Epidemiological Analysis of Cardiovascular Diseases with Consideration of Risk Factors, Health Awareness, and Preventive Behaviors in Civilian and Military Populations
Abstract
1. Introduction
- Metabolic factors: systolic blood pressure, low-density lipoprotein (LDL) cholesterol levels, body mass index (BMI), fasting blood glucose, and kidney function impairment;
- Behavioral (lifestyle-related) factors: diet, smoking, exposure to secondhand smoke, alcohol consumption, and physical activity.
2. Materials and Methods
- Eligibility for participation in this study, based on inclusion and exclusion criteria;
- Expressing written, informed consent to participate in this study;
- Survey study;
- Blood pressure measurement;
- Blood sampling for cardiovascular risk parameters;
- Laboratory testing—lipid profile parameters (total cholesterol, HDL cholesterol, LDL cholesterol, triglycerides) in the context of cardiovascular risk;
- Entering the obtained results into the database;
- Statistical analysis of the obtained results.
- Soldier or civilian employee of the military;
- Provision of informed consent to participate in this study.
- Lack of informed consent to participate in this study;
- Any clinical condition that prevents cooperation;
- Cancer or acute chronic inflammatory conditions.
Statistical Analysis
3. Results
Characteristics of the Respondents
4. Discussion
- This study was based on a relatively small sample size, which may limit the statistical power of the analyses and reduce the generalizability of the findings to a broader population;
- The study population consisted exclusively of soldiers and civilian military employees, which limits the applicability of the results to the general civilian population. The unique working conditions of this occupational group may significantly influence cardiovascular risk;
- This study had a cross-sectional design, meaning that it presents only a single-time-point assessment of cardiovascular risk. It does not allow for causal inference or evaluation of changes in risk over time;
- Although some lifestyle factors were considered, no detailed quantitative data were collected regarding dietary quality, caloric intake, or objectively measured physical activity (e.g., via accelerometers), which may limit the accuracy of lifestyle-related risk assessment;
- Data on health behaviors and self-rated health status were based on participant self-reports, which may be subject to recall bias or social desirability bias—particularly in a hierarchical environment such as the military;
- This study did not assess health-related motivation or interpersonal relationships, which may act as relevant psychosocial factors differentiating cardiovascular risk profiles between groups;
- This analysis did not account for the menstrual cycle phase, which may influence the emotional and physiological state of female participants and affect certain risk factor assessments;
- Metabolically heterogeneous phenotypes of obesity were not distinguished, which could have provided additional insights into cardiovascular risk beyond BMI-based categorization;
- This study did not include an evaluation of occupational burnout, which may be a relevant stress-related factor contributing to cardiovascular risk, especially in demanding professional environments such as the military;
- This analysis was limited to descriptive statistics, which may reduce the strength of the evidence and limit the ability to detect deeper associations between variables.
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Gielerak, G.; Krzesiński, P.; Piotrowicz, K.; Murawski, P.; Skrobowski, A.; Stańczyk, A.; Galas, A.; Uziębło-Życzkowska, B.; Kaźmierczak-Dziuk, A.; Maksimczuk, J.; et al. The Prevalence of Cardiovascular Risk Factors among Polish Soldiers: The Results from the MIL-SCORE Program. Cardiol. Res. Pract. 2020, 2020, 1–7. [Google Scholar] [CrossRef]
- Yusuf, S.; Hawken, S.; Ôunpuu, S.; Dans, T.; Avezum, A.; Lanas, F.; McQueen, M.; Budaj, A.; Pais, P.; Varigos, J.; et al. Effect of potentially modifiable risk factors associated with myocardial infarction in 52 countries (the INTERHEART study): Case-control study. Lancet 2004, 364, 937–952. [Google Scholar] [CrossRef]
- Opolski, K.; Zdrojewski, T.; Opolska, Z. (Eds.) Antynomie Systemu Ochrony Zdrowia; Polska Akademia Nauk: Warszawa, Poland, 2021; pp. 113–122. [Google Scholar]
- Agencja Oceny Technologii Medycznych i Taryfikacji [Internet]. Rekomendacja nr 1/2023 Prezesa AOTMiT z 29 Grudnia 2023 r. w Sprawie Zalecanych Technologii Medycznych, Działań Przeprowadzanych w Ramach Programów Polityki Zdrowotnej oraz Warunków Realizacji Tych Programów, Dotyczących Profilaktyki Uzależnień od Tytoniu (nikotyny). 29 December 2023. Available online: https://www.aotm.gov.pl (accessed on 15 June 2025).
- Martin, S.S.; Aday, A.W.; Almarzooq, Z.I.; Anderson, C.A.M.; Arora, P.; Avery, C.L.; Baker-Smith, C.M.; Gibbs, B.B.; Beaton, A.Z.; Boehme, A.K.; et al. 2024 Heart Disease and Stroke Statistics: A Report of US and Global Data From the American Heart Association. Circulation 2024, 149, e347–e913. [Google Scholar] [CrossRef]
- Żbikowski, J.; Nieporęcki, R.; Bzdęga, J.; Lach, J.; Kubiak, L.; Ostalska, J. Wojskowe zakłady lecznicze armii polskiej. Część I. Chorzy leczeni w latach 1922–1931 na podstawie sprawozdania gen. Stanisława Roupperta do Marszałka Józefa Piłsudskiego. Hygeia Public Health 2014, 49, 774–778. [Google Scholar]
- Trzeciak, B.G.; Kowalczyk, W.; Grymek, S.; Gutknecht, P.; Siebert, J. Cardiovascular risk factors among Polish employees of uniformed services. Int. J. Occup. Med. Environ. Health 2023, 36, 656–671. [Google Scholar] [CrossRef]
- Vemu, P.L.; Yang, E.; Ebinger, J. 2023 ESH Hypertension Guideline Update: Bringing us Closer Together Across the Pond. American College of Cardiology [Internet]. 5 February 2024. Available online: https://www.acc.org/Latest-in-Cardiology/Articles/2024/02/05/11/43/2023-ESH-Hypertension-Guideline-Update (accessed on 15 June 2025).
- De Backer, G. European guidelines on cardiovascular disease prevention in clinical practice Third Joint Task Force of European and other Societies on Cardiovascular Disease Prevention in Clinical Practice (constituted by representatives of eight societies and by invited experts). Eur. Heart J. 2003, 24, 1601–1610. [Google Scholar]
- Conroy, R. Estimation of ten-year risk of fatal cardiovascular disease in Europe: The SCORE project. Eur. Heart J. 2003, 24, 987–1003. [Google Scholar] [CrossRef]
- SCORE2 Working Group and ESC Cardiovascular Risk Collaboration. SCORE2 risk prediction algorithms: New models to estimate 10-year risk of cardiovascular disease in Europe. Eur. Heart J. 2021, 42, 2439–2454. [Google Scholar] [CrossRef]
- Zdrojewski, T.; Jankowski, P.; Bandosz, P.; Bartuś, S.; Chwojnicki, K.; Drygas, W.; Gaciong, Z.; Hoffman, P.; Kalarus, Z.; Kaźmierczak, J.; et al. A new version of cardiovascular risk assessment system and risk charts calibrated for Polish population. Kardiol. Pol. 2015, 73, 958–961. [Google Scholar] [CrossRef]
- Csenteri, O.; Jancsó, Z.; Szöllösi, G.J.; Andréka, P.; Vajer, P. Differences of cardiovascular risk assessment in clinical practice using SCORE and SCORE2. Open Heart 2022, 9, e002087. [Google Scholar] [CrossRef]
- Boskovic, N.; Giga, V.; Djordjevic-Dikic, A.; Beleslin, B.; Stojkovic, S.; Nedeljkovic, I.; Aleksandric, S.; Tesic, M.; Dedic, S.; Burazor, I.; et al. Comparison of SCORE and SCORE 2 risk prediction tools in contemporary very high risk european population. Eur. Heart J. 2022, 43 (Suppl. S2), ehac544.2281. [Google Scholar] [CrossRef]
- Rzepka-Cholasinska, A.; Kasprzak, M.; Michalski, P.; Pietrzykowski, Ł.; Grzelakowska, K.; Kubica, A. Cardiovascular risk assessment based on SCORE and SCORE2. Med. Res. J. 2022, 7, 164–169. [Google Scholar] [CrossRef]
- Woodruff, S.I.; Hurtado, S.L.; Simon-Arndt, C.M.; Lawrenz, J. An exploratory case study of environmental factors related to military alcohol misuse. BMC Public Health 2018, 18, 902. [Google Scholar] [CrossRef]
- World Obesity Federation [Internet]. World Obesity Atlas 2023. March 2023. Available online: https://worldobesity.org/resources/resource-library/world-obesity-atlas-2023 (accessed on 15 June 2025).
