Invasive and Echocardiographic Mean Transvalvular Pressure Gradients of Different Transcatheter Aortic Valve Prostheses
Abstract
1. Introduction
2. Materials and Methods
2.1. Invasive Gradient
2.2. Echocardiography
2.3. Aortic Annuli
2.4. Statistics
3. Results
4. Discussion
Limitations
5. Conclusions
- 1.
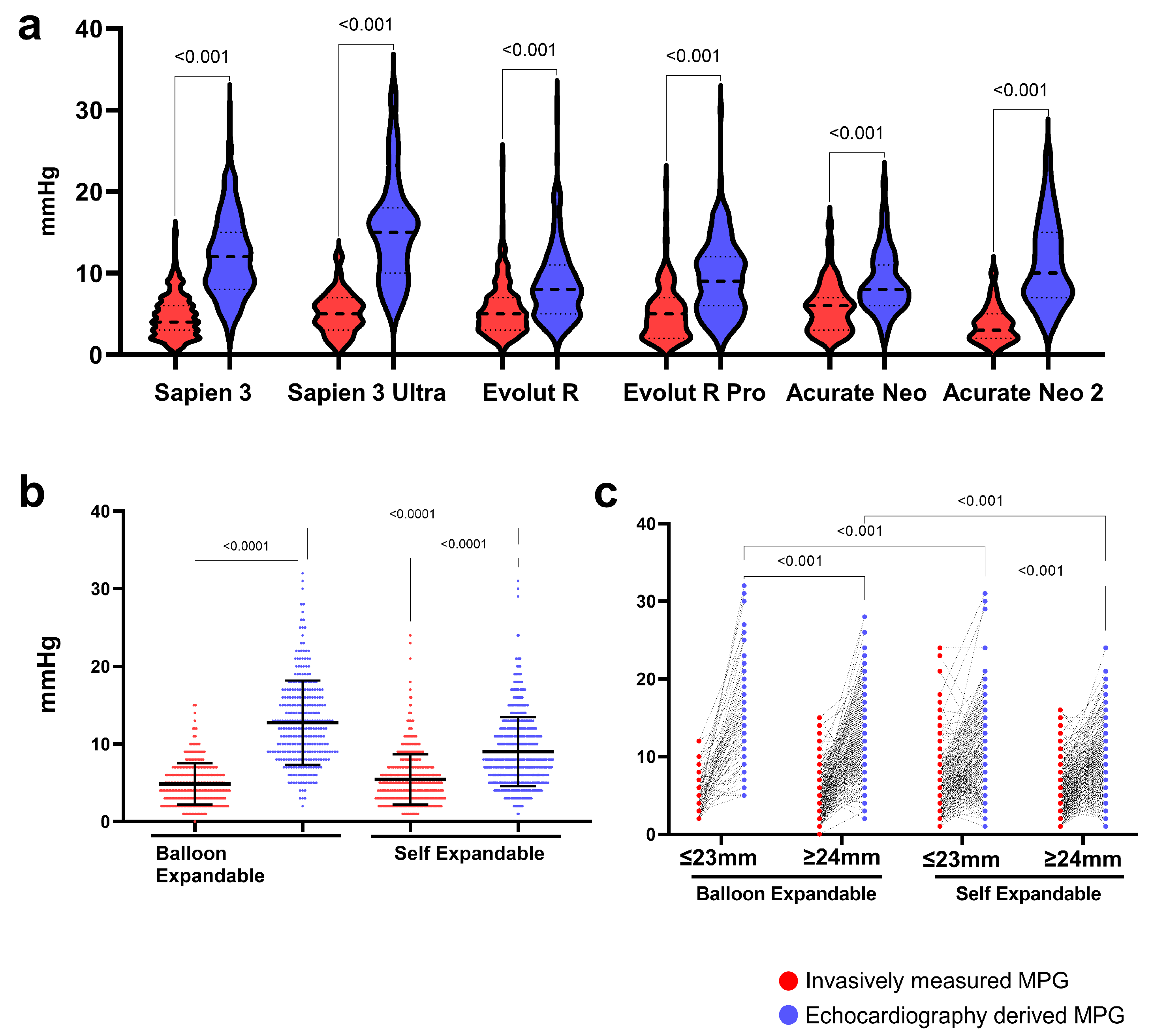
