Fracture Patterns in Fatal Free Falls: A Systematic Review of Intrinsic and Extrinsic Risk Factors and the Role of Postmortem CT
Abstract
1. Introduction
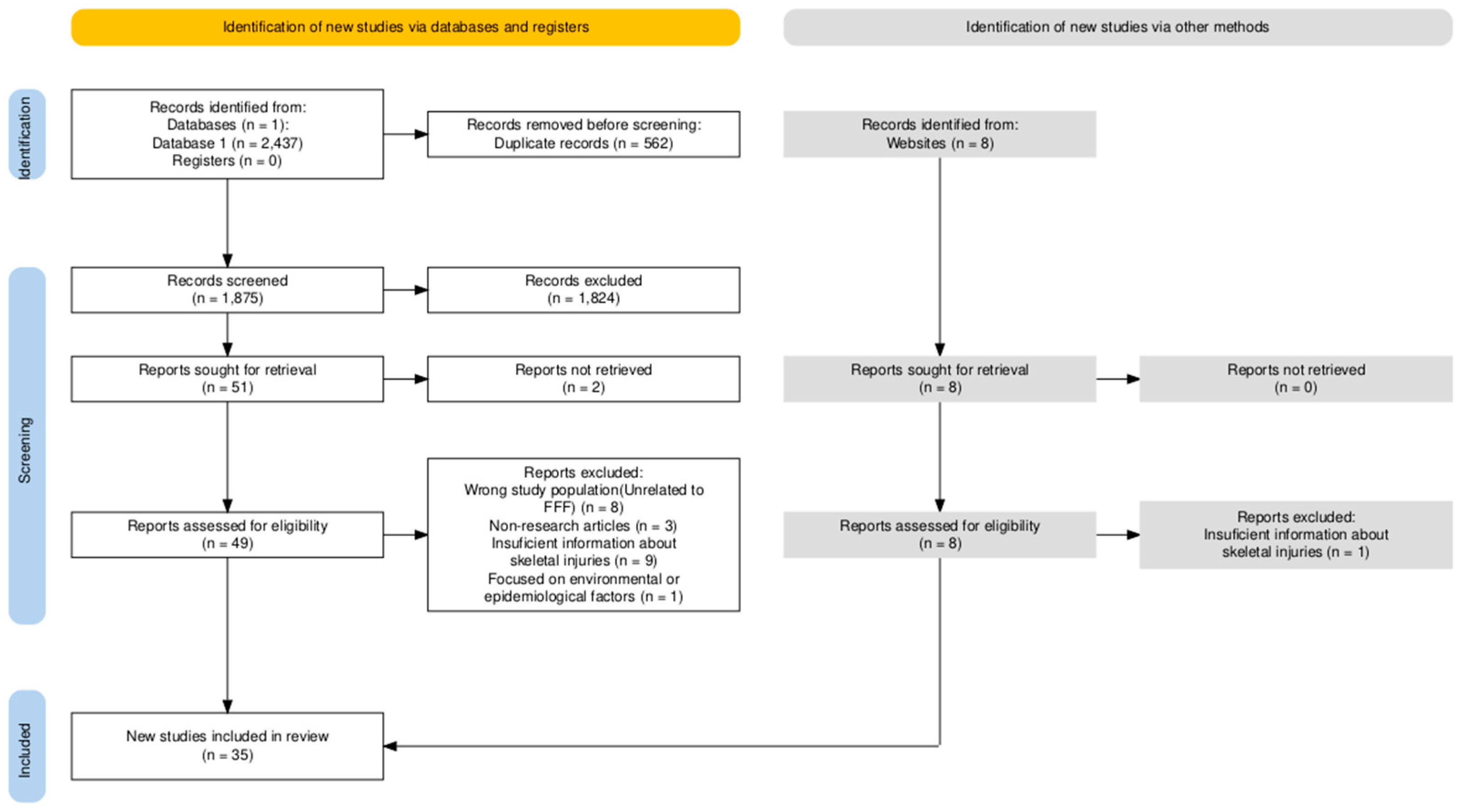
2. Methods for Literature Selection
- Studies published in English.
- Studies that comprise at least 10 cases were considered, as papers with fewer cases were deemed unlikely to provide reliable conclusions regarding skeletal injuries.
- Studies that focus exclusively on fatal falls, given that injuries from non-fatal falls differ in severity and nature.
- Clear descriptions of skeletal injuries, along with provided frequencies and patterns.
- Original studies featuring postmortem or PMCT findings.
- Full text available online (paywalled studies were included as long as the complete work was accessible).
- Publications in peer-reviewed journals.
- Studies published in languages other than English.
- Studies with fewer than 10 cases.
- Studies that describe injuries in survivors or hospitalized patients following falls.
- Injuries described in vague detail or reported only partially.
- Studies focusing on types of falls other than free falls—such as stair falls or interrupted falls. However, it is essential to note that many studies combine different types of falls; in our study, we decided that these can be included if they meet the inclusion criteria, provided that other types of falls account for a minority of cases.
- Studies about FFF that do not focus on the injuries.
- Conference abstracts, dissertations, organizational reports, and other forms of grey literature.
3. Intrinsic Variables
4. Extrinsic Variables
5. General Fracture Frequencies and Their Anatomical Distribution
5.1. Skull Fractures
- The cranial vault and skull base were fractured with similar frequency, with an average prevalence of 29.36% for vault fractures and 25.06% for skull base fractures.
- When studies combined vault and base fractures, the reported prevalence was 29.86%. Facial skeleton fractures were observed in 0% to 32.5% of cases, with an average prevalence of 12.79%. Four studies mentioned the occipital “ring fracture,” often associated with deceleration injuries, nine cases were reported. Mandible fractures were reported in two studies, acounting for 9.4% and 15% of all fractures, respectively.
5.2. Spinal Column Fractures
- The cervical spine was fractured in an average of 14% of cases, which had referred spinal fractures (median: 12.2%, range: 1.1–50%).
- Upper cervical fractures were more common than lower cervical fractures (59.89% vs. 40.11%). Among upper cervical fractures, C1 was fractured in 21.1% of cases, while C2 fractures accounted for 62.39%, and 16.5% of victims experienced C0/C1 dislocation. Dens fractures were nearly twice as common as arch fractures. Thoracic spine fractures occurred in an average of 16.46% of cases in related studies (median: 10%, range: 1.3–52.27%). Lumbar spine injuries were reported in an average of 6.8% of cases (median: 4.1%), making it the least commonly injured spinal region, with only 145 cases reported. Thoracolumbar fractures were reported with rates of 31.2%, 42.1%, and 67.9%. The average prevalence was 47.07%, affecting 253 victims. Only one study separately examined the sacrum and coccyx, with fractures reported in 9% (28/307) of cases.
5.3. Pelvic Fractures
- Pelvic fractures were observed in an average of 29.56% of cases related to this injury (median: 19.78%), with reported frequencies ranging from 1.1% to 100%.
- The pubic symphysis was disrupted in 4.8% to 36% of cases across the two studies that examined it. Sacroiliac joint damage was noted in three studies with an average prevalence of 22.07%.
- One study reported pubic bone fractures in 13.97% of cases, while another found fractures in 22% of the ilio-pubic rami and 16% of the ischio-pubic rami.
5.4. Upper and Lower Limbs Fractures
- Upper limb fractures occurred in an average of 36.72% of cases throughout related studies (median, 20.7%; range, 5–100%).
