Quality of Life, Social Networking, and Mental Health: Generational Differentiation and Uniqueness in the Context of South Korea
Abstract
1. Introduction
2. Materials and Methods
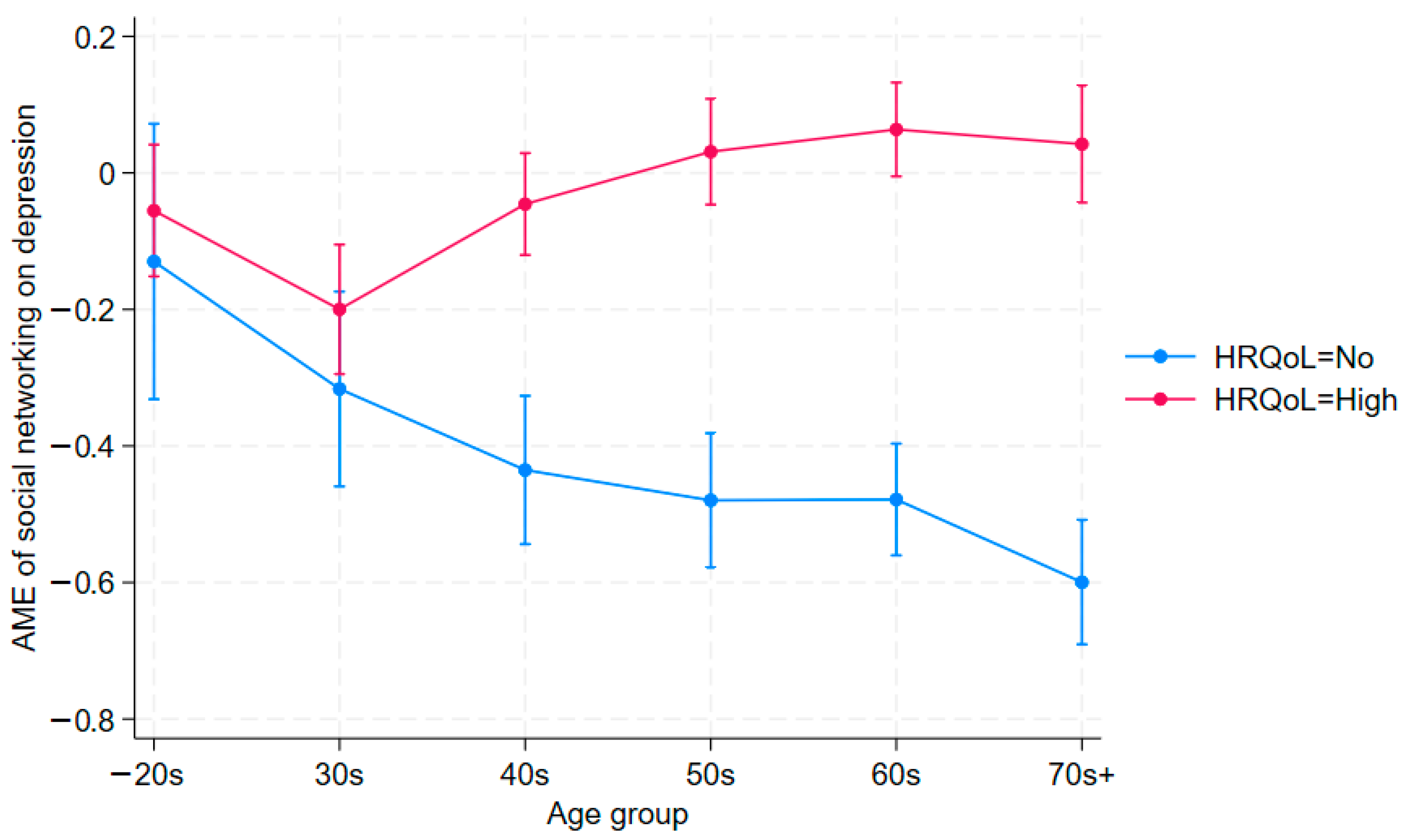
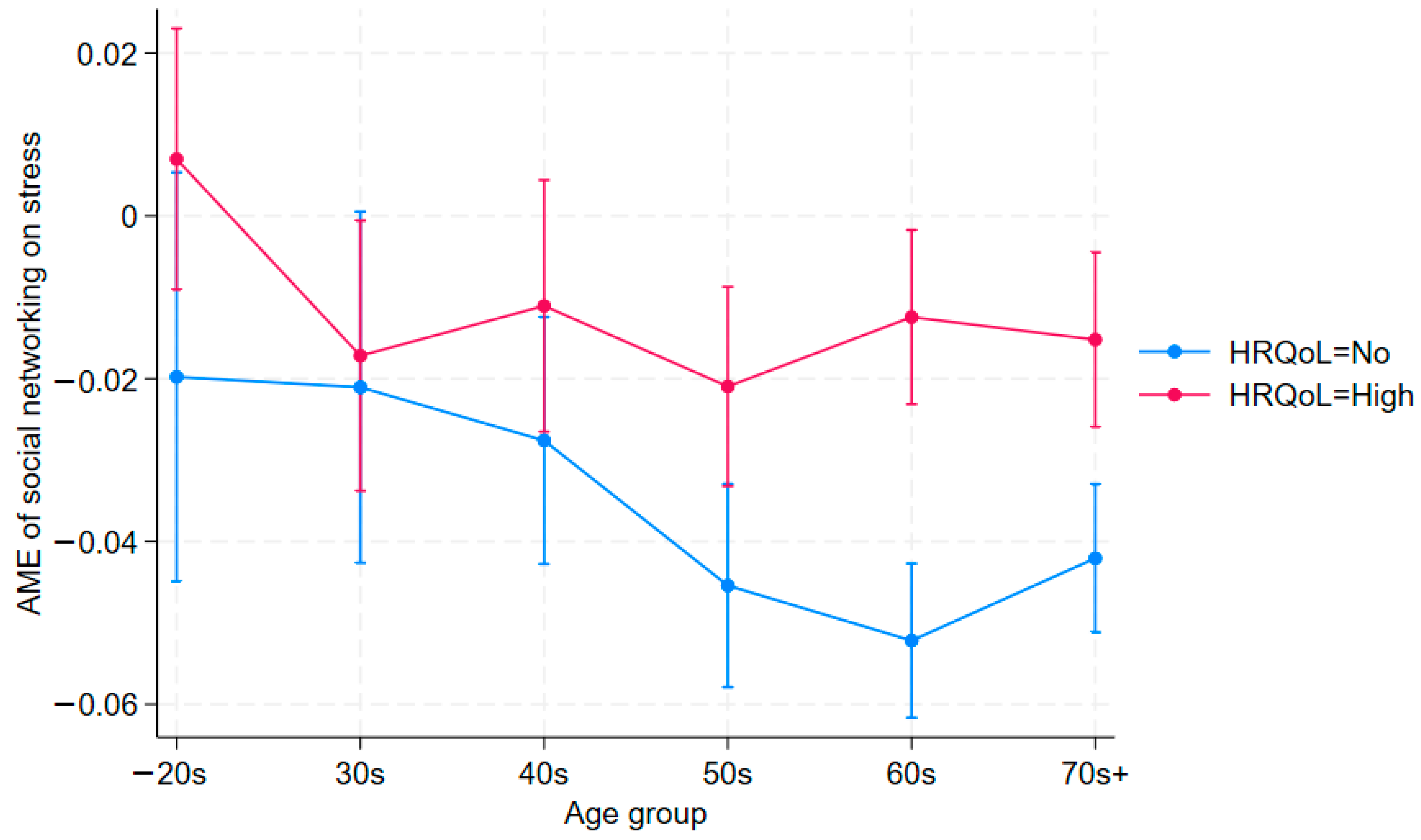
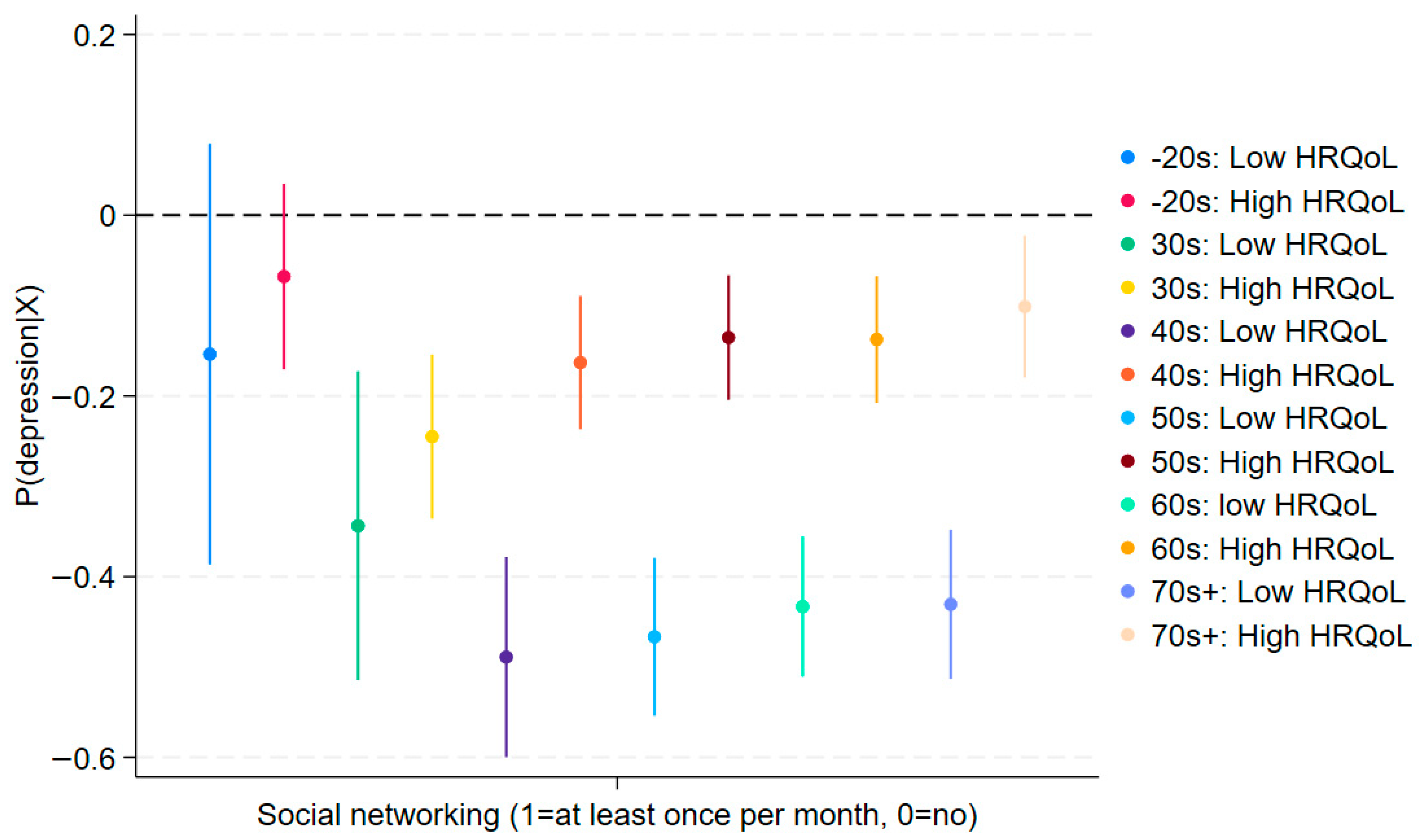
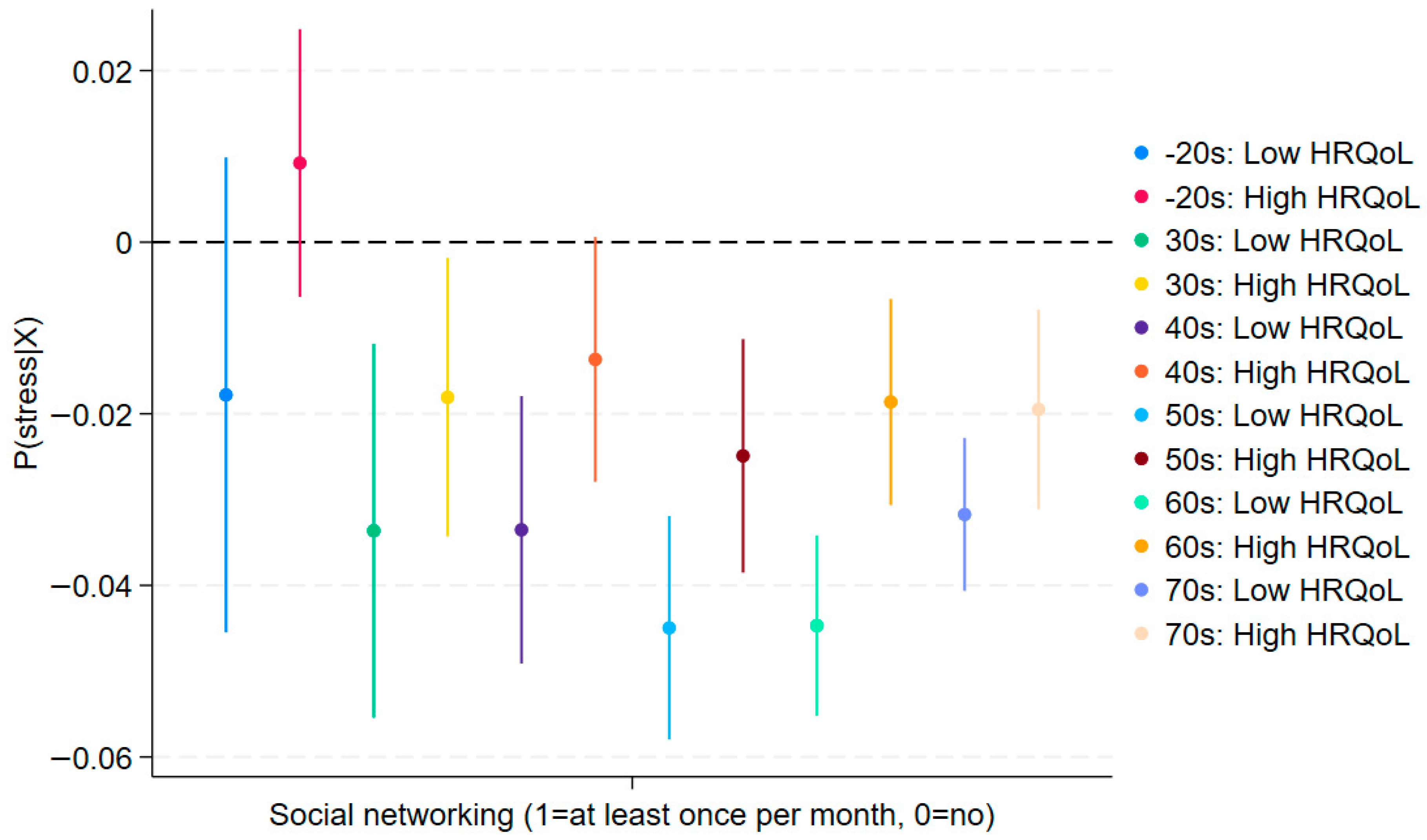
3. Results
Robustness Checks
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- GBD 2019 Mental Disorders Collaborators. Global, regional, and national burden of 12 mental disorders in 204 countries and territories, 1990–2019: A systematic analysis for the Global Burden of Disease Study 2019. Lancet Psychiatry 2022, 9, 137–150. [Google Scholar] [CrossRef]
