Preoperative Opioid Use Disorder Predicts Prolonged Ventilation, Central Line Placement, and Major Anesthesiology Complications After ACDF Surgery: A Big Data Analysis of 180,000 Cases
Abstract
1. Introduction
Research Questions
2. Methods
2.1. Data Source, Data Access, and Processing
2.2. Patient Selection and Procedure Code Identification
2.3. Opioid Use Disorder Classification
2.4. Baseline Variables and Comorbidities
2.5. Cost-Effectiveness Analysis
2.6. Ethical Considerations
3. Results
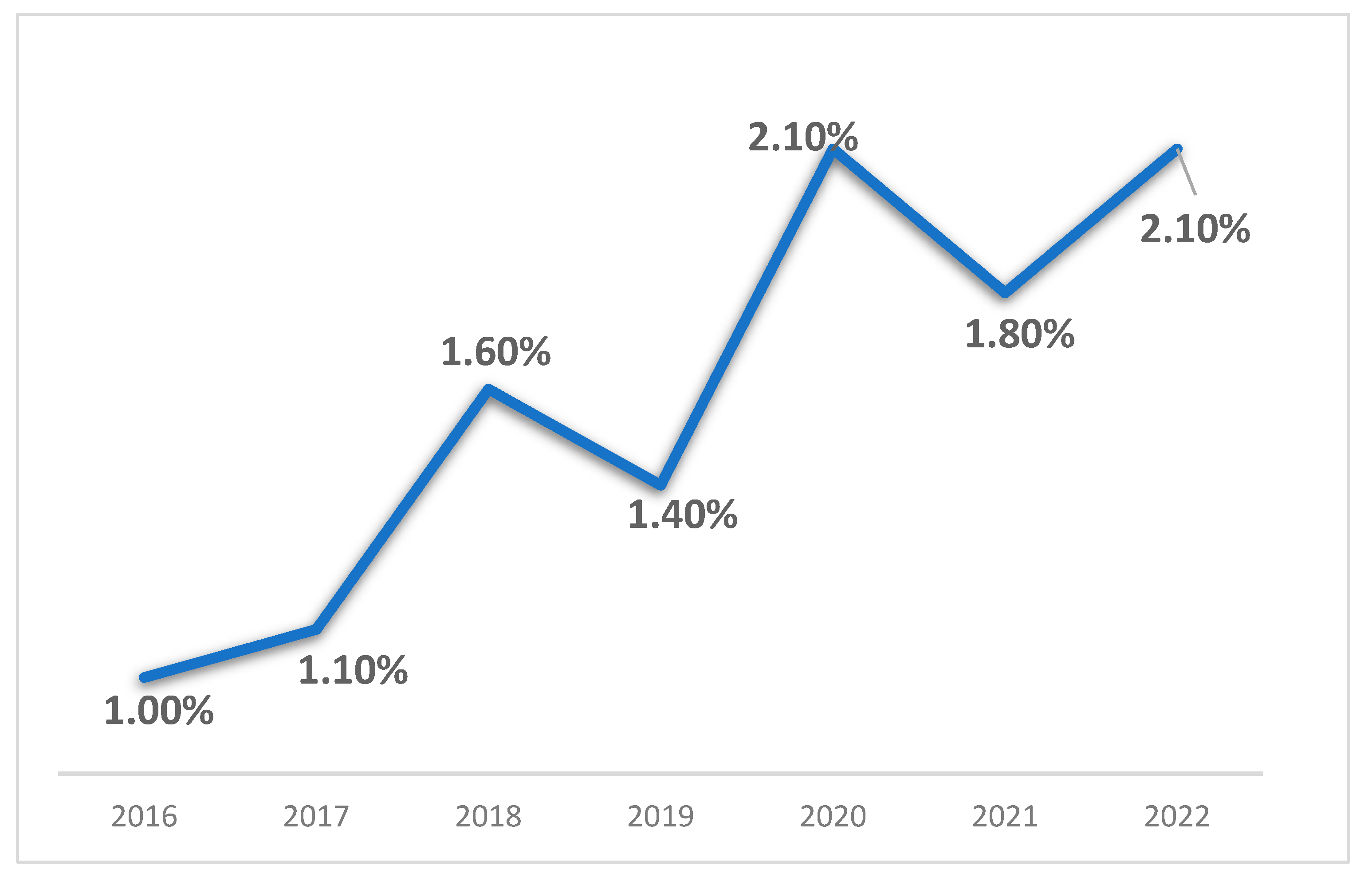
3.1. Trends in Opioid Use Disorder Among ACDF Patients
3.2. Baseline Characteristics of ACDF Patients with and Without OUD
3.3. Perioperative Resource Utilization Among ACDF Patients with and Without Opioid Use Disorder
3.4. Propensity Score-Matched Comparison of ACDF Patients with and Without Opioid Use Disorder
3.5. Impact of Opioid Use Disorder on Perioperative Resource Utilization After Propensity Score Matching
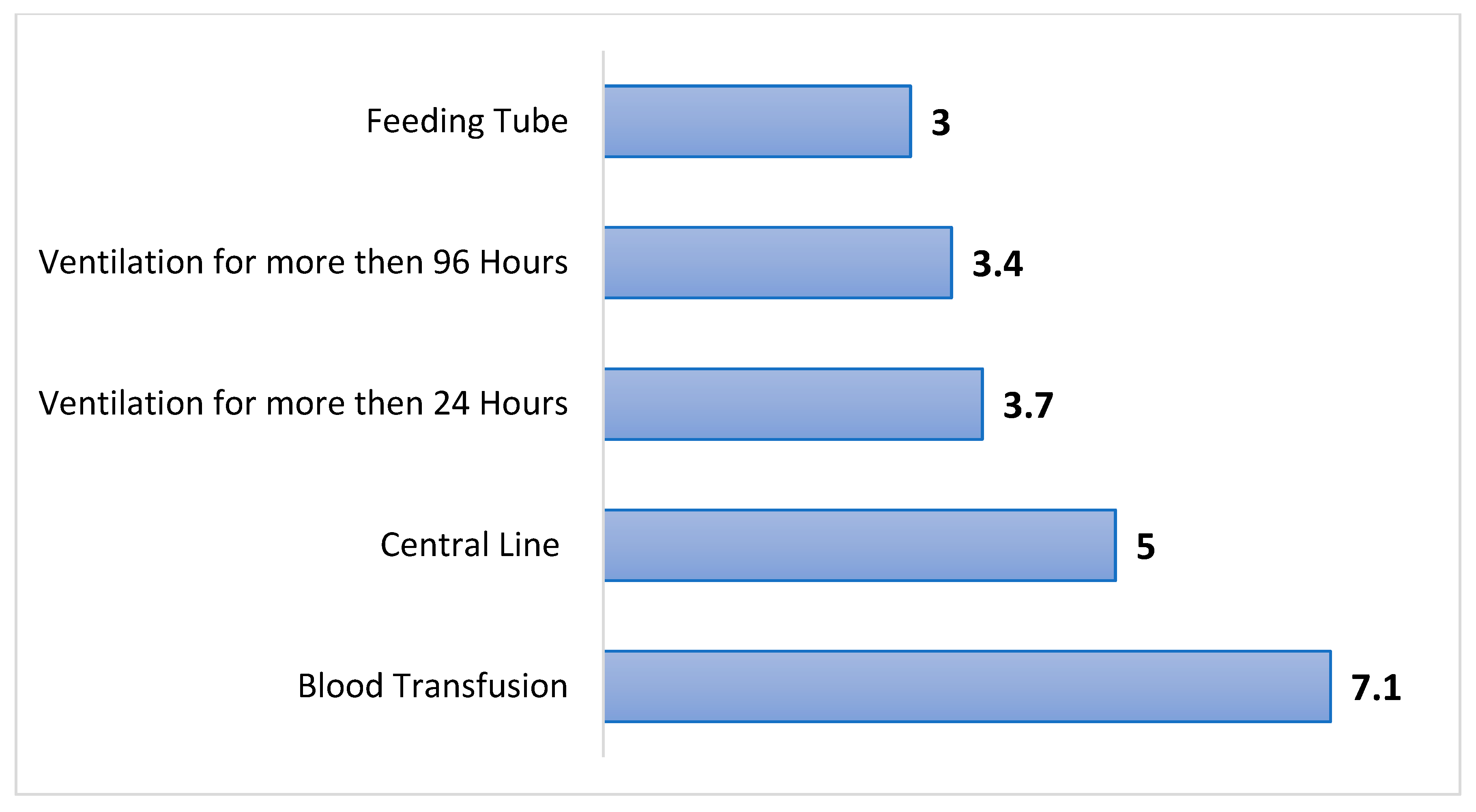
3.6. Risk of Anesthesia and Intensive Care-Related Interventions After Propensity Score Matching
3.7. Postoperative Complication Risk in Propensity Score-Matched ACDF Patients with Opioid Use Disorder
3.8. Economic Justification for Routine Preoperative Opioid Screening in ACDF Patients
4. Discussion
4.1. Key Observations
4.2. How This Compares to Earlier Studies
4.3. Underlying Risk Factors
4.4. Practical Considerations for Clinical Teams
4.5. Financial Impact and Health System Implications
4.6. Strengths and Study Constraints
4.7. Areas for Further Study
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| ACDF | Anterior Cervical Discectomy and Fusion |
| AKI | Acute Kidney Injury |
| CI | Confidence Interval |
| CKD | Chronic Kidney Disease |
| CMS | Centers for Medicare & Medicaid Services |
| DM | Diabetes Mellitus |
| HCUP | Healthcare Cost and Utilization Project |
| HMO | Health Maintenance Organization |
| HTN | Hypertension |
| IBD | Inflammatory Bowel Disease |
| ICD-10-CM | International Classification of Diseases, Tenth Revision, Clinical Modification |