- Clavicle fractures showed a mean prevalence of 7.69%, scapula fractures 2.74%, humerus fractures 11.19%, forearm fractures (radius and ulna) 10.52%, and hand fractures 2.52%.
- Lower limb fractures were observed with an average prevalence of 39.18% in studies related to this topic (median: 29.07%, range: 8–100%).
- Femur fractures showed a mean prevalence of 13.47%, shin fractures a prevalence of 10.01%, and foot fractures a prevalence of 5.23%. Seven cases of calcaneal rupture were observed.
5.5. Chest Fractures
- Rib fractures emerged as the most frequently reported skeletal injury in fatal falls, occurring in an average of 65.67% of cases (median 71%).
- Fractures of the right and left ribs were noted at comparable rates (14.34% and 14.63%, respectively).
- Bilateral rib fractures had a mean prevalence of 33.18% (median: 37.88%), while unilateral fractures accounted for an average of 26.76% of cases (median: 25.61%).
- Sternal fractures were documented with an average prevalence of 19.49% (median, 17.3%; range, 3.3–46%).
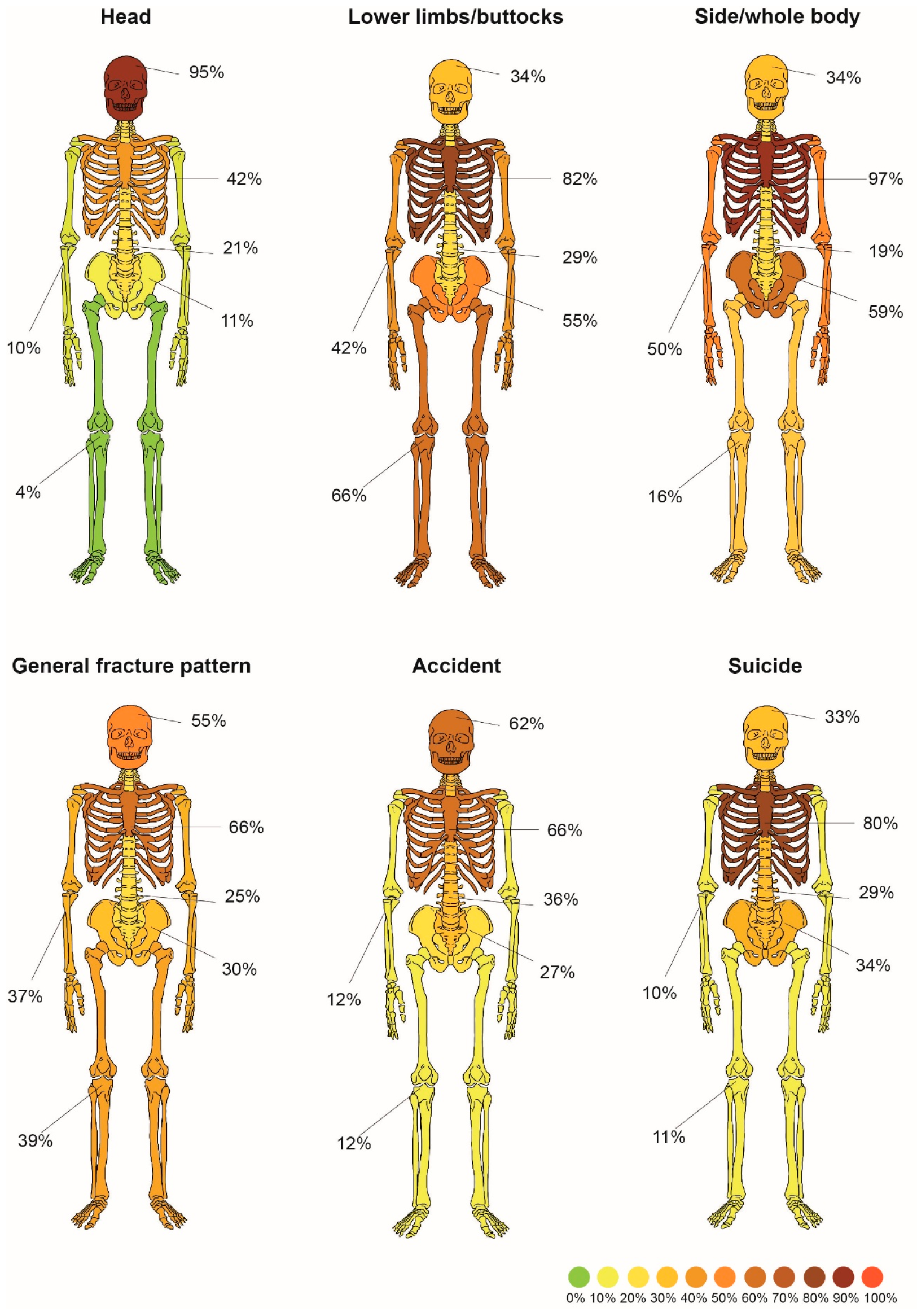
5.6. Patterns of Injury
6. PMCT Detected Fracture Frequencies
- Skull 83%
- Chest 95%
- Spine 79%
- Pelvis 83%
- Upper limbs 78%
- Lower limbs 69%
Risk of Bias Assessment
7. Discussion
7.1. Population
7.2. Toxicology
7.3. Psychiatric Disorders
7.4. Heights and Damage Profile
7.4.1. Chest
7.4.2. Skull
7.4.3. Spine
7.4.4. Pelvis
7.4.5. Upper and Lower Limbs
8. Impact Surface and Landing Position
9. Accident vs. Suicide
10. PMCT and Autopsy
11. Gaps in Knowledge
12. Limitations
13. Key Takeaways
- Fractures in FFF are dispersed throughout the entire skeleton, with a predominance in the axial skeleton.
- Males > females both in accidental and suicidal FFF.
- Variables associated with suicide: intoxication, psychiatric history.
- No definitive connection between fracture pattern and intoxication in FFF, possible correlation of cause of death and upper limb injury.
- Factors influencing fracture pattern are the height of the fall, impact surface, cause of the fall, sex.
- General fracture frequencies: chest > skull > limbs > pelvis > spine.
- There are no specific indicators that the death is accidental or suicidal, only arguments for and against those hypothesizes.
- Accident damage profile: chest > skull > spine > pelvis > limbs.
- Suicide damage profile: chest > pelvis/skull > limbs.
14. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| FFF | fatal free fall |
| BFT | blunt force trauma |
| WHO | World Health Organization |
| MVA | motor vehicle accidents |
| BMI | body mass index |
| PMCT | postmortem computed tomography |
| PE | potential energy |
| AI | artificial intelligence |
| NOS | Newcastle–Ottawa Scale |
References
- Rowbotham, S.K.; Blau, S. Skeletal fractures resulting from fatal falls: A review of the literature. Forensic Sci. Int. 2016, 266, 582.e1–582.e15. [Google Scholar] [CrossRef] [PubMed]
- Nadhim, E.A.; Hon, C.; Xia, B.; Stewart, I.; Fang, D. Falls from height in the construction industry: A critical review of the scientific literature. Int. J. Environ. Res. Public Health 2016, 13, 638. [Google Scholar] [CrossRef]
- Dong, X.S.; Largay, J.A.; Choi, S.D.; Choi, S.D.; Choi, S.D.; Romano, N. Fatal falls and PFAS use in the construction industry: Findings from the NIOSH FACE reports. Accid. Anal. Prev. 2017, 102, 136–143. [Google Scholar] [CrossRef]
- Chi, C.F.; Lin, S.Z.; Dewi, R.S. Graphical fault tree analysis for fatal falls in the construction industry. Accid. Anal. Prev. 2014, 72, 359–369. [Google Scholar] [CrossRef]
- Ramachandran, S.; Mathipa, S.; Veerakumar, K.; Krishnashree, H. Pattern of Deaths Due to Fall from Height—A Prospective Study. J. Cardiovasc. Dis. Res. 2023, 14, 3. [Google Scholar]
- Ferguson, C.; Sutherland, T. Murder by Pushing: An Exploratory Analysis of Homicidal Falls from a Height. Am. J. Forensic Med. Pathol. 2018, 39, 192–200. [Google Scholar] [CrossRef]
- Doberentz, E.; Geile, J.; Madea, B. Fatal free falls from very great heights. Rom. J. Leg. Med. 2019, 27, 354–360. [Google Scholar] [CrossRef]
- Tsai, W.-T.; Hu, C.-I.; Chang, C.-Y. Effect of Wind on Horizontal Displacement of Fatal Fall from a Height. J. Forensic Sci. 2020, 65, 255–258. [Google Scholar] [CrossRef]
- Tsai, W.-T.; Chang, C.Y.; Hu, C.I. Forensic Application of Analytical Mechanics in Fatal Fall from a Height. J. Forensic Sci. 2019, 64, 1230–1233. [Google Scholar] [CrossRef]
- Yanagida, Y.; Maeda, M.; Nushida, H.; Asano, M.; Ueno, Y. Determining falling patterns by estimation of horizontal distance and height. Int. J. Legal Med. 2011, 125, 1–10. [Google Scholar] [CrossRef]
- Içer, M.; Güloǧlu, C.; Orak, M.; Üstündaǧ, M. Yüksekten düşmelerde mortaliteyi etkileyen faktörler. Ulus. Travma Acil Cerrahi Derg. 2013, 19, 529–535. [Google Scholar]
- Chow, K.P.; Fong, D.Y.T.; Wang, M.P.; Wong, J.Y.H.; Chau, P.H. Meteorological factors to fall: A systematic review. Int. J. Biometeorol. 2018, 62, 2073–2088. [Google Scholar] [CrossRef]
- Rissep, D.; Bijnsch, A.; Schneiderb, B.; Bauer, G. Pmnsic Science Risk of Dying After a Free Fall from Height. Forensic Sci. Int. 1996, 78, 187–191. [Google Scholar] [CrossRef]
- Jones, M.D.; Cory, C.Z. A Fatal Fall from a Balcony? A Biomechanical Approach to Resolving Conflicting Witness Accounts. Med. Sci. Law 2006, 46, 233–244. [Google Scholar] [CrossRef] [PubMed]
- Tavone, A.M.; Marinelli, R.; Cazzato, F.; Piizzi, G.; Piselli, F.; Ceccobelli, G.; Giuga, G.; Vella, R.; Romaniello, N.; Oliva, A.; et al. Distinguishing injury patterns in fatal falls from heights versus pedestrian impacts: An autopsy study for differential diagnosis in ambiguous cases. Forensic Sci. Med. Pathol. 2024, 21, 665–673. [Google Scholar] [CrossRef]
- Jalalzadeh, H.; Giannakopoulos, G.F.; Berger, F.H.; Fronczek, J.; van de Goot, F.R.W.; Reijnders, U.J.; Zuidema, W.P. Post-Mortem imaging compared with autopsy in trauma victims—A systematic review. Forensic Sci. Int. 2015, 257, 29–48. [Google Scholar] [CrossRef] [PubMed]
- Chandy, P.E.; Murray, N.; Khasanova, E.; Nasir, M.U.; Nicolaou, S.; Macri, F. Postmortem CT in Trauma: An Overview. Can. Assoc. Radiol. J. 2020, 71, 403–414. [Google Scholar] [CrossRef]
- Steffen, R.; Suter, C.; Patricia, F.; Lars, O.; Michael, T.; Stephan, B. Multi-slice computed tomography (MSCT) of mountaineering casualties in the Swiss Alps—Advantages and limitations. Leg. Med. 2010, 12, 271–275. [Google Scholar] [CrossRef] [PubMed]
- Haddaway, N.R.; Page, M.J.; Pritchard, C.C.; McGuinness, L.A. PRISMA2020: An R package and Shiny app for producing PRISMA 2020-compliant flow diagrams, with interactivity for optimised digital transparency and Open Synthesis. Campbell Syst. Rev. 2022, 18, e1230. [Google Scholar] [CrossRef]
- Lau, G.; Ooi, L.; Phoon, B. Fatal Falls from a Height: The Use of Mathematical Models to Estimate the Height of Fall from the Injuries Sustained. Forensic Sci. Int. 1998, 93, 33–44. [Google Scholar] [CrossRef]
- Milaszkiewicz, A.; Cywka, T.; Teresiński, G. Weryfikacja użyteczności metody określania wysokości śmiertelnych upadków opracowanej przez Lau i wsp. Arch. Med. Sadowej Kryminol. 2019, 69, 93–99. [Google Scholar]
- Goonetilleke, U.K.D.A.; Frcpa, M. Injuries Caused by Falls from Heights. Med. Sci. Law 1980, 20, 262–275. [Google Scholar] [CrossRef]
- Lukas, G.M.; Hutton, J.E.; Lim, R.C.; Mathewson, C. Injuries Sustained from High Velocity Impact with Water. J. Trauma Inj. Infect. Crit. Care 1981, 21, 612–618. [Google Scholar] [CrossRef]
- Gupta, S.M.; Chandra, J.; Dogra, T.D. Blunt force lesions related to the height of a fall. Am. J. Forensic Med. Pathol. 1982, 3, 35–44. [Google Scholar] [CrossRef]
- Simonsen, J. Injuries sustained from high-velovity impact with water after jumps from high bridges. Am. J. Forensic Med. Pathol. 1983, 4, 139–142. [Google Scholar] [CrossRef]
- Hanzlick, R.; Masterson, K.; Walker, B. Suicide by Jumping from High-Rise Hotels. Am. J. Forensic Med. Pathol. 1990, 11, 294–297. [Google Scholar] [CrossRef] [PubMed]