- Rosellini, A.J.; Stein, M.B.; Benedek, D.M.; Bliese, P.D.; Chiu, W.T.; Hwang, I.; Monahan, J.; Nock, M.K.; Petukhova, M.V.; Sampson, N.A.; et al. Using self-report surveys at the beginning of service to develop multi-outcome risk models for new soldiers in the U.S. Army. Psychol. Med. 2017, 47, 2275–2287. [Google Scholar] [CrossRef]
- Faryabi, R.; Movahed, E.; Sheidaei, A.; Clark, C.C.T. Predictors of behavioral risk factors associated with myocardial infarction and stroke based on protection motivation theory in middle-aged adults of Southern Iran: Threat appraisal or coping appraisal? Russ. Open Med. J. 2025, 14, e0101. [Google Scholar] [CrossRef]
- Nieh, C.; Mancuso, J.D.; Powell, T.M.; Welsh, M.M.; Gackstetter, G.D.; Hooper, T.I. Cigarette smoking patterns among U.S. military service members before and after separation from the military. PLoS ONE 2021, 16, e0257539. [Google Scholar] [CrossRef]
- Jung, S.; Kang, H.; Cho, S.-i. Age-period-cohort analysis of smoking prevalence trends among career military personnel in South Korea. Tob. Induc. Dis. 2024, 22, 185. [Google Scholar] [CrossRef]
- Aragiannis, D.; Kasiakogias, A.; Iliakis, P.; Sagris, M.; Tatakis, F.P.; Manta, E.; Andrikou, I.; Konstantinidis, D.; Tsioufis, K. The Combined Effect of Smoking and Obesity on Hypertension: Implications for Clinical Management. Curr. Hypertens. Rev. 2025, 21, 2–14. [Google Scholar] [CrossRef]
- Vincent, S.R.; Schlenk, M.A.; Horan, K.A.; Moore, B.A. Incidences and trends of cardiovascular determinants and diagnoses in active duty service members. J. Mil. Veterans Health 2024, 32, 42–51. Available online: https://jmvh.org/wp-content/uploads/2024/10/AMMA-JMVH-October-2024-S-R-Vincent.pdf (accessed on 15 June 2025).