| ICD-10-PCS | International Classification of Diseases, Tenth Revision, Procedure Coding System |
| ICU | Intensive Care Unit |
| IRB | Institutional Review Board |
| LOS | Length of Stay |
| NIS | Nationwide Inpatient Sample |
| OUD | Opioid Use Disorder |
| OSA | Obstructive Sleep Apnea |
| PE | Pulmonary Embolism |
| PSM | Propensity Score Matching |
| RR | Relative Risk |
| Std. deviation | Standard Deviation |
| UTI | Urinary Tract Infection |
References
- Blevins Peratikos, M.; Weeks, H.L.; Pisansky, A.J.B.; Yong, R.J.; Stringer, E.A. Effect of Preoperative Opioid Use on Adverse Outcomes, Medical Spending, and Persistent Opioid Use Following Elective Total Joint Arthroplasty in the United States: A Large Retrospective Cohort Study of Administrative Claims Data. Pain Med. 2020, 21, 521–531. [Google Scholar] [CrossRef] [PubMed]
- Dowell, D.; Ragan, K.R.; Jones, C.M.; Baldwin, G.T.; Chou, R. CDC Clinical Practice Guideline for Prescribing Opioids for Pain—United States, 2022. MMWR Recomm. Rep. 2022, 71, 1–95. [Google Scholar] [CrossRef] [PubMed]
- Hilliard, P.E.; Waljee, J.; Moser, S.; Metz, L.; Mathis, M.; Goesling, J.; Cron, D.; Clauw, D.J.; Englesbe, M.; Howard, R. Prevalence of Preoperative Opioid Use and Characteristics Associated with Opioid Use Among Patients Presenting for Surgery. JAMA Surg. 2018, 153, 929–937. [Google Scholar] [CrossRef] [PubMed]
- Tran, Z.; Madrigal, J.; Pan, C.; Rahimtoola, R.; Verma, A.; Gandjian, M.; Tillou, A.; Benharash, P. Impact of Opioid Use Disorder on Resource Utilization and Readmissions after Operative Trauma. Surgery 2022, 171, 541–548. [Google Scholar] [CrossRef] [PubMed]
- Burgess, J.R.; Heneghan, K.C.; Barot, T.G.; Hwang, C.J.; Gani, F.; Sedrakyan, A.; Morris, M.S. Surgeons’ Knowledge Regarding Perioperative Pain Management in Patients with Opioid Use Disorder: A Survey among 260 Members of the American College of Surgeons. Patient Saf. Surg. 2024, 18, 9. [Google Scholar] [CrossRef] [PubMed]
