Long-Term Effectiveness of a Monofocal Intraocular Lens (IOL) Enhanced for Intermediate Vision: A 5-Year Follow-Up Study
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design and Patients
2.2. Intraocular Lens
2.3. Surgical Technique
2.4. Postoperative Evaluation
2.5. Statistical Analysis
3. Results
3.1. PCO Development
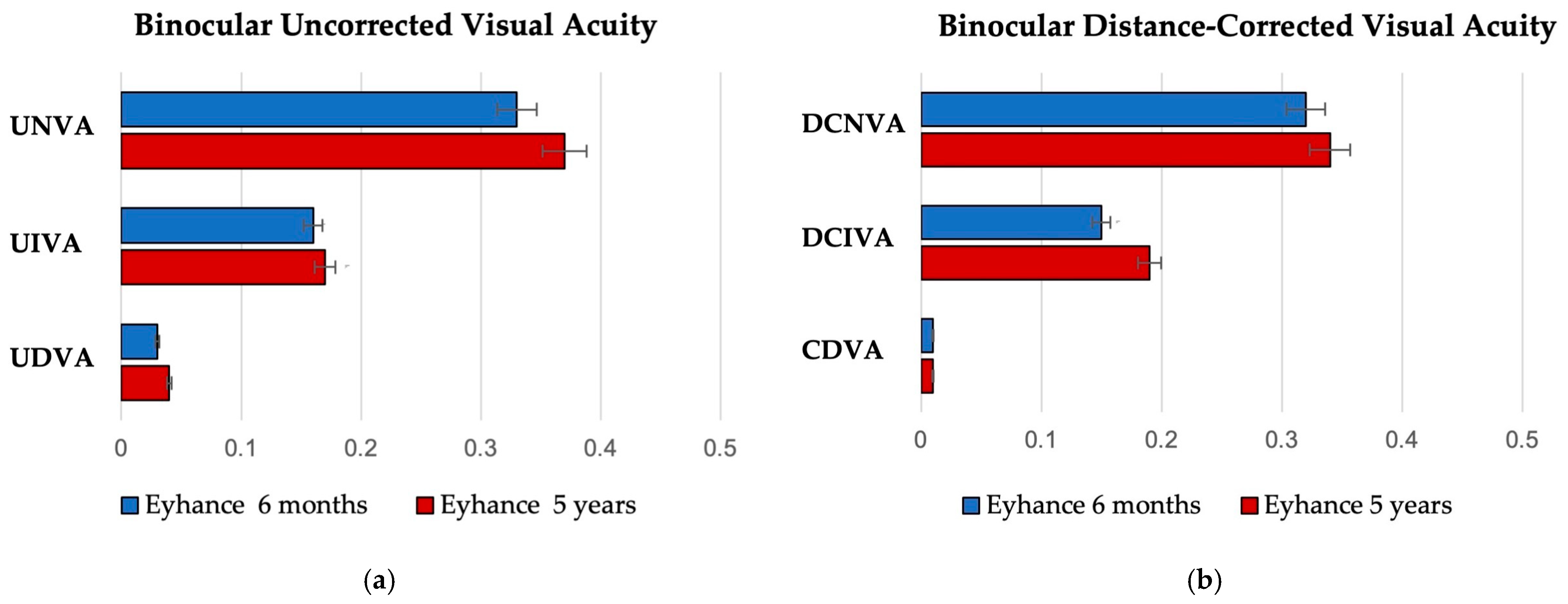
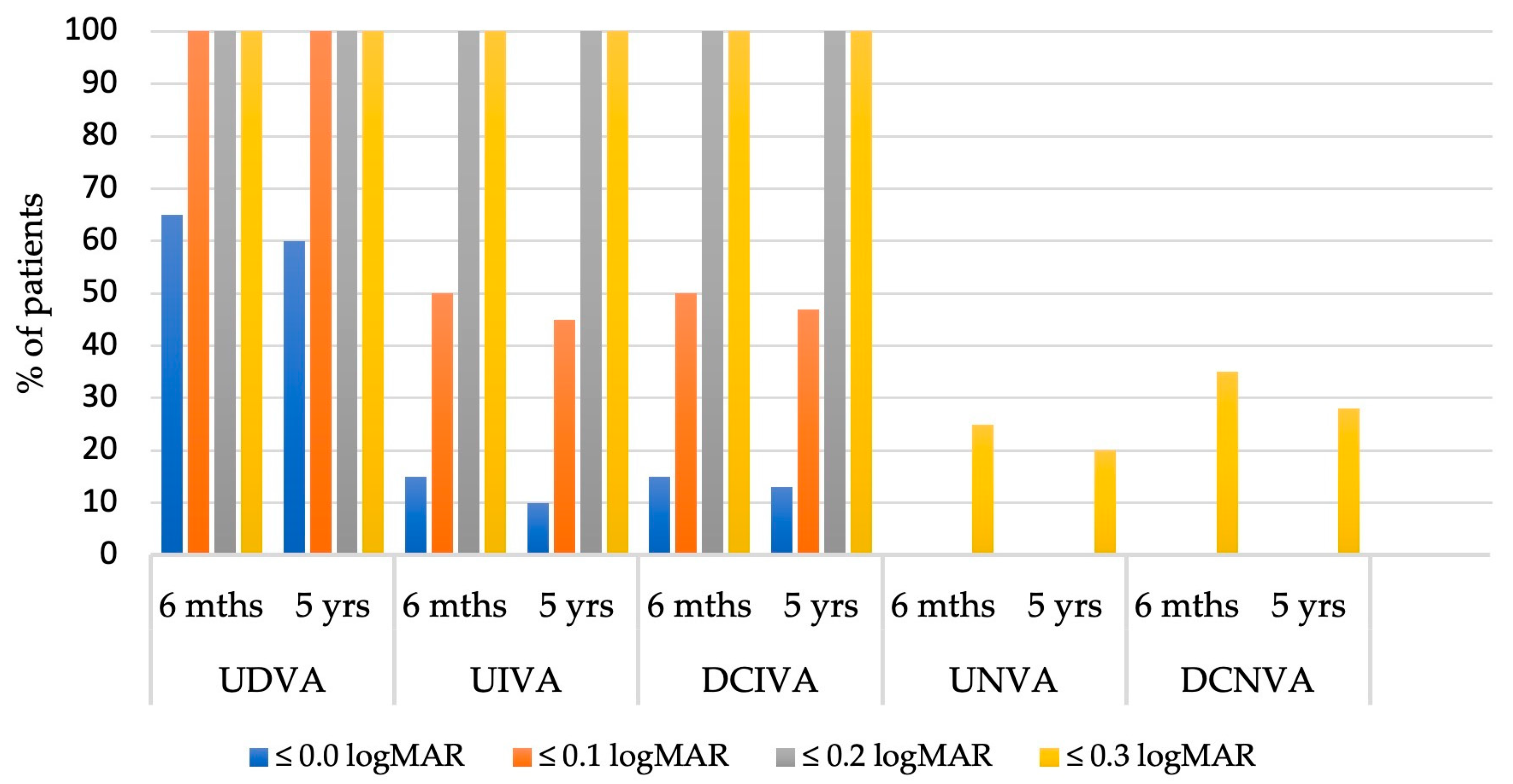
3.2. Visual Outcomes
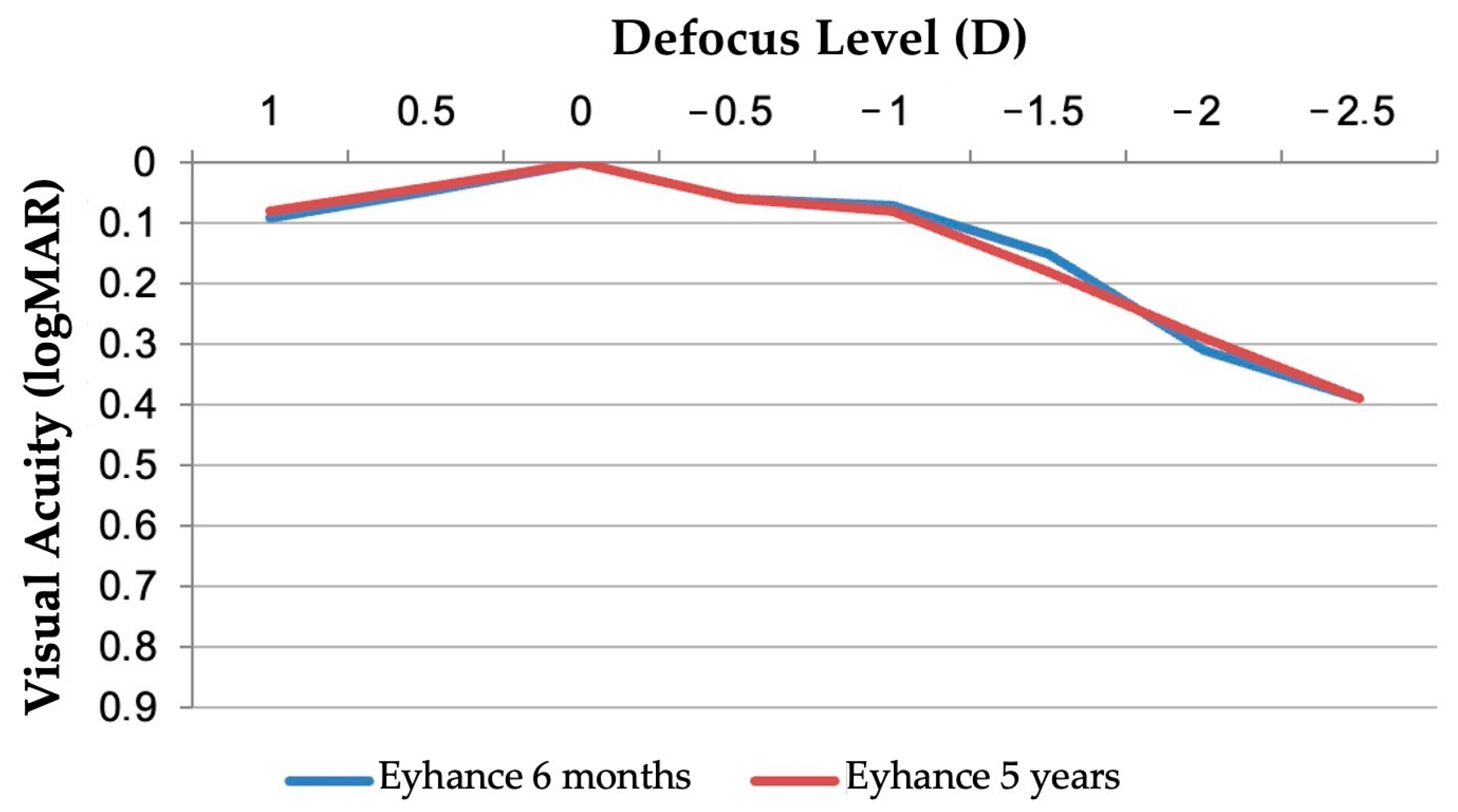
3.3. Binocular Defocus Curve
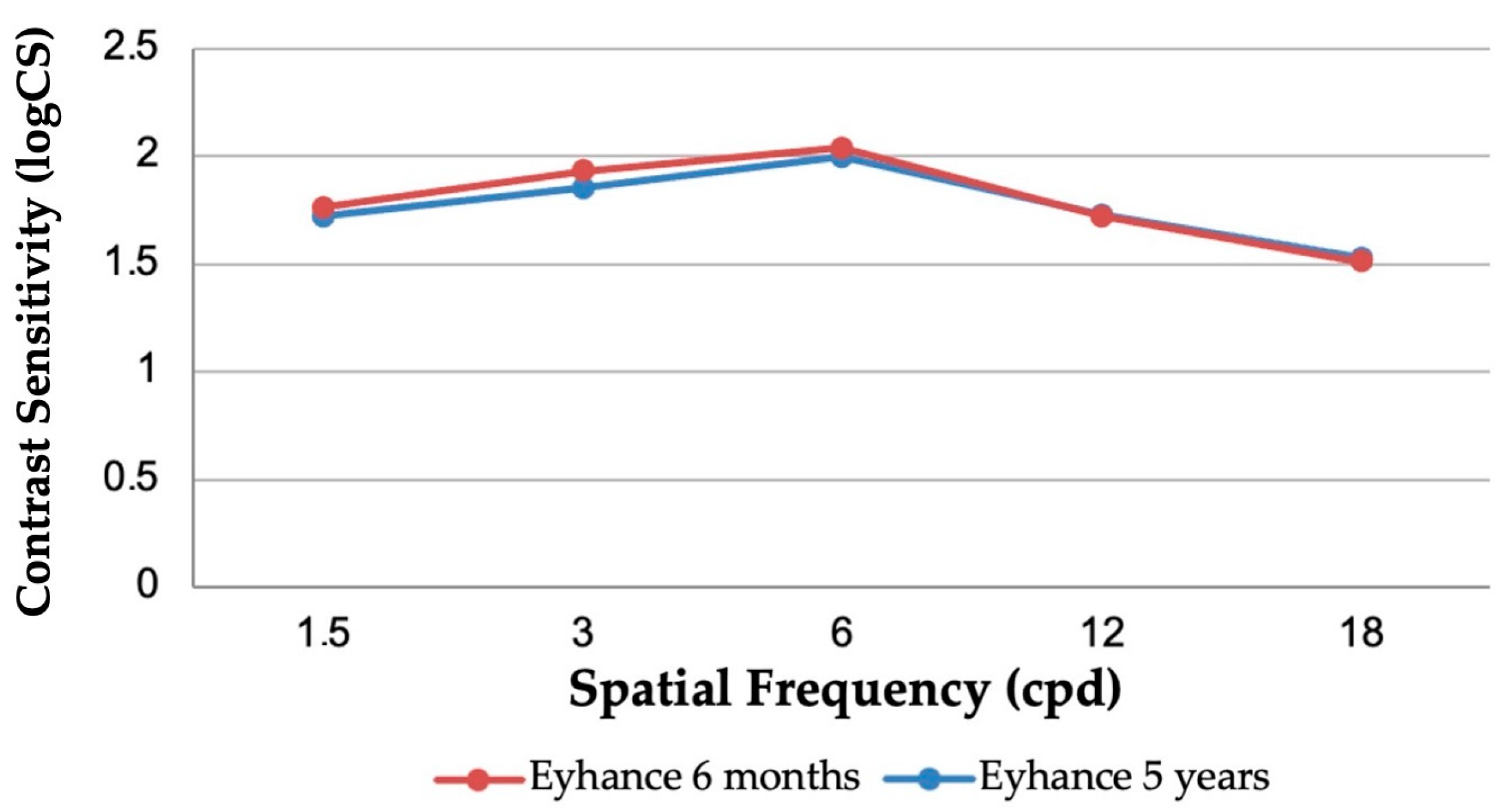
3.4. Contrast Sensitivity
3.5. Optical Quality Parameters
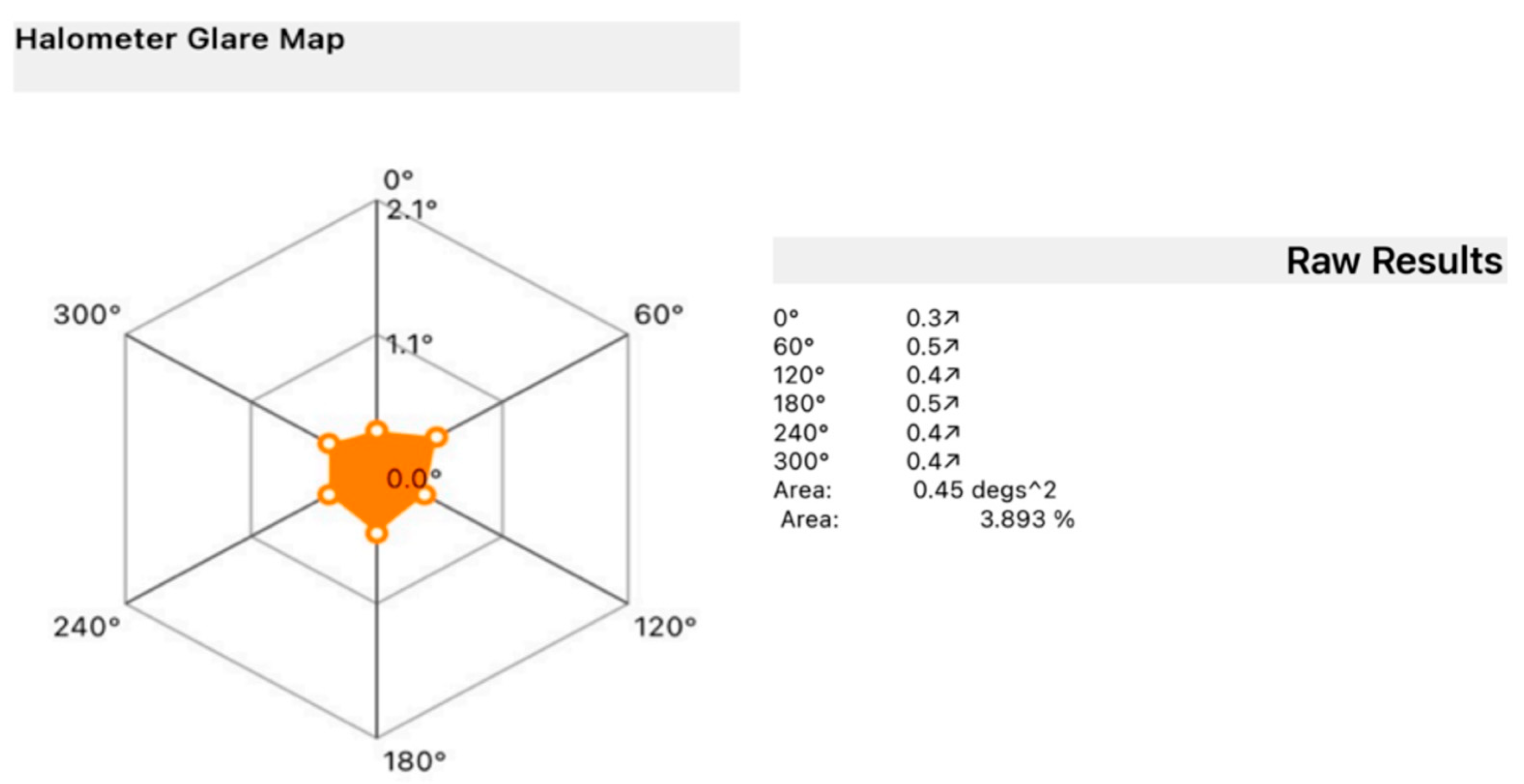
3.6. Halo Size
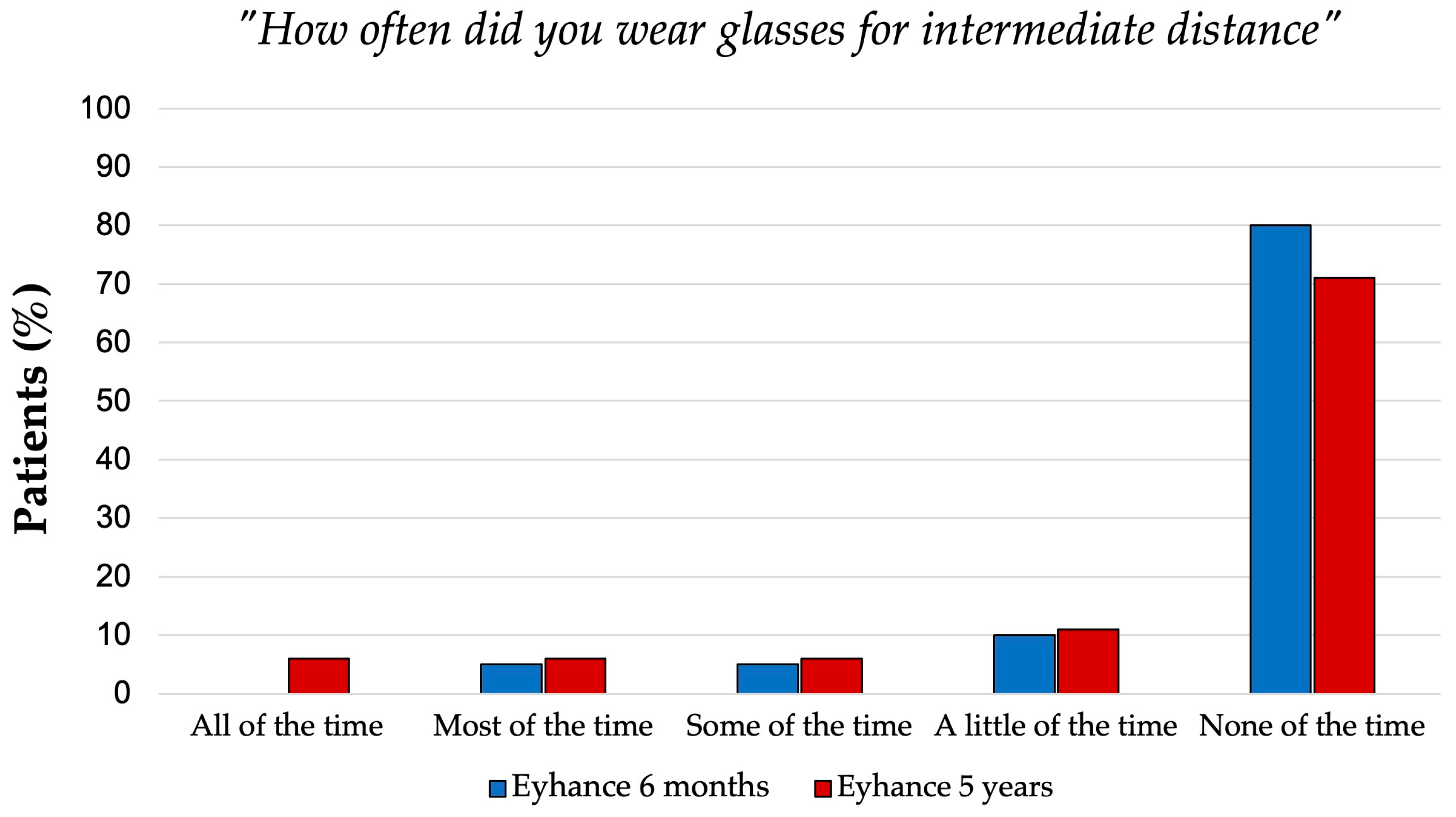
3.7. Glare Perception and Spectacle Independence
3.8. Effective Lens Position (ELP)
4. Discussion
4.1. Posterior Capsular Opacification and IOL Design Considerations
4.2. Long-Term Visual and Optical Performance
4.3. Effective Lens Position (ELP) Stability
4.4. Patient-Reported Outcomes and Spectacle Independence
4.5. Study Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Ribeiro, F.; Dick, H.B.; Kohnen, T.; Findl, O.; Nuijts, R.; Cochener, B.; Fernández, J. Evidence-Based Functional Classification of Simultaneous Vision Intraocular Lenses: Seeking a Global Consensus by the ESCRS Functional Vision Working Group. J. Cataract. Refract. Surg. 2024, 50, 794–798. [Google Scholar] [CrossRef] [PubMed]