- Grósz, A.; Tóth, E.; Péter, I. A 10-year follow-up of ischemic heart disease risk factors in military pilots. Mil. Med. 2007, 172, 214–219. [Google Scholar] [CrossRef]
- Radjen, S.D.; Jovelic, A.S.; Radjen, G.S.; Hajdukovic, Z.V.; Radakovic, S.S. Metabolic syndrome and carotid artery intima-media thickness in military pilots. Aviat. Space Environ. Med. 2011, 82, 622–626. [Google Scholar] [CrossRef]
- Gendron, P.; Lajoie, C.; Laurencelle, L.; Trudeau, F. Cardiovascular health profile among Québec male and female police officers. Arch. Environ. Occup. Health 2019, 74, 331–340. [Google Scholar] [CrossRef]
- Banach, M.; Burchardt, P.; Chlebus, K.; Dobrowolski, P.; Dudek, D.; Dyrbuś, K.; Gąsior, M.; Jankowski, P.; Jóźwiak, J.; Kłosiewicz-Latoszek, L.; et al. PoLA/CFPiP/PCS/PSLD/PSD/PSH guidelines on diagnosis and therapy of lipid disorders in Poland 2021. Arch. Med. Sci. 2021, 17, 1447–1547. [Google Scholar] [CrossRef]
- Vaicaitiene, R.; Cerniauskiene, L.R.; Luksiene, D.I.; Margeviciene, L. Hypercholesterolemia and Smoking Habits of Lithuanian Military Personnel. Mil. Med. 2006, 171, 512–515. [Google Scholar] [CrossRef]
- Webber, B.J.; Bornstein, D.B.; Kiel, M.A.; Wilkins, R.C.; Bryant, C.X. Physical Activity and the Health of a Nation: A National Challenge and Collective Response. Am. J. Lifestyle Med. 2024, 18, 632–637. [Google Scholar] [CrossRef]