- Nadarajah, V.; Meredith, S.J.; Jauregui, J.J.; Smuda, M.P.; Medina, S.; Gilotra, M.N.; Hasan, S.A.; Henn, R.F. Preoperative Opioid Use in Patients Undergoing Shoulder Surgery. Shoulder Elb. 2021, 13, 248–259. [Google Scholar] [CrossRef] [PubMed]
- Harris, A.B.; Marrache, M.; Jami, M.; Raad, M.; Puvanesarajah, V.; Hassanzadeh, H.; Lee, S.H.; Skolasky, R.; Bicket, M.; Jain, A. Chronic Opioid Use Following Anterior Cervical Discectomy and Fusion Surgery for Degenerative Cervical Pathology. Spine J. 2020, 20, 78–86. [Google Scholar] [CrossRef] [PubMed]
- Berardino, K.; Carroll, A.H.; Kaneb, A.; Civilette, M.D.; Sherman, W.F.; Kaye, A.D. An Update on Postoperative Opioid Use and Alternative Pain Control Following Spine Surgery. Orthop. Rev. 2021, 13, 24978. [Google Scholar] [CrossRef] [PubMed]
- Kim, N.S.; Lam, A.W.; Golub, I.J.; Sheth, B.K.; Vakharia, R.M.; Saleh, A.; Razi, A.E. Opioid Use Disorder in Patients Undergoing Primary 1- to 2-Level Anterior Cervical Discectomy and Fusion Is Associated with Longer In-Hospital Lengths of Stay and Higher Rates of Readmissions, Complications, and Costs of Care. Glob. Spine J. 2023, 13, 1467–1473. [Google Scholar] [CrossRef] [PubMed]
- Boltunova, A.; Bailey, C.; Weinberg, R.; Ma, X.; Thalappillil, R.; Tam, C.W.; White, R.S. Preoperative Opioid Use Disorder Is Associated with Poorer Outcomes after Coronary Bypass and Valve Surgery: A Multistate Analysis, 2007–2014. J. Cardiothorac. Vasc. Anesth. 2020, 34, 3267–3274. [Google Scholar] [CrossRef] [PubMed]
- Madrigal, J.; Sanaiha, Y.; Hadaya, J.; Dhawan, P.; Benharash, P. Impact of Opioid Use Disorders on Outcomes and Readmission Following Cardiac Operations. Heart 2021, 107, 909–915. [Google Scholar] [CrossRef] [PubMed]
- Szabo, A.; Szabo, D.; Toth, K.; Szecsi, B.; Sandor, A.; Szentgroti, R.; Parkanyi, B.; Merkely, B.; Gal, J.; Szekely, A. Effect of Preoperative Chronic Opioid Use on Mortality and Morbidity in Vascular Surgical Patients. Cureus 2021, 13, e20484. [Google Scholar] [CrossRef] [PubMed]
- Menendez, M.E.; Ring, D.; Bateman, B.T. Preoperative Opioid Misuse Is Associated with Increased Complications After Elective Orthopaedic Surgery. Clin. Orthop. Relat. Res. 2015, 473, 2402–2412. [Google Scholar] [CrossRef] [PubMed]