- Arias, D.; Saxena, S.; Verguet, S. Quantifying the global burden of mental disorders and their economic value. eClinicalMedicine 2022, 54, 101675. [Google Scholar] [CrossRef]
- Herbig, B.; Coe, E.; Enomoto, K. Investing in the Future: How Better Mental Health Benefits Everyone; McKinsey Health Institute: New York, NY, USA, 2025; Available online: https://www.mckinsey.com/mhi/our-insights/investing-in-the-future-how-better-mental-health-benefits-everyone#/ (accessed on 1 August 2025).
- Vollset, S.E.; Ababneh, H.S.; Abate, Y.H.; Abbafati, C.; Abbasgholizadeh, R.; Abbasian, M.; Abbastabar, H.; Abd Al Magied, A.H.A.; Abd ElHafeez, S.; Abdelkader, A.; et al. Burden of disease scenarios for 204 countries and territories, 2022–2050: A forecasting analysis for the Global Burden of Disease Study 2021. Lancet 2024, 403, 2204–2256. [Google Scholar] [CrossRef]
- World Health Organization. COVID-19 Pandemic Triggers 25% Increase in Prevalence of Anxiety and Depression Worldwide. Available online: https://www.who.int/news/item/02-03-2022-covid-19-pandemic-triggers-25-increase-in-prevalence-of-anxiety-and-depression-worldwide (accessed on 1 August 2025).