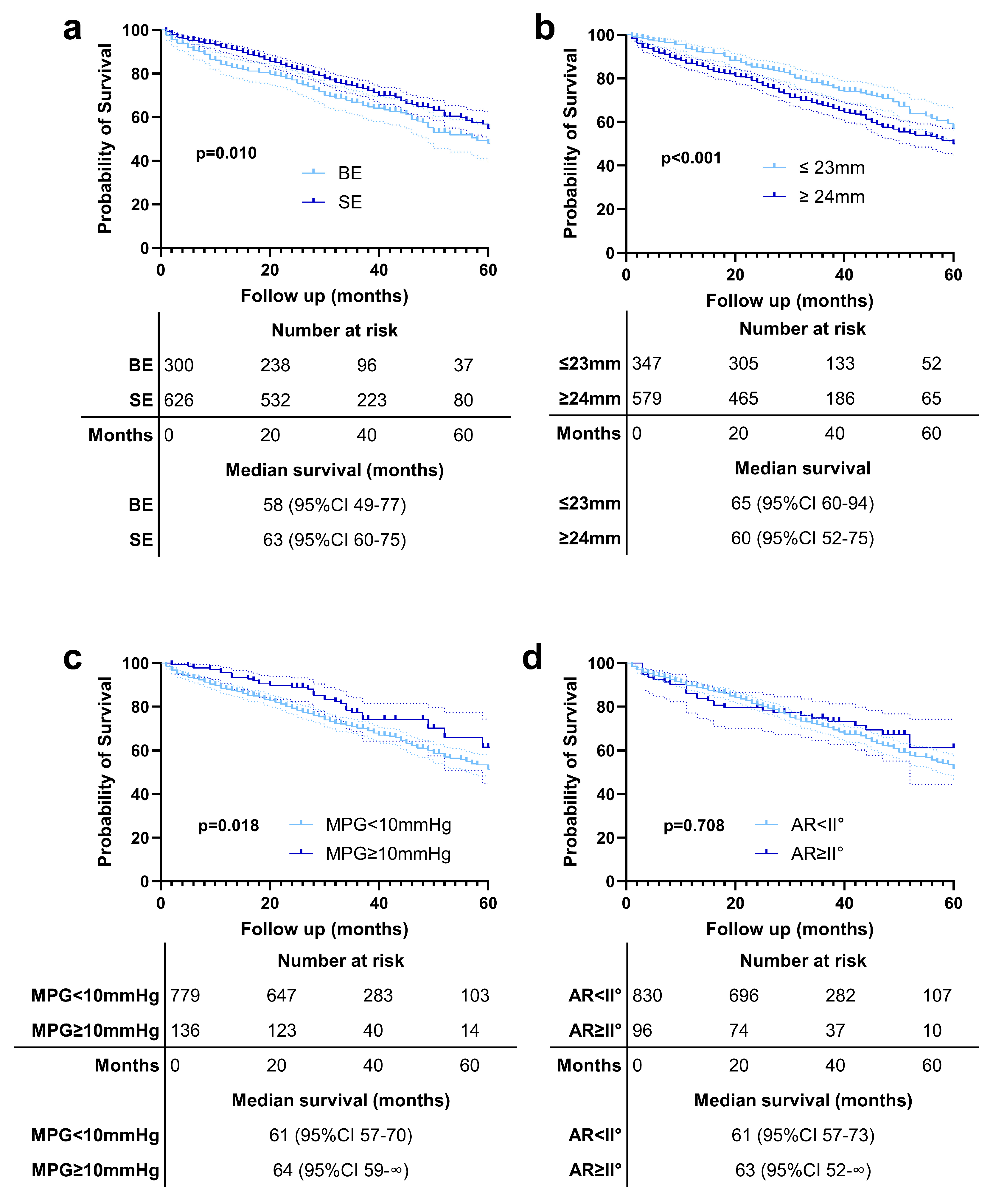
- Post-TAVR, discharge EC MPGs are higher than IC MPGs measured immediately post-procedure, particularly in BEV compared to SEV, with smaller BEVs showing the highest gradients. This difference could be attributed to the significantly different settings in which both measurements are made.
- 2.