- Wan, K.H.; Au, A.C.K.; Kua, W.N.; Ng, A.L.K.; Cheng, G.P.M.; Lam, N.M.; Chow, V.W.S. Enhanced Monofocal Versus Conventional Monofocal Intraocular Lens in Cataract Surgery: A Meta-Analysis. J. Refract. Surg. 2022, 38, 538–546. [Google Scholar] [CrossRef] [PubMed]
- Mencucci, R.; Cennamo, M.; Venturi, D.; Vignapiano, R.; Favuzza, E. Visual Outcome, Optical Quality, and Patient Satisfaction with a New Monofocal IOL, Enhanced for Intermediate Vision: Preliminary Results. J. Cataract. Refract. Surg. 2020, 46, 378–387. [Google Scholar] [CrossRef] [PubMed]
- Vega, F.; Millán, M.S.; Gil, M.A.; Garzón, N. Optical Performance of a Monofocal Intraocular Lens Designed to Extend Depth of Focus. J. Refract. Surg. 2020, 36, 625–632. [Google Scholar] [CrossRef]
- Alarcon, A.; Cánovas, C.; Koopman, B.; Weeber, H.; Auffarth, G.U.; Piers, P.A. Enhancing the Intermediate Vision of Monofocal Intraocular Lenses Using a Higher Order Aspheric Optic. J. Refract. Surg. 2020, 36, 520–527. [Google Scholar] [CrossRef]
- Hoffer, K.J.; Savini, G. IOL Power Calculation in Short and Long Eyes. Asia-Pac. J. Ophthalmol. 2017, 6, 330–331. [Google Scholar] [CrossRef]
- Kane, J.X.; Chang, D.F. Intraocular Lens Power Formulas, Biometry, and Intraoperative Aberrometry: A Review. Ophthalmology 2021, 128, e94–e114. [Google Scholar] [CrossRef]
- Artal, P.; Benito, A.; Pérez, G.M.; Alcón, E.; de Casas, Á.; Pujol, J.; Marín, J.M. An Objective Scatter Index Based on Double-Pass Retinal Images of a Point Source to Classify Cataracts. PLoS ONE 2011, 6, e16823. [Google Scholar] [CrossRef]