- Kieling, C.; Buchweitz, C.; Caye, A.; Silvani, J.; Ameis, S.H.; Brunoni, A.R.; Cost, K.T.; Courtney, D.B.; Georgiades, K.; Merikangas, K.R.; et al. Worldwide Prevalence and Disability From Mental Disorders Across Childhood and Adolescence: Evidence From the Global Burden of Disease Study. JAMA Psychiatry 2024, 81, 347. [Google Scholar] [CrossRef]
- Orban, E.; Li, L.Y.; Gilbert, M.; Napp, A.-K.; Kaman, A.; Topf, S.; Boecker, M.; Devine, J.; Reiß, F.; Wendel, F.; et al. Mental health and quality of life in children and adolescents during the COVID-19 pandemic: A systematic review of longitudinal studies. Front. Public Health 2024, 11, 1275917. [Google Scholar] [CrossRef] [PubMed]
- Dumas, S.E.; Dongchung, T.Y.; Sanderson, M.L.; Bartley, K.; Levanon Seligson, A. A comparison of the four healthy days measures (HRQOL-4) with a single measure of self-rated general health in a population-based health survey in New York City. Health Qual Life Outcomes 2020, 18, 315. [Google Scholar] [CrossRef]
- Long, D.; Bonsel, G.J.; Lubetkin, E.I.; Yfantopoulos, J.N.; Janssen, M.F.; Haagsma, J.A. Health-Related Quality of Life and Mental Well-Being during the COVID-19 Pandemic in Five Countries: A One-Year Longitudinal Study. J. Clin. Med. 2022, 11, 6467. [Google Scholar] [CrossRef]
- Ki, Y.; Mcaleavey, A.A.; Øien, J.-M.T.; Moger, T.A.; Moltu, C. Measuring health-related quality of life: A qualitative study of mental health patients’ experiences of impacts of mental health issues. Int. J. Qual. Stud. Health Well-Being 2025, 20, 2465209. [Google Scholar] [CrossRef]
- Farivar, S.S.; Cunningham, W.E.; Hays, R.D. Correlated physical and mental health summary scores for the SF-36 and SF-12 Health Survey, V.1. Health Qual Life Outcomes 2007, 5, 54. [Google Scholar] [CrossRef]
- Gamst-Klaussen, T.; Gudex, C.; Olsen, J.A. Exploring the causal and effect nature of EQ-5D dimensions: An application of confirmatory tetrad analysis and confirmatory factor analysis. Health Qual Life Outcomes 2018, 16, 153. [Google Scholar] [CrossRef]
- Laucis, N.C.; Hays, R.D.; Bhattacharyya, T. Scoring the SF-36 in Orthopaedics: A Brief Guide. J. Bone Jt. Surg. 2015, 97, 1628–1634. [Google Scholar] [CrossRef]
- LoMartire, R.; Äng, B.O.; Gerdle, B.; Vixner, L. Psychometric properties of Short Form-36 Health Survey, EuroQol 5-dimensions, and Hospital Anxiety and Depression Scale in patients with chronic pain. Pain 2020, 161, 83–95. [Google Scholar] [CrossRef]
- Hohls, J.K.; König, H.-H.; Quirke, E.; Hajek, A. Anxiety, Depression and Quality of Life—A Systematic Review of Evidence from Longitudinal Observational Studies. Int. J. Environ. Res. Public Health 2021, 18, 12022. [Google Scholar] [CrossRef]
- Liu, X.; Haagsma, J.; Sijbrands, E.; Buijks, H.; Boogaard, L.; Mackenbach, J.P.; Erasmus, V.; Polinder, S. Anxiety and depression in diabetes care: Longitudinal associations with health-related quality of life. Sci. Rep. 2020, 10, 8307. [Google Scholar] [CrossRef]
- Hajek, A.; Brettschneider, C.; Ernst, A.; Lange, C.; Wiese, B.; Prokein, J.; Weyerer, S.; Werle, J.; Pentzek, M.; Fuchs, A.; et al. Complex coevolution of depression and health-related quality of life in old age. Qual. Life Res. 2015, 24, 2713–2722. [Google Scholar] [CrossRef]
- Rodrigues, A.N.; Paranhos, A.C.M.; Da Silva, L.C.M.; Xavier, S.S.; Silva, C.C.; Da Silva, R.; De Vasconcelos, L.A.; Peixoto, I.V.P.; Panzetti, T.M.N.; Tavares, P.R.; et al. Effect of long COVID-19 syndrome on health-related quality of life: A cross-sectional study. Front. Psychol. 2024, 15, 1394068. [Google Scholar] [CrossRef]
- Alwhaibi, M.; Balkhi, B.; AlRuthia, Y. Anxiety and depression and health-related quality of life among adults with migraine: A National Population-Based Study. Front. Public Health 2023, 11, 1241800. [Google Scholar] [CrossRef]
- Marufi, N.; Malekzadeh, R.; Naderi, F.; Garmabi, M.; Sharifnezhad, A.; Darrudi, F.; Andishmand, Z.; Gholami, A. Association of depression and anxiety with health-related quality of life in beginning Medical Sciences Student. Sci. Rep. 2024, 14, 24515. [Google Scholar] [CrossRef]
- Soong, R.Y.; Low, C.E.; Ong, V.; Sim, I.; Lee, C.; Lee, F.; Chew, L.; Yau, C.E.; Lee, A.R.Y.B.; Chen, M.Z. Exercise Interventions for Depression, Anxiety, and Quality of Life in Older Adults With Cancer: A Systematic Review and Meta-Analysis. JAMA Netw. Open 2025, 8, e2457859. [Google Scholar] [CrossRef]
- Weng, W.H.; Wang, Y.H.; Yeh, N.C.; Yang, Y.R.; Wang, R.Y. Effects of physical training on depression and related quality of life in pre-frail and frail older adults: A systematic review and meta-analysis. J. Nutr. Health Aging 2024, 28, 100237. [Google Scholar] [CrossRef]
- Wu, M.; Li, C.; Hu, T.; Zhao, X.; Qiao, G.; Gao, X.; Zhu, X.; Yang, F. Effectiveness of Telecare Interventions on Depression Symptoms Among Older Adults: Systematic Review and Meta-Analysis. JMIR nHealth uHealth 2024, 12, e50787. [Google Scholar] [CrossRef]
- Fan, Y.; Fan, A.; Yang, Z.; Fan, D. Global burden of mental disorders in 204 countries and territories, 1990–2021: Results from the global burden of disease study 2021. BMC Psychiatry 2025, 25, 486. [Google Scholar] [CrossRef]
- Holt-Lunstad, J. Social Connection as a Public Health Issue: The Evidence and a Systemic Framework for Prioritizing the “Social” in Social Determinants of Health. Annu. Rev. Public Health 2022, 43, 193–213. [Google Scholar] [CrossRef]
- World Health Organization. Social Connection Linked to Improved Health and Reduced Risk of Early Death. 2025. Available online: https://www.who.int/news/item/30-06-2025-social-connection-linked-to-improved-heath-and-reduced-risk-of-early-death (accessed on 1 August 2025).
- Garcia, L.; Hunter, R.; Anderson, N. WHO Commission on Social Connection. In From Loneliness to Social Connection—Charting a Path to Healthier Societies: Report of the WHO Commission on Social Connection; WHO: Geneve, Switzerland, 2025; Available online: https://iris.who.int/bitstream/handle/10665/381746/9789240112360-eng.pdf?sequence=1 (accessed on 1 August 2025).
- Fostering Social Connection for Global Health: The Essential Role of Social Connection in Combating Loneliness, Social Isolation and Inequities in Health. Available online: https://apps.who.int/gb/ebwha/pdf_files/EB156/B156_CONF18-en.pdf (accessed on 18 August 2025).
