Tibial Anterior Cruciate Ligament Avulsion Fractures in Pediatric and Adult Populations: A Systematic Literature Review
Abstract
1. Introduction
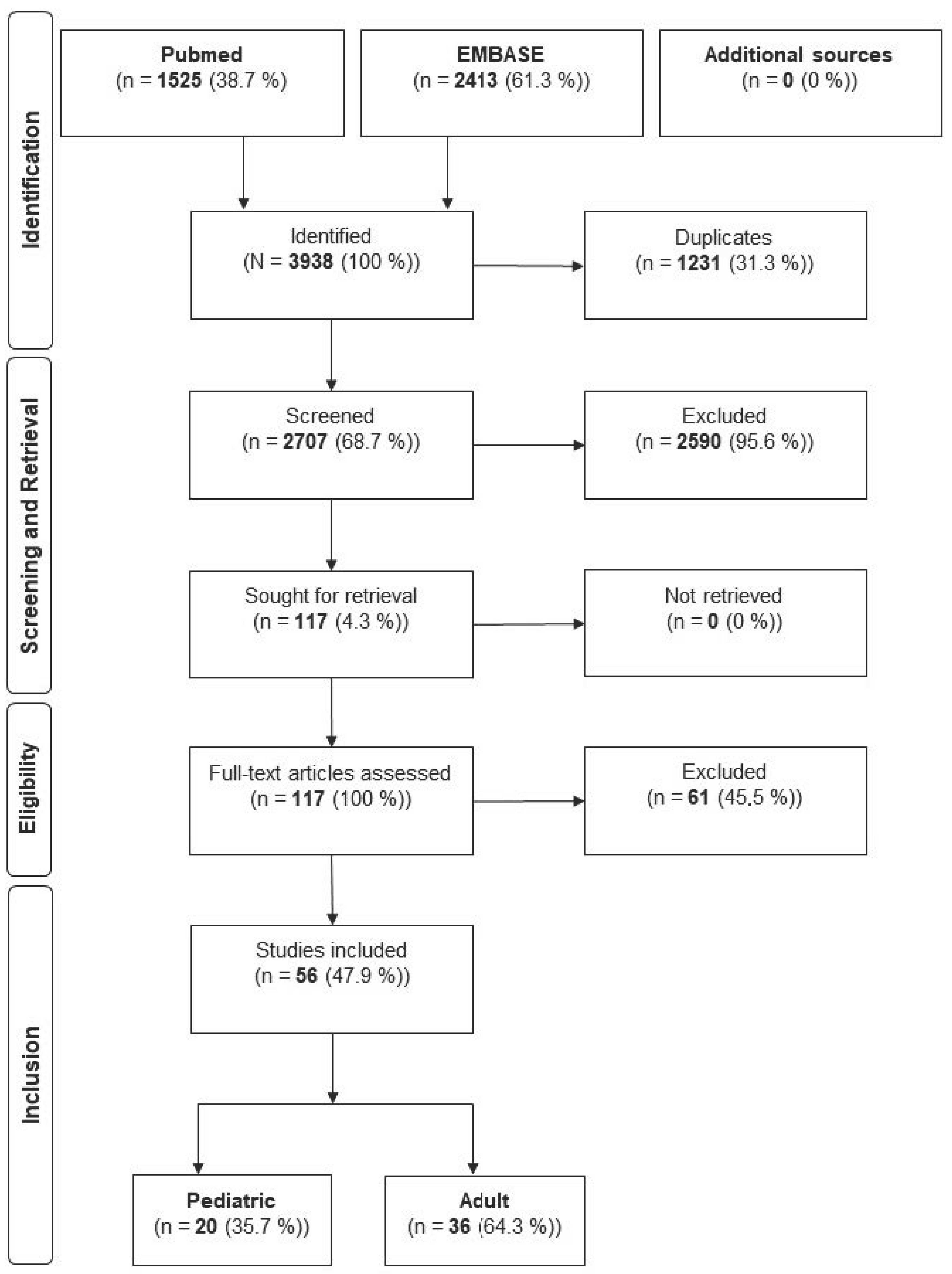
2. Material and Methods
3. Results
4. Discussion
- While TAFs are more common in males overall, the underlying mechanism in the pediatric population is usually sports trauma, whereas the underlying mechanism in the adult population is usually a road traffic accident.