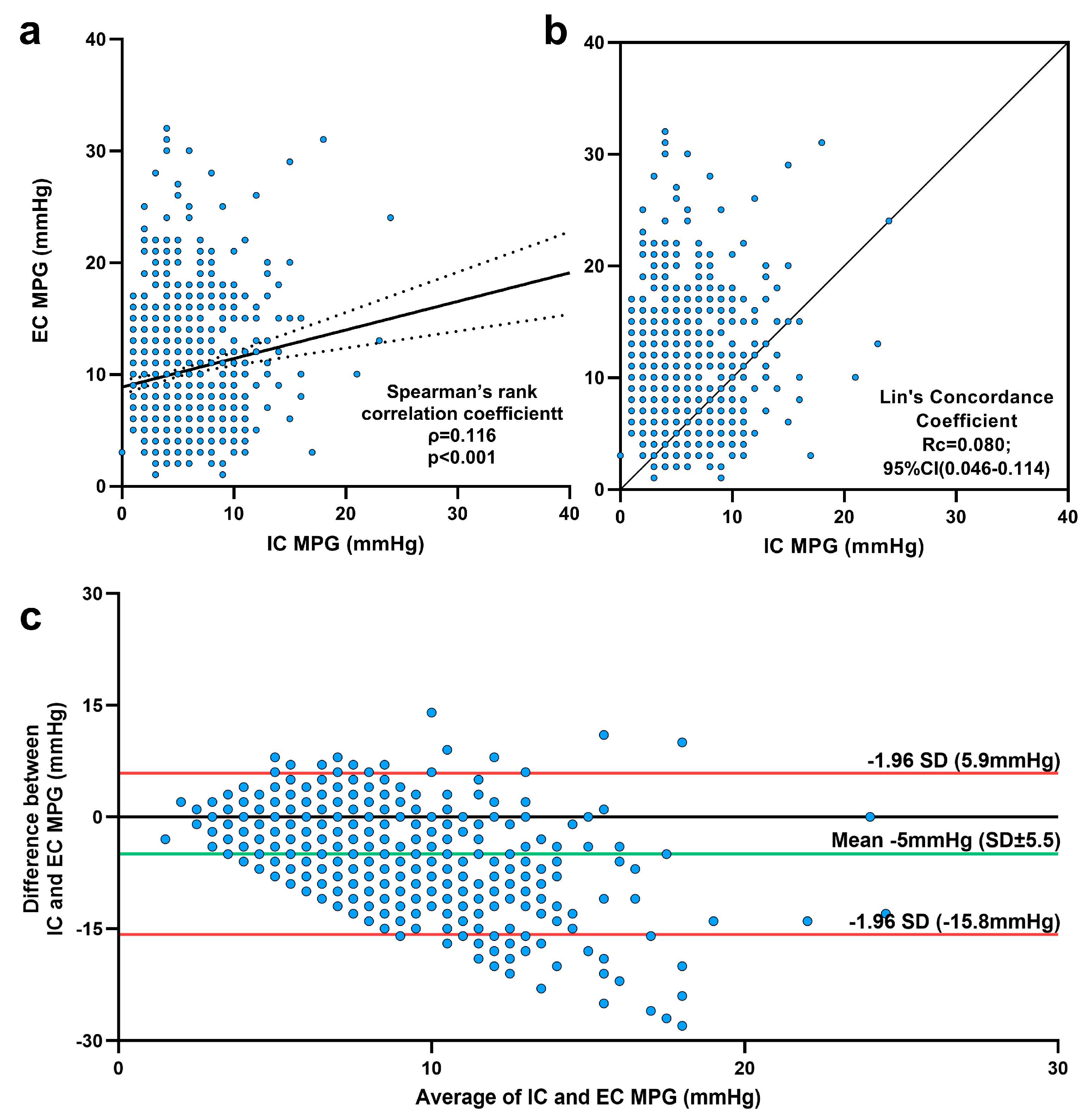
- The very small difference between invasively measured and echocardiographic-derived MPGs over the aortic valve resulted in, at first glance, a weak to non-existent correlation, irrespective of valve type. Importantly, the vast majority of measurements were within the limits of agreement, actually confirming the utility of both modalities.
- 3.
- Invasive mean gradients post-TAVR are similar across all valve sizes, but echocardiographically, smaller BEVs have higher gradients than larger BEVs. Both small and large SEVs show comparable echocardiographic gradients.
- 4.
- Both BEVs and SEVs demonstrate an excellent hemodynamic performance, with low mean gradients both immediately post-TAVR and at discharge.
- 5.
- The invasively measured differential delta did not predict echocardiographic paravalvular regurgitation, underscoring the need for a multimodal evaluation.