- Mahamid, A.; Laver, L.; Alfandari, L.; Jabareen, H.; Martonovich, N.; Keren, A.; Behrbalk, E. Opioid Dependence Increases Complications and Costs Following Lumbar Spinal Fusion: Insights from a Nationwide Database. J. Clin. Med. 2025, 14, 3929. [Google Scholar] [CrossRef] [PubMed]
- Palkovic, B.; Marchenko, V.; Zuperku, E.J.; Stuth, E.A.E.; Stucke, A.G. Multi-Level Regulation of Opioid-Induced Respiratory Depression. Physiology 2020, 35, 391–404. [Google Scholar] [CrossRef] [PubMed]
- Bettinger, J.J.; Friedman, B.C. Opioids and Immunosuppression: Clinical Evidence, Mechanisms of Action, and Potential Therapies. Palliat. Med. Rep. 2024, 5, 70–80. [Google Scholar] [CrossRef] [PubMed]
- Burns, S.L.; Majdak, P.; Urman, R.D. Perioperative and Periprocedural Anesthetic Management of Opioid Tolerant Patients and Patients with Active and Medically Treated Opioid Use Disorder. Curr. Opin. Anaesthesiol. 2022, 35, 514–520. [Google Scholar] [CrossRef] [PubMed]
- Qeadan, F.; Nicolson, A.; Tingey, B.; Moffett, M.L.; Azagba, S. Healthcare Utilization Trends among Patients with Opioid Use Disorder in U.S. Hospitals: An Analysis of Length of Stay, Total Charges, and Costs, 2005–2020. BMC Health Serv. Res. 2025, 25, 927. [Google Scholar] [CrossRef] [PubMed]
- Cohen Nissan, E.; Berkovich, Y.; Maman, D.; Yonai, Y.; Steinfeld, Y.; Berkovich, Y. Opioid Use Disorder Significantly Increases Complications and Costs in Primary and Revision Total Knee Arthroplasty: A Nationwide Analysis and the Case for Preoperative Screening. J. Clin. Med. 2025, 14, 3832. [Google Scholar] [CrossRef] [PubMed]
- Black, N. Patient Reported Outcome Measures Could Help Transform Healthcare. BMJ 2013, 346, f167. [Google Scholar] [CrossRef] [PubMed]


| Variable | No Opioid Use Disorder | Opioid Use Disorder | p Value |
|---|---|---|---|
| Patient count (%) | 175,565 (98.5%) | 2650 (1.5%) | - |
| Average Age (y) | 55.9 | 52.1 | p < 0.01 * |
| Female (%) | 48.2 | 49.6 | p = 0.15 |
