Use of Lipid-Lowering Treatment in Primary Prevention in Spain (Lipidspain)
Abstract
1. Introduction
2. Material and Methods
2.1. Contextualization, Data Request and Eligibility Criteria
2.2. Study Variables
2.3. Statistical Analyses
3. Results
4. Discussion
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- INEbase. Estadística de Defunciones Según La Causa de Muerte. Últimos Datos. Available online: https://www.ine.es/dyngs/INEbase/es/operacion.htm?c=Estadistica_C&cid=1254736176780&menu=ultiDatos&idp=1254735573175 (accessed on 24 November 2024).
- Pedro-Botet, J.; Plana, N.; Mostaza, J.M.; Gómez-Doblas, J.J.; Fernández Olmo, M.R.; Escobar Cervantes, C.; Díaz-Díaz, J.L.; Campuzano Ruiz, R.; Valdivielso, P.; Cosín-Sales, J. Control de La Hipercolesterolemia En España: Una Misma Situación Con Diferentes Realidades Autonómicas. Clín. Investig. Arterioscler. 2023, 35, 219–225. [Google Scholar] [CrossRef]
- Cosín-Sales, J.; Campuzano Ruiz, R.; Díaz Díaz, J.L.; Escobar Cervantes, C.; Fernández Olmo, M.R.; Gómez-Doblas, J.J.; Mostaza, J.M.; Pedro-Botet, J.; Plana Gil, N.; Valdivielso, P. Dyslipidemia Observatory: Treatment of Hypercholesterolemia in Spain, Context and Levers for Improvement in Clinical Practice. Clín. Investig. Arterioscler. 2022, 34, 253–260. [Google Scholar] [CrossRef] [PubMed]
- Nuotio, J.; Vähämurto, L.; Pahkala, K.; Magnussen, C.G.; Hutri-Kähönen, N.; Kähönen, M.; Laitinen, T.; Taittonen, L.; Tossavainen, P.; Lehtimäki, T.; et al. CVD Risk Factors and Surrogate Markers—Urban-Rural Differences. Scand. J. Public Health 2020, 48, 752–761. [Google Scholar] [CrossRef] [PubMed]
- Studziński, K.; Tomasik, T.; Windak, A.; Banach, M.; Wójtowicz, E.; Mastej, M.; Tomaszewski, M.; Mikhailidis, D.P.; Toth, P.P.; Catapano, A.; et al. The Differences in the Prevalence of Cardiovascular Disease, Its Risk Factors, and Achievement of Therapeutic Goals among Urban and Rural Primary Care Patients in Poland: Results from the LIPIDOGRAM 2015 Study. J. Clin. Med. 2021, 10, 5656. [Google Scholar] [CrossRef] [PubMed]
- Pedro-Botet, J.; Climent, E.; Giralt Martínez, E.; Flores-Le Roux, J.A. Mapa de Recursos y Necesidades Asistenciales Del Paciente Dislipidémico En España: Estudio MADI. Clín. Investig. Arterioscler. 2016, 28, 257–264. [Google Scholar] [CrossRef]
- Ministerio de Sanidad. Sanidad en Datos. Base de Datos Clínicos de Atención Primaria—BDCAP. Available online: https://www.sanidad.gob.es/estadEstudios/estadisticas/estadisticas/estMinisterio/SIAP/home.htm (accessed on 29 March 2025).
