Assessment of Biomechanics Following Calcaneal Fracture Treatment with Internal Plate Fixation or Ilizarov External Fixation: A Retrospective, Two-Center Study
Abstract
1. Introduction
2. Materials and Methods
2.1. Subjects
2.2. Protocol of Pedobarographic Analysis
2.3. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Biz, C.; Barison, E.; Ruggieri, P.; Iacobellis, C. Radiographic and functional outcomes after displaced intra-articular calcaneal fractures: A comparative cohort study among the traditional open technique (ORIF) and percutaneous surgical procedures (PS). J. Orthop. Surg. Res. 2016, 11, 92. [Google Scholar] [CrossRef]
- van Hoeve, S.; de Vos, K.; Verbruggen, J.; Willems, P.; Meijer, K.; Poeze, M. Gait analysis and functional outcome after calcaneal fracture. J. Bone Jt. Surg. 2015, 97, 1879–1888. [Google Scholar] [CrossRef]
- Wang, Q.; Zhang, N.; Guo, W.; Wang, W.; Zhang, Q. Cannulated screw fixation versus plate fixation in treating displaced intra-articular calcaneus fractures: A systematic review and meta-analysis. Int. Orthop. 2021, 45, 2411–2421. [Google Scholar] [CrossRef] [PubMed]
- Schepers, T.; Backes, M.; Dingemans, S.A.; De Jong, V.M.; Luitse, J.S.K. Similar anatomical reduction and lower complication rates with the sinus tarsi approach compared with the extended lateral approach in displaced intra-articular calcaneal fractures. J. Orthop. Trauma 2017, 31, 293–298. [Google Scholar] [CrossRef]
- Fan, B.; Zhou, X.; Wei, Z.; Ren, Y.; Lin, W.; Hao, Y.; Shi, G.; Feng, S. Cannulated screw fixation and plate fixation for displaced intra-articular calcaneus fracture: A meta-analysis of randomized controlled trials. Int. J. Surg. 2016, 34, 64–72. [Google Scholar] [CrossRef]
- Bohl, D.D.; Ondeck, N.T.; Samuel, A.M.; Diaz-Collado, P.J.; Nelson, S.J.; Basques, B.A.; Leslie, M.P.; Grauer, J.N. Demographics, Mechanisms of Injury, and Concurrent Injuries Associated with Calcaneus Fractures: A Study of 14,516 Patients in the American College of Surgeons National Trauma Data Bank. Foot Ankle Spec. 2017, 10, 402–410. [Google Scholar] [CrossRef]