- Holt-Lunstad, J.; Smith, T.B.; Layton, J.B. Social Relationships and Mortality Risk: A Meta-analytic Review. PLoS Med. 2010, 7, e1000316. [Google Scholar] [CrossRef]
- Holt-Lunstad, J.; Smith, T.B.; Baker, M.; Harris, T.; Stephenson, D. Loneliness and Social Isolation as Risk Factors for Mortality: A Meta-Analytic Review. Perspect. Psychol. Sci. 2015, 10, 227–237. [Google Scholar] [CrossRef]
- Cohen, S.; Wills, T.A. Stress, Social Support, and the Buffering Hypothesis. Psychol. Bull. 1985, 98, 310. [Google Scholar] [CrossRef]
- Kawachi, I. Social Ties and Mental Health. J. Urban Health Bull. N. Y. Acad. Med. 2001, 78, 458–467. [Google Scholar] [CrossRef]
- Ow, Y.S.Y.; Wei, C.-S.; Li, Y.-T. Moderating effect of social participation on the relationship between health status and depressive symptoms in older adults. Front. Public Health 2025, 13, 1458961. [Google Scholar] [CrossRef]
- Krause, N. Exploring age differences in the stress-buffering function of social support. Psychol. Aging 2005, 20, 714–717. [Google Scholar] [CrossRef]
- Turner, S.T.; Carmel, S.; O’Rourke, N.; Raveis, V.H.; Tovel, H.; Cohn-Schwartz, E. Social Support and Symptoms of Depression in Late Life: Bidirectional Associations over Time. Int. J. Environ. Res. Public Health 2022, 19, 16065. [Google Scholar] [CrossRef]
- National Academies of Sciences, Engineering, and Medicine. Social Isolation and Loneliness in Older Adults: Opportunities for the Health Care System; National Academies Press: Washington, DC, USA, 2020. [Google Scholar]
- Charles, S.T. Strength and Vulnerability Integration: A Model of Emotional Well-Being Across Adulthood. Psychol. Bull. 2010, 136, 1068–1091. [Google Scholar] [CrossRef]
- Luhmann, M.; Hawkley, L.C. Age differences in loneliness from late adolescence to oldest old age. Dev. Psychol. 2016, 52, 943–959. [Google Scholar] [CrossRef]
- Holt-Lunstad, J. Social connection as a critical factor for mental and physical health: Evidence, trends, challenges, and future implications. World Psychiatry 2024, 23, 312–332. [Google Scholar] [CrossRef]
- Steen, O.D.; Ori, A.P.S.; Wardenaar, K.J.; Van Loo, H.M. Loneliness associates strongly with anxiety and depression during the COVID pandemic, especially in men and younger adults. Sci. Rep. 2022, 12, 9517. [Google Scholar] [CrossRef]
- Korea Disease Control and Prevention Agency. Community Health Survey Raw Data Usage Guidelines 2023. Available online: https://chs.kdca.go.kr/chs/mnl/mnlBoardMain.do (accessed on 18 August 2025).
- Manea, L.; Gilbody, S.; McMillan, D. A diagnostic meta-analysis of the Patient Health Questionnaire-9 (PHQ-9) algorithm scoring method as a screen for depression. Gen. Hosp. Psychiatry 2015, 37, 67–75. [Google Scholar] [CrossRef]
- Kroenke, K.; Spitzer, R.; Williams, J. The PHQ-9: Validity of a brief depression severity measure. J. Gen. Intern. Med. 2001, 16, 606–613. [Google Scholar] [CrossRef]
- Rotnitzky, A.; Robins, J. Inverse probability weighted estimation in survival analysis. Encycl. Biostat. 2005, 4, 2619–2625. [Google Scholar]
- Park, J. Why Unification Perception of the Younger Generation in Their 20s and 30s Is Different from the Older Generation? Korea Institute for National Unification: Seoul, Republic of Korea, 2018. [Google Scholar]
- Kim, U.; Kim, J. Economic Development, Sociocultural Change and Quality of Life in Korea: Analysis of Three Generations Growing up in Colonial, Industrial and Digital Age. Psychol. Dev. Soc. 2022, 34, 200–239. [Google Scholar] [CrossRef]
- Festinger, L. A theory of social comparison processes. Hum. Relat. 1954, 7, 117–140. [Google Scholar] [CrossRef]
- Jang, J. Why the Number of South Korean ‘Hikikomori’ Is Rising…” Foreign Media Are ‘Shocked’. 27 May 2024. Available online: https://www.hankyung.com/article/2024052764877 (accessed on 15 August 2025).
- Tan, K.W.K. Seoul’s $322 Million Gambit to Save the City from Crushing Loneliness Won’t Fix the Source of Its Problems. Business Insider. 2024. Available online: https://www.businessinsider.com/experts-say-seoul-322-million-plan-fight-loneliness-not-work-2024-11?utm_source=chatgpt.com (accessed on 15 August 2025).
- Anspach, N.M.; Carlson, T.N. What to Believe? Social Media Commentary and Belief in Misinformation. Polit. Behav. 2020, 42, 697–718. [Google Scholar] [CrossRef]
- Samra, A.; Warburton, W.A.; Collins, A.M. Social comparisons: A potential mechanism linking problematic social media use with depression. J. Behav. Addict. 2022, 11, 607–614. [Google Scholar] [CrossRef]
- Kim, S.; Jang, Y.S.; Park, E.-C. Associations between social isolation, withdrawal, and depressive symptoms in young adults: A cross-sectional study. BMC Psychiatry 2025, 25, 327. [Google Scholar] [CrossRef] [PubMed]
- Park, S.M.; Joo, M.J.; Lim, J.H.; Jang, S.-Y.; Park, E.-C.; Ha, M.J. Association between hikikomori (social withdrawal) and depression in Korean young adults. J. Affect. Disord. 2025, 380, 647–654. [Google Scholar] [CrossRef] [PubMed]
- Lee, S.Y.; Hong, J.S.; Espelage, D.L. An ecological understanding of youth suicide in South Korea. Sch. Psychol. Int. 2010, 31, 531–546. [Google Scholar] [CrossRef]
- Zhao, S.; Yan, W.; Tao, L.; Zhang, J. The Association Between Relative Deprivation, Depression, and Youth Suicide: Evidence From a Psychological Autopsy Study. OMEGA 2024, 89, 1691–1713. [Google Scholar] [CrossRef]
- Lee, E. Comparative Study of Mental Health Care Availability and Stigma in the United States and South Korea. Research Archive of Rising Scholars. Available online: https://research-archive.org/index.php/rars/preprint/view/2831/3961 (accessed on 18 August 2025).
