain, S.; Aboud, T.; Mehta, N.; Elowitz, E.; Pahuta, M.; Datta, S. A systematic review of full endoscopic versus micro-endoscopic or open discectomy for lumbar disc herniation. Pain Manag. 2022, 12, 87–104. [Google Scholar] [CrossRef] [PubMed]
- Yang, C.-C.; Chen, C.-M.; Lin, M.H.-C.; Huang, W.-C.; Lee, M.-H.; Kim, J.-S.; Chen, K.-T. Complications of Full-Endoscopic Lumbar Discectomy versus Open Lumbar Microdiscectomy: A Systematic Review and Meta-Analysis. World Neurosurg. 2022, 168, 333–348. [Google Scholar] [CrossRef] [PubMed]
- Park, S.M.; Lee, H.J.; Park, H.J.; Choi, J.Y.; Kwon, O.; Lee, S.; Kim, H.J.; Yeom, J.S. Biportal endoscopic versus microscopic discectomy for lumbar herniated disc: A randomized controlled trial. Spine J. 2023, 23, 18–26. [Google Scholar] [CrossRef]
- Ali, R.; Hagan, M.J.; Bajaj, A.; Alastair Gibson, J.N.; Hofstetter, C.P.; Waschke, A.; Lewandrowski, K.-U.; Telfeian, A.E. Impact of the learning curve of percutaneous endoscopic lumbar discectomy on clinical outcomes: A systematic review. Interdiscip. Neurosurg. 2023, 32, 101738. [Google Scholar] [CrossRef]
- Burkett, D.; Brooks, N. Advances and Challenges of Endoscopic Spine Surgery. J. Clin. Med. 2024, 13, 1439. [Google Scholar] [CrossRef]
- Ahmed, M.; Nawaz, F.; Ullah, H.; Sameja, M.S. To compare the frequency of unintended durotomy in open discectomy versus endoscopic discectomy. Med. Forum Mon. 2019, 30, 105–108. [Google Scholar]
- Ahmed, O.E.F.; Molla, S.T.E.; Sabaa, A.M.E. Minimally invasive surgical management of symptomatic lumbar disc herniation: Can the endoscope replace the microscope? Egypt. J. Neurol. Psychiatry Neurosurg. 2022, 58, 107. [Google Scholar] [CrossRef]
- Ahn, J.S.; Lee, H.J.; Choi, D.J.; Lee, K.Y.; Hwang, S.J. Extraforaminal approach of biportal endoscopic spinal surgery: A new endoscopic technique for transforaminal decompression and discectomy. J. Neurosurg. Spine 2018, 28, 492–498. [Google Scholar] [CrossRef] [PubMed]
- An, J.; Zhang, J.; Yu, T.; Wu, J.; Nie, X.; He, T.; Yun, Z.; Liu, R.; Xue, W.; Qi, L.; et al. A Retrospective Comparative Study of Modified Percutaneous Endoscopic Transforaminal Discectomy and Open Lumbar Discectomy for Gluteal Pain Caused by Lumbar Disc Herniation. Front. Surg. 2022, 9, 930036. [Google Scholar] [CrossRef] [PubMed]
- Bai, J.; Zhang, W.; Liu, X.; Cheng, J.; Wang, X.; Ding, W.; Shen, Y. Percutaneous transforaminal endoscopic discectomy in the treatment of senior patients with lumbar degenerative disc disease. Exp. Ther. Med. 2019, 17, 874–882. [Google Scholar] [CrossRef] [PubMed]
- Belykh, E.; Giers, M.B.; Preul, M.C.; Theodore, N.; Byvaltsev, V. Prospective Comparison of Microsurgical, Tubular-Based Endoscopic, and Endoscopically Assisted Diskectomies: Clinical Effectiveness and Complications in Railway Workers. World Neurosurg. 2016, 90, 273–280. [Google Scholar] [CrossRef]
- Bhaisare, R.; Kamble, B.; Patond, K. Long-Term Results of Endoscopic Lumbar Discectomy by “Destandau’s Technique”. Asian Spine J. 2016, 10, 289. [Google Scholar] [CrossRef][Green Version]
- Casimiro, M. Short-Term Outcome Comparison Between Full-Endoscopic Interlaminar Approach and Open Minimally Invasive Microsurgical Technique for Treatment of Lumbar Disc Herniation. World Neurosurg. 2017, 108, 894–900.e891. [Google Scholar] [CrossRef]
- Chang, F.; Zhang, T.; Gao, G.; Yu, C.; Liu, P.; Zuo, G.; Huang, X. Therapeutic effect of percutaneous endoscopic lumbar discectomy on lumbar disc herniation and its effect on oxidative stress in patients with lumbar disc herniation. Exp. Ther. Med. 2018, 15, 295–299. [Google Scholar] [CrossRef]
- Chang, H.; Xu, J.; Yang, D.; Sun, J.; Gao, X.; Ding, W. Comparison of full-endoscopic foraminoplasty and lumbar discectomy (FEFLD), unilateral biportal endoscopic (UBE) discectomy, and microdiscectomy (MD) for symptomatic lumbar disc herniation. Eur Spine J 2023, 32, 542–554. [Google Scholar] [CrossRef]
- Chen, H.C.; Lee, C.H.; Wei, L.; Lui, T.N.; Lin, T.J. Comparison of percutaneous endoscopic lumbar discectomy and open lumbar surgery for adjacent segment degeneration and recurrent disc herniation. Neurol. Res. Int. 2015, 2015, 791943. [Google Scholar] [CrossRef]
- Chen, Q.; Zhang, Z.; Liu, B.; Liu, S. Evaluation of Percutaneous Transforaminal Endoscopic Discectomy in the Treatment of Lumbar Disc Herniation: A Retrospective Study. Orthop. Surg. 2021, 13, 599–607. [Google Scholar] [CrossRef]