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| TAVR | Transcatheter aortic valve replacement |
| THV | Transcatheter heart valve |
| BE | Balloon-expandable |
| SE | Self-expandable |
| IC MPG | Invasive catheterization mean pressure gradient |
| EC MPG | Echocardiographic mean pressure gradient |
| DD | Differential delta |
| LV | Left ventricle |
| LVOT | Left ventricular outflow tract |
| LVEDP | Left ventricle end-diastolic pressure |
| EF | Ejection fraction |
| LVEF | Left ventricle ejection fraction |
| PVL | Paravalvular leakage |
| AR | Aortic regurgitation |
References
- Forrest, J.K.; Deeb, G.M.; Yakubov, S.J.; Gada, H.; Mumtaz, M.A.; Ramlawi, B.; Bajwa, T.; Teirstein, P.S.; Tchetche, D.; Huang, J.; et al. 4-Year Outcomes of Patients with Aortic Stenosis in the Evolut Low Risk Trial. J. Am. Coll. Cardiol. 2023, 82, 2163–2165. [Google Scholar] [CrossRef]
- Mack, M.J.; Leon, M.B.; Thourani, V.H.; Pibarot, P.; Hahn, R.T.; Genereux, P.; Kodali, S.K.; Kapadia, S.R.; Cohen, D.J.; Pocock, S.J.; et al. Transcatheter Aortic-Valve Replacement in Low-Risk Patients at Five Years. N. Engl. J. Med. 2023, 389, 1949–1960. [Google Scholar] [CrossRef]
- Hahn, R.T.; Leipsic, J.; Douglas, P.S.; Jaber, W.A.; Weissman, N.J.; Pibarot, P.; Blanke, P.; Oh, J.K. Comprehensive Echocardiographic Assessment of Normal Transcatheter Valve Function. JACC Cardiovasc. Imaging 2019, 12, 25–34. [Google Scholar] [CrossRef]
- Herrmann, H.C.; Mehran, R.; Blackman, D.J.; Bailey, S.; Möllmann, H.; Abdel-Wahab, M.; Ben Ali, W.; Mahoney, P.D.; Ruge, H.; Wood, D.A.; et al. Self-Expanding or Balloon-Expandable TAVR in Patients with a Small Aortic Annulus. N. Engl. J. Med. 2024, 390, 1959–1971. [Google Scholar] [CrossRef]
- Saikrishnan, N.; Kumar, G.; Sawaya, F.J.; Lerakis, S.; Yoganathan, A.P. Accurate assessment of aortic stenosis: A review of diagnostic modalities and hemodynamics. Circulation 2014, 129, 244–253. [Google Scholar] [CrossRef]
- Baumgartner, H.; Stefenelli, T.; Niederberger, J.; Schima, H.; Maurer, G. “Overestimation” of catheter gradients by Doppler ultrasound in patients with aortic stenosis: A predictable manifestation of pressure recovery. J. Am. Coll. Cardiol. 1999, 33, 1655–1661. [Google Scholar] [CrossRef]
- Geleijnse, M.L.; Di Martino, L.F.; Vletter, W.B.; Ren, B.; Galema, T.W.; Van Mieghem, N.M.; de Jaegere, P.P.; Soliman, O.I. Limitations and difficulties of echocardiographic short-axis assessment of paravalvular leakage after corevalve transcatheter aortic valve implantation. Cardiovasc. Ultrasound 2016, 14, 37. [Google Scholar] [CrossRef] [PubMed]
- Rooijakkers, M.J.P.; Stens, N.A.; van Wely, M.H.; van der Wulp, K.; Rodwell, L.; Gehlmann, H.; van Garsse, L.; Geuzebroek, G.S.C.; Verkroost, M.W.A.; Habets, J.; et al. Diastolic delta best predicts paravalvular regurgitation after transcatheter aortic valve replacement as assessed by cardiac magnetic resonance: The APPOSE trial. Eur. Heart J. Cardiovasc. Imaging 2023, 24, 1072–1081. [Google Scholar] [CrossRef]