- Eghbalian, M.; Akbari, H.; Norozi, M.; Nasab, H.; Karamali, M.; Imani, M.; Zahiri, H.; Raei, M. Correlation Between Obesity and Risk Factors of Cardiovascular Diseases in Military Personnel. Iran. J. Public Health 2025, 54, 205–213. Available online: https://publish.kne-publishing.com/index.php/ijph/article/view/17592 (accessed on 15 June 2025). [CrossRef]
- Movsisyan, N.K.; Vinciguerra, M.; Medina-Inojosa, J.R.; Lopez-Jimenez, F. Cardiovascular diseases in Central and Eastern Europe: A call for more surveillance and evidence-based health promotion. Ann. Glob. Health 2020, 86, 21. [Google Scholar] [CrossRef]
- Zawadzka, M.; Marszałkowska-Jakubik, J.; Ejchman-Pac, E.; Pająk-Tarnacka, B.; Szymański, P. Assessing Cardiovascular Risk Among Polish Soldiers: Insights Using the POL SCORE Tool. J. Clin. Med. 2025, 14, 2130. [Google Scholar] [CrossRef]
- Espinoza-Derout, J.; Shao, X.M.; Lao, C.J.; Hasan, K.M.; Rivera, J.C.; Jordan, M.C.; Echeverria, V.; Roos, K.P.; Sinha-Hikim, A.P.; Friedman, T.C. Electronic Cigarette Use and the Risk of Cardiovascular Diseases. Front. Cardiovasc. Med. 2022, 9, 879726. [Google Scholar] [CrossRef]



| Variables | SD | Me | Min | Max | Q1 | Q3 | |
|---|---|---|---|---|---|---|---|
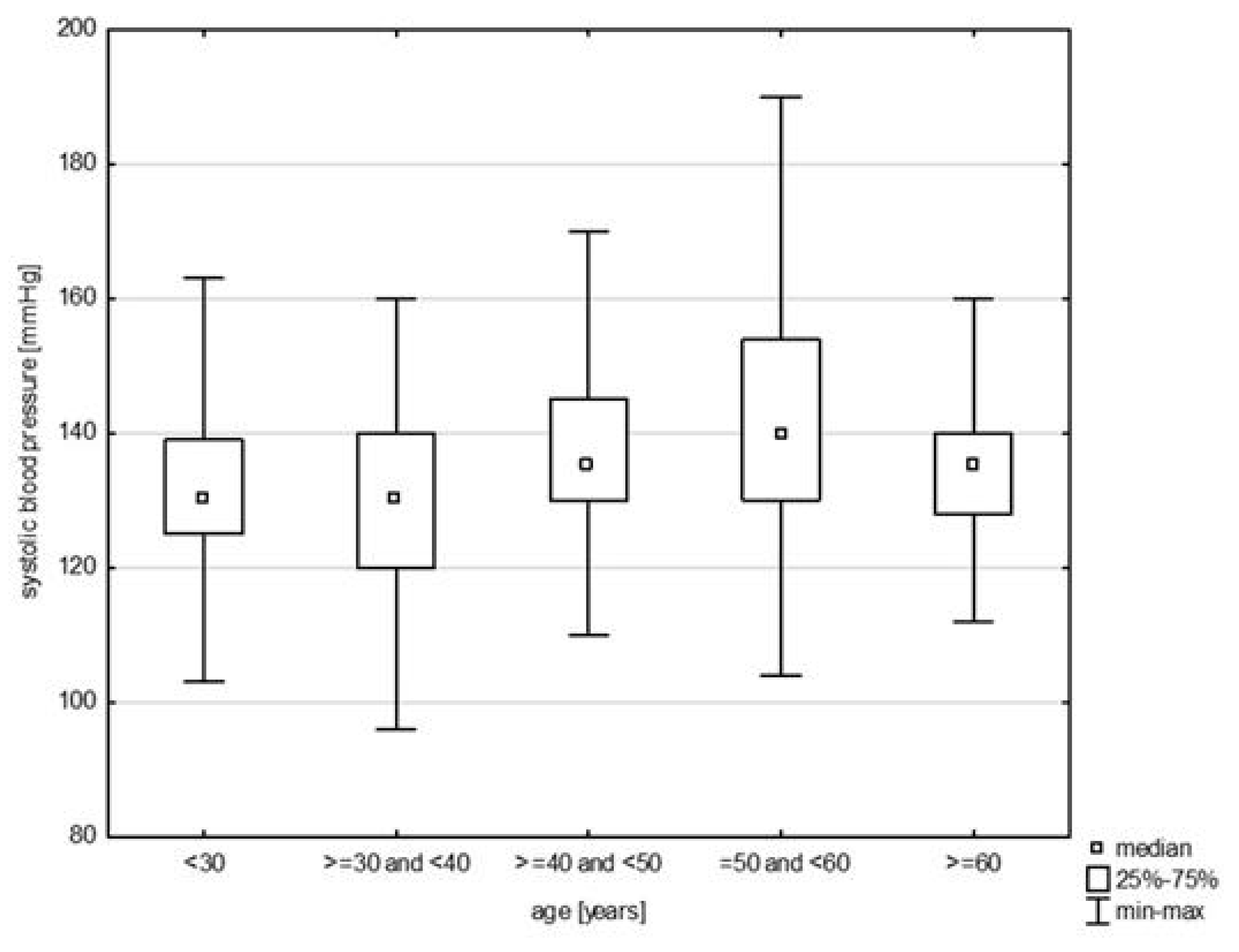
| systolic blood pressure | 136.03 | 15.85 | 135.00 | 96.00 | 190.00 | 125.00 | 145.00 |
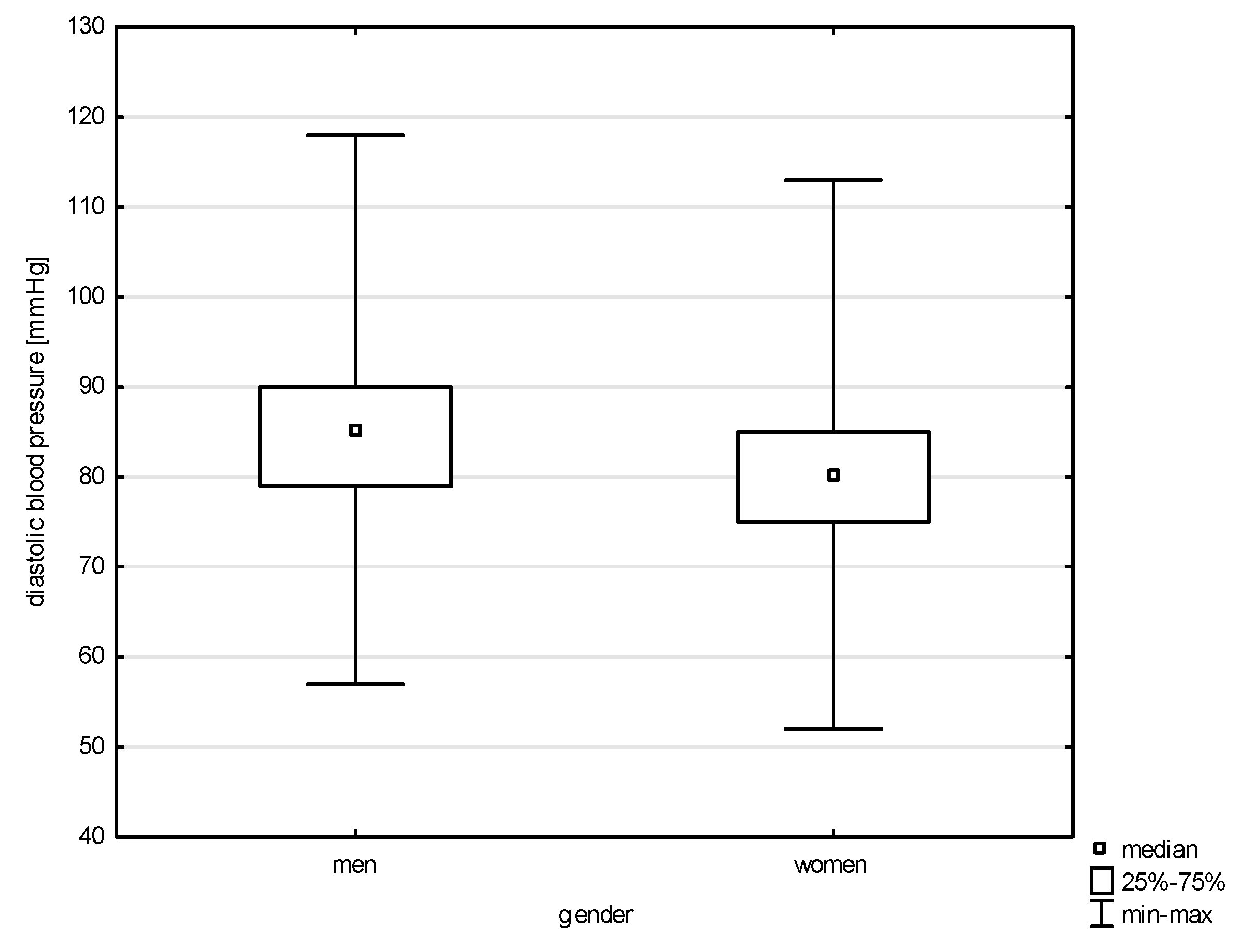
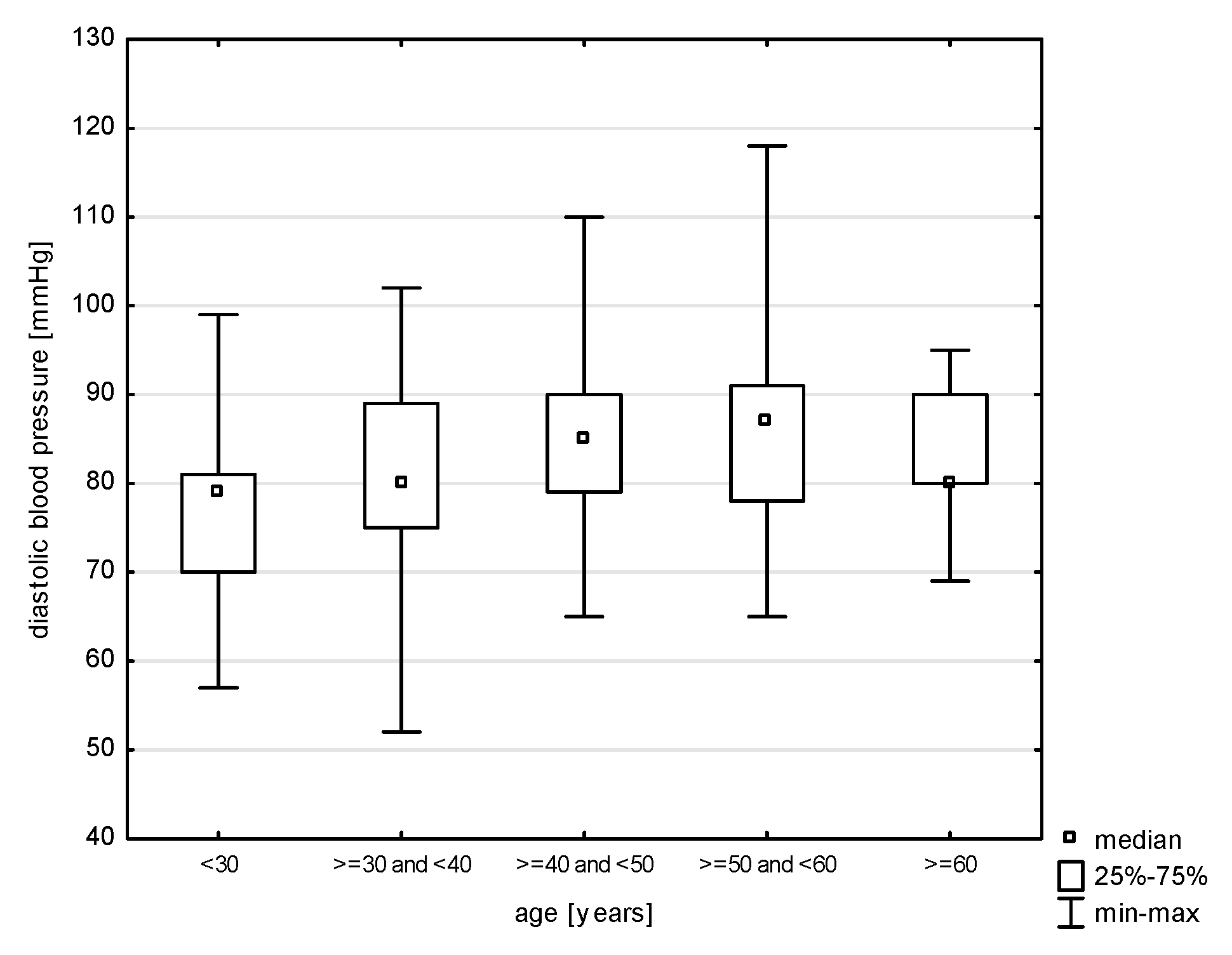
| diastolic blood pressure | 83.21 | 9.99 | 81.00 | 52.00 | 118.00 | 76.50 | 90.00 |
| total cholesterol | 222.16 | 44.85 | 216.40 | 117.00 | 459.60 | 193.70 | 250.90 |
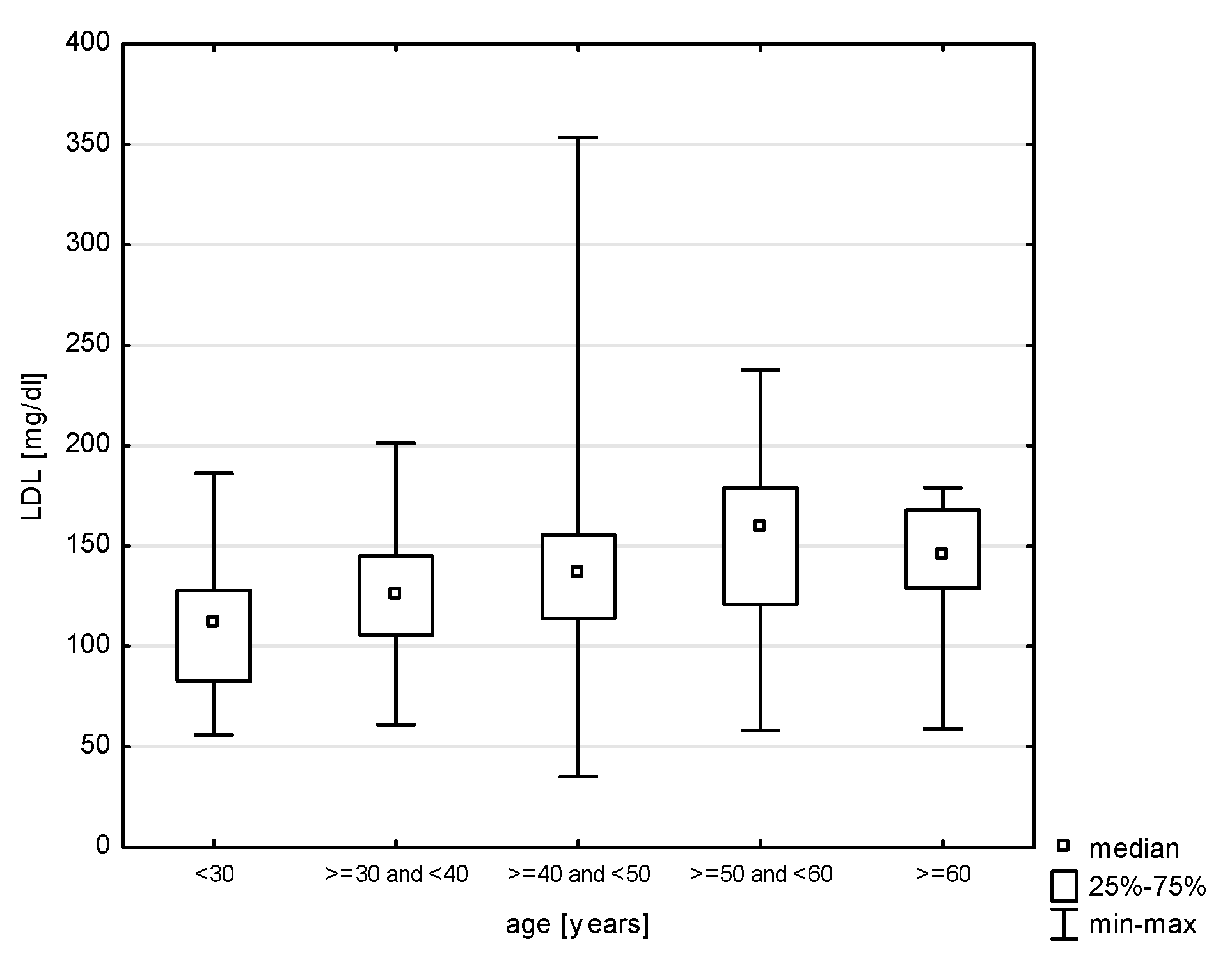
| LDL | 135.92 | 37.64 | 134.50 | 35.00 | 353.60 | 111.30 | 160.10 |
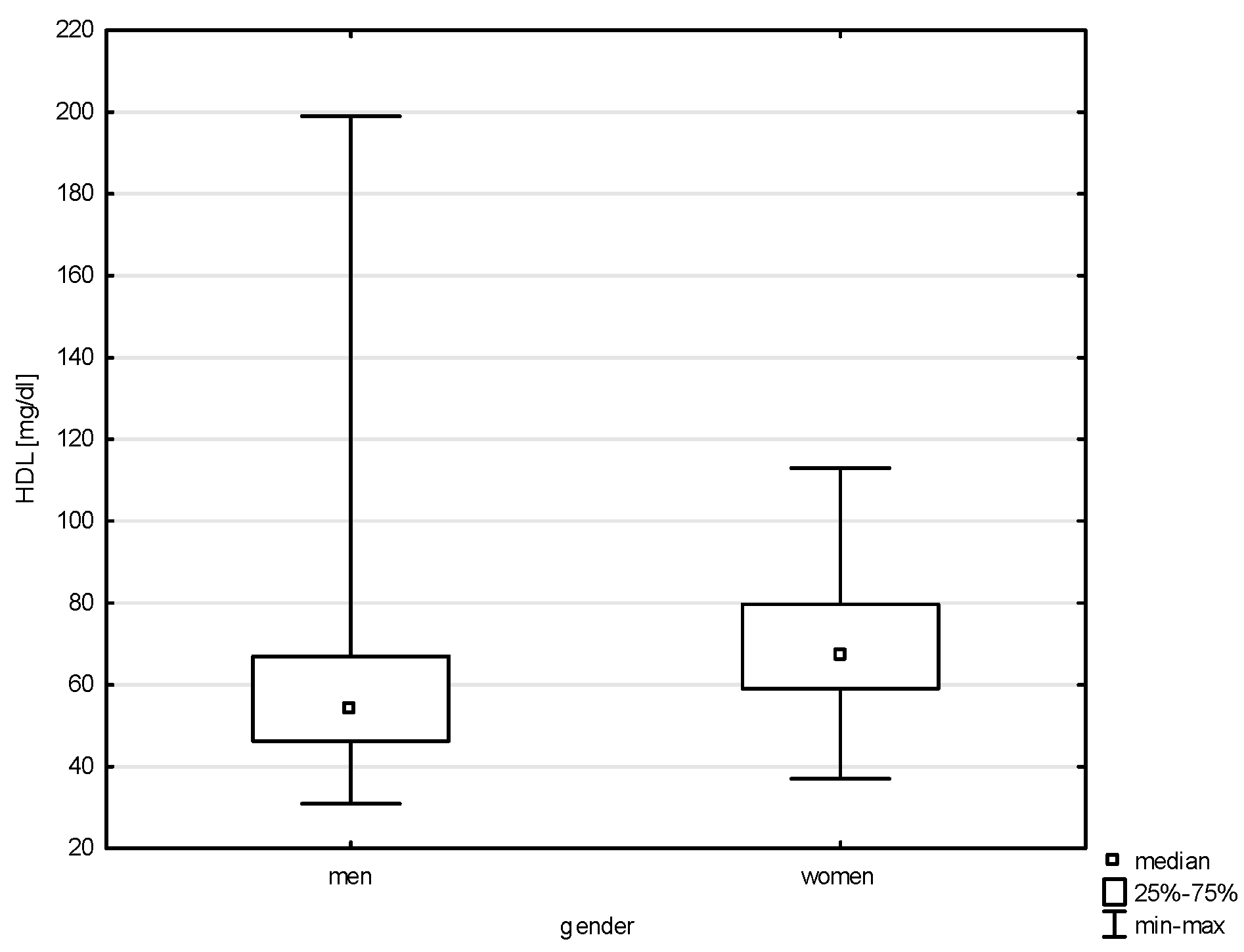