- Lafave, M.; LaPorta, A.J.; Hutton, J.; Mallory, P.L. History of high-velocity impact water trauma at Letterman Army Medical Center: A 54-year experience with the Golden Gate Bridge. Mil. Med. 1995, 160, 197–199. [Google Scholar] [CrossRef] [PubMed]
- Èrsel, G.; Ëetin, C.; Gu Ènay, Y.; Fincanci, S.K.; OÈ Zdemir Kolusayin, R. Suicides by Jumping from Bosphorus Bridge in Istanbul. Forensic Sci. Int. 2001, 116, 157–162. [Google Scholar] [CrossRef]
- Goren, S.; Subasi, M.; Týrasci, Y.; Gurkan, F. Fatal falls from heights in and around Diyarbakir, Turkey. Forensic Sci. Int. 2003, 137, 37–40. [Google Scholar] [CrossRef] [PubMed]
- Türk, E.E.; Tsokos, M. Pathologic features of fatal falls from height. Am. J. Forensic Med. Pathol. 2004, 25, 194–199. [Google Scholar] [CrossRef]
- Kohli, A.; Banerjee, K.K. Pattern of injuries in fatal falls from buildings. Med. Sci. Law 2006, 46, 335–341. [Google Scholar] [CrossRef]
- Venkatesh, V.T.; Kumar, M.V.P.; Jagannatha, S.R.; Radhika, R.H.; Pushpalatha, K. Pattern of skeletal injuries in cases of falls from a height. Med. Sci. Law. 2007, 47, 330–334. [Google Scholar] [CrossRef]
- Weilemann, Y.; Thali, M.J.; Kneubuehl, B.P.; Bolliger, S.A. Correlation between skeletal trauma and energy in falls from great height detected by post-mortem multislice computed tomography (MSCT). Forensic Sci. Int. 2008, 180, 81–85. [Google Scholar] [CrossRef]
- Atanasijevic, T.C.; Popovic, V.M.; Nikolic, S.D. Characteristics of chest injury in falls from heights. Leg. Med. 2009, 11, S315–S317. [Google Scholar] [CrossRef] [PubMed]
- Behera, C.; Rautji, R.; Dogra, T.D. Fatal accidental fall from height in infants and children: A study from South Delhi. Med. Sci. Law. 2010, 50, 22–24. [Google Scholar] [CrossRef]
- Thierauf, A.; Preuß, J.; Lignitz, E.; Madea, B. Retrospective analysis of fatal falls. Forensic Sci. Int. 2010, 198, 92–96. [Google Scholar] [CrossRef] [PubMed]
- Papadopoulos, I.N.; Kanakaris, N.K.; Bonovas, S.; Konstantoudakis, G.; Petropoulou, K.; Christodoulou, S.; Kotsilianou, O.; Leukidis, C. Patients with pelvic fractures due to falls: A paradigm that contributed to autopsy-based audit of trauma in Greece. J. Trauma Manag. Outcomes 2011, 5, 2. [Google Scholar] [CrossRef]
- Petaros, A.; Slaus, M.; Coklo, M.; Sosa, I.; Cengija, M.; Bosnar, A. Retrospective analysis of free-fall fractures with regard to height and cause of fall. Forensic Sci. Int. 2013, 226, 290–295. [Google Scholar] [CrossRef] [PubMed]
- Freeman, M.D.; Eriksson, A.; Leith, W. Head and neck injury patterns in fatal falls: Epidemiologic and biomechanical considerations. J. Forensic Leg. Med. 2014, 21, 64–70. [Google Scholar] [CrossRef]
- Bruno, C.M.; Alessio, B.; Alberto, B.; Cristina, C. The injury pattern in fatal suicidal falls from a height: An. examination of 307 cases. Forensic Sci. Int. 2014, 244, 57–62. [Google Scholar] [CrossRef]
- Obeid, N.R.; Bryk, D.J.; Lee, T.; Hemmert, K.C.; Frangos, S.G.; Simon, R.J.; Pachter, H.L.; Cohen, S.M. Fatal falls in New York City: An autopsy analysis of injury patterns. Am. J. Forensic Med. Pathol. 2016, 37, 80–85. [Google Scholar] [CrossRef]
- Rao, B.V.N.M.; Badisha, R.; Mohiddin, S.K. A Study of Pattern of Injuries of Fatal Fall from Heights. Indian J. Forensic Med. Toxicol. 2016, 10, 43. [Google Scholar] [CrossRef]
- Rowbotham, S.K.; Blau, S.; Hislop-Jambrich, J.; Francis, V. Skeletal Trauma Resulting From Fatal Low (≤3 m) Free Falls: An Analysis of Fracture Patterns and Morphologies. J. Forensic Sci. 2018, 63, 1010–1020. [Google Scholar] [CrossRef]
- Abder-Rahman, H.; Jaber, M.S.O.; Al-Sabaileh, S.S. Injuries sustained in falling fatalities in relation to different distances of falls. J. Forensic Leg. Med. 2018, 54, 69–73. [Google Scholar] [CrossRef]
- Eş, H.; Şahin, M.F.; Özdemir, E. Laryngohyoid Fractures in Fatal Nonhomicidal Falls from a Height. Am. J. Forensic Med. Pathol. 2017, 38, 289–293. [Google Scholar] [CrossRef] [PubMed]
- Heimer, J.; Gascho, D.; Thali, M.J.; Schweitzer, W. Thoracic trauma in fatal falls from height—Traumatic pneumopericardium correlates with height of fall and severe injury. Forensic Sci. Med. Pathol. 2018, 14, 188–193. [Google Scholar] [CrossRef]
- Rowbotham, S.K.; Blau, S.; Hislop-Jambrich, J.; Francis, V. An Anthropological Examination of the Types of Skeletal Fractures Resulting from Fatal High (˃3 m) Free Falls. J. Forensic Sci. 2019, 64, 375–384. [Google Scholar] [CrossRef] [PubMed]
- Türkoğlu, A.; Sehlikoğlu, K.; Tokdemir, M. A study of fatal falls from height. J. Forensic Leg. Med. 2019, 61, 17–21. [Google Scholar] [CrossRef]
- Casali, M.B.; Blandino, A.; Grignaschi, S.; Florio, E.M.; Travaini, G.; Genovese, U.R. The pathological diagnosis of the height of fatal falls: A mathematical approach. Forensic Sci. Int. 2019, 302, 109883. [Google Scholar] [CrossRef] [PubMed]
- Çakı, İ.E.; Karadayı, B.; Çetin, G. Relationship of injuries detected in fatal falls with sex, body mass index, and fall height: An autopsy study. J. Forensic Leg. Med. 2021, 78, 102113. [Google Scholar] [CrossRef]
- Ramadan, A.F.; Soliman, E.M.; Abo El-Noor, M.M.; Marwa; Shahin, M.M. Patterns of Injuries in Fatal Fall from Height Cases in Gharbia Governorate: Autopsy Study. Egypt. J. Forensic Sci. Appl. Toxicol. 2020, 20, 27–42. [Google Scholar] [CrossRef]
- Tsellou, M.; Dona, A.; Antoniou, A.; Goutas, N.; Skliros, E.; Papadopoulos, I.N.; Spiliopoulou, C.; Papadodima, S.A. A comparative autopsy study of the injury distribution and severity between suicidal and accidental high falls. Forensic Sci. Med. Pathol. 2022, 18, 407–414. [Google Scholar] [CrossRef]
