Traumatic Bilateral Lumbosacral Jumped Facet Without Fracture in Childhood: Case Report and Systematic Review
Abstract
1. Introduction
1.1. Epidemiology
1.2. Anatomy and Biomechanics
1.3. Mechanism of Trauma
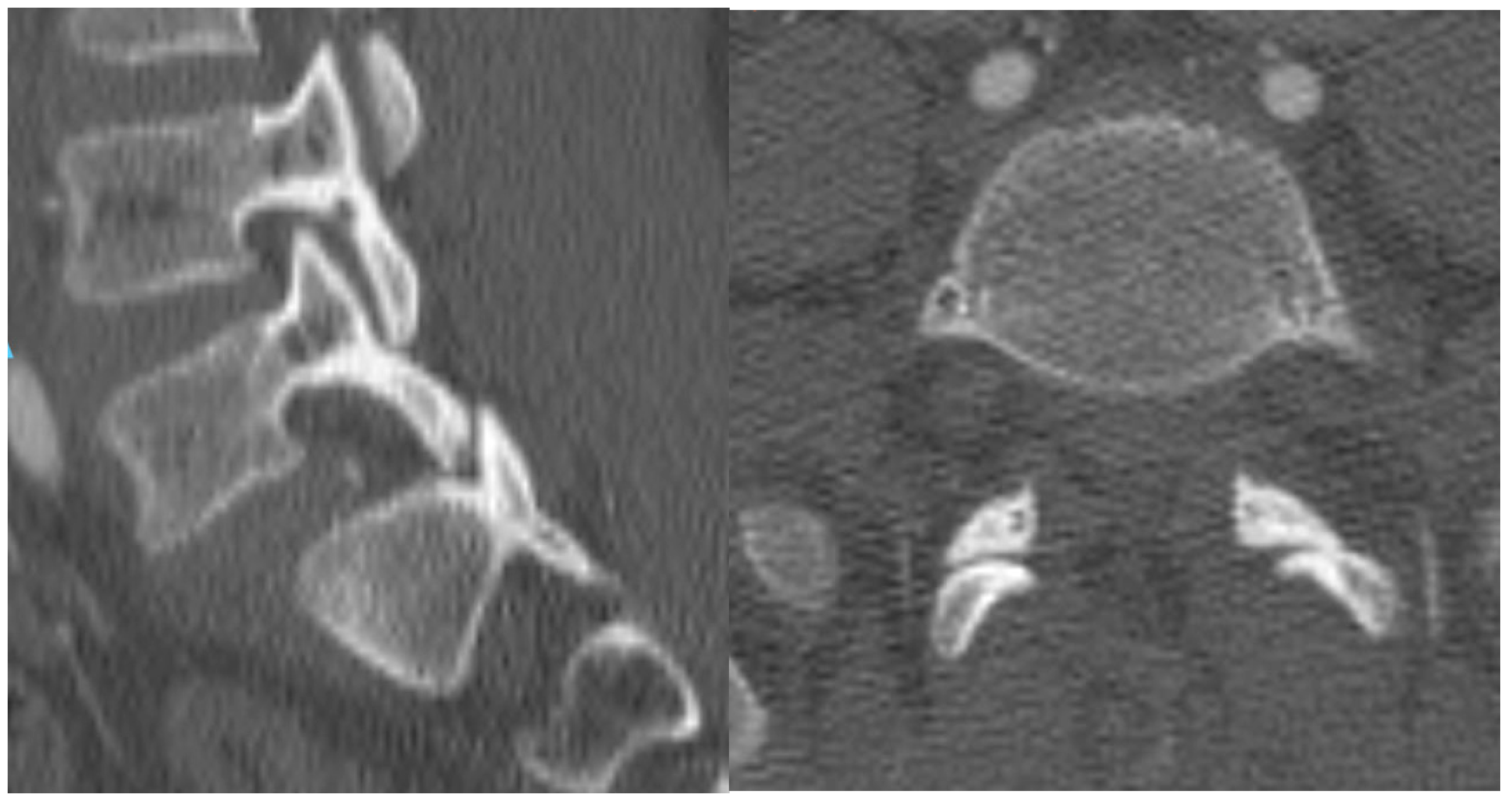
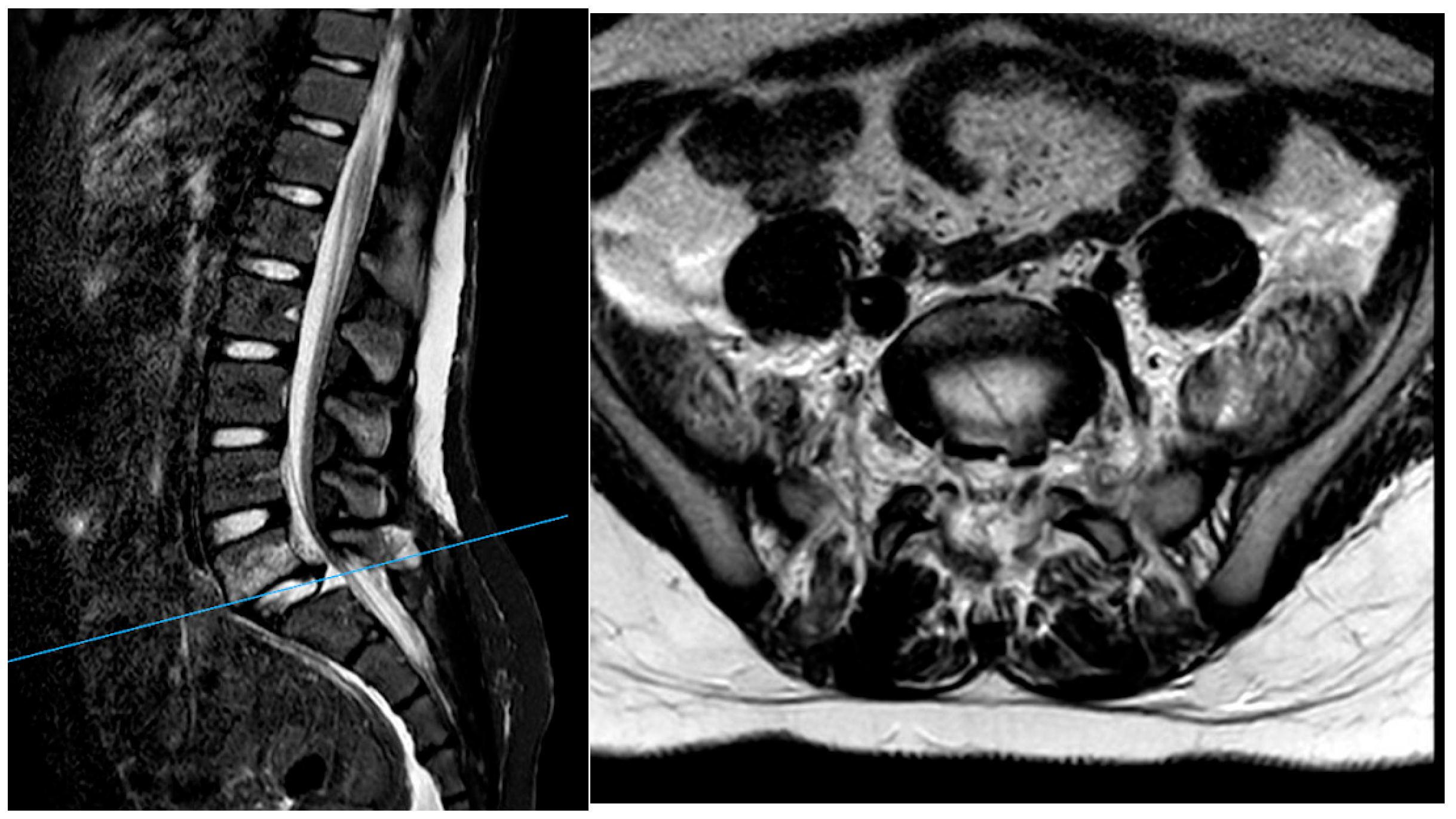
1.4. Radiological Findings
1.5. Clinical Presentation
1.6. Management
2. Materials and Methods
2.1. Study Setting and Search Strategy
2.2. Inclusion and Exclusion Criteria
2.3. Data Extraction and Analysis
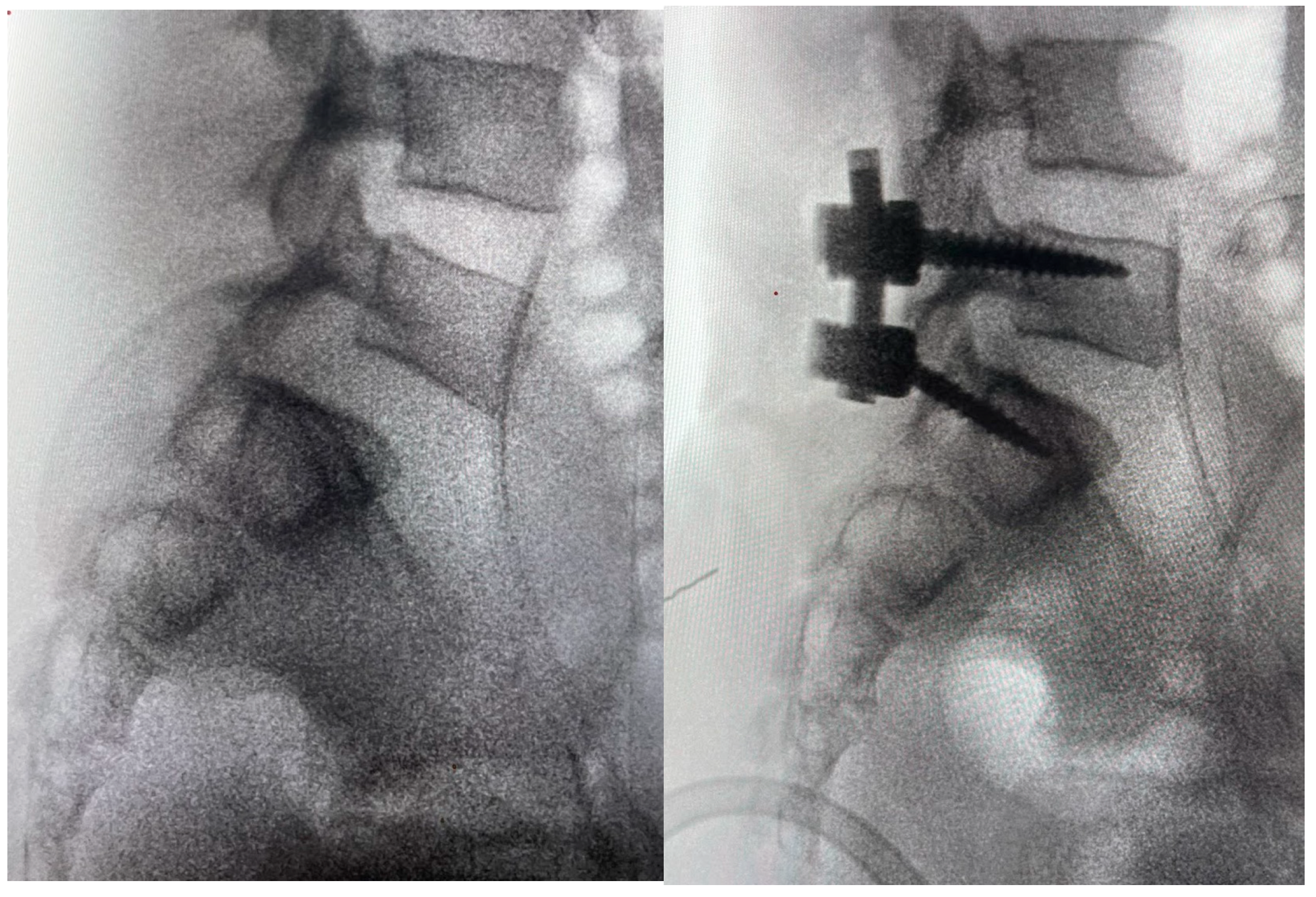
3. Case Report
4. Results
4.1. Demographic and Clinical Characteristics
4.2. Injury Patterns and Neurological Status
4.3. Surgical Management and Clinical Outcomes
4.4. Radiological and Functional Outcomes
5. Discussion
6. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Jaumard, N.V.; Welch, W.C.; Winkelstein, B.A. Spinal facet joint biomechanics and mechanotransduction in normal, injury and degenerative conditions. J. Biomech. Eng. 2011, 133, 071010. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Kwee, R.M.; Kwee, T.C. Imaging of facet joint diseases. Clin. Imaging. 2021, 80, 167–179. [Google Scholar] [CrossRef] [PubMed]
- Moon, A.S.; Atesok, K.; Niemeier, T.E.; Manoharan, S.R.; Pittman, J.L.; Theiss, S.M. Traumatic Lumbosacral Dislocation: Current Concepts in Diagnosis and Management. Adv. Orthop. 2018, 2018, 6578097. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Konan, L.M.; Davis, D.D.; Mesfin, F.B. Traumatic Lumbar Spondylolisthesis. In StatPearls [Internet]; StatPearls Publishing: Treasure Island, FL, USA, 2024. [Google Scholar] [PubMed]
- Ver, M.L.P.; Dimar, J.R.; Carreon, L.Y. Traumatic Lumbar Spondylolisthesis: A Systematic Review and Case Series. Glob. Spine J. 2019, 9, 767–782. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Cho, N.; Alkins, R.; Khan, O.H.; Ginsberg, H.; Cusimano, M.D. Unilateral Lumbar Facet Dislocation: Case Report and Review of the Literature. World Neurosurg. 2019, 123, 310–316. [Google Scholar] [CrossRef] [PubMed]