- Baumgartner, H.C.; Hung, J.C.-C.; Bermejo, J.; Chambers, J.B.; Edvardsen, T.; Goldstein, S.; Lancellotti, P.; LeFevre, M.; Miller, F., Jr.; Otto, C.M. Recommendations on the echocardiographic assessment of aortic valve stenosis: A focused update from the European Association of Cardiovascular Imaging and the American Society of Echocardiography. Eur. Heart J. Cardiovasc. Imaging 2017, 18, 254–275. [Google Scholar] [CrossRef] [PubMed]
- Pibarot, P.; Hahn, R.T.; Weissman, N.J.; Monaghan, M.J. Assessment of paravalvular regurgitation following TAVR: A proposal of unifying grading scheme. JACC Cardiovasc. Imaging 2015, 8, 340–360. [Google Scholar] [CrossRef] [PubMed]
- Freitas-Ferraz, A.B.; Tirado-Conte, G.; Dagenais, F.; Ruel, M.; Al-Atassi, T.; Dumont, E.; Mohammadi, S.; Bernier, M.; Pibarot, P.; Rodés-Cabau, J. Aortic Stenosis and Small Aortic Annulus. Circulation 2019, 139, 2685–2702. [Google Scholar] [CrossRef]
- Abbas, A.E.; Mando, R.; Hanzel, G.; Gallagher, M.; Safian, R.; Hanson, I.; Almany, S.; Pibarot, P.; Dalal, P.; Vivacqua, A.; et al. Invasive Versus Echocardiographic Evaluation of Transvalvular Gradients Immediately Post-Transcatheter Aortic Valve Replacement. Circ. Cardiovasc. Interv. 2019, 12, e007973. [Google Scholar] [CrossRef]
- Abbas, A.E.; Mando, R.; Kadri, A.; Khalili, H.; Hanzel, G.; Shannon, F.; Al-Azizi, K.; Waggoner, T.; Kassas, S.; Pilgrim, T.; et al. Comparison of Transvalvular Aortic Mean Gradients Obtained by Intraprocedural Echocardiography and Invasive Measurement in Balloon and Self-Expanding Transcatheter Valves. J. Am. Heart Assoc. 2021, 10, e021014. [Google Scholar] [CrossRef] [PubMed]
- Biersmith, M.; Alston, M.; Makki, N.; Hatoum, H.; Yeats, B.; Egbuche, O.; Biswas, M.; Orsinelli, D.; Boudoulas, K.D.; Dasi, L.; et al. Comparison of Catheterization Versus Echocardiographic-Based Gradients in Balloon-Expandable Versus Self-Expanding Transcatheter Aortic Valve Implantation. J. Invasive Cardiol. 2022, 34, E442–E447. [Google Scholar] [CrossRef]
- DeSa, T.B.; Tecson, K.M.; Lander, S.R.; Stoler, R.C.; Vallabhan, R.C.; Hebeler, R.F.; Henry, A.C.; Grayburn, P.A. Comparison of Echocardiographic and Catheter Mean Gradient to Assess Stenosis After Transcatheter Aortic Valve Implantation. Am. J. Cardiol. 2023, 191, 110–118. [Google Scholar] [CrossRef] [PubMed]
- Khalili, H.; Pibarot, P.; Hahn, R.T.; Elmariah, S.; Pilgrim, T.; Bavry, A.A.; Maini, B.; Okuno, T.; Al-Azizi, K.; Waggoner, T.E.; et al. Transvalvular Pressure Gradients and All-Cause Mortality Following TAVR: A Multicenter Echocardiographic and Invasive Registry. JACC Cardiovasc. Interv. 2022, 15, 1837–1848. [Google Scholar] [CrossRef]
- Abdel-Wahab, M.; Landt, M.; Neumann, F.J.; Massberg, S.; Frerker, C.; Kurz, T.; Kaur, J.; Toelg, R.; Sachse, S.; Jochheim, D.; et al. 5-Year Outcomes After TAVR With Balloon-Expandable Versus Self-Expanding Valves: Results From the CHOICE Randomized Clinical Trial. JACC Cardiovasc. Interv. 2020, 13, 1071–1082. [Google Scholar] [CrossRef] [PubMed]