- Shaban Kandeel, F.; Mamdoh Azab, R. Kandeel & Azab Fatal falls from height: Pattern of injuries and effect of level of fall. Egypt. J. Forensic Sci. Appli. Toxicol. 2022, 22, 17–31. [Google Scholar]
- Chelly, S.; Mtira, A.; Gharesellaoui, S.; Hassine, M.; Jedidi, M.; Mahjoub, M.; Masmoudi, T. Fatal Falls from Great Height in Sousse (Tunisia): Study of 141 Medicolegal Autopsy Cases (Les Chutes Mortelles de Grande Hauteur Dans La Région de Sousse (Tunisie): Etude Autopsique de 141 Cas). Tunis. Med. 2023, 101, 800–804. [Google Scholar]
- Peng, T.A.; Lee, C.; Lin, J.C.; Shun, C.; Shaw, K.; I Weng, T. Fatal falls from height in Taiwan. J. Forensic Sci. 2014, 59, 978–982. [Google Scholar] [CrossRef]
- Darke, S.; Duflou, J.; Torok, M. Drugs and violent death: Comparative toxicology of homicide and non-substance toxicity suicide victims. Addiction 2009, 104, 1000–1005. [Google Scholar] [CrossRef]
- Fanton, L.; Bévalot, F.; Schoendorff, P.; Lalliard, S.; Jdeed, K.; Malicier, D. Toxicologic aspects of deaths due to falls from height. Am. J. Forensic Med. Pathol. 2007, 28, 262–266. [Google Scholar] [CrossRef]
- Wen, S.; Unuma, K.; Hanazawa, R.; Nagano, S.; Watanabe, R.; Hirakawa, A.; Uemura, K. Alcohol and toxicological factors influencing fatal falls from height in the Greater Tokyo Area: A retrospective study. Int. J. Legal Med. 2024, 138, 793–800. [Google Scholar] [CrossRef]
- Katz, K.; Gonen, N.; Goldberg, I.; Mizrahi, J.; Radwan, M.; Yosipovitch, Z. Injuries in Attempted Suicide by Jumping from a Height. Injury 1988, 19, 371–374. [Google Scholar] [CrossRef]
- Wanek, S.; Mayberry, J.C. Blunt thoracic trauma: Flail chest, pulmonary contusion, and blast injury. Crit. Care Clin. 2004, 20, 71–81. [Google Scholar] [CrossRef]
- Abel, S.M.; Ramsey, S. Patterns of skeletal trauma in suicidal bridge jumpers: A retrospective study from the southeastern United States. Forensic Sci. Int. 2013, 231, 399.e1–399.e5. [Google Scholar] [CrossRef]
- Smith, M.D.; Burrington, J.D.; Woolf, A.D. Injuries in Children Sustained in Free Falls. J. Trauma: Inj. Infect. Crit. Care 1975, 15, 987–991. [Google Scholar] [CrossRef]
- Pascoletti, G.; Catelani, D.; Conti, P.; Cianetti, F.; Zanetti, E.M. Multibody Models for the Analysis of a Fall from Height: Accident, Suicide, or Murder? Front. Bioeng. Biotechnol. 2019, 7, 419. [Google Scholar] [CrossRef]
- Mollica, P.G.; McEwen, E.C.; Hoffman, G.R. Falls from Height, Facial Injuries and Fatalities: An Institutional Review. Craniomaxillofac. Trauma Reconstr. 2022, 15, 325–331. [Google Scholar] [CrossRef]
- Gurdjian, E.S.; Webster, E.; Lissner, H.R. Radiology a monthly journal devoted to clinical radiology and allied sciences published by the radiological society of north america. Mech. Skull Fract. 1950, 54, 313–339. [Google Scholar]
- Richter, D.; Hahn, M.P.; Ostermann, P.A.W.; Ekkernkamp, A.; Muhr, G. Vertical deceleration injuries: A comparative study of the injury patterns of 101 patients after accidental and intentional high falls. Injury 1996, 27, 655–659. [Google Scholar] [CrossRef]
- Alton, T.B.; Gee, A.O. Classifications in brief: Young and Burgess classification of pelvic ring injuries. Clin. Orthop. Relat. Res. 2014, 472, 2338–2342. [Google Scholar] [CrossRef]
- Dalal, S.A.; Burgess, A.R.; Siegel, J.H.; Young, J.W.; Brumback, R.J.; Poka, A.; Dunham, C.M.; Gens, D.; Bathon, H. Pelvic fracture in multiple trauma: Classification by mechanism is key to pattern of organ injury, resuscitative requirements, and outcome. J. Trauma. 1989, 29, 981–1000; discussion 1000–1002. [Google Scholar] [CrossRef]
- Young, J.W.R.; Burgess, A.R.; Brumback, R.J.; Poka, A. Pelvic Fractures: Value of Plain Radiography in Early Assessment and Management. Radiology 1986, 160, 445–451. [Google Scholar] [CrossRef]
- Blum, L.; Hake, M.E.; Charles, R.; Conlan, T.; Rojas, D.; Martin, M.T.; Mauffrey, C. Vertical shear pelvic injury: Evaluation, management, and fixation strategies. Int. Orthop. 2018, 42, 2663–2674. [Google Scholar] [CrossRef]
- Kusior, M.E.; Pejka, K.; Knapik, M.; Sajuk, N.; Kłaptocz, S.; Konopka, T. Analysis of the nature of injuries in victims of fall from height. Arch. Med. Sadowej Kryminol. 2016, 66, 106–124. [Google Scholar] [CrossRef] [PubMed]
- Schick, S.; Heinrich, D.; Graw, M.; Aranda, R.; Ferrari, U.; Peldschus, S. Fatal falls in the elderly and the presence of proximal femur fractures. Int. J. Legal Med. 2018, 132, 1699–1712. [Google Scholar] [CrossRef]
- Kang, B.H.; Jung, K.; Huh, Y. Suicidal intent as a risk factor for mortality in high-level falls: A comparative study of suicidal and accidental falls. Clin. Exp. Emerg. Med. 2021, 8, 16–20. [Google Scholar] [CrossRef]
- Cywka, T.; Milaszkiewicz, A.; Teresiński, G. Różnicowanie samobójczych i przypadkowych upadków z wysokości z wykorzystaniem metody Teh i wsp. Arch. Med. Sadowej Kryminol. 2019, 69, 100–107. [Google Scholar]
- Terayama, T.; Toda, H.; Tanaka, Y.; Saitoh, D.; Yoshino, A. Differences in Trauma Injury Patterns and Severity Between Intentional and Accidental Falls from a Height: A Japanese Nationwide Trauma Database Study. Cureus 2022, 14, e25861. [Google Scholar] [CrossRef]
- Papadakis, S.A.; Pallis, D.; Galanakos, S.; Georgiou, D.F.; Kateros, K.; Macheras, G.; Sapkas, G. Falls from height due to accident and suicide attempt in Greece. A comparison of the injury patterns. Injury 2020, 51, 230–234. [Google Scholar] [CrossRef]
- Teresiński, G.; Cywka, T.; Milaszkiewicz, A. Evaluation of possibilities of differentiating the causes of fatal falls from a height using the Berghaus scale. Arch. Med. Sadowej Kryminol. 2016, 66, 141–148. [Google Scholar] [CrossRef][Green Version]