| (1) | (2) | (3) | (4) | (5) | |
|---|---|---|---|---|---|
| Variables | N | Mean | S.D. | Min. | Max. |
| Dependent Variables | |||||
| Depressed (PHQ-9) | 203,320 | 2.298 | 3.194 | 0 | 27 |
| Stressed (1 = high, 0 = low) | 203,320 | 0.224 | 0.417 | 0 | 1 |
| Key Independent Variables of Interest | |||||
| Health-related quality of life (1 = high, 0 = no) | 203,320 | 0.385 | 0.487 | 0 | 1 |
| Participate in social networking activities at least once per month (1 = at least once per month, 0 = no) | 203,320 | 0.496 | 0.500 | 0 | 1 |
| Covariates | |||||
| Age | 203,320 | 55.99 | 17.449 | 19 | 106 |
| Sex (1 = man, 0 = woman) | 203,320 | 0.456 | 0.498 | 0 | 1 |
| Neighborhood type code (1 = Dong, 2 = Eup/Myeon) | 203,320 | 1.425 | 0.494 | 1 | 2 |
| Housing type code (1 = Non-APT, 2 = APT) | 203,320 | 1.459 | 0.498 | 1 | 2 |
| Diverse family or not (1 = yes, 0 = no) | 203,320 | 0.0139 | 0.117 | 0 | 1 |
| Use a safety belt? (1 = don’t drive, 2 = not at all, 3 = rarely, 4 = sometimes, 5 = often, 6 = always) | 203,320 | 3.908 | 2.399 | 1 | 6 |
| High-intensity physical activity in the last week (days) | 203,320 | 0.801 | 1.677 | 0 | 7 |
| Moderate-intensity physical activity in the last week (days) | 203,320 | 1.382 | 2.166 | 0 | 7 |
| Walked more than 10 min a week (days) | 203,320 | 4.263 | 2.613 | 0 | 7 |
| How often did you have your breakfast for the past 1 year (in a week)? (1 = 5–7 days, 2 = 3–4 days, 3 = 1–2 days, 4 = 0 day) | 203,320 | 1.809 | 1.226 | 1 | 4 |
| Height (cm) | 202,689 | 163.9 | 9.017 | 50 | 200 |
| Weight (kg) | 203,245 | 63.93 | 12.52 | 20 | 163 |
| Received influenza vaccine (1 = yes, 0 = no) | 203,320 | 0.597 | 0.490 | 0 | 1 |
| Had high blood pressure (1 = yes, 0 = no)? | 203,320 | 0.311 | 0.463 | 0 | 1 |
| Had diabetes (1 = yes, 0 = no)? | 203,320 | 0.136 | 0.343 | 0 | 1 |
| Havent’ received medical service when needed in the past year (1 = yes, 2 = no, 3 = didn’t need it)? | 203,320 | 2.027 | 0.360 | 1 | 3 |
| Had accident or addicted in the last year (1 = yes, 0 = no)? | 203,320 | 0.0605 | 0.238 | 0 | 1 |
| Trust your neighbor (1 = yes, 0 = no)? | 203,320 | 0.709 | 0.454 | 0 | 1 |
| Neighbors help each other for events (1 = yes, 0 = no)? | 203,320 | 0.485 | 0.500 | 0 | 1 |
| Safe neighborhood (1 = yes, 0 = no)? | 203,320 | 0.867 | 0.340 | 0 | 1 |
| Good natural environment of the neighborhood (1 = yes, 0 = no)? | 203,320 | 0.834 | 0.372 | 0 | 1 |
| Neighborhood equipped with good living conditions (1 = yes, 0 = no)? | 203,320 | 0.857 | 0.350 | 0 | 1 |
| Good access to public transportation (1 = yes, 0 = no)? | 203,320 | 0.706 | 0.456 | 0 | 1 |