| Medicare (%) | 34.4 | 37 | p < 0.01 * |
| Medicaid (%) | 12.4 | 27.2 | |
| Private, including HMO (%) | 41.5 | 26.4 | |
| Self-pay (%) | 2.6 | 5.1 | |
| No charge (%) | 0.2 | 0.6 | |
| Other (%) | 8.9 | 3.8 | |
| Hypertension (%) | 43.3 | 40.9 | p = 0.17 |
| Dyslipidemia (%) | 31.7 | 23.8 | p < 0.01 * |
| OSA (%) | 9.3 | 11.3 | p < 0.01 * |
| Nicotine Dependence (%) | 19.5 | 14.5 | p < 0.01 * |
| Chronic Anemia (%) | 3.3 | 6.4 | p < 0.01 * |
| Osteoporosis (%) | 2.3 | 2.1 | p < 0.01 * |
| Parkinson’s Disease (%) | 0.6 | 0.2 | p = 0.01 * |
| Alzheimer’s Disease (%) | 0.2 | 0.2 | p = 0.70 |
| Chronic Kidney Disease (%) | 5.2 | 6.6 | p < 0.01 * |
| Congestive Heart Failure (%) | 1.1 | 1.3 | p = 0.34 |
| Obesity (%) | 19 | 16.8 | p < 0.01 * |
| Diabetes Mellitus (%) | 20.8 | 20.2 | p = 0.41 |
| IBD (%) | 0.5 | 0.6 | p = 0.91 |
| Thyroid Disorder (%) | 11.8 | 12.3 | p = 0.45 |
| No Opioid Use Disorder | Opioid Use Disorder | Significance | |
|---|---|---|---|
| Length of stay mean (Days) | 3.3 (Std. deviation 6.2) | 7.9 (Std. deviation 12.8) | p < 0.01 * |
| Total charges mean ($) | 96,311 (Std. deviation 109,386) | 139,207 (Std. deviation 141,288) | p < 0.01 * |
| Number of procedures on this record | 3.5 (Std. deviation 2.2) | 4.2 (Std. deviation 2.8) | p < 0.01 * |
| Variable | No Opioid Use Disorder | Opioid Use Disorder | p Value |
|---|---|---|---|
| Patient count (%) | 2650 | 2650 | - |
| Average Age (y) | 52.1 | 52.1 | p = 0.97 |
| Female (%) | 48.3 | 49.6 | p = 0.34 |
| Medicare (%) | 37 | 37 | p = 0.08 |
| Medicaid (%) | 26.4 | 27.2 | |
| Private, including HMO (%) | 28.5 | 26.4 | |
| Self-pay (%) | 4.2 | 5.1 | |
| No charge (%) | 0.2 | 0.6 | |
| Other (%) | 3.8 | 3.8 | |
| Hypertension (%) | 40.2 | 40.9 | p = 0.58 |
| Dyslipidemia (%) | 24.5 | 23.8 | p = 0.52 |
| OSA (%) | 11.5 | 11.3 | p = 0.83 |
| Nicotine Dependence (%) | 14.9 | 14.5 | p = 0.70 |
| Chronic Anemia (%) | 5.5 | 6.4 | p = 0.15 |
| Osteoporosis (%) | 2.3 | 2.1 | p = 0.78 |
| Parkinson’s Disease (%) | 0.4 | 0.2 | p = 0.20 |
| Alzheimer’s Disease (%) | 0.2 | 0.2 | p = 1 |