- Ibrahim, T.; Rowsell, M.; Rennie, W.; Brown, A.R.; Taylor, G.J.; Gregg, P.J. Displaced intra-articular calcaneal fractures: 15- year follow-up of a randomised controlled trial of conservative versus operative treatment. Injury 2007, 38, 848–855. [Google Scholar] [CrossRef]
- Jiang, N.; Lin, Q.R.; Diao, X.C.; Wu, L.; Yu, B. Surgical versus nonsurgical treatment of displaced intra-articular calcaneal fracture: A meta-analysis of current evidence base. Int. Orthop. 2012, 36, 1615–1622. [Google Scholar] [CrossRef] [PubMed]
- Potter, M.Q.; Nunley, J.A. Long-term functional outcomes after operative treatment for intra-articular fractures of the calcaneus. J. Bone Jt. Surg. 2009, 91, 1854–1860. [Google Scholar] [CrossRef]
- Brand, A.; Klopfer-Kramer, I.; Bottger, M.; Kroger, I.; Gaul, L.; Wackerle, H.; Musig, J.A.; Dietrich, A.; Gabel, J.; Augat, P. Gait characteristics and functional outcomes during early follow-up are comparable in patients with calcaneal fractures treated by either the sinus tarsi or the extended lateral approach. Gait Posture 2019, 70, 190–195. [Google Scholar] [CrossRef] [PubMed]
- Mauffrey, C.; Klutts, P.; Seligson, D. The use of circular fine wire frames for the treatment of displaced intra-articular calcaneal fractures. J. Orthop. Traumatol. 2009, 10, 9. [Google Scholar] [CrossRef][Green Version]
- Zgonis, T.; Roukis, T.S.; Polyzois, V.D. The use of Ilizarov technique and other types of external fixation for the treatment of intra-articular calcaneal fractures. Clin. Podiatr. Med. Surg. 2006, 23, 343–353. [Google Scholar] [CrossRef] [PubMed]
- Buckley, R.; Tough, S.; McCormack, R.; Pate, G.; Leighton, R.; Petrie, D.; Galpin, R. Operative compared with nonoperative treatment of displaced intra-articular calcaneal fractures: A prospective, randomized, controlled multicenter trial. J. Bone. Jt. Surg. 2002, 84, 1733–1744. [Google Scholar] [CrossRef] [PubMed]
- Audet, M.A.; Benedick, A.; Breslin, M.A.; Schmidt, T.; Vallier, H.A. Determinants of functional outcome following ankle fracture. OTA Int. 2021, 4, e139. [Google Scholar] [CrossRef] [PubMed]