- Chen, Z.; Pei, F. Learning Curve of Biportal Endoscopic Spinal Surgery: A Retrospective 2-Center Study. World Neurosurg. 2024, 187, e543–e550. [Google Scholar] [CrossRef] [PubMed]
- Cheng, L.; Cai, H.; Liu, Z.; Yu, Y.; Li, W.; Li, Q. Modified Full-Endoscopic Interlaminar Discectomy via an Inferior Endplate Approach for Lumbar Disc Herniation: Retrospective 3-Year Results from 321 Patients. World Neurosurg. 2020, 141, e537–e544. [Google Scholar] [CrossRef] [PubMed]
- Choi, K.C.; Kim, J.S.; Ryu, K.S.; Kang, B.U.; Ahn, Y.; Lee, S.H. Percutaneous endoscopic lumbar discectomy for L5-S1 disc herniation: Transforaminal versus interlaminar approach. Pain Physician 2013, 16, 547–556. [Google Scholar] [PubMed]
- Connolly, J.; Borja, A.J.; Kvint, S.; Glauser, G.; Strouz, K.; McClintock, S.D.; Marcotte, P.J.; Malhotra, N.R. Postoperative Outcomes and Resource Utilization Following Open vs Endoscopic Far Lateral Lumbar Discectomy. Int. J. Spine Surg. 2023, 17, 350–355. [Google Scholar] [CrossRef]
- Deng, C.; Feng, H.; Ma, X.; Chen, C.; Mei, J.; Sun, L. Comparing oblique lumbar interbody fusion with lateral screw fixation and percutaneous endoscopic transforaminal discectomy (OLIF-PETD) and minimally invasive transforaminal lumbar interbody fusion (MIS-TLIF) for the treatment of lumbar disc herniation complicated with lumbar instability. BMC Musculoskelet. Disord. 2022, 23, 1104. [Google Scholar] [CrossRef]
- Deng, Z.; Yang, W.; Han, L.; Gao, F.; Li, C.; Li, Y.; Liu, W.; Zhang, H. The minimally invasive spinal surgery in the treatment of posterior edge separation. Ann. Palliat. Med. 2020, 9, 1937–1943. [Google Scholar] [CrossRef]
- Duojun, W.; Hui, Z.; Zaijun, L.; Yuxiang, G.; Haihong, C. Enhanced recovery after surgery pathway reduces the length of hospital stay without additional complications in lumbar disc herniation treated by percutaneous endoscopic transforaminal discectomy. J. Orthop. Surg. Res. 2021, 16, 461. [Google Scholar] [CrossRef]
- Fan, G.; Zhang, H.; Gu, X.; Wang, C.; Guan, X.; Fan, Y.; He, S. Significant reduction of fluoroscopy repetition with lumbar localization system in minimally invasive spine surgery: A prospective study. Medicine 2017, 96, e6684. [Google Scholar] [CrossRef]
- Goparaju, P.; Rajamani, P.A.; Kulkarni, A.G.; Kumar, P.; Adbalwad, Y.M.; Bhojraj, S.; Nene, A.; Rajasekaran, S.; Acharya, S.; Bhanot, A.; et al. A 2-Year Outcomes and Complications of Various Techniques of Lumbar Discectomy: A Multicentric Prospective Study. Glob. Spine J. 2025, 15, 1003–1012. [Google Scholar] [CrossRef]
- Gu, X.; Zhu, W.; He, H.; Wang, Z.; Ding, S.; Guo, G. Efficacy and safety of percutaneous transforaminal endoscopic discectomy in the treatment of lumbar spinal stenosis combined with osteoporosis. Rev. Assoc. Med. Bras. 1992 2019, 65, 779–785. [Google Scholar] [CrossRef]
- Hanu, G.; Thota, S.; Venkat, K.; Changdra, V.V.R.; Prasad, B.C.M.; Kumar Reddy, S.; Geetanvita, N.; Indupriya, E. Comparative study of microsurgical lumbar discectomy and percutaneous endoscopic lumbar discectomy based on clinical outcome and muscle injury markers. J. Krishna Inst. Med. Sci. 2023, 12, 12–19. [Google Scholar]
- Hao, J.; Cheng, J.; Xue, H.; Zhang, F. Clinical comparison of unilateral biportal endoscopic discectomy with percutaneous endoscopic lumbar discectomy for single l4/5-level lumbar disk herniation. Pain. Pract. 2022, 22, 191–199. [Google Scholar] [CrossRef]
- He, S.; Sun, Z.; Wang, Y.; Ma, D.; Tan, W.; Lai, J. Combining YESS and TESSYS techniques during percutaneous transforaminal endoscopic discectomy for multilevel lumbar disc herniation. Medicine 2018, 97, e11240. [Google Scholar] [CrossRef] [PubMed]
- Hu, M.; Zhang, Y.; Zhao, W.J.; Liu, X.; Shi, P.Z.; Wang, J.W.; Cai, T.C.; Zhang, L. Perioperative Hidden Blood Loss in Lumbar Disk Herniation Patients With Percutaneous Endoscopic Transforaminal Discectomy and Influencing Factors. Clin. Spine Surg. 2022, 35, e438–e443. [Google Scholar] [CrossRef] [PubMed]
- Hu, Z.; Li, X.; Cui, J.; He, X.; Li, C.; Han, Y.; Pan, J.; Yang, M.; Tan, J.; Li, L. Significance of preoperative planning software for puncture and channel establishment in percutaneous endoscopic lumbar DISCECTOMY: A study of 40 cases. Int. J. Surg. 2017, 41, 97–103. [Google Scholar] [CrossRef] [PubMed]