- Across the reviewed studies, concomitant injuries were more often reported in adult patients than in pediatric patients, although differences may also reflect study design and reporting variability.
- Complications in general and arthrofibrosis, pain and revision surgery in particular are more common in the pediatric population, while malunion and non-union are more common in adults.
Supplementary Materials
Author Contributions
Funding
Conflicts of Interest
Abbreviations
| ACL | Anterior Cruciate Ligament |
| CT | Computed Tomography |
| MeSH | Medical Subject Headings |
| MRI | Magnetic Resonance Imaging |
| ORCID | Open Researcher and Contributor ID |
| PRISMA | Preferred Reporting Items for Systematic Reviews and Meta-Analyses |
| RTA | Road Traffic Accidents |
| SD | Standard deviation |
| TAF | Tibial Anterior Cruciate Ligament Avulsion Fractures |
References
- Shelbourne, K.D.; Patel, D.V.; Martini, D.J. Classification and management of arthrofibrosis of the knee after anterior cruciate ligament reconstruction. Am. J. Sports Med. 1996, 24, 857–862. [Google Scholar] [CrossRef]
- Meyers, A.L.; Tiwari, V.; Nelson, R. Tibial Eminence Fractures. In StatPearls; StatPearls Publishing LLC.: Treasure Island, FL, USA, 2025. [Google Scholar]
- van Loon, T.; Marti, R.K. A fracture of the intercondylar eminence of the tibia treated by arthroscopic fixation. Arthroscopy 1991, 7, 385–388. [Google Scholar] [CrossRef] [PubMed]
- Gans, I.; Baldwin, K.D.; Ganley, T.J. Treatment and Management Outcomes of Tibial Eminence Fractures in Pediatric Patients: A Systematic Review. Am. J. Sports Med. 2014, 42, 1743–1750. [Google Scholar] [CrossRef] [PubMed]
- McKoy, B.E.; Stanitski, C.L. Acute tibial tubercle avulsion fractures. Orthop. Clin. N. Am. 2003, 34, 397–403. [Google Scholar] [CrossRef] [PubMed]
- Hefferan, S.A.; Blaker, C.L.; Ashton, D.M.; Little, C.B.; Clarke, E.C. Structural Variations of Tendons: A Systematic Search and Narrative Review of Histological Differences Between Tendons, Tendon Regions, Sex, and Age. J. Orthop. Res. 2025, 43, 994–1011. [Google Scholar] [CrossRef]
- Zaricznyj, B. Avulsion fracture of the tibial eminence: Treatment by open reduction and pinning. J. Bone Jt. Surg. Am. 1977, 59, 1111–1114. [Google Scholar] [CrossRef]
- Shen, P.C.; Williams, B.A.; Edobor-Osula, O.F.; Blanco, J.S.; Crawford, L.M.; Greenhill, D.A.; Griffith, A.H.; Kaushal, N.K.; Kell, D.M.; Rashiwala, A.; et al. What is the Utilization and Impact of Advanced Imaging for Tibial Tubercle Fractures? An Analysis of 598 Patients from the Tibial Tubercle Study (TITUS) Group. J. Pediatr. Orthop. 2024, 44, e876–e882. [Google Scholar] [CrossRef] [PubMed]
- Tuca, M.; Bernal, N.; Luderowski, E.; Green, D.W. Tibial spine avulsion fractures: Treatment update. Curr. Opin. Pediatr. 2019, 31, 103–111. [Google Scholar] [CrossRef]
- Lubowitz, J.H.; Elson, W.S.; Guttmann, D. Part II: Arthroscopic treatment of tibial plateau fractures: Intercondylar eminence avulsion fractures. Arthroscopy 2005, 21, 86–92. [Google Scholar] [CrossRef]
