Retrograde Vital Pulp Treatment in External Root Resorption Due to Third Molar Impaction: A Proof-of-Concept and Case Report
Abstract
1. Introduction
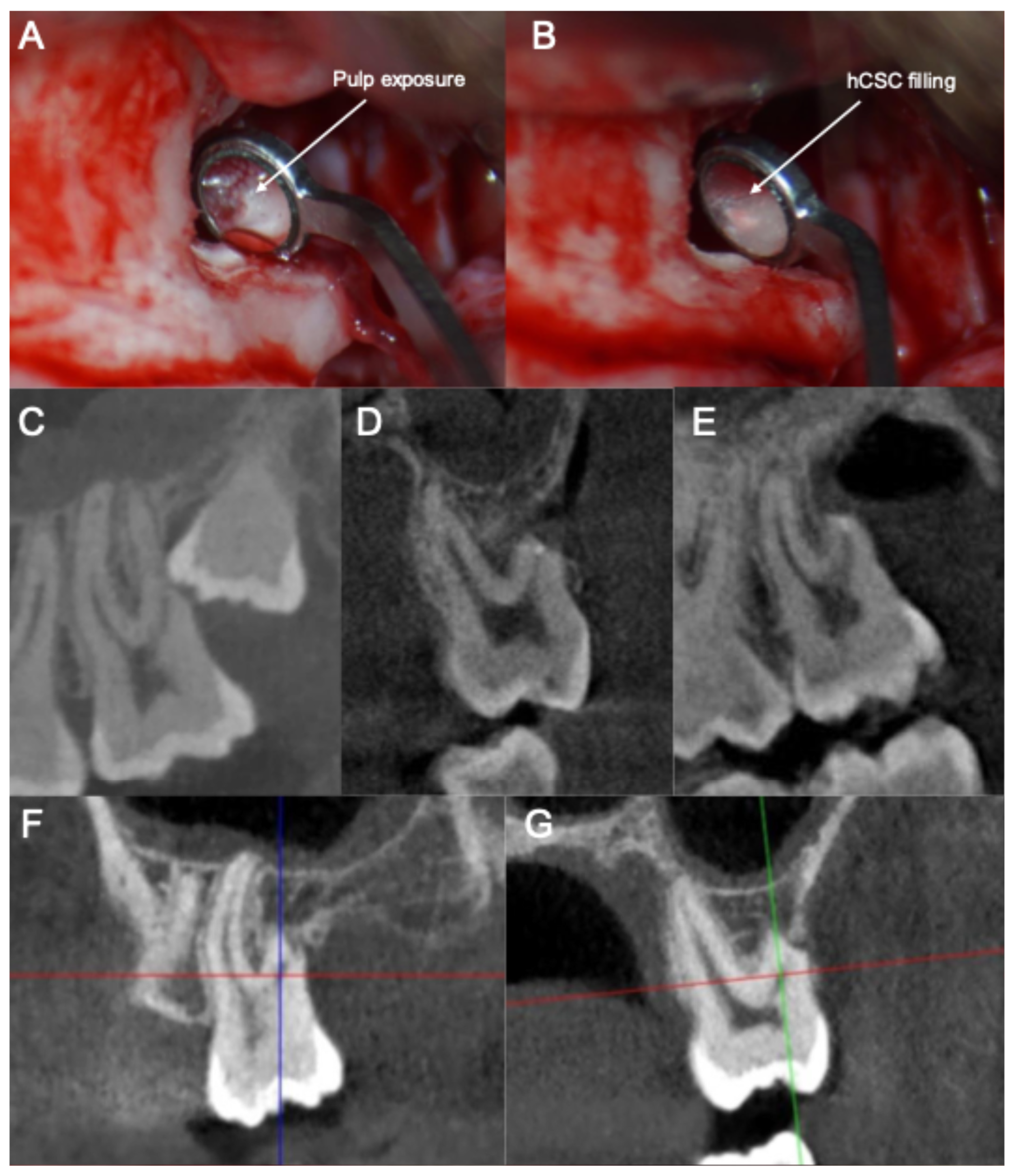
2. Case Report
2.1. Patient History and Chief Complaint
2.2. Diagnosis
2.3. Treatment Plan and Execution
- (1)
- The smoothening of the ERR to allow for a clear visualization and access to the pulp exposure.