- Jarebi, M.; Awaf, A.; Lefranc, M.; Peltier, J. A matched comparison of outcomes between percutaneous endoscopic lumbar discectomy and open lumbar microdiscectomy for the treatment of lumbar disc herniation: A 2-year retrospective cohort study. Spine J. 2021, 21, 114–121. [Google Scholar] [CrossRef]
- Jasper, G.P.; Francisco, G.M.; Telfeian, A.E. A retrospective evaluation of the clinical success of transforaminal endoscopic discectomy with foraminotomy in geriatric patients. Pain Physician 2013, 16, 225–229. [Google Scholar] [CrossRef]
- Jhala, A.; Mistry, M. Endoscopic lumbar discectomy: Experience of first 100 cases. Indian J. Orthop. 2010, 44, 184–190. [Google Scholar] [CrossRef]
- Jiang, H.W.; Chen, C.D.; Zhan, B.S.; Wang, Y.L.; Tang, P.; Jiang, X.S. Unilateral biportal endoscopic discectomy versus percutaneous endoscopic lumbar discectomy in the treatment of lumbar disc herniation: A retrospective study. J. Orthop. Surg. Res. 2022, 17, 30. [Google Scholar] [CrossRef]
- Jiang, X. Pin-assisted retraction technique in unilateral biportal endoscopic discectomy: A retrospective cohort study. Journal of international medical research. J. Int. Med. Res. 2023, 51, 3000605231164006. [Google Scholar] [CrossRef]
- Kandeel, M.M.; Yousef, M.G.A.K.; Saoud, A.M.F.; Abu-Elghait, Z.H.I. Percutaneous full-endoscopic transforaminal discectomy versus open microdiscectomy in the treatment of lumbar disc herniation: Randomized controlled trial. Egypt. J. Neurol. Psychiatry Neurosurg. 2024, 60, 11. [Google Scholar] [CrossRef]
- Kang, M.S.; Hwang, J.H.; Choi, D.J.; Chung, H.J.; Lee, J.H.; Kim, H.N.; Park, H.J. Clinical outcome of biportal endoscopic revisional lumbar discectomy for recurrent lumbar disc herniation. J. Orthop. Surg. Res. 2020, 15, 557. [Google Scholar] [CrossRef] [PubMed]
- Katzell, J.L. Risk factors predicting less favorable outcomes in endoscopic lumbar discectomies. J. Spine Surg. 2020, 6, S155–S164. [Google Scholar] [CrossRef]
- Kim, C.H.; Chung, C.K.; Choi, Y.; Shin, S.; Kim, M.J.; Lee, J.; Park, B.J. The Selection of Open or Percutaneous Endoscopic Lumbar Discectomy According to an Age Cut-off Point: Nationwide Cohort Study. Spine 2015, 40, E1063–E1070. [Google Scholar] [CrossRef]
- Kim, J.E.; Yoo, H.S.; Choi, D.J.; Park, E.J.; Jee, S.M. Comparison of Minimal Invasive Versus Biportal Endoscopic Transforaminal Lumbar Interbody Fusion for Single-level Lumbar Disease. Clin. Spine Surg. 2021, 34, e64–e71. [Google Scholar] [CrossRef]
- Kolcun, J.P.G.; Brusko, G.D.; Basil, G.W.; Epstein, R.; Wang, M.Y. Endoscopic transforaminal lumbar interbody fusion without general anesthesia: Operative and clinical outcomes in 100 consecutive patients with a minimum 1-year follow-up. Neurosurg. Focus 2019, 46, E14. [Google Scholar] [CrossRef]
- Kong, W.; Liao, W.; Ao, J.; Cao, G.; Qin, J.; Cai, Y. The Strategy and Early Clinical Outcome of Percutaneous Full-Endoscopic Interlaminar or Extraforaminal Approach for Treatment of Lumbar Disc Herniation. Biomed Res. Int. 2016, 2016, 4702946. [Google Scholar] [CrossRef]
- Kuonsongtum, V.; Paiboonsirijit, S.; Kesornsak, W.; Chaiyosboorana, V.; Rukskul, P.; Chumnanvej, S.; Ruetten, S. Result of full endoscopic uniportal lumbar discectomy: Preliminary report. J. Med. Assoc. Thai. 2009, 92, 776–780. [Google Scholar]
- Lee, J.H.; Lee, S.H. Which clinical and radiological variables could predict clinical outcomes of percutaneous endoscopic lumbar discectomy for treatment of patients with lumbosacral disc herniation? Spine J. 2018, 18, 1338–1346. [Google Scholar] [CrossRef]
- Li, H.; Ou, Y.; Xie, F.; Liang, W.; Tian, G.; Li, H. Linical efficacy of percutaneous endoscopic lumbar discectomy for the treatment of lumbar spinal stenosis in elderly patients: A retrospective study. J. Orthop. Surg. Res. 2020, 15, 441. [Google Scholar] [CrossRef] [PubMed]
- Li, T.; He, H.; Zhang, T.; Li, X.; Xie, W.; Huang, B.; Xu, F.; Xiong, C. Comprehensive comparison of three techniques for the treatment of adjacent segment degeneration after lumbar fusion. Front. Surg. 2023, 10, 1096483. [Google Scholar] [CrossRef] [PubMed]
- Li, Z.; Jiang, C.Y.; Xu, B.S. A comparative study on the clinical efficacy of percutaneous endoscopic lumbar discectomy and conventional open surgery in the treatment of lumbar disc herniation. Pak. J. Med. Sci. 2024, 40, 297–302. [Google Scholar] [CrossRef] [PubMed]