- Gencer, B.; Marston, N.A.; Im, K.; Cannon, C.P.; Sever, P.; Keech, A.; Braunwald, E.; Giugliano, R.P.; Sabatine, M.S. Efficacy and Safety of Lowering LDL Cholesterol in Older Patients: A Systematic Review and Meta-Analysis of Randomised Controlled Trials. Lancet 2020, 396, 1637–1643. [Google Scholar] [CrossRef]
- Nanna, M.G.; Wang, T.Y.; Xiang, Q.; Goldberg, A.C.; Robinson, J.G.; Roger, V.L.; Virani, S.S.; Wilson, P.W.F.; Louie, M.J.; Koren, A.; et al. Sex Differences in the Use of Statins in Community Practice. Circ. Cardiovasc. Qual. Outcomes 2019, 12, e005562. [Google Scholar] [CrossRef]
- Karalis, D.G.; Wild, R.A.; Maki, K.C.; Gaskins, R.; Jacobson, T.A.; Sponseller, C.A.; Cohen, J.D. Gender Differences in Side Effects and Attitudes Regarding Statin Use in the Understanding Statin Use in America and Gaps in Patient Education (USAGE) Study. J. Clin. Lipidol. 2016, 10, 833–841. [Google Scholar] [CrossRef]
- Carr, M.C. The Emergence of the Metabolic Syndrome with Menopause. J. Clin. Endocrinol. Metab. 2003, 88, 2404–2411. [Google Scholar] [CrossRef]
- Matthews, K.A.; Meilahn, E.; Kuller, L.H.; Kelsey, S.F.; Caggiula, A.W.; Wing, R.R. Menopause and Risk Factors for Coronary Heart Disease. N. Engl. J. Med. 1989, 321, 641–646. [Google Scholar] [CrossRef]
- Zhang, X.; Ji, L.; Ran, X.; Su, B.; Ji, Q.; Hu, D. Gender Disparities in Lipid Goal Attainment among Type 2 Diabetes Outpatients with Coronary Heart Disease: Results from the CCMR-3B Study. Sci. Rep. 2017, 7, 12648. [Google Scholar] [CrossRef]
- Lee, S.-Y.; Lee, S.; Lee, W. Association between Medication Adherence to Chronic Diseases and Shift-Work Schedules in the Korean Working Population. Sci. Rep. 2022, 12, 22595. [Google Scholar] [CrossRef]
- Suero-Abreu, G.A.; Karatasakis, A.; Rashid, S.; Tysarowski, M.; Douglas, A.; Patel, R.; Siddiqui, E.; Bhardwaj, A.; Gerula, C.M.; Matassa, D. Factors Associated with Disparities in Appropriate Statin Therapy in an Outpatient Inner City Population. Healthcare 2020, 8, 361. [Google Scholar] [CrossRef]
- Maria, M.-S.; Silvia, A.-N.; Beatriz, D.G.; Andrew, D.; Guillermo, P.-F. Health Care in Rural Areas: Proposal of a New Telemedicine Program Assisted from the Reference Health Centers, for a Sustainable Digitization and Its Contribution to the Carbon Footprint Reduction. Heliyon 2022, 8, e09812. [Google Scholar] [CrossRef]
- Gabriel, R.; Saiz, C.; Susi, R.; Alonso, M.; Vega, S.; López, I.; Cruz Cardenal, M.M.; Antonio Gómez-Gerique, J.; Porres, A.; Muñiz, J. Epidemiología Del Perfil Lipídico de La Población Anciana Española: El Estudio EPICARDIAN. Med. Clin. 2004, 122, 605–609. [Google Scholar] [CrossRef]