- Park, E.S.; Choi, Y.; Lee, J.; Park, S.H.; Lee, H.S. Calcaneal fracture: Results of earlier rehabilitation after open reduction and internal fixation. Arch. Orthop. Trauma Surg. 2021, 141, 929–936. [Google Scholar] [CrossRef]
- Sanders, R. Displaced intra-articular fractures of the calcaneus. J. Bone Jt. Surg. 2000, 82, 225–250. [Google Scholar] [CrossRef]
- Wei, N.; Zhou, Y.; Chang, W.; Zhang, Y.; Chen, W. Displaced Intra-articular Calcaneal Fractures: Classification and Treatment. Orthopedics 2017, 40, e921–e929. [Google Scholar] [CrossRef]
- Barei, D.P.; Bellabarba, C.; Sangeorzan, B.J.; Benirschke, S.K. Fractures of the Calcaneus. Orthop. Clin. 2002, 33, 263–285. [Google Scholar] [CrossRef]
- Esenkaya, İ.; Türkmensoy, F.; Kemah, B.; Poyanlı, O.Ş. Surgical treatment of displaced intraarticular calcaneus fractures using anatomical lateral frame plate. Ulus. Travma Acil Cerrahi Derg. Turk. J. Trauma Emerg. Surg. 2018, 24, 156–161. [Google Scholar] [CrossRef]
- Radnay, C.S.; Clare, M.P.; Sanders, R.W. Subtalar fusion after displaced intra-articular calcaneal fractures: Does initial operative treatment matter? J. Bone Jt. Surg. 2010, 92 (Suppl. 1), 32–43. [Google Scholar] [CrossRef]
- Vicenti, G.; Carrozzo, M.; Solarino, G.; Caizzi, G.; De Crescenzo, A.; Portaluri, M.; Mori, C.M.; Vittore, D.; Moretti, B. Comparison of Plate, Calcanealplasty and External Fixation in the Management of Calcaneal Fractures. Injury 2019, 50 (Suppl. 4), S39–S46. [Google Scholar] [CrossRef]
- Hetsroni, I.; Ben-Sira, D.; Nyska, M.; Ayalon, M. Plantar pressure anomalies after open reduction with internal fixation of high-grade calcaneal fractures. Foot Ankle Int. 2014, 35, 712–718. [Google Scholar] [CrossRef]
- Schepers, T.; van der Stoep, A.; van der Avert, H.; van Lieshout, E.M.; Patka, P. Plantar pressure analysis after percutaneous repair of displaced intra-articular calcaneal fractures. Foot Ankle Int. 2008, 29, 128–135. [Google Scholar] [CrossRef]