- Li, Z.Z.; Cao, Z.; Zhao, H.L.; Shang, W.L.; Hou, S.X. A Pilot Study of Full-Endoscopic Annulus Fibrosus Suture Following Lumbar Discectomy: Technique Notes and One-Year Follow-Up. Pain Physician 2020, 23, e497–e506. [Google Scholar] [CrossRef]
- Liang, J.Q.; Chen, C.; Zhao, H. Revision Surgery after Percutaneous Endoscopic Transforaminal Discectomy Compared with Primary Open Surgery for Symptomatic Lumbar Degenerative Disease. Orthop. Surg. 2019, 11, 620–627. [Google Scholar] [CrossRef]
- Liu, C.; Zhou, Y. Comparison Between Percutaneous Endoscopic Lumbar Discectomy and Minimally Invasive Transforaminal Lumbar Interbody Fusion for Lumbar Disc Herniation with Biradicular Symptoms. World Neurosurg. 2018, 120, e72–e79. [Google Scholar] [CrossRef]
- Lv, J.; Wang, X.; Chen, M.; Wu, J. Comparison of Percutaneous Transforaminal Endoscopic Discectomy with and without Epidural Steroid Application in the Treatment of Lumbar Disc Herniation: A Minimum of 2 Years of Follow-Up. Turk. Neurosurg. 2020, 30, 387–393. [Google Scholar] [CrossRef]
- Ma, C.; Li, H.; Wei, Y.; Liu, L.; Shi, Y.; Ren, Y. Percutaneous Endoscopic Lumbar Discectomy for Huge Lumbar Disc Herniation with Complete Dural Sac Stenosis via an Interlaminar Approach: An Observational Retrospective Cohort Study. Int. J. Gen. Med. 2021, 14, 8317–8324. [Google Scholar] [CrossRef]
- Mlaka, J.; Rapcan, R.; Burianek, M.; Rapcanova, S.; Gajdos, M.; Kocanova, M.; Griger, M.; Kovalicova, L.; Vaskova, J.; Kocan, L. Endoscopic discectomy as an effective treatment of a herniated intervertebral disc. Bratisl. Lek. Listy 2020, 121, 199–205. [Google Scholar] [CrossRef]
- Morgenstern, R.; Morgenstern, C. Percutaneous Transforaminal Lumbar Interbody Fusion (pTLIF) with a Posterolateral Approach for the Treatment of Denegerative Disk Disease: Feasibility and Preliminary Results. Int. J. Spine Surg. 2015, 9, 41. [Google Scholar] [CrossRef]
- Nakamura, J.I.; Yoshihara, K. Initial Clinical Outcomes of Percutaneous Full-Endoscopic Lumbar Discectomy Using an Interlaminar Approach at the L4-L5. Pain Physician 2017, 20, e507–e512. [Google Scholar] [CrossRef]
- Ouyang, Z.H.; Tang, M.; Li, H.W.; Zou, M.X.; Li, X.L.; Wang, W.J.; Yan, Y.G. Full-Endoscopic Foraminoplasty Using a Visualized Bone Reamer in the Treatment of Lumbar Disc Herniation: A Retrospective Study of 80 Cases. World Neurosurg. 2021, 149, e292–e297. [Google Scholar] [CrossRef]
- Pang, J.Y.; Tan, F.; Chen, W.W.; Li, C.H.; Dou, S.P.; Guo, J.R.; Zhao, L.Y. Comparison of microendoscopic discectomy and open discectomy for single-segment lumbar disc herniation. World J. Clin. Cases 2020, 8, 2942–2949. [Google Scholar] [CrossRef] [PubMed]
- Priola, S.M.; Ganau, M.; Raffa, G.; Scibilia, A.; Farrash, F.; Germanò, A. A Pilot Study of Percutaneous Interlaminar Endoscopic Lumbar Sequestrectomy: A Modern Strategy to Tackle Medically-Refractory Radiculopathies and Restore Spinal Function. Neurospine 2019, 16, 120–129. [Google Scholar] [CrossRef] [PubMed]
- Rao, P.; Maharaj, M.M.; Maalouly, J. Endoscopic lumbar discectomy vs microdiscectomy: Early results, complications and learning curve an Australian perspective. Interdiscip. Neurosurg. 2023, 31, 101674. [Google Scholar] [CrossRef]
- Ren, W.; Chen, Y.; Xiang, L. Minimally invasive surgical techniques for the therapy of far lateral disc herniation in middle-aged and elderly patients. Comput. Assist. Surg. 2019, 24, 13–19. [Google Scholar] [CrossRef]
- Ruetten, S.; Komp, M.; Merk, H.; Godolias, G. Full-endoscopic interlaminar and transforaminal lumbar discectomy versus conventional microsurgical technique: A prospective, randomized, controlled study. Spine 2008, 33, 931–939. [Google Scholar] [CrossRef]
- Ruetten, S.; Komp, M.; Merk, H.; Godolias, G. Recurrent lumbar disc herniation after conventional discectomy: A prospective, randomized study comparing full-endoscopic interlaminar and transforaminal versus microsurgical revision. J. Spinal Disord. Tech. 2009, 22, 122–129. [Google Scholar] [CrossRef]
- Sharma, S.B.; Lin, G.X.; Jabri, H.; Sidappa, N.D.; Song, M.S.; Choi, K.C.; Kim, J.S. Radiographic and clinical outcomes of huge lumbar disc herniations treated by transforaminal endoscopic discectomy. Clin. Neurol. Neurosurg. 2019, 185, 105485. [Google Scholar] [CrossRef]