- Ra, I.H.; Min, W.K. Traumatic bilateral facet dislocation of lumbar spine: “double facet sign”. Spine J. 2013, 13, 1705–1707. [Google Scholar] [CrossRef] [PubMed]
- Watson-Jones, R. Fractures and Other Bone and Joint Injuries, 2nd ed.; Williams & Wilkins: Baltimore, MD, USA, 1941. [Google Scholar]
- Wiltse, L.L.; Newman, P.H.; Macnab, I. Classification of spondylolisis and spondylolisthesis. Clin. Orthop. Relat. Res. 1976, 117, 23–29. [Google Scholar] [CrossRef]
- Fabris, D.; Costantini, S.; Nena, U.; Lo Scalzo, V. Traumatic L5-S1 spondylolisthesis: Report of three cases and a review of the literature. Eur. Spine J. 1999, 8, 290–295. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Tsirikos, A.I.; Saifuddin, A.; Noordeen, M.H.; Tucker, S.K. Traumatic lumbosacral dislocation: Report of two cases. Spine 2004, 29, E164–E168. [Google Scholar] [CrossRef] [PubMed]
- Zenonos, G.A.; Agarwal, N.; Monaco, E.A.; Okonkwo, D.O.; Kanter, A.S. Traumatic L4–5 bilateral locked facet joints. Eur. Spine J. 2016, 25 (Suppl. S1), 129–133. [Google Scholar] [CrossRef]
- Szentirmai, O.; Seinfeld, J.; Beauchamp, K.; Patel, V. Traumatic unilateral lumbosacral jumped facet without fracture in a child. Patient Saf. Surg. 2008, 2, 29. [Google Scholar] [CrossRef][Green Version]
- Yamaki, V.N.; Morais, B.A.; Brock, R.S.; Paiva, W.S.; de Andrade, A.F.; Teixeira, M.J. Traumatic lumbosacral spondyloptosis in a pediatric patient: Case report and literature review. Pediatr. Neurosurg. 2018, 53, 263–269. [Google Scholar] [CrossRef] [PubMed]
- Mishra, A.; Agrawal, D.; Gupta, D.; Sinha, S.; Satyarthee, G.D.; Singh, P.K. Traumatic spondyloptosis: A series of 20 patients. J. Neurosurg. Spine 2015, 22, 647–652. [Google Scholar] [CrossRef] [PubMed]