- (2)
- The creation of a retrograde cavity and partial pulpotomy of the pulp exposure.
- (3)
- The placement of a pulp capping agent in the cavity over the remaining vital pulp tissue.
2.4. Follow-Up
3. Discussion
4. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Kazeminia, M.; Abdi, A.; Shohaimi, S.; Jalali, R.; Vaisi-Raygani, A.; Salari, N.; Mohammadi, M. Dental Caries in Primary and Permanent Teeth in Children’s Worldwide, 1995 to 2019: A Systematic Review and Meta-Analysis. Head Face Med. 2020, 16, 22. [Google Scholar] [CrossRef]
- Levin, L.; Day, P.F.; Hicks, L.; O’Connell, A.; Fouad, A.F.; Bourguignon, C.; Abbott, P.V. International Association of Dental Traumatology Guidelines for the Management of Traumatic Dental Injuries: General Introduction. Dent. Traumatol. 2020, 36, 309–313. [Google Scholar] [CrossRef] [PubMed]
- Călin, C.; Sajin, M.; Moldovan, V.T.; Coman, C.; Stratul, S.I.; Didilescu, A.C. Immunohistochemical Expression of Non-Collagenous Extracellular Matrix Molecules Involved in Tertiary Dentinogenesis Following Direct Pulp Capping: A Systematic Review. Ann. Anat. Anat. Anz. 2021, 235, 151674. [Google Scholar] [CrossRef]
- Ricucci, D.; Loghin, S.; Lin, L.M.; Spångberg, L.S.W.; Tay, F.R. Is Hard Tissue Formation in the Dental Pulp after the Death of the Primary Odontoblasts a Regenerative or a Reparative Process? J. Dent. 2014, 42, 1156–1170. [Google Scholar] [CrossRef] [PubMed]
- da Rosa, W.L.O.; Piva, E.; da Silva, A.F. Disclosing the Physiology of Pulp Tissue for Vital Pulp Therapy. Int. Endod. J. 2018, 51, 829–846. [Google Scholar] [CrossRef] [PubMed]
- Ricucci, D.; Siqueira, J.F.; Li, Y.; Tay, F.R. Vital Pulp Therapy: Histopathology and Histobacteriology-Based Guidelines to Treat Teeth with Deep Caries and Pulp Exposure. J. Dent. 2019, 86, 41–52. [Google Scholar] [CrossRef]
- Bjørndal, L.; Simon, S.; Tomson, P.L.; Duncan, H.F. Management of Deep Caries and the Exposed Pulp. Int. Endod. J. 2019, 52, 949–973. [Google Scholar] [CrossRef]
- Duncan, H.F. Present Status and Future Directions—Vital Pulp Treatment and Pulp Preservation Strategies. Int. Endod. J. 2022, 55, 497–511. [Google Scholar] [CrossRef]
- Ramani, A.; Sangwan, P.; Tewari, S.; Duhan, J.; Mittal, S.; Kumar, V. Comparative Evaluation of Complete and Partial Pulpotomy in Mature Permanent Teeth with Symptomatic Irreversible Pulpitis: A Randomized Clinical Trial. Int. Endod. J. 2022, 55, 430–440. [Google Scholar] [CrossRef]
- Singh, D.V.V.; Taneja, S.; Fatima, S. Comparative Evaluation of Treatment Outcome of Partial Pulpotomy Using Different Agents in Permanent Teeth—A Randomized Controlled Trial. Clin. Oral Investig. 2023, 27, 5171–5180. [Google Scholar] [CrossRef]
- Taha, N.A.; Al-Rawash, M.H.; Imran, Z.A. Outcome of Full Pulpotomy in Mature Permanent Molars Using 3 Calcium Silicate-based Materials: A Parallel, Double Blind, Randomized Controlled Trial. Int. Endod. J. 2022, 55, 416–429. [Google Scholar] [CrossRef]
- Wolters, W.J.; Duncan, H.F.; Tomson, P.L.; Karim, I.E.; McKenna, G.; Dorri, M.; Stangvaltaite, L.; van der Sluis, L.W.M. Minimally Invasive Endodontics: A New Diagnostic System for Assessing Pulpitis and Subsequent Treatment Needs. Int. Endod. J. 2017, 50, 825–829. [Google Scholar] [CrossRef]