- Son, S.; Ahn, Y.; Lee, S.G.; Kim, W.K.; Yoo, B.R.; Jung, J.M.; Cho, J. Learning curve of percutaneous endoscopic transforaminal lumbar discectomy by a single surgeon. Medicine 2021, 100, e24346. [Google Scholar] [CrossRef] [PubMed]
- Son, S.; Yoo, B.R.; Kim, H.J.; Song, S.K.; Ahn, Y. Efficacy of Transforaminal Endoscopic Lumbar Discectomy in Elderly Patients Over 65 Years of Age Compared to Young Adults. Neurospine 2023, 20, 597–607. [Google Scholar] [CrossRef] [PubMed]
- Tang, Y.; Li, H.; Qin, W.; Liu, Z.; Liu, H.; Zhang, J.; Mao, H.; Zhang, K.; Chen, K. Comparison of percutaneous endoscopic interlaminar discectomy and conventional open lumbar discectomy for L4/5 and L5/S1 double-segmental lumbar disk herniation. J. Orthop. Surg. Res. 2023, 18, 950. [Google Scholar] [CrossRef]
- Teli, M.; Lovi, A.; Brayda-Bruno, M.; Zagra, A.; Corriero, A.; Giudici, F.; Minoia, L. Higher risk of dural tears and recurrent herniation with lumbar micro-endoscopic discectomy. Eur. Spine J. 2010, 19, 443–450. [Google Scholar] [CrossRef] [PubMed]
- Wang, B.; Lü, G.; Patel, A.A.; Ren, P.; Cheng, I. An evaluation of the learning curve for a complex surgical technique: The full endoscopic interlaminar approach for lumbar disc herniations. Spine J. 2011, 11, 122–130. [Google Scholar] [CrossRef]
- Wang, H.; Huang, B.; Li, C.; Zhang, Z.; Wang, J.; Zheng, W.; Zhou, Y. Learning curve for percutaneous endoscopic lumbar discectomy depending on the surgeon’s training level of minimally invasive spine surgery. Clin. Neurol. Neurosurg. 2013, 115, 1987–1991. [Google Scholar] [CrossRef]
- Wang, Z.; Huang, S.; Xu, L.; Bu, J.; Liu, G.; Wang, H.; Liang, J.; Xia, M.; Chen, T.; Ma, C.; et al. A retrospective study of the mid-term efficacy of full-endoscopic annulus fibrosus suture following lumbar discectomy. Front. Surg. 2022, 9, 1011746. [Google Scholar] [CrossRef]
- Wang, Z.; Tan, Y.; Fu, K.; Meng, Z.; Wang, L. Minimally invasive trans-superior articular process percutaneous endoscopic lumbar discectomy with robot assistance. BMC Musculoskelet. Disord. 2022, 23, 1144. [Google Scholar] [CrossRef]
- Wasinpongwanich, K.; Pongpirul, K.; Lwin, K.M.M.; Kesornsak, W.; Kuansongtham, V.; Ruetten, S. Full-Endoscopic Interlaminar Lumbar Discectomy: Retrospective Review of Clinical Results and Complications in 545 International Patients. World Neurosurg. 2019, 132, e922–e928. [Google Scholar] [CrossRef]
- Wei, H.; Shunli, K.; Zehua, J.; Tengfei, Z.; Yidong, L.; Rusen, Z. Comparative Study of Three Minimally Invasive Surgical Approaches for the Treatment of L5/S1 Lumbar Intervertebral Disc Herniation. Turk. Neurosurg. 2021, 31, 324–332. [Google Scholar] [CrossRef]
- Wu, J.; Zhang, C.; Lu, K.; Li, C.; Zhou, Y. Percutaneous Endoscopic Lumbar Reoperation for Recurrent Sciatica Symptoms: A Retrospective Analysis of Outcomes and Prognostic Factors in 94 Patients. World Neurosurg. 2018, 109, e761–e769. [Google Scholar] [CrossRef] [PubMed]
- Wu, X.; Ma, Y.; Ding, R.; Xiao, X.; Yang, D. Should adjacent asymptomatic lumbar disc herniation be simultaneously rectified? A retrospective cohort study of 371 cases that received an open fusion or endoscopic discectomy only on symptomatic segments. Spine J. 2021, 21, 411–417. [Google Scholar] [CrossRef] [PubMed]
- Xie, W.; Wu, C.J.; Li, Y.; Lu, Q.L.; Gan, X.W.; Li, X.G.; Tang, J. Effect analysis of sacral canal therapy combined with Fufang Wulingzhi Tangjiang in the treatment of residual root pain after lumbar surgery. Eur. Rev. Med. Pharmacol. Sci. 2022, 26, 9212–9220. [Google Scholar] [CrossRef] [PubMed]
- Xu, H.; Liu, X.; Liu, G.; Zhao, J.; Fu, Q.; Xu, B. Learning curve of full-endoscopic technique through interlaminar approach for L5/S1 disk herniations. Cell Biochem. Biophys. 2014, 70, 1069–1074. [Google Scholar] [CrossRef]
- Xu, J.; Li, Y.; Wang, B.; Lv, G.H.; Wu, P.; Dai, Y.; Jiang, B.; Zheng, Z.; Xiao, S. Percutaneous Endoscopic Lumbar Discectomy for Lumbar Disc Herniation with Modic Changes via a Transforaminal Approach: A Retrospective Study. Pain Physician 2019, 22, E601–E608. [Google Scholar] [CrossRef]
- Xu, P.; Yuan, J.; Wu, T.; He, D.; Miao, X.; Cheng, X. Modified Percutaneous Endoscopic Interlaminar Discectomy through the Near-spinous Process Approach for L4/5 Disc Herniation: A Retrospective Clinical Study. Orthop. Surg. 2024, 16, 1064–1072. [Google Scholar] [CrossRef]