- Esteves, A.; Gouveia, D.; Lixa, J.; Pinho, A.; Sousa, A. Traumatic Spondylolisthesis of L5-S1 in a Pediatric Age: A Rarely Described Injury. Cureus 2024, 16, e69674. [Google Scholar] [CrossRef]
- Villarreal-Arroyo, M.; Mejía-Herrera, J.C. Inveterate unilateral lumbosacral dislocation in children. Case report and literature review. Acta Ortop. Mex. 2011, 25, 227–231. [Google Scholar]
- Chandrashekhara, S.H.; Kumar, A.; Gamanagatti, S.; Kapoor, K.; Mukund, A.; Aggarwal, D.; Sinha, S. Erratum to: Unusual traumatic spondyloptosis causing complete transection of spinal cord. Int. Orthop. 2017, 41, 1285. [Google Scholar] [CrossRef]
- Yang, X.; Kong, Q.; Dou, Q.; Song, Y. Traumatic high-grade L5–S1 spondylolisthesis with vertebral physeal injury. Spine J. 2015, 15, 2097–2098. [Google Scholar] [CrossRef]
- Rodrigues, L.M.; Valesin, E.S.; Pohl, P.H.I.; Milani, C. Traumatic L5–S1 spondylolisthesis in a 15-year-old. J. Pediatr. Orthop. B 2013, 22, 420–423. [Google Scholar] [CrossRef] [PubMed]
- Verhelst, L.; Ackerman, P.; Van Meirhaeghe, J. Traumatic posterior lumbosacral spondyloptosis in a six-year-old: Case report and literature review. Spine 2009, 34, E629–E634. [Google Scholar] [CrossRef]
- Yazici, M.; Alanay, A.; Aksoy, M.C.; Acaroglu, E.; Surat, A. Traumatic L1–L2 dislocation without fracture in a six-year-old girl. Spine 1999, 24, 1483–1486. [Google Scholar] [CrossRef]
- Abdel-Fattah, F.H.; Rizik, A.H. Complete fracture-dislocation of the lower lumbar spine with spontaneous neurologic decompression. Clin. Orthop. Relat. Res. 1990, 251, 140–143. [Google Scholar] [CrossRef]
- Dogan, S.; Safavi-Abbasi, S.; Theodore, N.; Chang, S.W.; Horn, E.M.; Mariwalla, N.R.; Rekate, H.L.; Sonntag, V.K. Thoracolumbar and sacral spinal injuries in children and adolescents: A review of 89 cases. J. Neurosurg. 2007, 106, 426–433. [Google Scholar] [CrossRef]