- Feucht, M.J.; Brucker, P.U.; Camathias, C.; Frosch, K.H.; Hirschmann, M.T.; Lorenz, S.; Mayr, H.O.; Minzlaff, P.; Petersen, W.; Saier, T.; et al. Meniscal injuries in children and adolescents undergoing surgical treatment for tibial eminence fractures. Knee Surg. Sports Traumatol. Arthrosc. 2017, 25, 445–453. [Google Scholar] [CrossRef]
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. BMJ 2021, 372, n71. [Google Scholar] [CrossRef] [PubMed]
- Patterson, S.P.; Christiansen, G.B.; Daffner, R.H. Avulsion fracture of the tibial eminence in an adult with a unique mechanism of injury. Radiol. Case Rep. 2018, 13, 843–847. [Google Scholar] [CrossRef] [PubMed]
- Song, E.K.; Seon, J.K.; Park, S.J.; Yoon, T.R. Clinical outcome of avulsion fracture of the anterior cruciate ligament between children and adults. J. Pediatr. Orthop. B 2009, 18, 335–338. [Google Scholar] [CrossRef] [PubMed]
- Kendall, N.S.; Hsu, S.Y.; Chan, K.M. Fracture of the tibial spine in adults and children. A review of 31 cases. J. Bone Jt. Surg. Br. 1992, 74, 848–852. [Google Scholar] [CrossRef]
- Reuter, S.; Mellerowicz, H. Acute tibial tubercle avulsion fractures. Orthopade 2016, 45, 226–228+230–232. [Google Scholar] [CrossRef]
- Hale, R.; Hausselle, J.G.; Gonzalez, R.V. A preliminary study on the differences in male and female muscle force distribution patterns during squatting and lunging maneuvers. Comput. Biol. Med. 2014, 52, 57–65. [Google Scholar] [CrossRef]
- Shin, Y.W.; Kim, D.W.; Park, K.B. Tibial tubercle avulsion fracture according to different mechanisms of injury in adolescents: Tibial tubercle avulsion fracture. Medicine 2019, 98, e16700. [Google Scholar] [CrossRef]
- Lin, C.Y.; Casey, E.; Herman, D.C.; Katz, N.; Tenforde, A.S. Sex Differences in Common Sports Injuries. Pm R 2018, 10, 1073–1082. [Google Scholar] [CrossRef]
- Behan, F.P.; Maden-Wilkinson, T.M.; Pain, M.T.G.; Folland, J.P. Sex differences in muscle morphology of the knee flexors and knee extensors. PLoS ONE 2018, 13, e0190903. [Google Scholar] [CrossRef]
- Willis, R.B.; Blokker, C.; Stoll, T.M.; Paterson, D.C.; Galpin, R.D. Long-term follow-up of anterior tibial eminence fractures. J. Pediatr. Orthop. 1993, 13, 361–364. [Google Scholar] [CrossRef] [PubMed]
- Woo, S.L.; Hollis, J.M.; Adams, D.J.; Lyon, R.M.; Takai, S. Tensile properties of the human femur-anterior cruciate ligament-tibia complex. The effects of specimen age and orientation. Am. J. Sports Med. 1991, 19, 217–225. [Google Scholar] [CrossRef] [PubMed]
- Menge, T.J.; Chahla, J.; Mitchell, J.J.; Dean, C.S.; LaPrade, R.F. Avulsion of the Anterior Lateral Meniscal Root Secondary to Tibial Eminence Fracture. Am. J. Orthop. 2018, 47. [Google Scholar] [CrossRef] [PubMed]
- Cole, W.; Brown, S.; Vopat, B.; Heard, W.; Mulcahey, M. Epidemiology, Diagnosis, and Management of Tibial Tubercle Avulsion Fractures in Adolescents. JBJS Rev. 2020, 8, e0186. [Google Scholar] [CrossRef]