- Lindgren, N.; Henningsen, M.J.; Jacobsen, C.; Villa, C.; Kleiven, S.; Li, X. Prediction of skull fractures in blunt force head traumas using finite element head models. Biomech. Model. Mechanobiol. 2024, 23, 207–225. [Google Scholar] [CrossRef]
- Teh, J.; Firth, M.; Sharma, A.; Wilson, A.; Reznek, R.; Chan, O. Jumpers and fallers: A comparison of the distribution of skeletal injury. Clin. Radiol. 2003, 58, 482–486. [Google Scholar] [CrossRef]
- Berghaus, G. Mathematisch-Statistische Differenzierungsmöglichkeiten zwischen Selbstmord und Unfall bei Sturz aus der Höhe. Z. Für Rechtsmed. 1978, 80, 273–286. [Google Scholar] [CrossRef]
- Yamaguchi, T.; Hattori, S.; Mizuo, K.; Watanabe, S. Falls from high-altitude with no fatal injuries: Report of two autopsy cases. Forensic Sci. Int. Rep. 2024, 9, 100361. [Google Scholar] [CrossRef]
- Wang, Q.; Ishikawa, T.; Michiue, T.; Maeda, H. Fatal facial-intracranial impalement injury in an accidental fall from a height: An autopsy case report with a review of the literature. Forensic Sci. Int. 2010, 200, e21–e24. [Google Scholar] [CrossRef] [PubMed]
| Authors, Year, | Reported FFF with Postmortem Examination [N] | Male Victims | Female Victims | Suicidal Deaths | Male Suicidal Deaths | Female Suicidal Deaths | Accidental Deaths | Accidental Deaths Among Males | Accidental Deaths Among Females | Homicides | Unknown Cause of the Fall | Alcohol Detected | Prescribed/Resuscitation Medications | Overdose/Substance Abuse Disorder | Depresive Disorder | Schizophrenia | Other | |||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Goonetilleke et al., 1980 [22] | 146 | 73.97% (108) | 26.03% (38) | 25.2% (37) | 51.35% (19) | 48.65% (19) | 56.85% (83) | 89.16% (74) | 10.84% (9) | 0% | 17.81% (26) | U | U | U | U | 10.27% | U | U | U | U |
| Lucas et al., 1981 [23] | 100 | 56% (56) | 44% (44) | 100% (100) | 56% (56) | 44% (44) | 0% | 0% | 0% | 0% | 0% | U | U | U | U | U | U | U | U | U |
| Gupta et al., 1982 [24] | 63 | 65.8% (41) | 28.57% (18) | 42.86% (27) | 55.56% (15) | 44.44% (12) | 49.21% (31) | 83.87% (26) | 16.13% (5) | 1.59% (1) | 6.35% (4) | U | U | U | U | U | U | U | U | U |
| Simonsen et al., 1983 [25] | 10 | 70% (7) | 30% (3) | 100% (10) | 70% (7) | 30% (3) | 0% | 0% | 0% | 0% | 0% | U | U | U | U | U | U | U | U | U |
| Hanzlick et al., 1990 [26] | 14 | 78.94% (15) | 21.05% (4) | 100% (14) | 78.95% (15) | 21.05% (4) | 0% | 0% | 0% | 0% | 0% | 10.53% (2) | 10.53% (2) | U | U | U | U | U | U | U |
| MAJ Mark Lafave et al., 1995 [27] | 281 | 85% (239) | 15% (42) | 100% (281) | 85% (239) | 15% (42) | 0% | U | U | 0% | 0% | U | U | U | U | U | U | U | U | U |
| Cetin et al., 2001 [28] | 20 | 93.8% (61) | 6.2% (4) | 100% (20) | 93.8% (61) | 6.2% (4) | 0% | 0% | 0% | 0% | 0% | U | U | U | U | 20% (4) | 10% (2) | U | U | 10% (2) |
| Goren, Subasi et al., 2003 [29] | 484 | 61.2% (296) | 38.8% (188) | 11.0% (53) | 45.3% (24) | 54.7% (29) | 89.0% (431) | 63.1% (272) | 36.9% (159) | 0% | 0% | U | U | U | U | 4.55% (22) | 0.78% (3) | 2.27% (11) | 0.83% (4) | 0.78% (3) |
| Tu¨rk et al., 2004 [30] | 68 | 72.06% (49) | 27.94% (19) | 50% (34) | 56% (19) | 44% (15) | 34% (23) | 91% (21) | 9% | 0% | 16% (11) | 33.92% (23) | 14.71% (10) | 13.24% (9) | 6% (4) | 32.35% (22) | 8.82% (6) | 7.35% (5) | 1.47% (1) | 10.29% (10) |
| Kohli, Banerjee, 2006 [31] | 151 | 88.74% (134) | 11.26% (17) | U | U | U | U | U | U | U | U | U | U | U | U | U | U | U | U | U |
| Venkatesh et al., 2007 [32] | 80 | 85% (68) | 15% (12) | 3.75% (3) | U | U | 95% (76) | U | U | 1.25% (1) | U | 10% (8) | 10% (8) | U | U | 2.5% (2) | U | U | U | U |
| Weilemann et al., 2007 [33] | 20 | 55% (11) | 45% (9) | 80% (16) | 50% (8) | 50% (8) | 15% (3) | 66.33% | 33.33% | 0% | 5% (1) | U | U | U | U | U | U | U | U | U |
| Atanasijevic et al., 2009 [34] | 660 | 469 71% (469) | 29% (191) | 56% (370) | U | U | 44% (290) | U | U | 0% | 0% | U | U | U | U | U | U | U | U | U |
| Behera et al., 2010 [35] | 174 | 60.9% (106) | 39.1% (68) | 0% | 0% | 0% | 100% (174) | 60.9% (106) | 39.1% (68) | 0% | 0% | U | U | U | U | U | U | U | U | U |
| Steffen et al., 2010 [18] | 10 | 90% (9) | 10% (10) | 0% | 0% | 0% | 100% (10) | 90% (9) | 10% (1) | 0% | 0% | U | U | U | U | U | U | U | U | U |
| Thierauf et al., 2010 [36] | 123 | 81.3% (100) | 18.7% (23) | 27.64% (34) | 64.71% (22) | 35.29% (12) | 72.36% (89) | 87.64% (78) | 12.36% (11) | 0% | 0% | 24.39% (30) | 24.39% (30) | U | U | U | U | U | U | U |
| Papadopoulos et al., 2011 [37] | 970 | 64.54% (626) | 35.46% (344) | 26.5% (257) | U | U | 60.41% (586) | U | U | 0.93% (9) | 12.17% (118) | 12.58% (122) | U | U | U | U | U | U | U | U |
| Petaros et al., 2013 [38] | 179 | U | U | 54% (96) | U | U | 46% (83) | U | U | 0% | 0% | U | U | U | U | U | U | U | U | U |
| Freeman et al., 2013 [39] | 1002 | 74.3% (1210) | 25.7% (418) | 61.4% (270) | U | U | 28% (1234) | U | U | 4.5% (6) | U | U | U | U | U | U | U | U | U | U |
| Casali et al., 2014 [40] | 307 | 61% (188) | 39% (119) | U | U | U | U | U | U | U | U | U | U | U | U | U | U | U | U | U |
| Obeid et al., 2016 [41] | 423 | 76.6% (324) | 23.4% (99) | 71% (291) | U | U | 29% (119) | U | U | <1% (1) | 0% | U | U | U | U | U | U | U | U | U |
| Rao et al., 2016 [42] | 73 | 80.8% (59) | 19.2% (14) | 5.5% (4) | U | U | 94.5% (69) | U | U | 0% | 0%% | U | U | U | U | U | U | U | U | U |
| Rowbotham et al., 2017 [43] | 145 | 59% (86) | 41% (59) | 3% (4) | U | U | 97% (141) | U | U | 0% | 0% | U | U | U | U | U | U | U | U | U |