- Denis, F. The three column spine and its significance. The classification of acute thoracolumbar spinal injuries. Spine 1983, 8, 817–831. [Google Scholar] [CrossRef] [PubMed]
- Sekhon, L.H.; Sears, W.; Lynch, J.J. Surgical management of traumatic thoracic spondyloptosis: Review of 2 cases. J. Clin. Neurosci. 2007, 14, 770–775. [Google Scholar] [CrossRef] [PubMed]
- Aihara, T.; Takahashi, K.; Yamagata, M.; Moriya, H. Fracture-dislocation of the fifth lumbar vertebra. A new classification. J. Bone Joint. Surg. Br. 1998, 80, 840–845. [Google Scholar] [CrossRef]
- Cebesoy, O.; Kose, K.C.; Yazar, T. The healing potential in cauda equina syndrome secondary to traumatic posterior L5–S1 dislocation. A case report with 16 years follow-up. Acta. Orthop. Belg. 2007, 73, 408–412. [Google Scholar]
- Dewey, P.; Browne, P.S.H. Fracture–dislocation of the lumbo-sacral spine with cauda equina lesion: Report of two cases. J. Bone Joint. Surg. Br. 1968, 50, 635–638. [Google Scholar] [CrossRef] [PubMed]
- Bhenderu, L.S.S.; Lyon, K.A.; Richardson, W.T.; Desai, R.; Kriel, H.H.; Rahm, M.D. Treatment of unilateral L5-S1 locked facet in a pediatric patient. Surg. Neurol. Int. 2023, 14, 133. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Łosiński, K.; Bryndal, A.; Grochulska, A.; Nawos-Wysocki, W.; Glowinski, S. Assessment of lumbosacral spinal curvatures before and after surgery using 3D posturography. Sci. Rep. 2025, 15, 16126. [Google Scholar] [CrossRef]


| Name, Year | Sex | Age | Trauma | Other Lesion | Level | Approach | Treatment | ASIA | ASIA Post | Treatment Outcome |
|---|---|---|---|---|---|---|---|---|---|---|
| Vetter SY, 2015 [13] | M | 12 | buried beneath a wall | open fracture left distal fibula, epiphysiolysis distal tibia. | L5–S1 | Posterior | closed reduction + percutaneo viti e barre | E | E | no deficit |
| Yamaki VN, 2018 [14] | F | 4 | buried beneath a wall | L5–S1 | ant + post | D | D | able to walk independently, despite a persistent left foot drop | ||