- Mauri, V.; Kim, W.K.; Abumayyaleh, M.; Walther, T.; Moellmann, H.; Schaefer, U.; Conradi, L.; Hengstenberg, C.; Hilker, M.; Wahlers, T.; et al. Short-Term Outcome and Hemodynamic Performance of Next-Generation Self-Expanding Versus Balloon-Expandable Transcatheter Aortic Valves in Patients with Small Aortic Annulus: A Multicenter Propensity-Matched Comparison. Circ. Cardiovasc. Interv. 2017, 10, e005013. [Google Scholar] [CrossRef]
- Yildirim, A.; Genc, O.; Pacaci, E.; Sen, O.; Kurt, I.H. Real-Life Performance and Clinical Outcomes of Portico Transcatheter Aortic Valve with FlexNav Delivery System: One-Year Data from a Single-Center Experience. J. Clin. Med. 2023, 12, 5373. [Google Scholar] [CrossRef]
- Athappan, G.; Patvardhan, E.; Tuzcu, E.M.; Svensson, L.G.; Lemos, P.A.; Fraccaro, C.; Tarantini, G.; Sinning, J.M.; Nickenig, G.; Capodanno, D.; et al. Incidence, predictors, and outcomes of aortic regurgitation after transcatheter aortic valve replacement: Meta-analysis and systematic review of literature. J. Am. Coll. Cardiol. 2013, 61, 1585–1595. [Google Scholar] [CrossRef]
- Chau, K.H.; Chen, S.; Crowley, A.; Redfors, B.; Li, D.; Hahn, R.T.; Douglas, P.S.; Alu, M.C.; Finn, M.T.; Kodali, S.; et al. Paravalvular regurgitation after transcatheter aortic valve replacement in intermediate-risk patients: A pooled PARTNER 2 study. EuroIntervention 2022, 17, 1053–1060. [Google Scholar] [CrossRef] [PubMed]
- Okuno, T.; Tomii, D.; Heg, D.; Lanz, J.; Praz, F.; Stortecky, S.; Reineke, D.; Windecker, S.; Pilgrim, T. Five-year outcomes of mild paravalvular regurgitation after transcatheter aortic valve implantation. EuroIntervention 2022, 18, 33–42. [Google Scholar] [CrossRef] [PubMed]

| Patient Characteristics | Results |
|---|---|
| Age (years) | 81; 78–85 |
| Men n, (%) | 445 (48.1%) |
| BMI (kg/m2) | 27.2; 24.3–30.4 |
| NYHA Class | |
| I n, (%) | 20 (2.2%) |
| II n, (%) | 286 (30.9%) |
| III n, (%) | 571 (61.7%) |
| IV n, (%) | 49 (5.3%) |
| Diabetes mellitus n, (%) | 323 (34.9%) |
| Dialysis n, (%) | 18 (1.9%) |
| COPD n, (%) | 164 (17.7%) |
| No CAD n, (%) | 407 (44.0%) |
| CAD 1 Vessel n, (%) | 195 (21.0%) |
| CAD 2 Vessel n, (%) | 139 (15.0%) |
| CAD 3 Vessel n, (%) | 185 (20.0%) |
| PAD n, (%) | 99 (10,7%) |
| Atrial fibrillation n, (%) | 271 (29.3%) |
| AVA (cm2) | 0.7; 0.6–0.9 |
| Valve annulus (mm) | 24; 23–26 |
| Annulus ≤ 23 mm n, (%) | 347 (37.5%) |
| Annulus ≥ 24 mm n, (%) | 579 (62.5%) |
| LVEF (%) | 55; 50–55 |
| Balloon dilatation before impl. n, (%) | 318 (34.3%) |
| Balloon dilatation after impl. n, (%) | 294 (31.7%) |
| TAVR TF n, (%) | 909 (98.2%) |
| Parameter | Pre TAVR (mmHG) Median; IQR | Post TAVR (mmHg) Median; IQR | p |
|---|---|---|---|
| LVEDP | 15; 11–21 | 18; 13–23 | <0.01 |
| Aortic pressure systolic | 103; 89–120 | 124; 107–144 | <0.01 |
| Aortic pressure diastolic | 50; 43–58 | 52; 45–62 | <0.01 |
| ICMPG | 43; 34–53 | 5; 3–7 | <0.01 |
| Valves | No. Patients | Valve Size | No. Patients | IC MPG (mmHg) Median; IQR | EC MPG (mmHg) Median; IQR |
|---|---|---|---|---|---|
| Sapien 3 | 244 (26.3%) | 23 mm | 49 | 4; 2–6 | 15; 12–18.5 |