- Xu, Z.; Zheng, J.-C.; Sun, B.; Zhang, K.; Wang, Y.-H.; Shi, C.-G.; Wu, H.-Q.; Wu, X.-D.; Chen, H.-J.; Yuan, W. Bi-needle technique versus transforaminal endoscopic spine system technique for percutaneous endoscopic lumbar discectomy in treating intervertebral disc calcification: A propensity score matched cohort analysis. Br. J. Neurosurg. 2020, 35, 245–250. [Google Scholar] [CrossRef]
- Yang, H.; Gao, W.; Duan, Y.; Kang, X.; He, B.; Hao, D.; Wang, B. Two-dimensional fluoroscopy-guided robot-assisted percutaneous endoscopic transforaminal discectomy: A retrospective cohort study. Am. J. Transl. Res. 2022, 14, 3121–3131. [Google Scholar]
- Yankang, L.; Leiming, Z.; Lewandrowski, K.U.; Xiangyu, T.; Zexing, Z.; Jianbiao, X.; Lin, Z.; Heng, Y.; Xifeng, Z. Full Endoscopic Lumbar Discectomy Versus Laminectomy for Cauda Equina Syndrome. Int. J. Spine Surg. 2021, 15, 105–112. [Google Scholar] [CrossRef]
- Yeung, A.; Wei, S.H. Surgical outcome of workman’s comp patients undergoing endoscopic foraminal decompression for lumbar herniated disc. J. Spine Surg. 2020, 6, S116–S119. [Google Scholar] [CrossRef]
- Ying, J.; Huang, K.; Zhu, M.; Zhou, B.; Wang, Y.; Chen, B.; Teng, H. The Effect and Feasibility Study of Transforaminal Percutaneous Endoscopic Lumbar Discectomy Via Superior Border of Inferior Pedicle Approach for Down-Migrated Intracanal Disc Herniations. Medicine 2016, 95, e2899. [Google Scholar] [CrossRef] [PubMed]
- Yu, H.; Zhu, B.; Song, Q.; Liu, X. Evaluation of full-endoscopic lumbar discectomy in the treatment of obese adolescents with lumbar disc herniation: A retrospective study. BMC Musculoskelet. Disord. 2021, 22, 562. [Google Scholar] [CrossRef] [PubMed]
- Yu, P.; Zan, P.; Zhang, X.; Qiang, H.; Samsonraj, R.M.; Tang, J.; Huang, P. Comparison of Percutaneous Transforaminal Endoscopic Discectomy and Microendoscopic Discectomy for the Surgical Management of Symptomatic Lumbar Disc Herniation: A Multicenter Retrospective Cohort Study with a Minimum of 2 Years’ Follow-Up. Pain Physician 2021, 24, e117–e125. [Google Scholar]
- Yu, Z.; Lu, Y.; Li, Y.; An, Y.; Wang, B. A one-step foraminoplasty via a large trephine in percutaneous endoscopic transforaminal discectomy for the treatment of lumbar disc herniation. PLoS ONE 2022, 17, e0268564. [Google Scholar] [CrossRef] [PubMed]
- Zhang, Q.; Du, P.; Zhang, Y. The effect of locating and sliding of facet combined with percutaneous endoscopic lumbar discectomy on cell inflammatory indicators and the treatment of disc herniation. Cell. Mol. Biol. 2022, 67, 181–187. [Google Scholar] [CrossRef]
- Zhang, Y.; Zhu, H.; Zhou, Z.; Wu, J.; Sun, Y.; Shen, X.; Li, C. Comparison Between Percutaneous Transforaminal Endoscopic Discectomy and Fenestration in the Treatment of Degenerative Lumbar Spinal Stenosis. Med. Sci. Monit. 2020, 26, e926631. [Google Scholar] [CrossRef]
- Zhou, Z.; Ni, H.J.; Hu, S.; Fan, Y.S.; Wang, C.F.; Chen, X.; Zhu, Y.J.; Li, G.; Liu, F.; Feng, C.B.; et al. Original Designed Uniportal-Bichannel Spinal Endoscopic System (UBiSES) for Foraminoplasty in Percutaneous Endoscopic Transforaminal Discectomy. Orthop. Surg. 2021, 13, 1987–1999. [Google Scholar] [CrossRef]
- Page, P.S.; Ammanuel, S.G.; Josiah, D.T. Evaluation of Endoscopic Versus Open Lumbar Discectomy: A Multi-Center Retrospective Review Utilizing the American College of Surgeons’ National Surgical Quality Improvement Program (ACS-NSQIP) Database. Cureus 2022, 14, e25202. [Google Scholar] [CrossRef]
- Leyendecker, J.; Prasse, T.; Rückels, P.; Köster, M.; Rumswinkel, L.; Schunk, V.; Marossa, I.; Eysel, P.; Bredow, J.; Hofstetter, C.P.; et al. Full-endoscopic spine-surgery in the elderly and patients with comorbidities. Sci. Rep. 2024, 14, 29188. [Google Scholar] [CrossRef]
- Patgaonkar, P.; Datar, G.; Agrawal, U.; Palanikumar, C.; Agrawal, A.; Goyal, V.; Patel, V. Suprailiac versus transiliac approach in transforaminal endoscopic discectomy at L5-S1: A new surgical classification of L5-iliac crest relationship and guidelines for approach. J. Spine Surg. 2020, 6, S145–S154. [Google Scholar] [CrossRef]
- Chen, K.T.; Jabri, H.; Lokanath, Y.K.; Song, M.S.; Kim, J.S. The evolution of interlaminar endoscopic spine surgery. J. Spine Surg. 2020, 6, 502–512. [Google Scholar] [CrossRef]
- Shepard, N.; Cho, W. Recurrent Lumbar Disc Herniation: A Review. Glob. Spine J. 2019, 9, 202–209. [Google Scholar] [CrossRef]