- Argimon, J.M.; Bengoa, R.; López-Casanovas, G. Value-Based Healthcare in Spain Regional Experimentation in a Shared Governance Setting. A Report; The Economist Intelligence Unit: London, UK, 2015. [Google Scholar]
- Mach, F.; Baigent, C.; Catapano, A.L.; Koskina, K.C.; Casula, M.; Badimon, L.; Chapman, M.J.; De Backer, G.G.; Delgado, V.; Ference, B.A.; et al. 2019 ESC/EAS Guidelines for the Management of Dyslipidaemias: Lipid Modification to Reduce Cardiovascular Risk. Atherosclerosis 2019, 290, 140–205. [Google Scholar] [CrossRef] [PubMed]
- Ray, K.K.; Molemans, B.; Schoonen, W.M.; Giovas, P.; Bray, S.; Kiru, G.; Murphy, J.; Banach, M.; De Servi, S.; Gaita, D.; et al. EU-Wide Cross-Sectional Observational Study of Lipid-Modifying Therapy Use in Secondary and Primary Care: The DA VINCI Study. Eur. J. Prev. Cardiol. 2021, 28, 1279–1289. [Google Scholar] [CrossRef] [PubMed]
- Ray, K.K.; Haq, I.; Bilitou, A.; Manu, M.C.; Burden, A.; Aguiar, C.; Arca, M.; Connolly, D.L.; Eriksson, M.; Ferrières, J.; et al. Treatment Gaps in the Implementation of LDL Cholesterol Control among High- and Very High-Risk Patients in Europe between 2020 and 2021: The Multinational Observational SANTORINI Study. Lancet Reg. Health Eur. 2023, 29, 100624. [Google Scholar] [CrossRef]
- Cannon, C.P.; De Lemos, J.A.; Rosenson, R.S.; Ballantyne, C.M.; Liu, Y.; Gao, Q.; Palagashvilli, T.; Alam, S.; Mues, K.E.; Bhatt, D.L.; et al. Use of Lipid-Lowering Therapies over 2 Years in GOULD, a Registry of Patients with Atherosclerotic Cardiovascular Disease in the US. JAMA Cardiol. 2021, 6, 1060–1068. [Google Scholar] [CrossRef] [PubMed]
- Ray, K.K.; Reeskamp, L.F.; Laufs, U.; Banach, M.; Mach, F.; Tokgözoǧlu, L.S.; Connolly, D.L.; Gerrits, A.J.; Stroes, E.S.G.; Masana, L.; et al. Combination Lipid-Lowering Therapy as First-Line Strategy in Very High-Risk Patients. Eur. Heart J. 2022, 43, 830–833. [Google Scholar] [CrossRef]
- Chaudhary, R.; Garg, J.; Shah, N.; Sumner, A. PCSK9 Inhibitors: A New Era of Lipid Lowering Therapy. World J. Cardiol. 2017, 9, 76. [Google Scholar] [CrossRef]
- Mansfield, B.S.; Mohamed, F.; Larouche, M.; Raal, F.J. The Hurdle of Access to Emerging Therapies and Potential Solutions in the Management of Dyslipidemias. J. Clin. Med. 2024, 13, 4160. [Google Scholar] [CrossRef] [PubMed]
- Lindley, K.J.; Aggarwal, N.R.; Briller, J.E.; Davis, M.B.; Douglass, P.; Epps, K.C.; Fleg, J.L.; Hayes, S.; Itchhaporia, D.; Mahmoud, Z.; et al. Socioeconomic Determinants of Health and Cardiovascular Outcomes in Women: JACC Review Topic of the Week. J. Am. Coll. Cardiol. 2021, 78, 1919–1929. [Google Scholar] [CrossRef] [PubMed]