| Mishra A, 2015 [15] | M | 16 | fall from height | bilat pneumothorax | T4–5 | posterior | T3–T5 laminectomy and T3–T6 PSF | A | A | no improvement |
| Mishra A, 2015 [15] | M | 12 | crushing accident | L4–L5 | posterior | L2–L5 PSF pedicle screw fixation | A | A | no improvement and development lumbar ernia | |
| Mishra A, 2015 [15] | M | 18 | fall from height | T9 compression fracture | L1–L2 | post + ant | L2 corpectomy + L3–L4 PSF | A | A | death |
| Esteves A, 2024 [16] | M | 5 | direct trauma to the lumbar spine (heavy object) | with L5 isthmic fractures and a sacral fracture | L5–S1 | posterior | open reduction of the L5–S1 facet joint dislocation associated with posterior lumbopelvic fixation (L4-iliac) | E | E | no neurological deficits |
| Villarreal-Arroyo M, 2011 [17] | F | 8 | traumatic | none | L5–S1 | posterolateral | pedicle scree fixation L4-S1 | E | E | no neurologigal deficit |
| Chandrashekhara SH 2011 [18] | M | 10 | fell from a running truck and was run over by the tractor-plough a | fracture of L3, disruption of articular facets | L4–L5 | Posterior | L2, L3, L4, L5 pedicle screw and rod fixation | A | B | paraplegia mild improvement |
| Chandrashekhara SH 2011 [18] | M | 16 | traumatic motor vehicle crash | L2–L3–L4 | Post + ant | vertebrectomy L3 + posterior L1–L5 | A | A | ||
| Yang X, 2015 [19] | F | 11 | crushed under a collapsed beam | transverse process fracture (L1–L5 in right) | L5–S1 | posterolateral | L5–S1 laminectomy, reduction, posterolateral fusion | D | E | No neurological deficit |
| Rodrigues LM, 2015 [20] | M | 15 | buried beneath a wall | L5–S1 | post + ante | pedicle fixation and an anterior cage | C | D | PRE: bilaterally decreased muscle strength was observed POST: significant recovery of muscle strength in the lower limbs | |