- Buckhurst, P.J.; Naroo, S.A.; Davies, L.N.; Shah, S.; Buckhurst, H.; Kingsnorth, A.; Drew, T.; Wolffsohn, J.S. Tablet App Halometer for the Assessment of Dysphotopsia. J. Cataract. Refract. Surg. 2015, 41, 2424–2429. [Google Scholar] [CrossRef]
- Hays, R.D.; Mangione, C.M.; Ellwein, L.; Lindblad, A.S.; Spritzer, K.L.; McDonnell, P.J. Psychometric Properties of the National Eye Institute-Refractive Error Quality of Life Instrument. Ophthalmology 2003, 110, 2292–2301. [Google Scholar] [CrossRef]
- Morlock, R.; Wirth, R.J.; Tally, S.R.; Garufis, C.; Heichel, C.W.D. Patient-Reported Spectacle Independence Questionnaire (PRSIQ): Development and Validation. Am. J. Ophthalmol. 2017, 178, 101–114. [Google Scholar] [CrossRef]
- Khoramnia, R.; Kretz, F.T.A.; Gerl, M.; Breyer, D.; Auffarth, G.U. Long-Term Clinical Outcomes After Bilateral Implantation of Two Trifocal Diffractive IOLs. J. Refract. Surg. 2023, 39, 798–807. [Google Scholar] [CrossRef]
- Shafer, B.M.; McCabe, C.; Reiser, H.; Newsom, T.H.; Berdahl, J. The REVIVE Study: Long Term Outcomes of a Novel Non-Diffractive Extended Vision IOL versus Monofocal Control IOL. Clin. Ophthalmol. 2022, 16, 3945–3950. [Google Scholar] [CrossRef]
- Awasthi, N.; Guo, S.; Wagner, B.J. Posterior Capsular Opacification: A Problem Reduced but Not yet Eradicated. Arch. Ophthalmol. 2009, 127, 555–562. [Google Scholar] [CrossRef] [PubMed]
- Apple, D.J.; Peng, Q.; Visessook, N.; Werner, L.; Pandey, S.K.; Escobar-Gomez, M.; Ram, J.; Auffarth, G.U. Eradication of Posterior Capsule Opacification: Documentation of a Marked Decrease in Nd:YAG Laser Posterior Capsulotomy Rates Noted in an Analysis of 5416 Pseudophakic Human Eyes Obtained Postmortem. Ophthalmology 2001, 108, 505–518. [Google Scholar] [CrossRef] [PubMed]