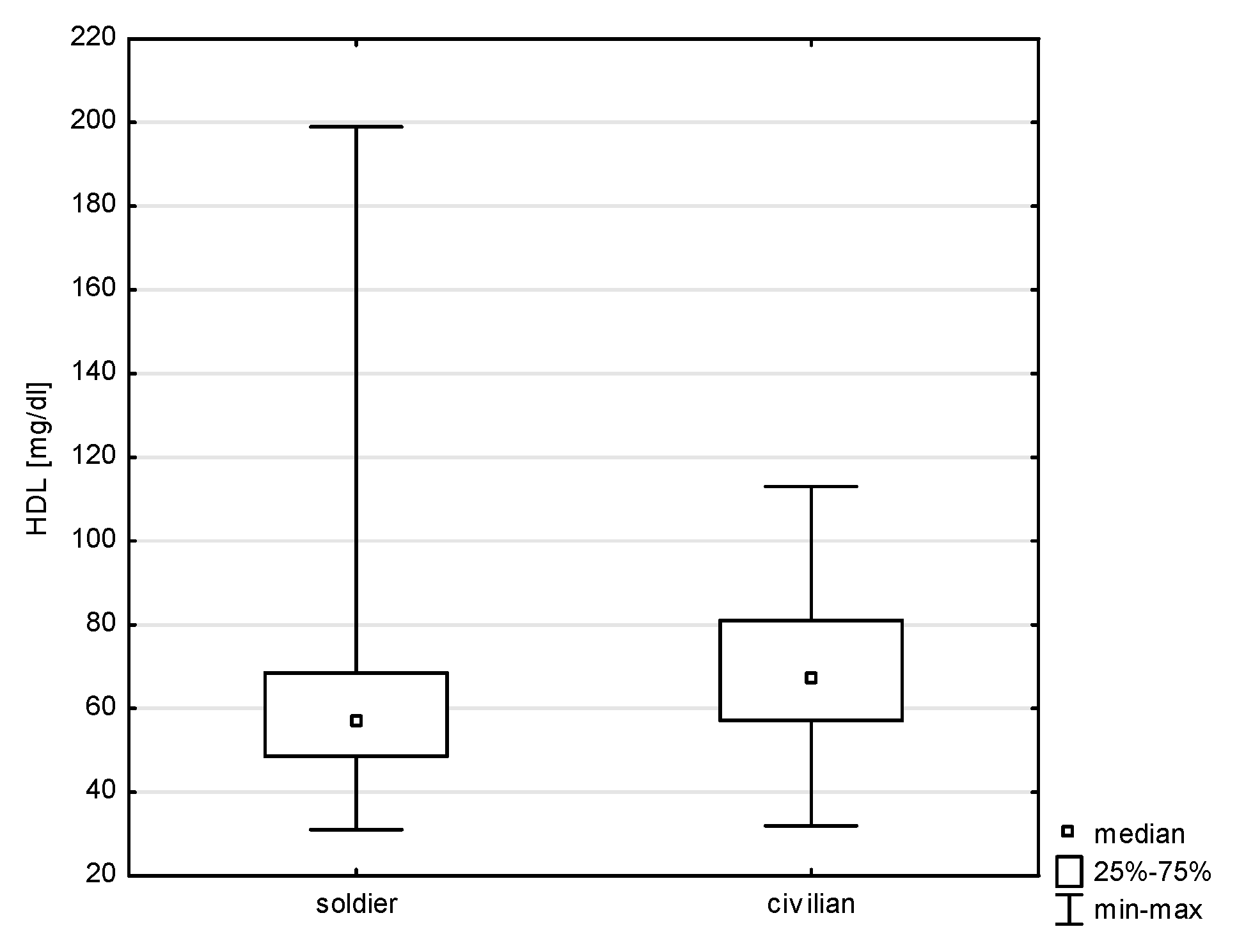
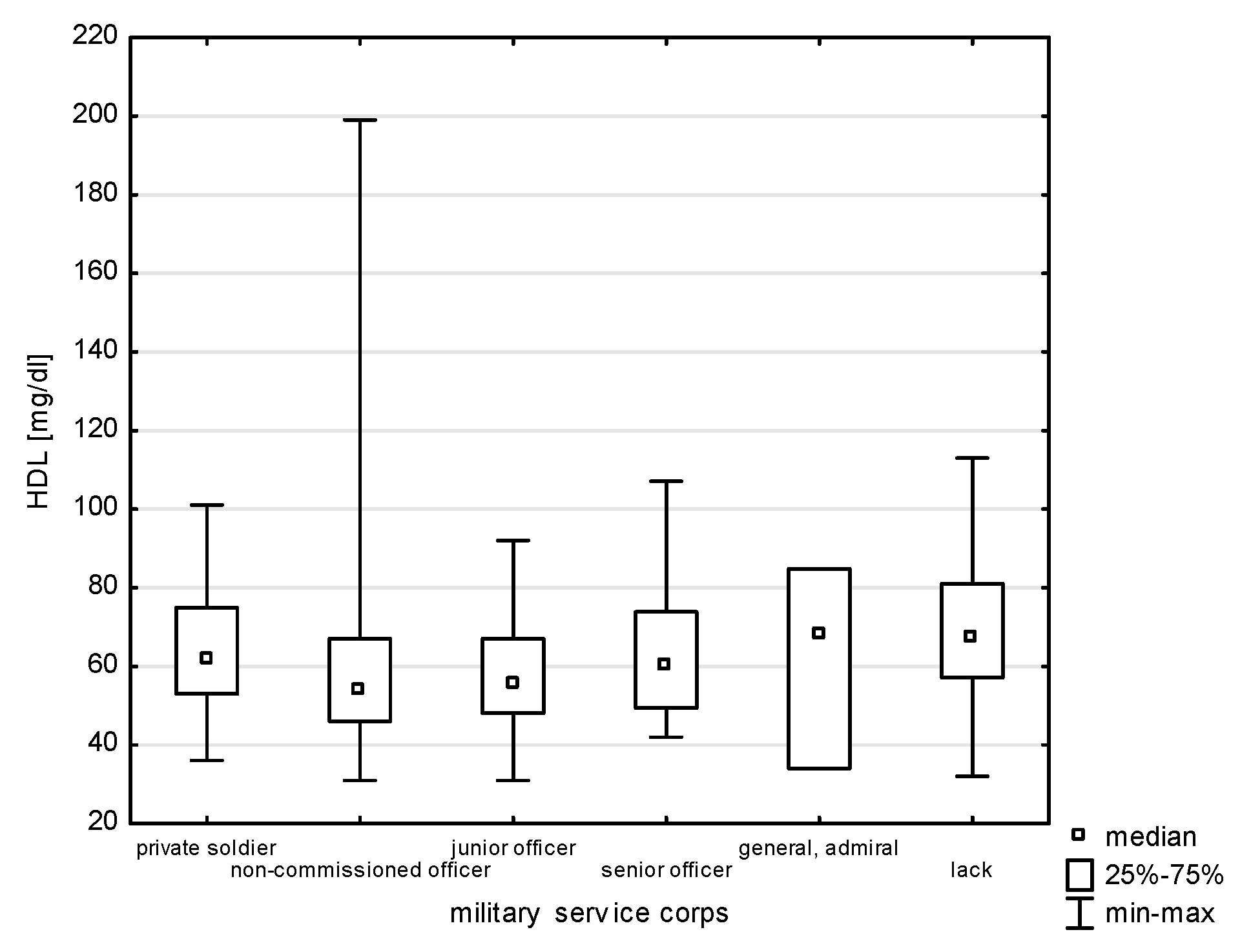
| HDL | 61.36 | 18.25 | 59.00 | 31.00 | 199.00 | 49.00 | 72.00 |
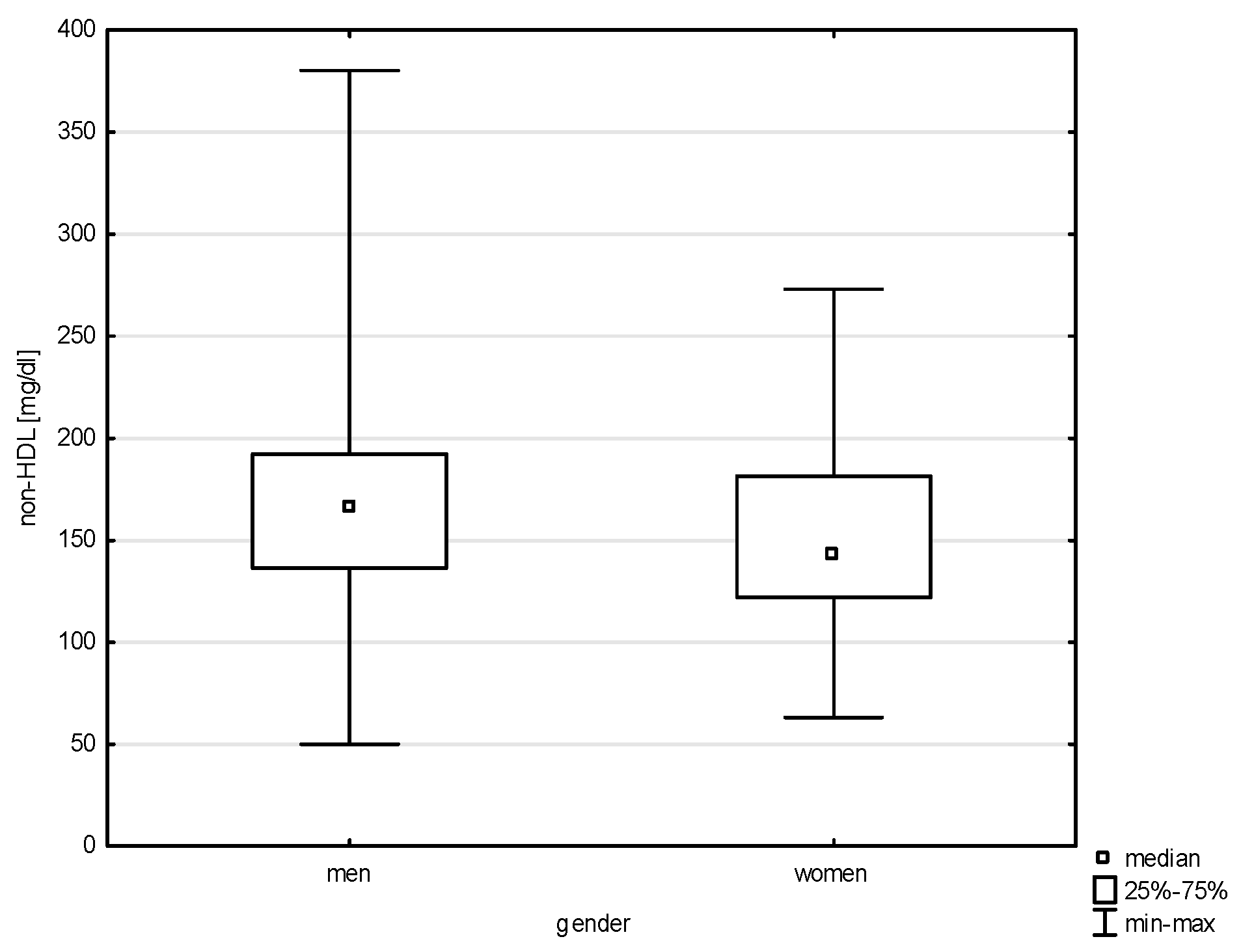
| non-HDL cholesterol | 160.80 | 44.66 | 161.50 | 50.00 | 380.20 | 128.90 | 190.00 |
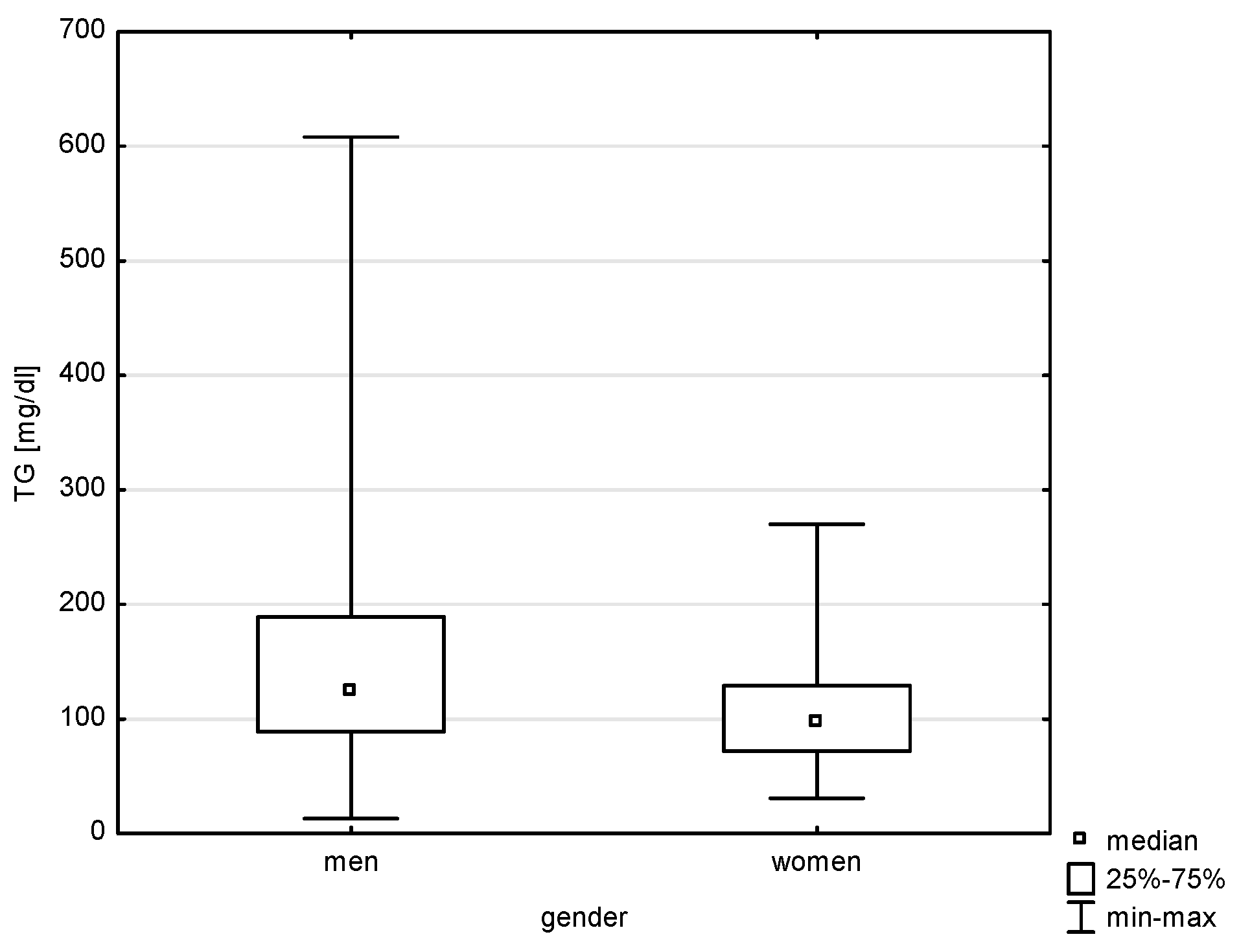
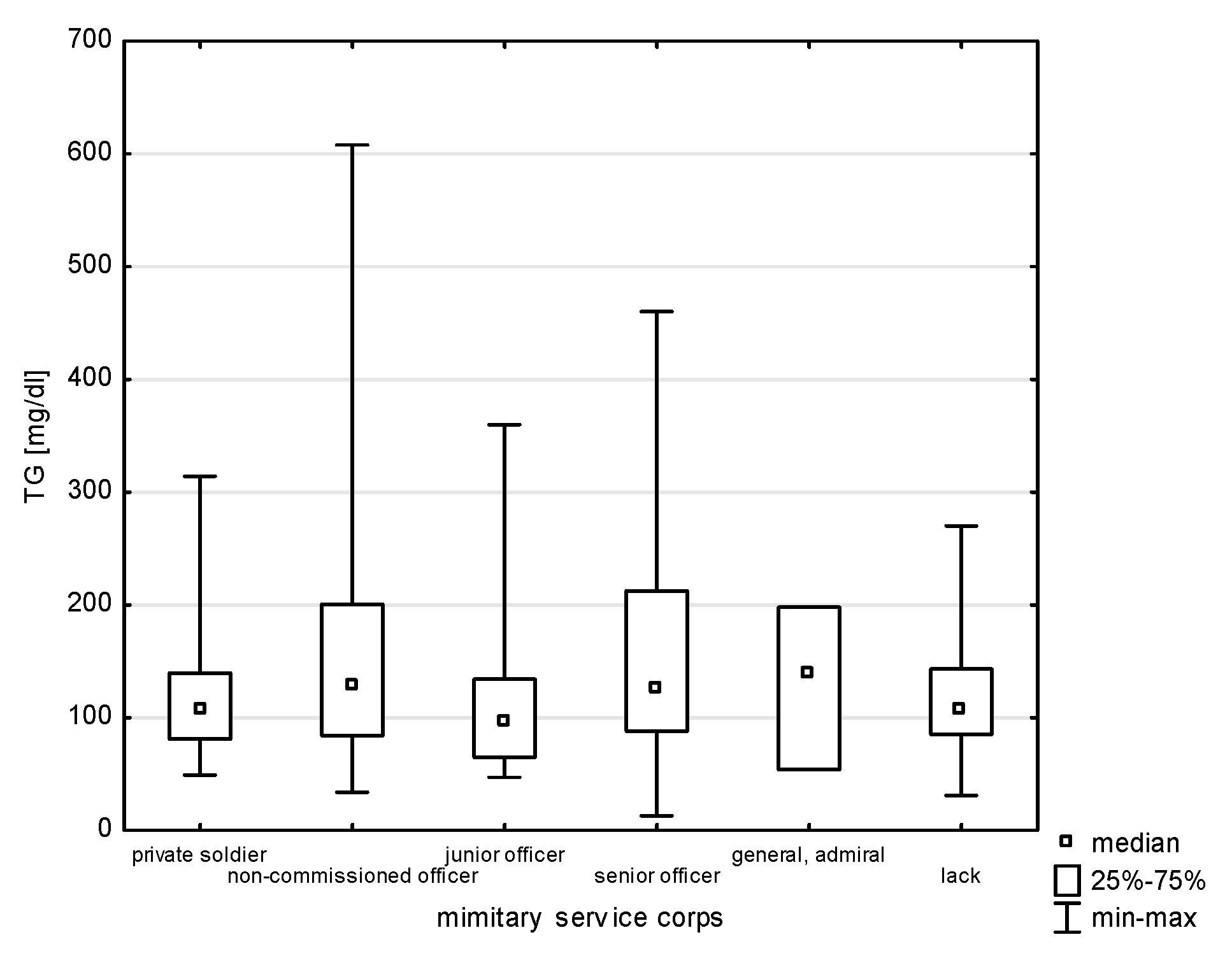
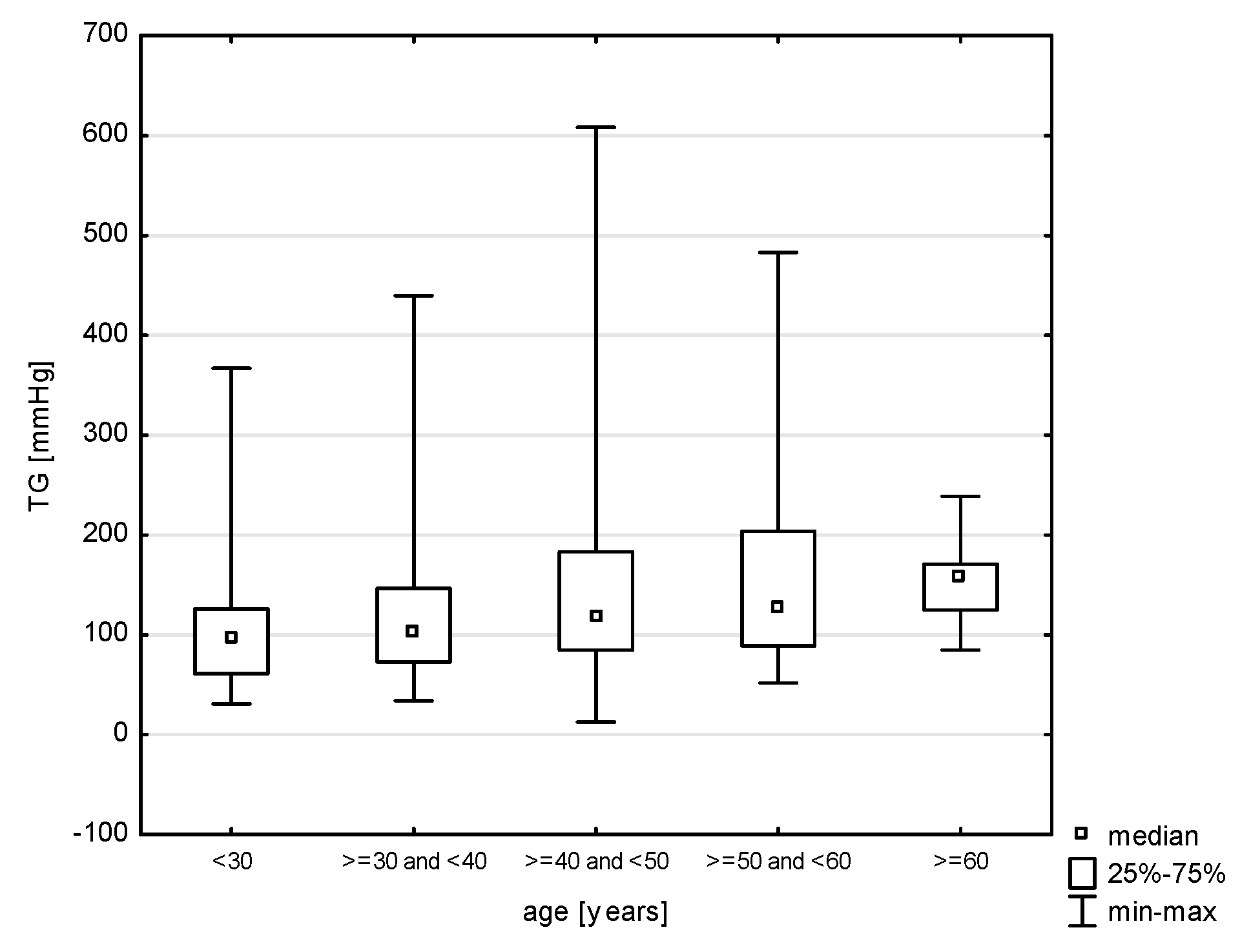
| TG | 141.42 | 91.53 | 114.55 | 13.00 | 608.00 | 82.00 | 171.50 |
| Variables | Military Service Corps [%] | ||||||
|---|---|---|---|---|---|---|---|
| Private Soldier | Non-Commissioned Officer | Junior Officer | Senior Officer | General, Admiral | Lack | ||
| chest pain | yes | 17.39 | 7.87 | 12.07 | 2.63 | - | 9.43 |
| no | 82.61 | 92.13 | 87.93 | 97.37 | 100.00 | 90.57 | |
| Statistics | Chi2 = 5.060, df = 5, p = 0.4085 | ||||||
| dyspnoea | yes | - | 3.94 | 3.45 | 5.26 | - | 11.32 |
| no | 100.00 | 96.06 | 96.55 | 94.74 | 100.00 | 88.68 | |
| Statistics | Chi2 = 6.467, df = 5, p = 0.2633 | ||||||
| dizziness | yes | 13.04 | 5.51 | 3.45 | 5.26 | - | 13.21 |
| no | 86.96 | 94.49 | 96.55 | 94.74 | 100.00 | 86.79 | |
| Statistics | Chi2 = 6.423, df = 5, p = 0.2671 | ||||||
| heart palpitations | yes | 8.70 | 11.81 | 8.62 | 7.89 | - | 16.98 |
| no | 91.30 | 88.19 | 91.38 | 92.11 | 100.00 | 83.02 | |
| Statistics | Chi2 = 3.142, df = 5, p = 0.6780 | ||||||
| pain in the lower limbs | yes | 4.35 | 8.66 | 5.17 | 2.63 | - | 15.09 |
| no | 95.65 | 91.34 | 94.83 | 97.37 | 100.00 | 84.91 | |
| Statistics | Chi2 = 6.533, df = 5, p = 0.2576 | ||||||
| headache | yes | 30.43 | 29.13 | 18.97 | 31.58 | - | 41.51 |