| Verhelst L, 2009 [21] | M | 6 | hit by a tractor | perineal breach, several hepatic lacerations, Morel-Lavalle’e lesion over the left hip and gluteal area | L5–S1 | posterior | L3-S2 pedicle screw fixation and posterolateral grafting. | A | A | complete loss of perineal sensation and loss of anal sphincter tone were found |
| M Yazici, 1999 [22] | F | 6 | traumatic | L1–L2 | Posterior | modified Luque frame with sublaminar wires. | C | E | pre: incomplete paraplegia post: no neurologic deficit | |
| H Abdel-Fattah, 1990 [23] | M | 18 | traumatic | L4–L5 | Posterior | Open reduction and internal fixation with a sacral rod and two Harrington rods | E | E | neurologically intact |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Borruto, M.I.; Pomponi, M.; Velluto, C.; Marciano, A.; Proietti, L.; Scaramuzzo, L. Traumatic Bilateral Lumbosacral Jumped Facet Without Fracture in Childhood: Case Report and Systematic Review. J. Clin. Med. 2025, 14, 6228. https://doi.org/10.3390/jcm14176228
Borruto MI, Pomponi M, Velluto C, Marciano A, Proietti L, Scaramuzzo L. Traumatic Bilateral Lumbosacral Jumped Facet Without Fracture in Childhood: Case Report and Systematic Review. Journal of Clinical Medicine. 2025; 14(17):6228. https://doi.org/10.3390/jcm14176228
Chicago/Turabian StyleBorruto, Maria Ilaria, Michele Pomponi, Calogero Velluto, Achille Marciano, Luca Proietti, and Laura Scaramuzzo. 2025. "Traumatic Bilateral Lumbosacral Jumped Facet Without Fracture in Childhood: Case Report and Systematic Review" Journal of Clinical Medicine 14, no. 17: 6228. https://doi.org/10.3390/jcm14176228
APA StyleBorruto, M. I., Pomponi, M., Velluto, C., Marciano, A., Proietti, L., & Scaramuzzo, L. (2025). Traumatic Bilateral Lumbosacral Jumped Facet Without Fracture in Childhood: Case Report and Systematic Review. Journal of Clinical Medicine, 14(17), 6228. https://doi.org/10.3390/jcm14176228