- Zhao, Y.; Yang, K.; Li, J.; Huang, Y.; Zhu, S. Comparison of Hydrophobic and Hydrophilic Intraocular Lens in Preventing Posterior Capsule Opacification after Cataract Surgery An Updated Meta-Analysis. Medicine 2017, 96, e8301. [Google Scholar] [CrossRef] [PubMed]
- Mencucci, R.; Favuzza, E.; Boccalini, C.; Gicquel, J.J.; Raimondi, L. Square-Edge Intraocular Lenses and Epithelial Lens Cell Proliferation: Implications on Posterior Capsule Opacification in an in Vitro Model. BMC Ophthalmol. 2015, 15, 5. [Google Scholar] [CrossRef]
- Auffarth, G.U.; Gerl, M.; Tsai, L.; Janakiraman, D.P.; Jackson, B.; Alarcon, A.; Dick, H.B. Clinical Evaluation of a New Monofocal IOL with Enhanced Intermediate Function in Patients with Cataract. J. Cataract. Refract. Surg. 2021, 47, 184–191. [Google Scholar] [CrossRef]
- Kanclerz, P.; Toto, F.; Grzybowski, A.; Alio, J.L. Extended Depth-of-Field Intraocular Lenses: An Update. Asia-Pac. J. Ophthalmol. 2020, 9, 194–202. [Google Scholar] [CrossRef]
- Gigon, E.; Bouthour, W.; Panos, G.D.; Pajic, B.; Massa, H. Real World Outcomes of the New Tecnis Eyhance IOL. Eur. J. Ophthalmol. 2022, 33, 1390. [Google Scholar] [CrossRef]
- Dołowiec-Kwapisz, A.; Piotrowska, H.; Misiuk-Hojło, M. Evaluation of Visual and Patient—Reported Outcomes, Spectacle Dependence after Bilateral Implantation with a Non-Diffractive Extended Depth of Focus Intraocular Lens Compared to Other Intraocular Lenses. J. Clin. Med. 2022, 11, 5246. [Google Scholar] [CrossRef] [PubMed]