| no | 69.57 | 70.87 | 81.03 | 68.42 | 100.00 | 58.49 | |
| Statistics | Chi2 = 8.127, df = 5, p = 0.1493 | ||||||
| increased blood pressure | yes | 17.39 | 18.11 | 17.24 | 36.84 | - | 13.21 |
| no | 82.61 | 81.89 | 82.76 | 63.16 | 100.00 | 86.79 | |
| Statistics | Chi2 = 9.850, df = 5, p = 0.0795 | ||||||
| Variables | Military Service Corps [%] | ||||||
|---|---|---|---|---|---|---|---|
| Private Soldier | Non-Commissioned Officer | Junior Officer | Senior Officer | General, Admiral | Lack | ||
| overweight | yes | 8.70 | 33.86 | 28.81 | 45.95 | - | 22.00 |
| no | 91.30 | 66.14 | 71.19 | 54.05 | 100.00 | 78.00 | |
| Statistics | Chi2 = 12.260, df = 5, p = 0.0313 | ||||||
| obesity | yes | 17.39 | 15.75 | 8.47 | 16.22 | - | 18.00 |
| no | 82.61 | 84.25 | 91.53 | 83.78 | 100.00 | 82.00 | |
| Statistics | Chi2 = 2.721, df = 5, p = 0.7428 | ||||||
| incorrect diet | yes | 13.04 | 42.52 | 38.98 | 43.24 | - | 38.00 |
| no | 86.96 | 57.48 | 61.02 | 56.76 | 100.00 | 62.00 | |
| Statistics | Chi2 = 8.126, df = 5, p = 0.1493 | ||||||
| increased cholesterol levels | yes | 8.70 | 17.32 | 11.86 | 24.32 | - | 22.00 |
| no | 91.30 | 82.68 | 88.14 | 75.68 | 100.00 | 78.00 | |
| Statistics | Chi2 = 4.689, df = 5, p = 0.4548 | ||||||
| low physical activity | yes | 26.09 | 18.11 | 11.86 | 21.62 | - | 38.00 |
| no | 73.91 | 81.89 | 88.14 | 78.30 | 100.00 | 62.00 | |
| Statistics | Chi2 = 12.847, df = 5, p = 0.0248 | ||||||
| smoking | yes | 26.09 | 22.05 | 15.25 | 32.43 | - | 16.00 |
| no | 73.91 | 77.95 | 84.75 | 67.57 | 100.00 | 84.00 | |
| Statistics | Chi2 = 5.502, df = 5, p = 0.3576 | ||||||