| 26 mm | 73 | 5; 3–7 | 11; 8–15 | ||
| 29 mm | 122 | 4.5; 3–6 | 11; 8–13 | ||
| Sapien 3 Ultra | 56 (6.0%) | 23 mm | 16 | 6; 4–7 | 16.5; 14.5–24 |
| 26 mm | 40 | 5; 3–7 | 14; 9–18 | ||
| Evolut R | 304 (32.8%) | 23 mm | 15 | 13; 10–16 | 17; 13–20 |
| 26 mm | 78 | 4.5; 3–7 | 7; 5–10 | ||
| 29 mm | 128 | 5; 3–7 | 8; 5–10 | ||
| 34 mm | 83 | 5; 4–7 | 8; 5–10 | ||
| Evolut Pro | 157 (17.0%) | 26 mm | 37 | 5; 3–7.5 | 10; 5.5–12.5 |
| 29 mm | 120 | 4; 2–7 | 9; 6–12 | ||
| Acurate Neo | 136 (14.7%) | S | 42 | 6; 3–9 | 10; 8–13 |
| M | 62 | 5; 3–7 | 8; 6–11 | ||
| L | 32 | 5; 3–7 | 7; 6–8 | ||
| Acurate Neo 2 | 29 (3.1%) | S | 11 | 3; 2–4 | 11; 7–17 |
| M | 12 | 4; 2–6 | 10.5; 8–14 | ||
| L | 5 | 2.5; 2–5.5 | 8; 6.5–13.5 |
| None | Mild | Moderate | Severe | |
|---|---|---|---|---|
| Balloon-expandable valves | 193 (64.3%) † | 92 (30.7%) † | 15 (5.0%) † | 0 (0.0%) |
| Sapien 3 | 153 (62.7%) | 78 (32.0%) | 13 (5.3%) | 0 (0.0%) |
| Sapien 3 Ultra | 40 (71.4%) | 14 (25.0%) | 2 (3.6%) | 0 (0.0%) |
| Self-expandable valves | 283 (45.2%) † | 262 (41.9%) † | 80 (12.8%) † | 1 (0.2%) |
| Evolut R | 154 (50.7%) | 122 (40.1%) | 28 (9.2%) | 0 (0.0%) |
| Evolut Pro | 66 (42.0%) | 66 (42.0%) | 25 (15.9%) | 0 (0.0%) |
| Accurate neo | 49 (36.0%) | 59 (43.4%) | 27 (19.9%) | 1 (0.7%) |
| Acurate neo2 | 14 (48.3%) | 15 (51.7%) | 0 (0.0%) | 0 (0.0%) |
| Total | 476 (51.4%) | 354 (38.2%) | 95 (10.3%) | 1 (0.1%) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
El-Hachem, G.; Deutsch, M.-A.; Rojas, S.; Paluszkiewicz, L.; Sharaf, M.; Gilis-Januszewski, T.; Rudolph, T.K.; Scholtz, S.; Friedrichs, K.P.; Schramm, R.; et al. Invasive and Echocardiographic Mean Transvalvular Pressure Gradients of Different Transcatheter Aortic Valve Prostheses. J. Clin. Med. 2025, 14, 5875. https://doi.org/10.3390/jcm14165875
El-Hachem G, Deutsch M-A, Rojas S, Paluszkiewicz L, Sharaf M, Gilis-Januszewski T, Rudolph TK, Scholtz S, Friedrichs KP, Schramm R, et al. Invasive and Echocardiographic Mean Transvalvular Pressure Gradients of Different Transcatheter Aortic Valve Prostheses. Journal of Clinical Medicine. 2025; 14(16):5875. https://doi.org/10.3390/jcm14165875
Chicago/Turabian StyleEl-Hachem, Georges, Marcus-André Deutsch, Sebastian Rojas, Lech Paluszkiewicz, Mohammad Sharaf, Tomasz Gilis-Januszewski, Tanja Katharina Rudolph, Smita Scholtz, Kai Peter Friedrichs, René Schramm, and et al. 2025. "Invasive and Echocardiographic Mean Transvalvular Pressure Gradients of Different Transcatheter Aortic Valve Prostheses" Journal of Clinical Medicine 14, no. 16: 5875. https://doi.org/10.3390/jcm14165875
APA StyleEl-Hachem, G., Deutsch, M.-A., Rojas, S., Paluszkiewicz, L., Sharaf, M., Gilis-Januszewski, T., Rudolph, T. K., Scholtz, S., Friedrichs, K. P., Schramm, R., Rudolph, V., Gummert, J. F., Opacic, D., & Bleiziffer, S. (2025). Invasive and Echocardiographic Mean Transvalvular Pressure Gradients of Different Transcatheter Aortic Valve Prostheses. Journal of Clinical Medicine, 14(16), 5875. https://doi.org/10.3390/jcm14165875