- Reinhard, T.; Maier, P.; Böhringer, D.; Bertelmann, E.; Brockmann, T.; Kiraly, L.; Salom, D.; Piovella, M.; Colonval, S.; Mendicute, J. Comparison of Two Extended Depth of Focus Intraocular Lenses with a Monofocal Lens: A Multi-Centre Randomised Trial. Graefe’s Arch. Clin. Exp. Ophthalmol. 2020, 259, 431. [Google Scholar] [CrossRef] [PubMed]
- Olsen, T. Calculation of Intraocular Lens Power: A Review. Acta Ophthalmol. Scand. 2007, 85, 472–485. [Google Scholar] [CrossRef] [PubMed]
- Khoramnia, R.; Auffarth, G.; Łabuz, G.; Pettit, G.; Suryakumar, R. Refractive Outcomes after Cataract Surgery. Diagnostics 2022, 12, 243. [Google Scholar] [CrossRef]
- Xiao, Z.; Wang, G.; Zhen, M.; Zhao, Z. Stability of Intraocular Lens With Different Haptic Design: A Swept-Source Optical Coherence Tomography Study. Front. Med. 2021, 8, 705873. [Google Scholar] [CrossRef]
- Schrecker, J.; Schröder, S.; Eppig, T.; Daas, L.; Langenbucher, A. Impact of Intraocular Lens Displacement on the Fixation Axis. J. Opt. Soc. Am. A. Opt. Image Sci. Vis. 2018, 35, 561–566. [Google Scholar] [CrossRef]
- Wu, J.; Yang, C.; Yin, Y.; Liu, L.; Wang, H. Impact of Material and Lens Design on Repositioning Surgery of Toric Intraocular Lenses: A Single-Arm Meta-Analysis. J. Ophthalmol. 2022, 2022, 6699596. [Google Scholar] [CrossRef]