- Pelc, M.; Hryniuk, W.; Bobiński, A.; Kochańska-Bieri, J.; Tomczyk, Ł.; Pili, D.; Urbański, W.; Lech, M.; Morasiewicz, P. Assessment of Function in Patients after Calcaneal Fracture Treatment with the Ilizarov Method. J. Clin. Med. 2024, 13, 4671. [Google Scholar] [CrossRef]
- Morasiewicz, P.; Pelc, M.; Tomczyk, Ł.; Kochanska-Bieri, J.; Bobiński, A.; Pili, D.; Reichert, P. Clinical and radiological assessment of the Polish modification of the Ilizarov external fixator for the treatment of intra-articular calcaneal fractures. Adv. Clin. Exp. Med. 2024; Online ahead of print. [Google Scholar] [CrossRef] [PubMed]
- Mitchell, M.J.; McKinley, J.C.; Robinson, C.M. The epidemiology of calcaneal fractures. Foot 2009, 19, 197–200. [Google Scholar] [CrossRef] [PubMed]
- Biggi, F.; Di Fabio, S.; D’Antimo, C. Percutaneous calcaneoplasty in displaced intraarticular calcaneal fractures. J. Orthop. Traumatol. 2013, 14, 307–310. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Labbe, J.L.; Peres, O.; Leclair, O.; Goulon, R.; Scemama, P.; Jourdel, F. Minimally invasive treatment of displaced intra-articular calcaneal fractures using the balloon kyphoplasty technique: Preliminary study. Orthop. Traumatol. Surg. Res. 2013, 99, 829–836. [Google Scholar] [CrossRef]
- Clare, M.P.; Crawford, W.S. Managing complications of calcaneus fractures. Foot Ankle Clin. 2017, 22, 105–116. [Google Scholar] [CrossRef]
- Ene, R.; Popescu, D.; Panaitescu, C.; Circota, G.; Cirstoiu, M.; Cirstoiu, C. Low complications after minimally invasive fixation of calcaneus fracture. J. Med. Life 2013, 6, 80–83. [Google Scholar]
- Arastu, M.; Sheehan, B.; Buckley, R. Minimally invasive reduction and fixation of displaced calcaneal fractures: Surgical technique and radiographic analysis. Int. Orthop. 2014, 38, 539–545. [Google Scholar] [CrossRef]
- Ebben, B.J.; Myerson, M.S. Management of the subtalar joint following calcaneal fracture malunion. Foot Ankle Clin. 2022, 27, 787–803. [Google Scholar] [CrossRef] [PubMed]