| Satisfactory medical service conditions in the neighborhood (1 = yes, 0 = no)? | 203,320 | 0.738 | 0.440 | 0 | 1 |
| How often do you contact your closest family or relative (1 = frequently, 0 = not so much)? | 203,320 | 0.591 | 0.492 | 0 | 1 |
| How often do you contact your closest neighbor (1 = frequently, 0 = not so much)? | 203,320 | 0.505 | 0.500 | 0 | 1 |
| How often do you contact your closest friend (1 = frequently, 0 = not so much)? | 203,320 | 0.520 | 0.500 | 0 | 1 |
| Occupation status (1 = employer, 2 = salaried, 3 = working with no salary, 8 = unemployed) | 203,310 | 4.019 | 3.021 | 1 | 8 |
| Basic livelihood security beneficiary or not (1 = yes, 0 = no) | 203,320 | 0.049 | 0.215 | 0 | 1 |
| Ever smoked (1 = yes, 0 = no)? | 203,320 | 0.387 | 0.487 | 0 | 1 |
| Indirectly smoked (1 = yes, 0 = no)? | 203,320 | 0.003 | 0.053 | 0 | 1 |
| Ever drank alcohol (1 = yes, 0 = no)? | 203,318 | 0.834 | 0.373 | 0 | 1 |
| Was on a diet (1 = yes, 0 = no)? | 203,319 | 0.642 | 0.479 | 0 | 1 |
| Good teeth condition (1 = yes, 0 = no)? | 203,320 | 0.259 | 0.438 | 0 | 1 |
| Ever gambled (1 = yes, 0 = no)? | 203,320 | 0.280 | 0.449 | 0 | 1 |
| Had a health check-up in the past 2 years? (Cronbach’s alpha = 0.77) | 203,320 | 0.697 | 0.409 | 0 | 1 |
| Had a stroke (1 = yes, 0 = no) (Cronbach’s alpha = 0.84)? | 203,320 | 0.812 | 0.302 | 0 | 1 |
| Had early signs of heart attack (1 = yes, 0 = no) (Cronbach’s alpha = 0.79)? | 203,320 | 0.738 | 0.337 | 0 | 1 |
| Had higher education (1 = yes, 0 = no)? | 203,284 | 0.403 | 0.490 | 0 | 1 |
| Married (1 = yes, 0 = no) | 203,306 | 0.666 | 0.472 | 0 | 1 |
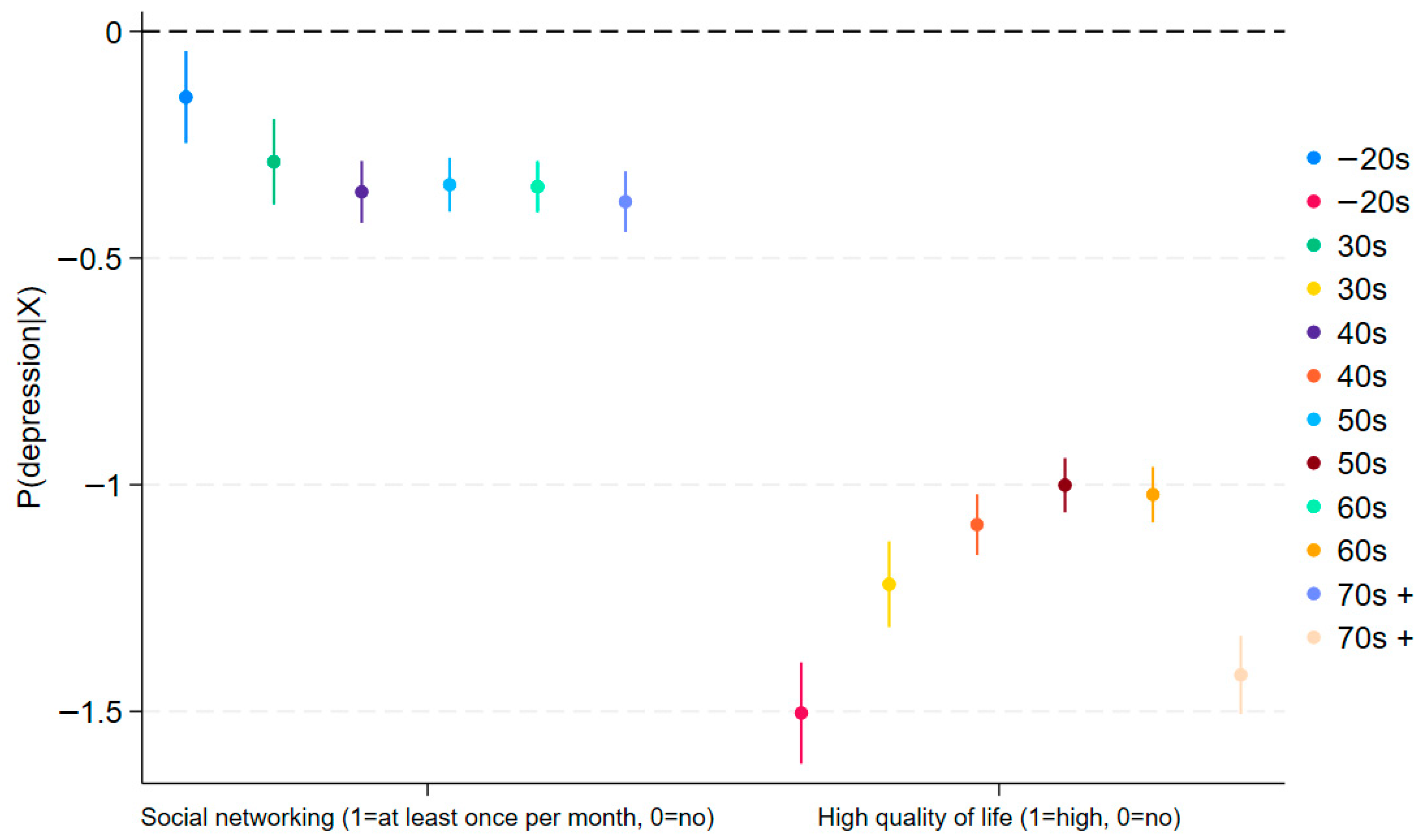
| (1) Depressed (PHQ-9) | (2) Depressed (PHQ-9) | (3) Depressed (PHQ-9) | (4) Depressed (PHQ-9) | (5) Depressed (PHQ-9) | (6) Depressed (PHQ-9) | |
|---|---|---|---|---|---|---|
| Variables | ||||||
| Good HRQoL (1 = good, 0 = else) | −1.482 *** | −1.208 *** | −1.199 *** | −1.206 *** | −1.238 *** | −1.474 *** |
| (0.062) | (0.051) | (0.051) | (0.055) | (0.046) | (0.047) | |
| Social networking activity (1 = at least once per month, 0 = no) | −0.185 | −0.317 *** | −0.471 *** | −0.507 *** | −0.502 *** | −0.424 *** |
| (0.101) | (0.071) | (0.053) | (0.048) | (0.040) | (0.047) | |
| Good HRQoL X social networking activity | 0.072 | 0.125 | 0.388 *** | 0.472 *** | 0.533 *** | 0.638 *** |
| (0.104) | (0.076) | (0.064) | (0.064) | (0.052) | (0.058) | |
| Constant | 6.733 *** | 7.962 *** | 6.213 *** | 5.531 *** | 5.086 *** | 7.676 *** |
| (0.678) | (0.705) | (0.550) | (0.457) | (0.444) | (0.552) | |
| Observations | 18,874 | 21,454 | 30,073 | 37,770 | 45,756 | 48,627 |