- Buckhurst, P.J.; Naroo, S.A.; Davies, L.N.; Shah, S.; Drew, T.; Wolffsohn, J.S. Assessment of Dysphotopsia in Pseudophakic Subjects with Multifocal Intraocular Lenses. BMJ Open Ophthalmol. 2017, 1, e000064. [Google Scholar] [CrossRef]
| Parameter | Eyhance 6 Months | Eyhance 5 Years |
|---|---|---|
| Number of patients (eyes) | 20 (40) | 18 (36) |
| Age (years) | ||
| Mean ± SD | 72.3 ± 6.7 | 77.4 ± 5.5 |
| Median (range) | 72 (60–85) | 77 (65–89) |
| Sex | ||
| Male | 9 | 8 |
| Female | 11 | 10 |
| Follow-up time (years) | 0.5 ± 0.1 | 5.6 ± 0.4 |
| 6-Month Follow-Up | 5-Year Follow-Up | p Value | |
|---|---|---|---|
| UDVA monocular | |||
| Mean ± SD | 0.04 ± 0.05 | 0.06 ± 0.05 | 0.188 |
| CDVA monocular | |||
| Mean ± SD | 0.02 ± 0.04 | 0.03 ± 0.09 | 0.447 |
| UDVA binocular | |||
| Mean ± SD | 0.03 ± 0.05 | 0.04 ± 0.05 | 0.358 |
| CDVA binocular | |||
| Mean ± SD | 0.01 ± 0.04 | 0.01 ± 0.01 | 0.748 |
| UIVA monocular | |||
| Mean ± SD | 0.28 ± 0.11 | 0.28 ± 0.10 | 0.534 |
| DCIVA monocular | |||
| Mean ± SD | 0.27 ± 0.11 | 0.25 ± 0.09 | 0.819 |
| CIVA monocular | |||
| Mean ± SD | 0.06 ± 0.09 | 0.07 ± 0.08 | 0.384 |
| UIVA binocular | |||
| Mean ± SD | 0.16 ± 0.10 | 0.17 ± 0.05 | 0.323 |
| DCIVA binocular | |||
| Mean ± SD | 0.15 ± 0.08 | 0.19 ± 0.05 | 0.180 |
| CIVA binocular | |||
| Mean ± SD | 0.04 ± 0.05 | 0.06 ± 0.05 | 0.483 |
| UNVA monocular | |||
| Mean ± SD | 0.46 ± 0.13 | 0.48 ± 0.14 | 0.630 |
| DCNVA monocular | |||
| Mean ± SD | 0.44 ± 0.05 | 0.44 ± 0.14 | 0.840 |
| CNVA monocular | |||
| Mean ± SD | 0.06 ± 0.08 | 0.05 ± 0.07 | 0.770 |
| UNVA binocular | |||