| Abder-Rahman et al., 2017 [44] | 352 | 72.7% (256) | 27.3% (96) | 8.8% (31) | U | U | 86.1% (303) | U | U | 0.6% (2) | 4.5% (16) | U | U | U | U | U | U | U | U | U |
| Eş et al., 2017 [45] | 170 | 70.6% (120) | 29.4% (50) | 30.6% (52) | U | U | 69.4% (118) | U | U | 0% | 0% | 81.18% (138) | 5.29% (9) | 2.35% (4) | 73.52% (125) | U | U | U | U | U |
| Heimer et al., 2018 [46] | 44 | 72.7% (32) | 27.3% (12) | 47.7% (21) | U | U | 22.7% (10) | U | U | 0% | 29.5% (13) | U | U | U | U | U | U | U | U | U |
| Rowbotham et al., 2018 [47] | 95 | 76.8% (73) | 23.2% (22) | 78.9% (75) | U | U | 20% (19) | U | U | 1.1% (1) | 0% | 64.21% | U | U | U | U | U | U | U | U |
| Türkoğlu et al., 2019 [48] | 213 | 67.6% (144) | 32.4% (69) | 19.2% (41) | 51.22% (21) | 48.78% (20) | 80.3% (171) | 71.35% (122) | 28.66% (49) | 0.5% (1) | 0% | 1.41% (3) | 0.94% (2) | 0.47% (1) | U | 15.02% (32) | U | 6.1% (13) | U | 8.92% (19) |
| Casali et al., 2019 [49] | 385 | 54.55% (210) | 45.45% (175) | U | U | U | U | U | U | U | U | U | U | U | U | U | U | U | U | U |
| Çakı et al.,2020 [50] | 206 | 82.5% (170) | 17.5% (36) | 11.2% (23) | 65.22% (15) | 34.78% (8) | 86.4% (178) | 85.96% (153) | 14.05% (25) | 2.4% (5) | 0% | U | U | U | U | U | U | U | U | U |
| Ramadan et al., 2020 [51] | 42 | 76.2% (32) | 23.8% (10) | 9.50% (4) | U | U | 66.7% (28) | U | U | 4.8% (2) | 9.52% (4) | 2.4% | 0% | 0% | 2.4% | 9.52% (4) | U | U | U | U |
| Tsellou et al., 2022 [52] | 261 | 73.9% (193) | 26.1% (68) | 53.6% (140) | 68.4% (96) | 31.43% (44) | 37.5% (98) | U | U | 0% | 8.9% (23) | U | U | U | U | 55.94% (146) | 2.68% (7) | 24.14% (63) | U | 31.03% (81) |
| Kandeel et al., 2022 [53] | 53 | 76.3% (39) | 26.4% (14) | 1.9% (1) | U | U | 98.1% (51) | U | U | 0% | 0% | U | U | U | U | U | U | U | U | U |
| Chelly et al., 2023 [54] | 141 | 85.8% (121) | 14.2% (20) | 13.48% (19) | 68.4% (13) | 31.6% (6) | 86.52% (122) | 73.05% (103) | 7.8% (11) | 0% | 0% | 3.55% (5) | 2.13% (3) | U | 1.42% (2) | 10.64% (15) | U | U | U | U |
| Tavone et al., 2024 [15] | 129 | U | U | U | U | U | U | U | U | U | U | U | U | U | U | U | U | U | U | U |
| Author, Year | Analyzed Heights (m) | Dominating Height Group | Nondeformable Surfaces | Deformable Surfaces | Water | Other * | PMCT Use |
|---|---|---|---|---|---|---|---|
| Goonetilleke et al., 1980 [22] | 0.76–51.82 m | 3.048–4.572 m (26.03%) | U | U | U | U | no |
| Lucas et al., 1981 [23] | 76.2–79.55 m | 76.2–79.55 m (100%) | 0% | 0% | 100% | 0% | no |
| Gupta et al., 1982 [24] | 0–27.43 m | 3.3528–6.096 m (25.43%) | 100% | 0% | 0% | 0% | no |
| Simonsen et al., 1983 [25] | 35–51 m | 30–40 m (90%) | 0% | 0% | 100% | 0% | no |
| Hanzlick et al., 1990 [26] | 18–141 m | 60–75 m (50%) * | 100% | 0% | 0% | 0% | no |
| MAJ Mark Lafave et al., 1995 [27] | 76.2–79.55 m | 76.2–79.55 m (100%) | 0% | 0% | 100% | 0% | no |
| Cetin et al., 2001 [28] | 64 m | 65 m (100%) | 0% | 0% | 100% | 0% | no |
| Goren, Subasi et al., 2003 [29] | 1–28 m | 1–5 m (50.41%) | U | U | U | U | no |
| Tu¨rk et al., 2004 [30] | 3–57 m | 6–10 m (20.59%) | U | U | U | U | no |
| Kohli, Banerjee, 2006 [31] | 3–<15 m | 3–6 m (62.9%) | U | U | U | U | no |
| Venkatesh et al., 2007 [32] | 0.6–23 m | 0–3.048 m (37.5%) | U | U | U | U | no |
| Weilemann et al., 2007 [33] | 5–70 m | 30–40 m (45%) | 100% | 0% | 0% | 0% | yes |
| Atanasijevic et al., 2009 [34] | 0–70 m | <7 m (45.61%) | 100% | 0% | 0% | 0% | no |
| Behera et al., 2010 [35] | 0.6–12 m | 5.38 m | U | U | U | U | no |
| Steffen et al., 2010 [18] | U | U | 100% | 0% | 0% | 0% | yes |
| Thierauf et al., 2010 [36] | 1.5–100 m | U | U | U | U | U | no |
| Papadopoulos et al., 2011 [37] | 1–200 m | U | U | U | U | U | no |
| Petaros et al., 2013 [38] | 1.5–101 m | 4–10 m (35.75%) | 100% | 0% | 0% | no | |
| Freeman et al., 2013 [39] | <3 m. >3 m | U | U | U | U | U | no |
| Casali et al., 2014 [40] | 3–84 m | <12 m (51.8%) | solid | no | |||
| Obeid et al., 2016 [41] | 1.83–128.02 m | 15.24 m–30.1752 m (39.72%) | U | U | U | U | no |
| Rao et al., 2016 [42] | U | U | U | U | U | U | no |
| Rowbotham et al., 2017 [43] | U | U | 99% | 1% | 0% | 0% | yes |
| Abder-Rahman et al., 2017 [44] | 1.5–15 m | >9 m (38.6%) | U | U | U | U | no |
| Eş et al., 2017 [45] | 3–60 m | U | U | U | U | U | no |
| Heimer et al., 2018 [46] | 3.3 m-70 m | 3–10 m (36.36%) = 20–70 m (36.36%) | 100% | 0% | 0% | 0% | yes |
| Rowbotham et al., 2018 [47] | >3–>51 m | 3–25 m (51.6%) | 86.3% | 13.7% | 0% | 0% | yes |
| Türkoğlu et al., 2019 [48] | <5 m >5 m | <5 m (52.6%) | U | U | U | U | no |
| Casali et al., 2019 [49] | <6 m–36 m | equinumerous groups | 100% | 0% | 0% | no | |
| Çakı et al., 2020 [50] | 8.2 m ± 0.7 m | U | U | U | U | U | no |
| Ramadan et al., 2020 [51] | <6.01 m >6.01 m | >6.01 m (78.6%) | U | U | U | U | no |
| Tsellou et al., 2022 [52] | 9.35 ± 7.35 m | U | U | U | U | U | no |
| Kandeel et al., 2022 [53] | <6 m >6 m | >6 m (56.6%) | U | U | U | U | no |
| Chelly et al., 2023 [54] | 3–>15 m | 3–6 m (41.8) | 77.30% | 0% | 0.00% | 22.7% | no |
| Tavone et al., 2024 [15] | U | U | U | U | U | U | no |
| Study | Design | N | PMCT_Used | NOS_Selection_(0–4) | NOS_Comparability_(0–2) | NOS_Outcome_(0–3) | NOS_Total_(0–9) | Overall_Risk_of_Bias |
|---|---|---|---|---|---|---|---|---|
| Goonetilleke et al. (1980) [22] | Retrospective autopsy series | 146 | No | 2 | 2 | 2 | 6 | Moderate |
| Lucas et al. (1981) [23] | Retrospective autopsy series | 100 | No | 2 | 2 | 2 | 6 | Moderate |
| Gupta et al. (1982) [24] | Retrospective autopsy series | 63 | No | 2 | 2 | 1 | 5 | Moderate |