| drinking alcohol | yes | 13.04 | 19.69 | 15.25 | 18.92 | - | 4.00 |
| no | 86.96 | 80.31 | 84.75 | 81.08 | 100.00 | 96.00 | |
| Statistics | Chi2 = 7.373, df = 5, p = 0.1942 | ||||||
| stress | yes | 56.52 | 47.24 | 61.02 | 67.57 | 100.00 | 54.00 |
| no | 43.48 | 52.76 | 38.98 | 32.43 | - | 46.00 | |
| Statistics | Chi2 = 7.477, df = 5, p = 0.1874 | ||||||
| Variables | Military Service Corps [%] | ||||||
|---|---|---|---|---|---|---|---|
| Private Soldier | Non-Commissioned Officer | Junior Officer | Senior Officer | General, Admiral | Lack | ||
| self-assessment of health | very good | 30.43 | 22.83 | 54.24 | 18.92 | - | 14.00 |
| good | 43.48 | 62.99 | 33.90 | 64.86 | 100.00 | 56.00 | |
| sufficient | 17.39 | 6.30 | 5.08 | 16.22 | - | 16.00 | |
| wrong | 4.35 | - | - | - | - | - | |
| no opinion | 4.35 | 7.87 | 6.78 | - | - | 14.00 | |
| Variables | Military Service Corps [%] | ||||||
|---|---|---|---|---|---|---|---|
| Private Soldier | Non-Commissioned Officer | Junior Officer | Senior Officer | General, Admiral | Lack | ||
| self-assessment of knowledge | very good | - | 0.79 | 3.39 | 5.26 | - | 4.00 |
| good | 22.73 | 27.78 | 18.64 | 21.05 | 100.00 | 30.00 | |
| sufficient | 63.64 | 53.97 | 64.41 | 65.79 | - | 42.00 | |
| below sufficient | 4.55 | 11.11 | 10.17 | 7.89 | - | 8.00 | |
| no opinion | 9.09 | 6.35 | 3.39 | - | - | 16.00 | |
| Variables | Military Service Corps [%] | ||||||
|---|---|---|---|---|---|---|---|
| Private Soldier | Non-Commissioned Officer | Junior Officer | Senior Officer | General, Admiral | Lack | ||