| Mean ± SD | 0.33 ± 0.05 | 0.37 ± 0.05 | 0.623 |
| DCNVA binocular | |||
| Mean ± SD | 0.32 ± 0.04 | 0.34 ± 0.07 | 0.900 |
| CNVA binocular | |||
| Mean ± SD | 0.03 ± 0.05 | 0.02 ± 0.04 | 0.867 |
| Eyhance 6 Months | Eyhance 5 Years | p Value | |
|---|---|---|---|
| OSI | 1.36 ± 0.63 | 1.45 ± 0.51 | 0.139 |
| MTF cutoff (c/deg) | 31.28 ± 8.70 | 31.34 ± 4.02 | 0.659 |
| Strehl ratio | 0.17 ± 0.04 | 0.16 ± 0.04 | 0.124 |
| Average Halo Size (Degrees2) | Numbers of Eyes (n) |
|---|---|
| 0.31–0.4 | 3 |
| 0.41–0.5 | 8 |
| 0.51–0.6 | 17 |
| 0.61–0.7 | 5 |
| 0.71–0.8 | 2 |
| 0.81–0.9 | - |
| >0.91 | 1 |
| Eyhance 6 Months n (%) | Eyhance 5 Years n (%) | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Cat. 1 | Cat 2. | Cat. 3 | Cat. 4 | Cat. 5 | Cat. 1 | Cat. 2 | Cat. 3 | Cat. 4 | Cat. 5 | ||
| Did you need glasses for: | Distance | - | 20 (100%) | - | - | - | - | 18 (100%) | - | - | - |
| Intermediate | 4 (20%) | 16 (80%) | - | - | - | 4 (22%) | 14 (78%) | - | - | - | |
| Near | 19 (95%) | 1 (5%) | - | - | - | 18 (100%) | - | - | - | - | |
| How often did you wear glasses or contacts for: | Distance | - | - | - | - | 20 (100%) | - | - | - | - | 18 (100%) |
| Intermediate | - | 1 (5%) | 1 (5%) | 2 (10%) | 16 (80%) | 1 (6%) | 1 (6%) | 1 (6%) | 2 (11%) | 13 (71%) | |
| Near | 8 (40%) | 4 (20%) | 4 (20%) | 2 (10%) | 2 (10%) | 8 (45%) | 2 (11%) | 2 (11%) | 4 (22%) | 2 (11%) | |
| Were you able to function comfortably without glasses or contacts for: | Distance | 20 (100%) | - | - | - | - | 18 (100%) | - | - | - | - |