| Simonsen et al. (1983) [25] | Retrospective autopsy series | 10 | No | 2 | 2 | 1 | 5 | Moderate |
| Hanzlick et al. (1990) [26] | Retrospective autopsy series | 14 | No | 2 | 2 | 1 | 5 | Moderate |
| Lafave et al. (1995) [27] | Retrospective autopsy series | 281 | No | 3 | 2 | 2 | 7 | Low |
| Cetin et al. (2001) [28] | Retrospective autopsy series | 20 | No | 2 | 2 | 1 | 5 | Moderate |
| Goren et al. (2003) [29] | Retrospective autopsy series | 484 | No | 3 | 2 | 2 | 7 | Low |
| Türk & Tsokos (2004) [30] | Retrospective autopsy series | 68 | No | 2 | 2 | 1 | 5 | Moderate |
| Kohli & Banerjee (2006) [31] | Retrospective autopsy series | 151 | No | 2 | 2 | 2 | 6 | Moderate |
| Venkatesh et al. (2007) [32] | Retrospective autopsy series | 80 | No | 2 | 2 | 1 | 5 | Moderate |
| Weilemann et al. (2007) [33] | Retrospective autopsy series with PMCT | 20 | Yes | 2 | 2 | 1 | 5 | Moderate |
| Atanasijevic et al. (2009) [34] | Retrospective autopsy series | 660 | No | 3 | 2 | 2 | 7 | Low |
| Behera et al. (2010) [35] | Retrospective autopsy series | 174 | No | 2 | 2 | 2 | 6 | Moderate |
| Steffen et al. (2010) [18] | Retrospective autopsy series with PMCT | 10 | Yes | 2 | 2 | 1 | 5 | Moderate |
| Thierauf et al. (2010) [36] | Retrospective autopsy series | 123 | No | 2 | 2 | 2 | 6 | Moderate |
| Papadopoulos et al. (2011) [37] | Retrospective autopsy series | 970 | No | 3 | 2 | 2 | 7 | Low |
| Petaros et al. (2013) [38] | Retrospective autopsy series | 179 | No | 2 | 2 | 2 | 6 | Moderate |
| Freeman et al. (2013) [39] | Retrospective autopsy series | 1002 | No | 3 | 2 | 2 | 7 | Low |
| Casali/Bruno et al. (2014) [40] | Retrospective autopsy series | 307 | No | 3 | 2 | 2 | 7 | Low |
| Obeid et al. (2016) [41] | Retrospective autopsy series | 423 | No | 3 | 2 | 2 | 7 | Low |
| Rao et al. (2016) [42] | Retrospective autopsy series | 73 | No | 2 | 2 | 1 | 5 | Moderate |
| Rowbotham et al. (2017) [43] | Retrospective autopsy series with PMCT | 145 | Yes | 2 | 2 | 2 | 6 | Moderate |
| Abder-Rahman et al. (2017) [44] | Retrospective autopsy series | 352 | No | 3 | 2 | 2 | 7 | Low |
| Eş et al. (2017) [45] | Retrospective autopsy series | 170 | No | 2 | 2 | 2 | 6 | Moderate |
| Heimer et al. (2018) [46] | Retrospective autopsy series with PMCT | 44 | Yes | 2 | 2 | 1 | 5 | Moderate |
| Rowbotham et al. (2018) [47] | Retrospective autopsy series with PMCT | 95 | Yes | 2 | 2 | 1 | 5 | Moderate |
| Türkoğlu et al. (2019) [48] | Retrospective autopsy series | 213 | No | 3 | 2 | 2 | 7 | Low |
| Casali et al. (2019) [49] | Retrospective autopsy series | 385 | No | 3 | 2 | 2 | 7 | Low |
| Çakı et al. (2020) [50] | Retrospective autopsy series | 206 | No | 3 | 2 | 2 | 7 | Low |
| Ramadan et al. (2020) [51] | Retrospective autopsy series | 42 | No | 2 | 2 | 1 | 5 | Moderate |
| Tsellou et al. (2022) [52] | Retrospective autopsy series | 261 | No | 3 | 2 | 2 | 7 | Low |
| Kandeel & Azab (2022) [53] | Retrospective autopsy series | 53 | No | 2 | 2 | 1 | 5 | Moderate |
| Chelly et al. (2023) [54] | Retrospective autopsy series | 141 | No | 2 | 2 | 2 | 6 | Moderate |
| Tavone et al. (2024) [18] | Retrospective autopsy series | 129 | No | 2 | 2 | 2 | 6 | Moderate |
| Argument | Accident | Suicide | Citation |
|---|---|---|---|
| Intoxication | - | + | [30,45,47,57] |
| Psychiatric history | - | + | [22,29,41,52] |
| High altitude | - | + | [29,32,37,47,52] |
| More severe, multifocal injuries | - | + | [38,47] |
| Feet/buttocks first impact | - | + | [47,54] |
| Side/whole body/headfirst impact | + | - | [33] |
| Fracture pattern: Chest > Skull > Spine > pelvis > limbs | + | - | [18,23,25,27,38,41,50,52] |
| Fracture pattern: Chest > pelvis/skull > limbs | - | + | [18,23,25,27,38,41,50,52] |
| Pelvis fractured | - | + | [37,38] |
| Bilateral lower limb fractures | - | + | [47,54] |
| Bilateral upper limb fractures | - | + | [38,47] |
| Severe bilateral chest fractures | - | + | [38,47] |
| Skeleton Part | PMCT | Autopsy |
|---|---|---|
| Skull | 83% | 53% |
| Chest | 95% | 62% |
| Spine | 79% | 19% |
| Pelvis | 83% | 24% |
| Upper limbs | 78% | 21% |
| Lower limbs | 69% | 28% |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Woliński, F.; Kraśnik, K.; Bryliński, Ł.; Sado, J.; Sagan, J.; Brylińska, K.; Teresiński, G.; Cywka, T.; Karpiński, R.; Baj, J. Fracture Patterns in Fatal Free Falls: A Systematic Review of Intrinsic and Extrinsic Risk Factors and the Role of Postmortem CT. J. Clin. Med. 2025, 14, 6305. https://doi.org/10.3390/jcm14176305
Woliński F, Kraśnik K, Bryliński Ł, Sado J, Sagan J, Brylińska K, Teresiński G, Cywka T, Karpiński R, Baj J. Fracture Patterns in Fatal Free Falls: A Systematic Review of Intrinsic and Extrinsic Risk Factors and the Role of Postmortem CT. Journal of Clinical Medicine. 2025; 14(17):6305. https://doi.org/10.3390/jcm14176305
Chicago/Turabian StyleWoliński, Filip, Kacper Kraśnik, Łukasz Bryliński, Jolanta Sado, Justyna Sagan, Katarzyna Brylińska, Grzegorz Teresiński, Tomasz Cywka, Robert Karpiński, and Jacek Baj. 2025. "Fracture Patterns in Fatal Free Falls: A Systematic Review of Intrinsic and Extrinsic Risk Factors and the Role of Postmortem CT" Journal of Clinical Medicine 14, no. 17: 6305. https://doi.org/10.3390/jcm14176305
APA StyleWoliński, F., Kraśnik, K., Bryliński, Ł., Sado, J., Sagan, J., Brylińska, K., Teresiński, G., Cywka, T., Karpiński, R., & Baj, J. (2025). Fracture Patterns in Fatal Free Falls: A Systematic Review of Intrinsic and Extrinsic Risk Factors and the Role of Postmortem CT. Journal of Clinical Medicine, 14(17), 6305. https://doi.org/10.3390/jcm14176305