- Polakoff, D.R.; Bucholz, R.W.; Ogden, J.A. Tension band wiring of displaced tibial tuberosity fractures in adolescents. Clin. Orthop. Relat. Res. 1986, 209, 161–165. [Google Scholar] [CrossRef]
- Griffith, J.F.; Antonio, G.E.; Tong, C.W.; Ming, C.K. Cruciate ligament avulsion fractures. Arthroscopy 2004, 20, 803–812. [Google Scholar] [CrossRef] [PubMed]
- Florkow, M.C.; Willemsen, K.; Mascarenhas, V.V.; Oei, E.H.G.; van Stralen, M.; Seevinck, P.R. Magnetic Resonance Imaging Versus Computed Tomography for Three-Dimensional Bone Imaging of Musculoskeletal Pathologies: A Review. J. Magn. Reson. Imaging 2022, 56, 11–34. [Google Scholar] [CrossRef]
- Rhodes, J.T.; Cannamela, P.C.; Cruz, A.I.; Mayo, M.; Styhl, A.C.; Richmond, C.G.; Ganley, T.J.; Shea, K.G. Incidence of Meniscal Entrapment and Associated Knee Injuries in Tibial Spine Avulsions. J. Pediatr. Orthop. 2018, 38, e38–e42. [Google Scholar] [CrossRef]
- Binnet, M.; Gurkan, I.; Bayraktar, K.; Karakas, A. Arthroscopic reduction and fixation of tibial eminantia fractures. Acta Orthop. Traumatol. Turc. 1996, 30, 526–532. [Google Scholar]
- Kocher, M.S.; Foreman, E.S.; Micheli, L.J. Laxity and functional outcome after arthroscopic reduction and internal fixation of displaced tibial spine fractures in children. Arthroscopy 2003, 19, 1085–1090. [Google Scholar] [CrossRef]
- Osti, L.; Merlo, F.; Bocchi, L. Our experience in the arthroscopic treatment of fracture-avulsion of the tibial spine. Chir. Organi Mov. 1997, 82, 295–299. [Google Scholar]
- Vargas, B.; Lutz, N.; Dutoit, M.; Zambelli, P.Y. Nonunion after fracture of the anterior tibial spine: Case report and review of the literature. J. Pediatr. Orthop. B 2009, 18, 90–92. [Google Scholar] [CrossRef] [PubMed]
- Bram, J.T.; Aoyama, J.T.; Mistovich, R.J.; Ellis, H.B., Jr.; Schmale, G.A.; Yen, Y.M.; McKay, S.D.; Fabricant, P.D.; Green, D.W.; Lee, R.J.; et al. Four Risk Factors for Arthrofibrosis in Tibial Spine Fractures: A National 10-Site Multicenter Study. Am. J. Sports Med. 2020, 48, 2986–2993. [Google Scholar] [CrossRef]
- Tudisco, C.; Giovarruscio, R.; Febo, A.; Savarese, E.; Bisicchia, S. Intercondylar eminence avulsion fracture in children: Long-term follow-up of 14 cases at the end of skeletal growth. J. Pediatr. Orthop. B 2010, 19, 403–408. [Google Scholar] [CrossRef] [PubMed]
- Hunter, R.E.; Willis, J.A. Arthroscopic fixation of avulsion fractures of the tibial eminence: Technique and outcome. Arthroscopy 2004, 20, 113–121. [Google Scholar] [CrossRef] [PubMed]
| Characteristics | Pediatric n (%) | Adult n (%) |
|---|---|---|
| n | 208 (30.4) | 469 (69.6) |
| Gender | ||
| Male | 126 (60.6) | 241 (62.9) |
| Female | 69 (39.4) | 142 (37.1) |
| Not reported | 13 | 86 |
| Meyers and McKeever | ||
| Type I | 4 (2.2) | 3 (0.8) |
| Type II | 60 (32.8) | 87 (23.8) |
| Type III | 117 (63.9) | 232 (63.4) |
| Type IV | 2 (1.1) | 44 (12) |