| Intermediate | 12 (60%) | 4 (20%) | 2 (10%) | 2 (10%) | - | 14 (78%) | - | 4 (22%) | - | - | |
| Near | - | 1 (5%) | 3 (15%) | 4 (20%) | 12 (60%) | - | 2 (11%) | 5 (28%) | 9 (50%) | 2 (11%) | |
| 6 Months | 5 Years | p Value | |
|---|---|---|---|
| ELP (mm) | 4.08 ± 0.21 | 4.15 ± 0.15 | 0.298 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Mencucci, R.; Romualdi, G.; Carnicci, A.; Panini, F.; Buzzi, M.; Giansanti, F. Long-Term Effectiveness of a Monofocal Intraocular Lens (IOL) Enhanced for Intermediate Vision: A 5-Year Follow-Up Study. J. Clin. Med. 2025, 14, 5831. https://doi.org/10.3390/jcm14165831
Mencucci R, Romualdi G, Carnicci A, Panini F, Buzzi M, Giansanti F. Long-Term Effectiveness of a Monofocal Intraocular Lens (IOL) Enhanced for Intermediate Vision: A 5-Year Follow-Up Study. Journal of Clinical Medicine. 2025; 14(16):5831. https://doi.org/10.3390/jcm14165831
Chicago/Turabian StyleMencucci, Rita, Giovanni Romualdi, Alberto Carnicci, Fabio Panini, Matilde Buzzi, and Fabrizio Giansanti. 2025. "Long-Term Effectiveness of a Monofocal Intraocular Lens (IOL) Enhanced for Intermediate Vision: A 5-Year Follow-Up Study" Journal of Clinical Medicine 14, no. 16: 5831. https://doi.org/10.3390/jcm14165831
APA StyleMencucci, R., Romualdi, G., Carnicci, A., Panini, F., Buzzi, M., & Giansanti, F. (2025). Long-Term Effectiveness of a Monofocal Intraocular Lens (IOL) Enhanced for Intermediate Vision: A 5-Year Follow-Up Study. Journal of Clinical Medicine, 14(16), 5831. https://doi.org/10.3390/jcm14165831