- Hao, L.; Li, S.; Liu, J.; Shan, Z.; Fan, S.; Zhao, F. Recurrent disc herniation following percutaneous endoscopic lumbar discectomy preferentially occurs when Modic changes are present. J. Orthop. Surg. Res. 2020, 15, 176. [Google Scholar] [CrossRef]
- Shamim, P.; Park, C.W. Why the Large Working Channel Uniportal Endoscope is Better for Patients with Obesity Than the Unilateral Biportal Endoscope at Lower Lumbar Levels: A Technical Note. J. Minim. Invasive Spine Surg. Tech. 2025, 10, S27–S33. [Google Scholar] [CrossRef]
- Rasouli, M.R.; Rahimi-Movaghar, V.; Shokraneh, F.; Moradi-Lakeh, M.; Chou, R. Minimally invasive discectomy versus microdiscectomy/open discectomy for symptomatic lumbar disc herniation. Cochrane Database Syst. Rev. 2014, 2014, Cd010328. [Google Scholar] [CrossRef]
| Endoscopy Group | 95% CI | Open Group | 95% CI | p-Value | |
|---|---|---|---|---|---|
| (N = 2074) | (N = 1167) | ||||
| Gender (Male %) | 58% | 56–60% | 55% | 52–58% | 0.02 |
| Age (Mean) | 48.2 years | 47.5–48.9 | 52.7 years | 51.3–54.1 | <0.001 |
| BMI (Mean) | 25.8 | 25.5–26.1 | 26.5 | 26.1–26.9 | 0.03 |
| Duration of Symptoms | 6.3 months | 6.0–6.6 | 8.1 months | 7.7–8.5 | <0.001 |
| Charlson Comorbidity Index | 4.44 | ±1.62 (SD) | 2.78 | ±0.92 (SD) | 0.02 |
| Level of Surgery | |||||
| L3–L4 | 8% (166) | 7–9% | 5% (58) | 4–6% | <0.001 |
| L4–L5 | 62% (1286) | 60–64% | 58% (677) | 55–61% | |
| L5–S1 | 30% (622) | 28–32% | 37% (432) | 34–40% | |
| Symptom Prevalence | |||||
| Radiculopathy | 78% (1618) | 76–80% | 72% (840) | 69–75% | 0.01 |
| Back Pain | 15% (311) | 13–17% | 20% (233) | 18–22% | |
| Weakness | 7% (145) | 6–8% | 8% (93) | 6–10% |
| VAS Leg Pain | Endoscopy Group | Open Group | 95% CI (Endoscopy vs. OD) | p-Value |
|---|---|---|---|---|
| 1 day | 1.7 ± 1.3 | 3.1 ± 2.2 | Δ = −1.4 [−1.7 to −1.1] (1 day) | <0.001 (t-test) |
| 1 year | 1.2 ± 0.6 | 2.1 ± 1.5 | ||
| Complications | ||||
| Dural Tear | Dural Tear: 13 (1.0%) | Dural Tear: 9 (2.2%) | OR: 0.91 [0.55–1.51] (Recurrence) | 0.71 (Fisher’s) |
| Wound Infection | Infection: 12 (0.9%) | Infection: 15 (3.7%) | OR: 0.71 [0.33–1.53] (Recurrence) | 0.38 (Fisher’s) |
| Recurrent disk | Recurrence: 63 (4.8%) | Recurrence: 21 (5.2%) | OR: 0.19 [0.11–0.31] (Recurrence) | <0.001 (Fisher’s) |
| Variable | MIS Group (N = 249) | Endoscopy Group (N = 1317) | 95% CI (MED vs. Other) | p-Value |
|---|---|---|---|---|
| Gender (Male:Female) | 146 M:103 F (58.6% M) | 725 M:592 F (55.1% M) | 0.24 | |
| Age (Years) | 44.9 ± 12.6 | 45.8 ± 11.3 | 0.38 | |
| BMI | 27.1 ± 2.8 (reported in 70% of MED cases) | 26.8 ± 3.1 (reported in 68% of cases) | 0.52 | |
| Duration of Symptoms | 82 ± 16.3 days | 84 ± 12.9 days (PTED), 85 ± 10.6 days (PEID) | 0.41 | |
| Level of surgery | ||||
| L2/L3 | 17 (6.8%) | 28 (2.1%) | [1.72–6.11] | <0.001 |
| L3/L4 | 23 (9.2%) | 48 (3.6%) | [1.53–4.28] | 0.001 |
| L4/L5 | 113 (45.4%) | 284 (21.6%) | [1.68–2.63] | <0.001 |
| L5/S1 | 96 (38.6%) | 231 (17.5%) | [1.73–2.82] | <0.001 |
| Symptom prevalence | ||||
| Radiculopathy | 249 (100%) | 1317 (100%) | [1.00–1.00] | 1 |
| Motor Weakness | 31 (12.4%) | 121 (9.2%) | [0.91–2.00] | 0.13 |
| Sensory Loss | 190 (76.3%) | 893 (67.8%) | [1.02–1.24] | 0.02 |
| Hyporeflexia | 13 (5.2%) | 45 (3.4%) | [0.82–2.86] | 0.18 |
| Post-operative Complications | ||||
| disk Recurrence | 10 (4%) | 63 (4.8%) | OR: 0.83 [0.41–1.66] | 0.59 (Fisher’s) |
| Dural Tear | 0 | 13 (1%) | OR: 0.21 [0.01–3.476] | 0.27 |
| Infection | 3 (1.2%) | 12 (0.9%) | OR: 1.28 [0.36–4.58] | 1.28 |
| VAS Leg Pain (Post-Op) | 1.9 ± 1.5 (1 day) | 1.7 ± 1.3 (1 day) | Δ = 0.2 [−0.1–0.5] (1 day) | 0.09 |
| 1.4 ± 0.8 (1 year) | 1.2 ± 0.6 (1 year) | Δ = 0.2 [−0.1–0.5] (1 day) | ||
| Variable | Interlaminar Group (N = 483) | Transforaminal Group (N = 1083) | 95% CI (Interlaminar Vs. Transforaminal) | p-Value |
|---|---|---|---|---|
| Gender (Male:Female) | 253 M:230 F (52.4% M) | 603 M:480 F (55.7% M) | 0.18 | |
| Age (Years) | 46.8 ± 11.2 | 44.9 ± 12.4 | 0.006 | |
| BMI | 26.5 ± 2.9 (reported in 70% of cases) | 26.8 ± 3.1 (reported in 66% of cases) | 0.09 | |
| Duration of Symptoms | 85 ± 10.6 days | 84 ± 12.9 days | 0.28 | |
| VAS Leg Pain (Post-Op) | 1.8 ± 1.4 (1 day) | 1.6 ± 1.2 (1 day) | Δ = 0.2 [−0.1–0.5] (1 day) | 0.07 |
| 1.3 ± 0.7 (1 year) | 1.1 ± 0.6 (1 year) | |||
| Complications | Recurrence: 22 (4.6%) | Recurrence: 41 (3.8%) | OR: 1.24 [0.73–2.10] (Recurrence) | 0.43 (Fisher’s) |