| Chronic Kidney Disease (%) | 7 | 6.6 | p = 0.59 |
| Congestive Heart Failure (%) | 1.1 | 1.3 | p = 0.34 |
| Obesity (%) | 17.5 | 16.8 | p = 0.47 |
| Diabetes Mellitus (%) | 20.3 | 20.2 | p = 0.86 |
| IBD (%) | 0.9 | 0.6 | p = 0.11 |
| Thyroid Disorder (%) | 12 | 12.3 | p = 0.74 |
| No Opioid Use Disorder | Opioid Use Disorder | Significance | |
|---|---|---|---|
| Length of stay mean (Days) | 2.7 (Std. deviation 4.6) | 7.9 (Std. deviation 12.8) | p < 0.01 * |
| Total charges mean ($) | 82,179 (Std. deviation 92,598) | 139,207 (Std. deviation 141,288) | p < 0.01 * |
| Number of procedures on this record | 3.0 (Std. deviation 2.2) | 4.2 (Std. deviation 2.8) | p < 0.01 * |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Maman, D.; Nandakumar, M.; Steinfeld, Y.; Berkovich, Y. Preoperative Opioid Use Disorder Predicts Prolonged Ventilation, Central Line Placement, and Major Anesthesiology Complications After ACDF Surgery: A Big Data Analysis of 180,000 Cases. J. Clin. Med. 2025, 14, 6661. https://doi.org/10.3390/jcm14186661
Maman D, Nandakumar M, Steinfeld Y, Berkovich Y. Preoperative Opioid Use Disorder Predicts Prolonged Ventilation, Central Line Placement, and Major Anesthesiology Complications After ACDF Surgery: A Big Data Analysis of 180,000 Cases. Journal of Clinical Medicine. 2025; 14(18):6661. https://doi.org/10.3390/jcm14186661
Chicago/Turabian StyleMaman, David, Maneesh Nandakumar, Yaniv Steinfeld, and Yaron Berkovich. 2025. "Preoperative Opioid Use Disorder Predicts Prolonged Ventilation, Central Line Placement, and Major Anesthesiology Complications After ACDF Surgery: A Big Data Analysis of 180,000 Cases" Journal of Clinical Medicine 14, no. 18: 6661. https://doi.org/10.3390/jcm14186661
APA StyleMaman, D., Nandakumar, M., Steinfeld, Y., & Berkovich, Y. (2025). Preoperative Opioid Use Disorder Predicts Prolonged Ventilation, Central Line Placement, and Major Anesthesiology Complications After ACDF Surgery: A Big Data Analysis of 180,000 Cases. Journal of Clinical Medicine, 14(18), 6661. https://doi.org/10.3390/jcm14186661