| R-squared | 0.208 | 0.186 | 0.177 | 0.191 | 0.191 | 0.202 |
| Control variables | Yes | Yes | Yes | Yes | Yes | Yes |
| District FE | Yes | Yes | Yes | Yes | Yes | Yes |
| Age | >20s | 30s | 40s | 50s | 60s | 70s + |
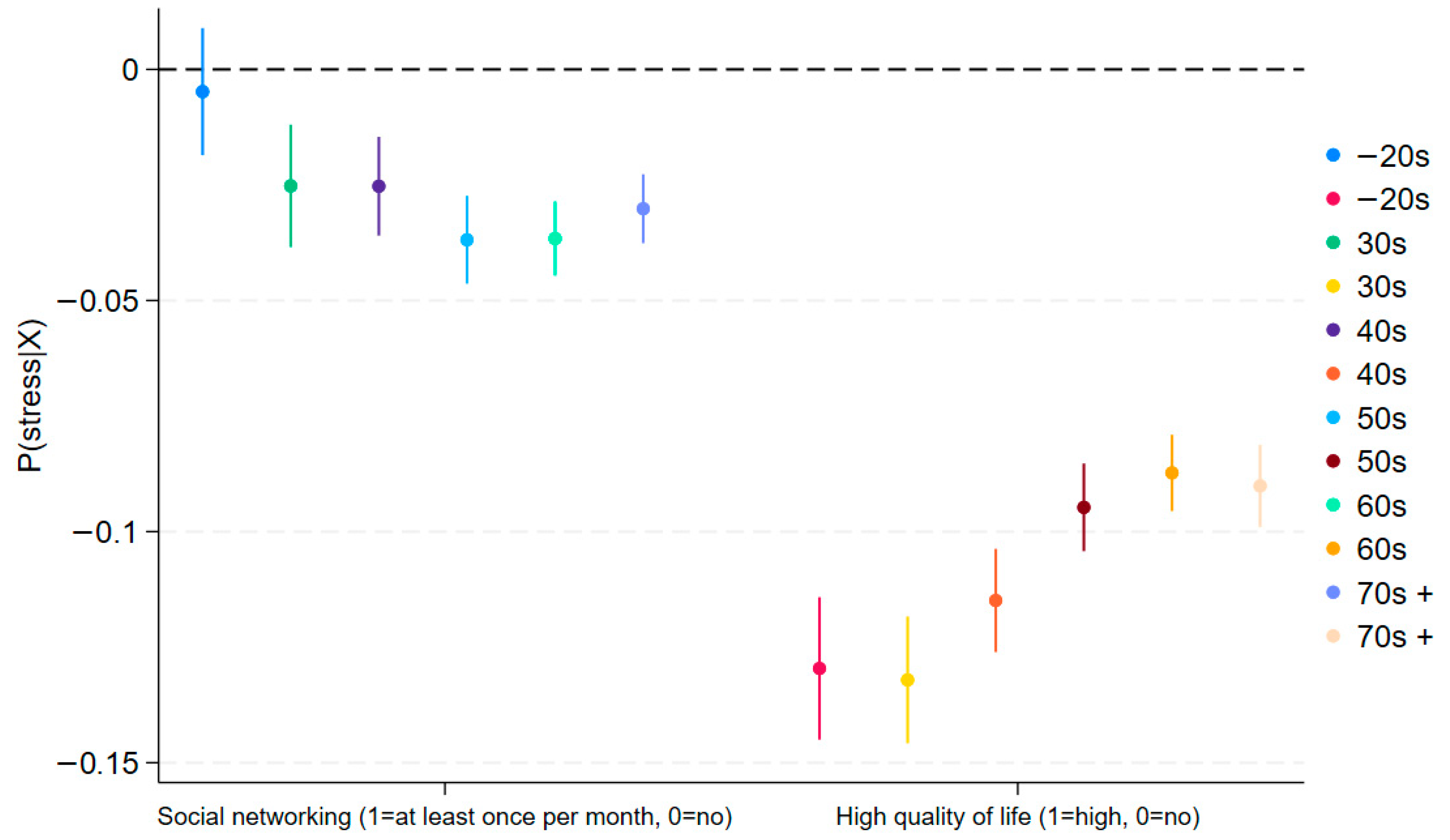
| (1) Stressed (1 = High, 0 = Low)? | (2) Stressed (1 = High, 0 = Low)? | (3) Stressed (1 = high, 0 = Low)? | (4) Stressed (1 = High, 0 = Low)? | (5) Stressed (1 = High, 0 = Low)? | (6) Stressed (1 = High, 0 = Low)? | |
|---|---|---|---|---|---|---|
| Variables | ||||||
| Good HRQoL (1 = good, 0 = else) | −0.138 *** | −0.132 *** | −0.120 *** | −0.106 *** | −0.109 *** | −0.090 *** |
| (0.008) | (0.008) | (0.008) | (0.007) | (0.006) | (0.006) | |
| Social networking activity (once per month; 1 = at least once per month, 0 = no) | −0.017 | −0.026 * | −0.030 *** | −0.045 *** | −0.052 *** | −0.034 *** |
| (0.013) | (0.011) | (0.008) | (0.007) | (0.005) | (0.005) | |
| Good HRQoL X social networking activity | 0.022 | 0.003 | 0.014 | 0.023 ** | 0.040 *** | 0.029 *** |
| (0.014) | (0.013) | (0.011) | (0.008) | (0.007) | (0.007) | |
| Constant | 0.761 *** | 0.594 *** | 0.480 *** | 0.556 *** | 0.409 *** | 0.422 *** |
| (0.095) | (0.101) | (0.087) | (0.069) | (0.050) | (0.050) | |
| Observations | 18,874 | 21,454 | 30,073 | 37,770 | 45,756 | 48,627 |
| R-squared | 0.099 | 0.082 | 0.076 | 0.070 | 0.071 | 0.072 |
| Control variables | Yes | Yes | Yes | Yes | Yes | Yes |
| District FE | Yes | Yes | Yes | Yes | Yes | Yes |
| Age | >20s | 30s | 40s | 50s | 60s | 70s + |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Shin, G.; Chae, J.; Rhee, Y.-C.; Lym, Y. Quality of Life, Social Networking, and Mental Health: Generational Differentiation and Uniqueness in the Context of South Korea. J. Clin. Med. 2025, 14, 6739. https://doi.org/10.3390/jcm14196739
Shin G, Chae J, Rhee Y-C, Lym Y. Quality of Life, Social Networking, and Mental Health: Generational Differentiation and Uniqueness in the Context of South Korea. Journal of Clinical Medicine. 2025; 14(19):6739. https://doi.org/10.3390/jcm14196739
Chicago/Turabian StyleShin, Geiguen, Jimin Chae, Yong-Chan Rhee, and Youngbin Lym. 2025. "Quality of Life, Social Networking, and Mental Health: Generational Differentiation and Uniqueness in the Context of South Korea" Journal of Clinical Medicine 14, no. 19: 6739. https://doi.org/10.3390/jcm14196739
APA StyleShin, G., Chae, J., Rhee, Y.-C., & Lym, Y. (2025). Quality of Life, Social Networking, and Mental Health: Generational Differentiation and Uniqueness in the Context of South Korea. Journal of Clinical Medicine, 14(19), 6739. https://doi.org/10.3390/jcm14196739