| Dural Tear: 7 (1.4%) | Dural Tear: 6 (0.6%) | OR: 2.70 [0.90–8.05] (Recurrence) | 1.65 | |
| Infection: 5 (1.0%) | Infection: 7 (0.6%) | OR: 1.65 [0.36–5.22] (Recurrence) | 0.4 |
| Level | Interlaminar Group (N = 483) | Transforaminal Group (N = 1083) | Risk Ratio (Interlaminar Vs. Transforaminal) | 95% CI | p-Value |
|---|---|---|---|---|---|
| L2/L3 | 8 (1.7%) | 20 (1.8%) | 0.91 | [0.40–2.08] | 0.83 |
| L3/L4 | 12 (2.5%) | 36 (3.3%) | 0.75 | [0.39–1.45] | 0.39 |
| L4/L5 | 207 (42.9%) | 621 (57.3%) | 0.75 | [0.64–0.88] | <0.001 |
| L5/S1 | 241 (49.9%) | 392 (36.2%) | 1.38 | [1.18–1.61] | <0.001 |
| Symptom | Interlaminar Group (N = 483) | Transforaminal Group (N = 1083) | Risk Ratio (Interlaminar Vs. Transforaminal) | 95% CI | p-value |
| Radiculopathy | 483 (100%) | 1,083 (100%) | 1 | [1.00–1.00] | 1 |
| Motor Weakness | 51 (10.6%) | 93 (8.6%) | 1.23 | [0.88–1.72] | 0.22 |
| Sensory Loss | 341 (70.6%) | 722 (66.7%) | 1.06 | [0.96–1.17] | 0.24 |
| Reflex Loss | 25 (5.2%) | 37 (3.4%) | 1.52 | [0.92–2.51] | 0.1 |
| Variable | BELD (N = 138) | FELD (N = 1428) | 95% CI | p-Value |
|---|---|---|---|---|
| Gender (Male:Female) | 79 M:59 F (57.2% M) | 777 M:651 F (54.4% M) | 0.52 | |
| Age (Years) | 47.1 ± 10.4 | 45.2 ± 12.1 | 0.08 | |
| BMI | 26.9 ± 2.6 (reported in 75% of cases) | 26.7 ± 3.2 (reported in 67% of cases) | 0.45 | |
| Duration of Symptoms | 39.3 ± 44.1 weeks | 84 ± 12.9 days (PTED), 85 ± 10.6 days (PEID) | <0.001 | |
| VAS Leg Pain (Post-Op) | 2.0 ± 1.5 (1 day) | 1.7 ± 1.3 (1 day) | Δ = 0.3 [−0.1–0.7] (1 day) | 0.11 |
| 1.2 ± 0.7 (1 year) | 1.1 ± 0.6 (1 year) | |||
| Complications | Recurrence: 8 (5.8%) | Recurrence: 55 (3.9%) | OR: 1.56 [0.73–3.35] (Recurrence) | 0.25 (Fisher’s) |
| Dural Tear: 3 (2.2%) | Dural Tear: 10 (0.7%) | OR: 3.22 [0.88–11.86] (Recurrence) | 0.08 | |
| Infection: 2 (1.4%) | Infection: 10 (0.7%) | OR: 2.15 [046–9.91] (Recurrence) | 0.33 |
| Level | BELD (N = 138) | FELD (N = 1428) | Risk Ratio (Biportal vs. Other) | 95% CI | p-Value |
|---|---|---|---|---|---|
| L2/L3 | 3 (2.2%) | 25 (1.8%) | 1.24 | [0.37–4.15] | 0.73 |
| L3/L4 | 7 (5.1%) | 41 (2.9%) | 1.76 | [0.79–3.93] | 0.16 |
| L4/L5 | 70 (50.7%) | 784 (54.9%) | 0.92 | [0.72–1.18] | 0.51 |
| L5/S1 | 53 (38.4%) | 583 (40.8%) | 0.94 | [0.71–1.24] | 0.67 |
| Symptom | |||||
| Radiculopathy | 138 (100%) | 1428 (100%) | 1 | [1.00–1.00] | 1 |
| Motor Weakness | 23 (16.7%) | 121 (8.5%) | 1.97 | [1.28–3.03] | 0.002 |
| Sensory Loss | 94 (68.1%) | 969 (67.9%) | 1.01 | [0.86–1.18] | 0.93 |
| Hyporeflexia | 9 (6.5%) | 44 (3.1%) | 2.11 | [1.03–4.31] | 0.04 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Di, L.; Wang, A.; Stillman, K.E.; Tierney, L.K.; Jackson, S.G.; Sasser, A.J.; Valecillo, A.; Cardinal, T.; Tigchelaar, S.; Khalafallah, A.M.; et al. A Systematic Review and Meta-Analysis of Preoperative Characteristics and Postoperative Outcomes in Patients Undergoing Endoscopic Spine Surgery: Part I Endoscopic Microdiscectomy. J. Clin. Med. 2025, 14, 6757. https://doi.org/10.3390/jcm14196757
Di L, Wang A, Stillman KE, Tierney LK, Jackson SG, Sasser AJ, Valecillo A, Cardinal T, Tigchelaar S, Khalafallah AM, et al. A Systematic Review and Meta-Analysis of Preoperative Characteristics and Postoperative Outcomes in Patients Undergoing Endoscopic Spine Surgery: Part I Endoscopic Microdiscectomy. Journal of Clinical Medicine. 2025; 14(19):6757. https://doi.org/10.3390/jcm14196757
Chicago/Turabian StyleDi, Long, Andrew Wang, Kate E. Stillman, Lauren K. Tierney, Solomon G. Jackson, Andrew J. Sasser, Alexander Valecillo, Tyler Cardinal, Seth Tigchelaar, Adham M. Khalafallah, and et al. 2025. "A Systematic Review and Meta-Analysis of Preoperative Characteristics and Postoperative Outcomes in Patients Undergoing Endoscopic Spine Surgery: Part I Endoscopic Microdiscectomy" Journal of Clinical Medicine 14, no. 19: 6757. https://doi.org/10.3390/jcm14196757
APA StyleDi, L., Wang, A., Stillman, K. E., Tierney, L. K., Jackson, S. G., Sasser, A. J., Valecillo, A., Cardinal, T., Tigchelaar, S., Khalafallah, A. M., & Basil, G. (2025). A Systematic Review and Meta-Analysis of Preoperative Characteristics and Postoperative Outcomes in Patients Undergoing Endoscopic Spine Surgery: Part I Endoscopic Microdiscectomy. Journal of Clinical Medicine, 14(19), 6757. https://doi.org/10.3390/jcm14196757