- Williams, B.A.; Voyce, S.; Sidney, S.; Roger, V.L.; Plante, T.B.; Larson, S.; Lamonte, M.J.; Labarthe, D.R.; Debarmore, B.M.; Chang, A.R.; et al. Establishing a National Cardiovascular Disease Surveillance System in the United States Using Electronic Health Record Data: Key Strengths and Limitations. J. Am. Heart Assoc. 2022, 11, e024409. [Google Scholar] [CrossRef]
- Tsiampalis, T.; Panagiotakos, D. Methodological Issues of the Electronic Health Records’ Use in the Context of Epidemiological Investigations, in Light of Missing Data: A Review of the Recent Literature. BMC Med. Res. Methodol. 2023, 23, 180. [Google Scholar] [CrossRef]
- Homco, J.; Carabin, H.; Nagykaldi, Z.; Garwe, T.; Duffy, F.D.; Kendrick, D.; Martinez, S.; Zhao, Y.D.; Stoner, J. Validity of Medical Record Abstraction and Electronic Health Record-Generated Reports to Assess Performance on Cardiovascular Quality Measures in Primary Care. JAMA Netw. Open 2020, 3, e209411. [Google Scholar] [CrossRef]
- Kalra, D.K. Bridging the Racial Disparity Gap in Lipid-Lowering Therapy. J. Am. Heart Assoc. 2021, 10, e019533. [Google Scholar] [CrossRef]
- Riestenberg, R.A.; Furman, A.; Cowen, A.; Pawlowksi, A.; Schneider, D.; Lewis, A.A.; Kelly, S.; Taiwo, B.; Achenbach, C.; Palella, F.; et al. Differences in Statin Utilization and Lipid Lowering by Race, Ethnicity, and HIV Status in a Real-World Cohort of Persons with Human Immunodeficiency Virus and Uninfected Persons. Am. Heart J. 2019, 209, 79–87. [Google Scholar] [CrossRef]
- Sawant, S.; Wang, N. Under-Representation of Ethnic and Regional Minorities in Lipid-Lowering Randomized Clinical Trials: A Systematic Review and Meta-Analysis. Eur. J. Prev. Cardiol. 2023, 30, 1120–1131. [Google Scholar] [CrossRef]
- Lee, S.J.; Joo, J.H.; Park, S.; Kim, C.; Choi, D.W.; Hong, S.J.; Ahn, C.M.; Kim, J.S.; Kim, B.K.; Ko, Y.G.; et al. Combination Lipid-Lowering Therapy in Patients Undergoing Percutaneous Coronary Intervention. J. Am. Coll. Cardiol. 2023, 82, 401–410. [Google Scholar] [CrossRef]


| Total Number | Per Thousand Attended | |
|---|---|---|
| Total | 7,373,297 | 167.96 |
| Gender | ||
| Women | 3,789,865 | 166.63 |
| Men | 3,583,433 | 169.38 |
| Type of drug | ||
| Plain | 6,241,581 | 149.48 |
| Combined | 1,131,716 | 24.2 |
| Type of prevention | ||
| Primary prevention | 5,807,868 | 139.64 |
| Secondary prevention | 1,565,429 | 678.0 |
| Total Number | Per Thousand Attended | p | |
|---|---|---|---|
| Total | 5,807,868 | 139.64 | |
| Gender | |||
| Women | 3,228,947 | 148.21 | |
| Men | 2,578,922 | 130.21 | <0.01 |
| Size of the municipality | |||