- Jandova, S.; Pazour, J.; Janura, M. Comparison of plantar pressure distribution during walking after two different surgical treatments for calcaneal fracture. J. Foot Ankle Surg. 2018, 57, 1135–1143. [Google Scholar] [CrossRef] [PubMed]
- Hetsroni, I.; Nyska, M.; Ben-Sira, D.; Arnson, Y.; Buksbaum, C.H.; Aliev, E.; Mann, G.; Massarwe, S.; Rozenfeld, G.; Ayalon, M. Analysis of Foot and Ankle Kinematics After Operative Reduction of High-Grade Intra-Articular Fractures of the Calcaneus. J. Trauma Acute Care Surg. 2011, 70, 5. [Google Scholar] [CrossRef] [PubMed]
- Genc, Y.; Gultekin, A.; Mutlu Duymus, T.; Mutlu, S.; Mutlu, H.; Komur, B. Pedobarography in the Assessment of Postoperative Calcaneal Fracture Pressure With Gait. J. Foot Ankle Surg. 2016, 55, 99–105. [Google Scholar] [CrossRef]
- Pataky, T.C.; Savage, R.; Bates, K.T.; Sellers, W.I.; Crompton, R.H. Short-term step-to-step correlation in plantar pressure distributions during treadmill walking, and implications for footprint trail analysis. Gait Posture 2013, 38, 1054–1057. [Google Scholar] [CrossRef][Green Version]
- Ali, A.M.; Elsaied, M.A.; Elmoghazy, N. Management of calcaneal fractures using the Ilizarov external fixator. Acta Orthop. Belg. 2009, 75, 51–56. [Google Scholar][Green Version]
- Morasiewicz, P.; Konieczny, G.; Dejnek, M.; Morasiewicz, L.; Urbanski, W.; Kulej, M.; Dragan, S.Ł.; Dragan, S.F.; Pawik, Ł. Pedobarographic analysis of body weight distribution on the lower limbs and balance after ankle arthrodesis with Ilizarov fixation and internal fixation. Biomed. Eng. Online 2018, 17, 174. [Google Scholar] [CrossRef]
- Pelc, M.; Kazubski, K.; Urbański, W.; Leyko, P.; Kochańska-Bieri, J.; Tomczyk, Ł.; Konieczny, G.; Morasiewicz, P. Balance and Weight Distribution over the Lower Limbs Following Calcaneal Fracture Treatment with the Ilizarov Method. J. Clin. Med. 2024, 13, 1676. [Google Scholar] [CrossRef]
- Kuzminas, E.; Komžienė, R.; Markauskienė, A.; Žukauskienė, M. Associations between Ankle Instability and Weight Distribution in the feet. Prof. Stud. Theory Pract. 2023, 27, 71–80. [Google Scholar] [CrossRef]