| Not reported | 25 | 103 |
| Type of Injury | Pediatric n (%) | Adult n (%) |
|---|---|---|
| n | 8 (8.2) | 100 (35.6) |
| Meniscus injuries | 8 (100) | 56 (19.9) |
| Other ligament injuries | 0 | 24 (8.5) |
| Osteochondral injuries | 0 | 32 (11.4) |
| Joint dislocations | 0 | 1 (0.4) |
| Not reported | 110 | 188 |
| Pediatric n (%) | Adult n (%) | |
|---|---|---|
| Sports | 94 (65.7) | 97 (27.6) |
| RTA with a car | 19 (13.3) | 103 (29.3) |
| RTA with a motor- or bicycle | 16 (11.2) | 106 (30.2) |
| Fall | 14 (9.6) | 45 (12.9) |
| Not reported | 65 | 118 |
| Pediatric n (%) | Adult n (%) | |
|---|---|---|
| Diagnostics | ||
| MRI performed | 7 out of 20 Authors (35) | 19 out of 36 Authors (52.8) |
| Surgical technique | ||
| Conservative | 10 (7.2) | 5 (1.1) |
| Arthroscopic | 110 (79.1) | 411 (87.8) |
| Open | 19 (13.7) | 53 (11.1) |
| Not reported | 69 | 1 |
| Fixation method | ||
| Screws | 70 (40.5) | 29 (6.6) |
| Suture | 66 (38.2) | 219 (49.7) |
| Suture anchors | 22 (12.7) | 102 (23.1) |
| Other | 15 (8.7) | 91 (20.6) |
| Not reported | 35 | 28 |
| Pediatric n (%) | Adult n (%) | |
|---|---|---|
| Period to last Follow-Up * | 50.5 months (SD 90.6) | 25 months (SD 39.1) |
| Revisions | 55 (26.4) | 74 (18.6) |
| Hardware removal | 33 (15.9) | 62 (15.6) |
| Long-term return to sport | 96 out of 99 (97) | 202 out of 233 (86.7) |
| Complications | 73 (35.1) | 80 (17.1) |
| Arthrofibrosis | 42 (20.2) | 31 (6.6) |
| Instability & Laxity | 23 (11.1) | 19 (4.1) |
| Malunion | 4 (1.9) | 11 (2.3) |
| Nonunion | 1 (0.5) | 15 (3.2) |
| Pain | 3 (1.4) | 4 (0.9) |
| Not reported | 2 out of 20 Authors (10) | 0 out of 36 Authors |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Landré, V.; Teuben, M.; Klingebiel, F.K.-L.; Shehu, A.; Ensle, F.; Pape, H.-C.; Rauer, T. Tibial Anterior Cruciate Ligament Avulsion Fractures in Pediatric and Adult Populations: A Systematic Literature Review. J. Clin. Med. 2025, 14, 6316. https://doi.org/10.3390/jcm14176316
Landré V, Teuben M, Klingebiel FK-L, Shehu A, Ensle F, Pape H-C, Rauer T. Tibial Anterior Cruciate Ligament Avulsion Fractures in Pediatric and Adult Populations: A Systematic Literature Review. Journal of Clinical Medicine. 2025; 14(17):6316. https://doi.org/10.3390/jcm14176316
Chicago/Turabian StyleLandré, Vincent, Michel Teuben, Felix Karl-Ludwig Klingebiel, Alba Shehu, Falko Ensle, Hans-Christoph Pape, and Thomas Rauer. 2025. "Tibial Anterior Cruciate Ligament Avulsion Fractures in Pediatric and Adult Populations: A Systematic Literature Review" Journal of Clinical Medicine 14, no. 17: 6316. https://doi.org/10.3390/jcm14176316
APA StyleLandré, V., Teuben, M., Klingebiel, F. K.-L., Shehu, A., Ensle, F., Pape, H.-C., & Rauer, T. (2025). Tibial Anterior Cruciate Ligament Avulsion Fractures in Pediatric and Adult Populations: A Systematic Literature Review. Journal of Clinical Medicine, 14(17), 6316. https://doi.org/10.3390/jcm14176316