| <10,000 inhab. | 1,039,095 | 162.36 | <0.001 |
| 10,001–50,000 inhab. | 1,765,079 | 127.36 | |
| 50,001–100,000 inhab. | 828,615 | 122.57 | |
| 100,001–500,000 inhab. | 1,338,874 | 128.16 | |
| >500,000 inhab. | 836,207 | 119.68 | |
| Employment status | |||
| Employed | 1,456,408 | 82.87 | |
| Unemployed | 325,622 | 121.92 | |
| Inactive | 647,168 | 51.64 | |
| Retired | 3,054,465 | 400.46 | <0.001 |
| Other | 324,205 | 80.03 |
| 2019 | 2020 | 2021 | 2022 | 2023 | ||
|---|---|---|---|---|---|---|
| Plain drug | Persons with drug | 4,595,119 | 4,533,839 | 4,829,340 | 4,823,337 | 5,312,405 |
| Persons with drug per thousand assigned | 106.35 | 104.68 | 110.83 | 114.96 | 119.50 | |
| Combined | Persons with drug | 313,089 | 337,092 | 426,734 | 359,716 | 690,837 |
| Persons with drug per thousand assigned | 7.25 | 7.78 | 9.79 | 10.42 | 15.54 | |
| Total | Persons with drug | 4,908,208 | 4,870,931 | 5,256,074 | 5,183,053 | 6,003,242 |
| Persons with drug per thousand assigned | 113.60 | 112.47 | 120.63 | 117.72 | 135.04 |
| Men | Women | Total | ||||
|---|---|---|---|---|---|---|
| Total Number | Per Thousand Attended | Total Number | Per Thousand Attended | Total Number | Per Thousand Attended | |
| 30–34 years | 18,028 | 13.09 | 11,568 | 8.43 | 29,596 | 10.76 |
| 35–39 years | 39,230 | 26.40 | 21,320 | 14.06 | 60,550 | 20.17 |
| 40–44 years | 87,712 | 49.52 | 47,532 | 26.77 | 135,244 | 38.13 |
| 45–49 years | 169,893 | 84.66 | 105,205 | 53.34 | 275,098 | 69.13 |
| 50–54 years | 252,927 | 137.74 | 214,907 | 116.08 | 467,834 | 126.86 |
| 55–59 years | 338,221 | 207.18 | 361,787 | 209.48 | 700,008 | 208.36 |
| 60–64 years | 381,919 | 284.19 | 455,450 | 302.18 | 837,369 | 293.70 |
| 65–69 years | 377,623 | 363.64 | 489,242 | 387.20 | 866,865 | 376.57 |
| 70–74 years | 335,080 | 421.29 | 470,756 | 449.61 | 805,836 | 437.38 |
| 75–79 years | 278,763 | 446.70 | 440,475 | 482.93 | 719,238 | 468,21 |
| 80–84 years | 166,502 | 436.06 | 304,152 | 480.14 | 470,654 | 463.56 |
| 85–89 years | 86,525 | 377.39 | 196,572 | 420.25 | 283,097 | 406.15 |
| 90–94 years | 29,596 | 282.31 | 82,280 | 310.91 | 111,876 | 302.80 |
| ≥95 years | 3637 | 146.72 | 14,505 | 167.63 | 18,142 | 162.97 |
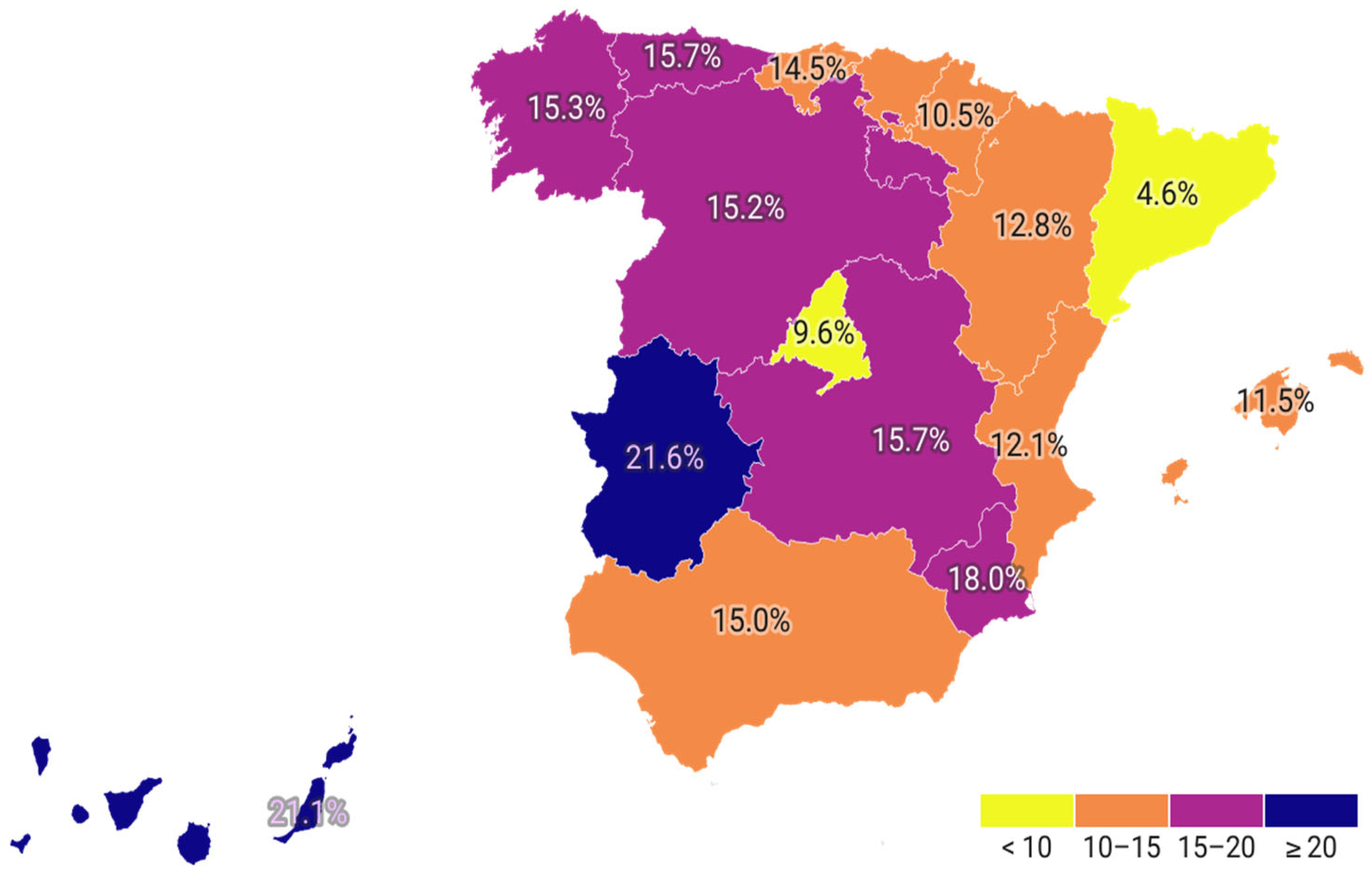
| Population Attended | Persons with Drug | Percentage with Drug | Plain Drug | Combined Drug | Percentage with Combined Drugs over Total Taking Lipid Lowering Drugs | |
|---|---|---|---|---|---|---|
| Andalucía | 7,908,922 | 1,017,200 | 12.86% | 884,749 | 132,451 | 14.97% |
| Aragón | 1,281,053 | 204,618 | 15.97% | 181,447 | 23,171 | 12.77% |
| Asturias | 926,723 | 151,201 | 16.32% | 130,718 | 20,483 | 15.67% |