- Cibura, C.; Lülsdorff, R.; Rosteius, T.; Brinkemper, A.; Bernstorff, M.; Jettkant, B.; Godolias, P.; Ramczykowski, T.; Königshausen, M.; Schildhauer, T.A.; et al. Effects on gait kinematics, pedobarography, functional and subjective results after isolated chopart injury. BMC Musculoskelet Disord. 2024, 25, 335. [Google Scholar] [CrossRef] [PubMed]
- Zhao, B.; Xu, X.; Sun, Q.; Liu, Y.; Zhao, Y.; Wang, D.; Gao, Y.; Zhou, J. Comparison between screw fixation and plate fixation via sinus tarsi approach for displaced intra-articular calcaneal fractures: A systematic review and meta-analysis. Arch. Orthop. Trauma Surg. 2024, 144, 59–71. [Google Scholar] [CrossRef] [PubMed]
- Purdie, S.D.; Hoskins, N.; Sumarlie, R.J.; Eiamampai, N.; Lebeslé, P.; Wood, F.; Chinmayee, A.; Lim, W.Q.; Senthilkumaran, S.; Fisher, L.; et al. Minimally invasive surgical techniques compared to an extensile lateral approach in the management of displaced intra-articular calcaneal fractures. A systematic review and meta-analysis of randomised controlled trials. Foot Ankle Surg. 2025, 31, 473–485. [Google Scholar] [CrossRef] [PubMed]
| Analyzed Variable | Ilizarov Group | Plate Group | p |
|---|---|---|---|
| Mean ± Standard Deviation | |||
| Entire foot load distribution NOL [%] | 53.11 ± 7.23 | 57.89 ± 18.35 | 0.46 |
| Forefoot load distribution NOL [%] | 47.33 ± 8.58 | 40.57 ± 16.52 | 0.261 |
| Hindfoot load distribution NOL [%] | 52.66 ± 8.58 | 59.42 ± 16.52 | 0.261 |
| Entire foot load distribution OL [%] | 46.89 ± 8.67 | 41.57 ± 17.83 | 0.489 |
| Forefoot load distribution OL [%] | 42.33 ± 9.48 | 35.94 ± 17.74 | 0.323 |
| Hindfoot load distribution OL [%] | 57.66 ± 9.48 | 64.05 ± 17.74 | 0.323 |
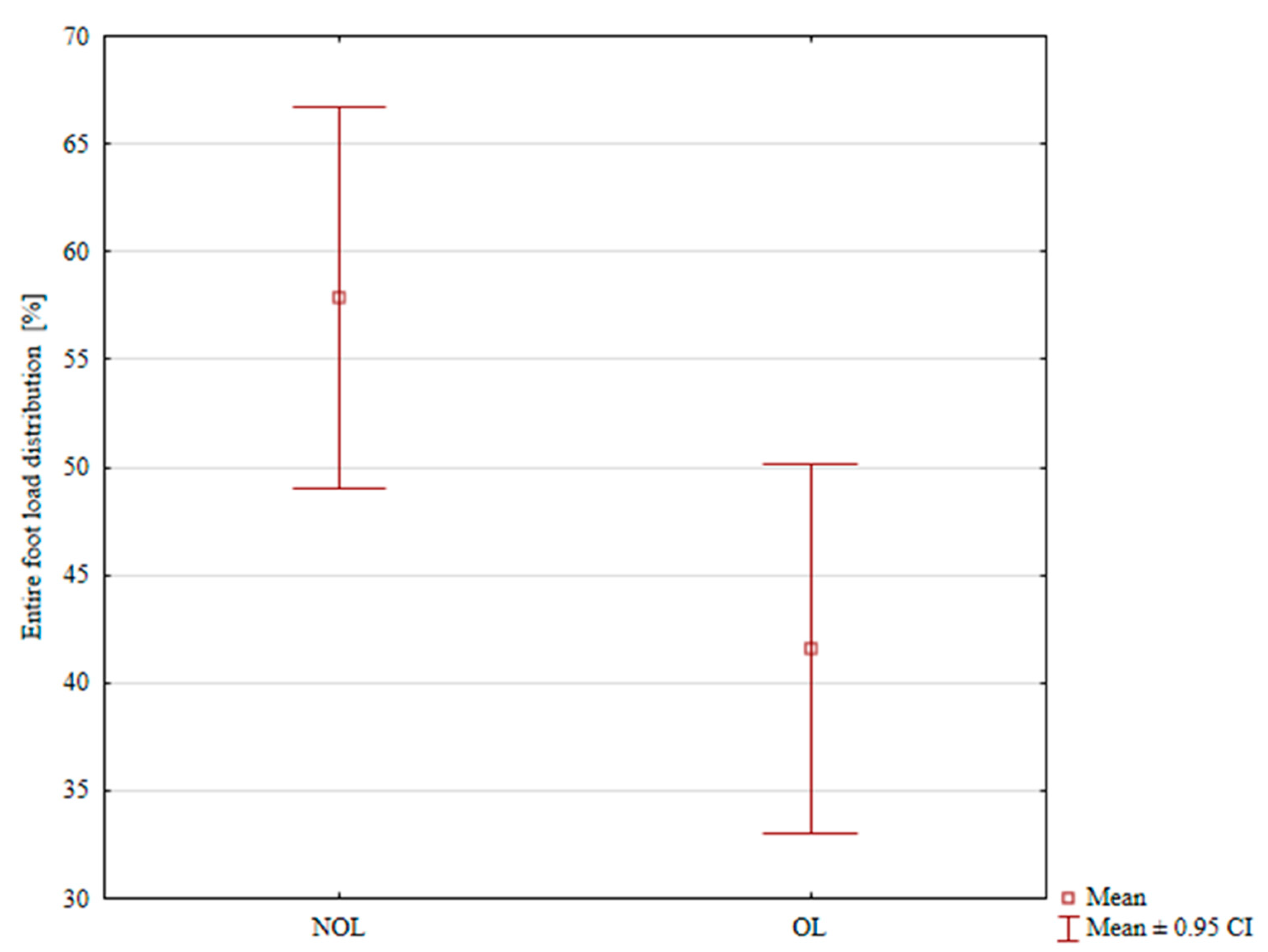
| Loads on Limb | Ilizarov Group | Plate Group |
|---|---|---|
| Mean ± Standard Deviation | ||
| entire foot load distribution NOL [%] | 53.11 ± 7.23 | 57.89 ± 18.35 |
| entire foot load distribution OL [%] | 46.89 ± 8.67 | 41.57 ± 17.83 |
| p | 0.077 | 0.008 |
| Forefoot load distribution NOL [%] | 47.33 ± 8.58 | 40.57 ± 16.52 |