| readiness to increase knowledge | yes | 81.82 | 64.29 | 66.10 | 78.95 | 100.00 | 62.75 |
| no | - | 9.52 | 8.47 | 7.89 | - | 5.88 | |
| no opinion | 18.18 | 26.19 | 25.42 | 13.16 | - | 31.37 | |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Zawadzka, M.; Ejchman-Pac, E.; Kowalska, A.; Szymański, P.; Marszałkowska-Jakubik, J. Epidemiological Analysis of Cardiovascular Diseases with Consideration of Risk Factors, Health Awareness, and Preventive Behaviors in Civilian and Military Populations. J. Clin. Med. 2025, 14, 5844. https://doi.org/10.3390/jcm14165844
Zawadzka M, Ejchman-Pac E, Kowalska A, Szymański P, Marszałkowska-Jakubik J. Epidemiological Analysis of Cardiovascular Diseases with Consideration of Risk Factors, Health Awareness, and Preventive Behaviors in Civilian and Military Populations. Journal of Clinical Medicine. 2025; 14(16):5844. https://doi.org/10.3390/jcm14165844
Chicago/Turabian StyleZawadzka, Magdalena, Ewelina Ejchman-Pac, Amelia Kowalska, Paweł Szymański, and Justyna Marszałkowska-Jakubik. 2025. "Epidemiological Analysis of Cardiovascular Diseases with Consideration of Risk Factors, Health Awareness, and Preventive Behaviors in Civilian and Military Populations" Journal of Clinical Medicine 14, no. 16: 5844. https://doi.org/10.3390/jcm14165844
APA StyleZawadzka, M., Ejchman-Pac, E., Kowalska, A., Szymański, P., & Marszałkowska-Jakubik, J. (2025). Epidemiological Analysis of Cardiovascular Diseases with Consideration of Risk Factors, Health Awareness, and Preventive Behaviors in Civilian and Military Populations. Journal of Clinical Medicine, 14(16), 5844. https://doi.org/10.3390/jcm14165844