| Baleares | 1,145,766 | 124,159 | 10.84% | 111,313 | 12,846 | 11.54% |
| Canarias | 2,000,880 | 301,081 | 15.05% | 248,577 | 52,504 | 21.12% |
| Cantabria | 540,606 | 98,185 | 18.16% | 85,736 | 12,449 | 14.52% |
| Castilla y León | 2,171,741 | 389,103 | 17.92% | 337,754 | 51,349 | 15.20% |
| Castilla la Mancha | 1,936,658 | 338,916 | 17.50% | 292,936 | 45,980 | 15.70% |
| Cataluña | 7,290,688 | 645,619 | 8.86% | 617,244 | 28,375 | 4.60% |
| Comunidad Valenciana | 4,643,138 | 652,315 | 14.05% | 582,034 | 70,281 | 12.08% |
| Extremadura | 987,095 | 175,590 | 17.79% | 144,436 | 31,154 | 21.57% |
| Galicia | 2,456,338 | 475,208 | 19.35% | 411,993 | 63,215 | 15.34% |
| Madrid | 6,640,044 | 856,412 | 12.90% | 781,479 | 74,933 | 9.59% |
| Murcia | 1,476,759 | 223,204 | 15.11% | 189,210 | 33,994 | 17.97% |
| Navarra | 622,949 | 76,899 | 12.34% | 69,570 | 7329 | 10.53% |
| País Vasco | 2,120,550 | 200,078 | 9.44% | 180,203 | 19,875 | 11.03% |
| La Rioja | 305,207 | 37,613 | 12.32% | 32,384 | 5229 | 16.15% |
| Total | 44,455,249 | 5,967,401 | 13.42% | 5,281,782 | 685,619 | 12.98% |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
García-Villarino, M.; Lozano-Aida, C.; Suárez-Gutiérrez, L.; Lambert, C.; González-Vidal, T.; García, A.V.; Pujante, P.; Villa-Fernández, E.; Delgado-Álvarez, E.; Menéndez-Torre, E.; et al. Use of Lipid-Lowering Treatment in Primary Prevention in Spain (Lipidspain). J. Clin. Med. 2025, 14, 6059. https://doi.org/10.3390/jcm14176059
García-Villarino M, Lozano-Aida C, Suárez-Gutiérrez L, Lambert C, González-Vidal T, García AV, Pujante P, Villa-Fernández E, Delgado-Álvarez E, Menéndez-Torre E, et al. Use of Lipid-Lowering Treatment in Primary Prevention in Spain (Lipidspain). Journal of Clinical Medicine. 2025; 14(17):6059. https://doi.org/10.3390/jcm14176059
Chicago/Turabian StyleGarcía-Villarino, Miguel, Claudia Lozano-Aida, Lorena Suárez-Gutiérrez, Carmen Lambert, Tomás González-Vidal, Ana Victoria García, Pedro Pujante, Elsa Villa-Fernández, Elías Delgado-Álvarez, Edelmiro Menéndez-Torre, and et al. 2025. "Use of Lipid-Lowering Treatment in Primary Prevention in Spain (Lipidspain)" Journal of Clinical Medicine 14, no. 17: 6059. https://doi.org/10.3390/jcm14176059
APA StyleGarcía-Villarino, M., Lozano-Aida, C., Suárez-Gutiérrez, L., Lambert, C., González-Vidal, T., García, A. V., Pujante, P., Villa-Fernández, E., Delgado-Álvarez, E., Menéndez-Torre, E., & Ares-Blanco, J. (2025). Use of Lipid-Lowering Treatment in Primary Prevention in Spain (Lipidspain). Journal of Clinical Medicine, 14(17), 6059. https://doi.org/10.3390/jcm14176059