| Forefoot load distribution OL [%] | 42.33 ± 9.48 | 35.94 ± 17.74 |
| p | 0.258 | 0.41 |
| Hindfoot load distribution NOL [%] | 52.66 ± 8.58 | 59.42 ± 16.527 |
| Hindfoot load distribution OL [%] | 57.66 ± 9.48 | 64.05 ± 17.74 |
| p | 0.258 | 0.41 |
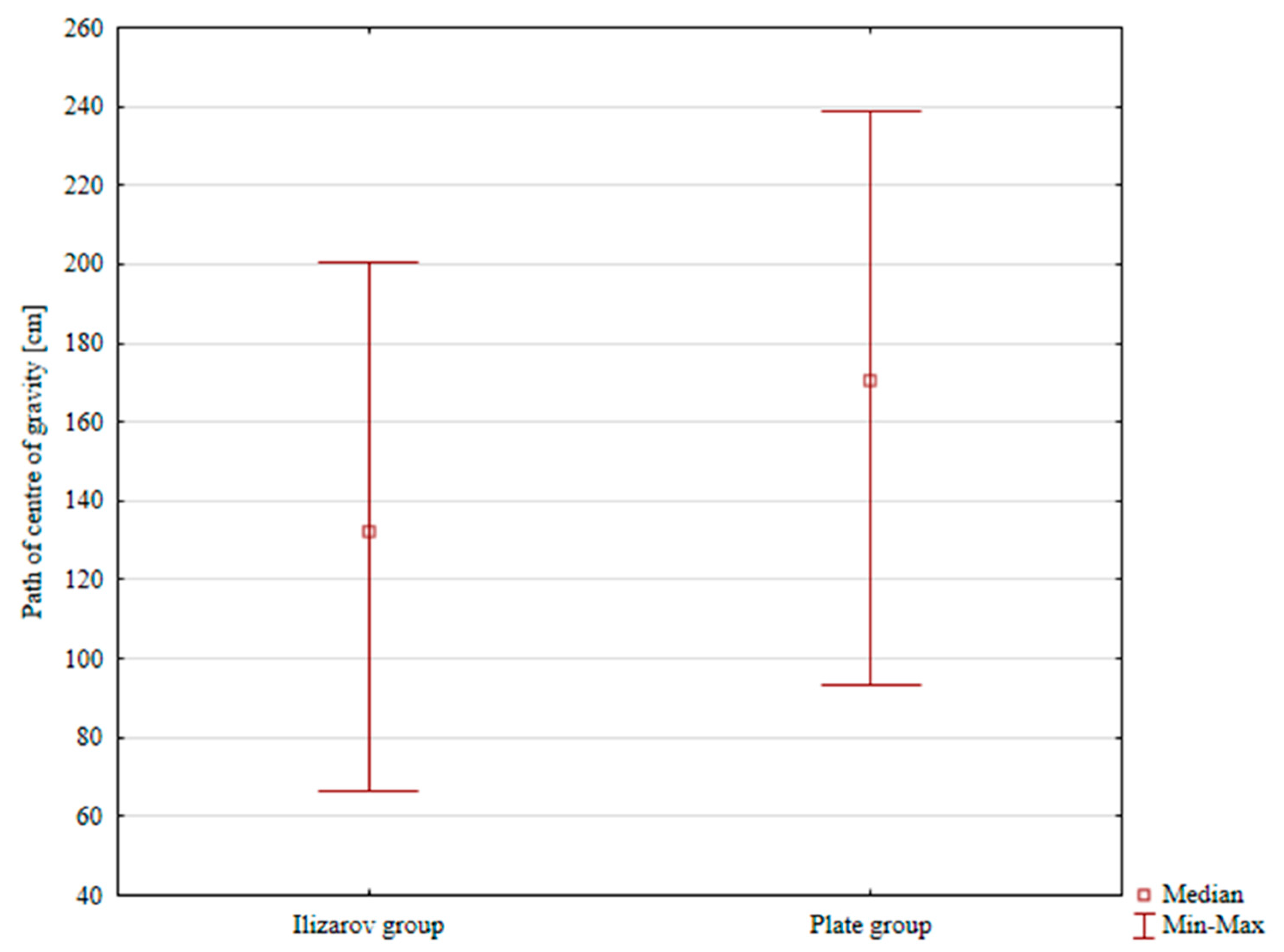
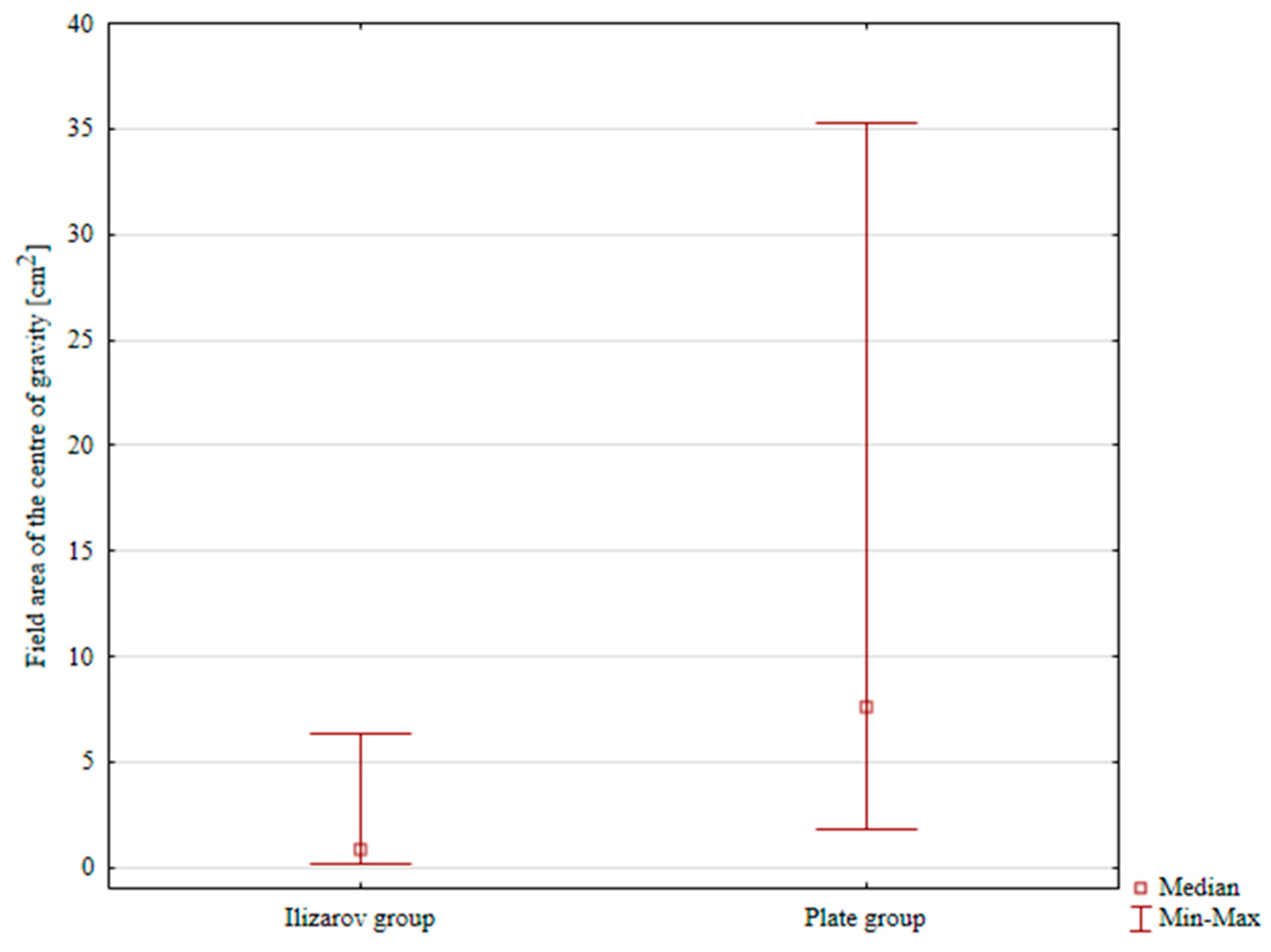
| Analyzed Variable | Ilizarov Group | Plate Group | Z | p | |
|---|---|---|---|---|---|
| Value | |||||
| Path of center of gravity [mm] | Q1 | 107.735 | 156.74 | −2.262 | 0.023 |
| Median | 132.416 | 170.21 | |||
| Q3 | 148.354 | 201.55 | |||
| Field area of the center of gravity [mm2] | Q1 | 0.608 | 4.5 | −3.787 | p < 0.001 |
| Median | 0.849 | 7.57 | |||
| Q3 | 1.806 | 10.04 | |||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kowal, I.; Pelc, M.; Pili, D.; Tomczyk, Ł.; Operacz, R.; Morasiewicz, P. Assessment of Biomechanics Following Calcaneal Fracture Treatment with Internal Plate Fixation or Ilizarov External Fixation: A Retrospective, Two-Center Study. J. Clin. Med. 2025, 14, 6651. https://doi.org/10.3390/jcm14186651
Kowal I, Pelc M, Pili D, Tomczyk Ł, Operacz R, Morasiewicz P. Assessment of Biomechanics Following Calcaneal Fracture Treatment with Internal Plate Fixation or Ilizarov External Fixation: A Retrospective, Two-Center Study. Journal of Clinical Medicine. 2025; 14(18):6651. https://doi.org/10.3390/jcm14186651
Chicago/Turabian StyleKowal, Igor, Marcin Pelc, Daniele Pili, Łukasz Tomczyk, Radosław Operacz, and Piotr Morasiewicz. 2025. "Assessment of Biomechanics Following Calcaneal Fracture Treatment with Internal Plate Fixation or Ilizarov External Fixation: A Retrospective, Two-Center Study" Journal of Clinical Medicine 14, no. 18: 6651. https://doi.org/10.3390/jcm14186651
APA StyleKowal, I., Pelc, M., Pili, D., Tomczyk, Ł., Operacz, R., & Morasiewicz, P. (2025). Assessment of Biomechanics Following Calcaneal Fracture Treatment with Internal Plate Fixation or Ilizarov External Fixation: A Retrospective, Two-Center Study. Journal of Clinical Medicine, 14(18), 6651. https://doi.org/10.3390/jcm14186651