- Careddu, R.; Duncan, H.F. A Prospective Clinical Study Investigating the Effectiveness of Partial Pulpotomy after Relating Preoperative Symptoms to a New and Established Classification of Pulpitis. Int. Endod. J. 2021, 54, 2156–2172. [Google Scholar] [CrossRef]
- Cushley, S.; Duncan, H.F.; Lappin, M.J.; Chua, P.; Elamin, A.D.; Clarke, M.; El-Karim, I.A. Efficacy of Direct Pulp Capping for Management of Cariously Exposed Pulps in Permanent Teeth: A Systematic Review and Meta-analysis. Int. Endod. J. 2021, 54, 556–571. [Google Scholar] [CrossRef]
- AAE. AAE Position Statement on Vital Pulp Therapy. J. Endod. 2021, 47, 1340–1344. [Google Scholar] [CrossRef] [PubMed]
- Parirokh, M.; Torabinejad, M.; Dummer, P.M.H. Mineral Trioxide Aggregate and Other Bioactive Endodontic Cements: An Updated Overview—Part I: Vital Pulp Therapy. Int. Endod. J. 2018, 51, 177–205. [Google Scholar] [CrossRef] [PubMed]
- Vallittu, P.K.; Boccaccini, A.R.; Hupa, L.; Watts, D.C. Bioactive Dental Materials—Do They Exist and What Does Bioactivity Mean? Dent. Mater. 2018, 34, 693–694. [Google Scholar] [CrossRef]
- Pedano, M.S.; Li, X.; Yoshihara, K.; Van Landuyt, K.; Van Meerbeek, B. Cytotoxicity and Bioactivity of Dental Pulp-Capping Agents towards Human Tooth-Pulp Cells: A Systematic Review of In-Vitro Studies and Meta-Analysis of Randomized and Controlled Clinical Trials. Materials 2020, 13, 2670. [Google Scholar] [CrossRef]
- Sanz, J.L.; Guerrero-Gironés, J.; Pecci-Lloret, M.P.; Pecci-Lloret, M.R.; Melo, M. Biological Interactions between Calcium Silicate-based Endodontic Biomaterials and Periodontal Ligament Stem Cells: A Systematic Review of in Vitro Studies. Int. Endod. J. 2021, 54, 2025–2043. [Google Scholar] [CrossRef] [PubMed]
- Torabinejad, M.; Parirokh, M.; Dummer, P.M.H. Mineral Trioxide Aggregate and Other Bioactive Endodontic Cements: An Updated Overview—Part II: Other Clinical Applications and Complications. Int. Endod. J. 2018, 51, 284–317. [Google Scholar] [CrossRef]
- Matoug-Elwerfelli, M.; ElSheshtawy, A.S.; Duggal, M.; Tong, H.J.; Nazzal, H. Vital Pulp Treatment for Traumatized Permanent Teeth: A Systematic Review. Int. Endod. J. 2022, 55, 613–629. [Google Scholar] [CrossRef] [PubMed]
- Santos, J.M.; Pereira, J.F.; Marques, A.; Sequeira, D.B.; Friedman, S. Vital Pulp Therapy in Permanent Mature Posterior Teeth with Symptomatic Irreversible Pulpitis: A Systematic Review of Treatment Outcomes. Medicina 2021, 57, 573. [Google Scholar] [CrossRef]
- Qu, T.; Lai, Y.; Luo, Y.; Pan, W.; Liu, C.; Cao, Y.; Hua, C. Prognosis of Second Molars with External Root Resorption Caused by Adjacent Embedded Third Molars. J. Endod. 2022, 48, 1113–1120. [Google Scholar] [CrossRef]
- Prasanna Kumar, D.; Sharma, M.; Vijaya Lakshmi, G.; Subedar, R.S.; Nithin, V.M.; Patil, V. Pathologies Associated with Second Mandibular Molar Due to Various Types of Impacted Third Molar: A Comparative Clinical Study. J. Maxillofac. Oral Surg. 2022, 21, 1126–1139. [Google Scholar] [CrossRef]
- Holcomb, J.B.; Dodds, R.N.; England, M.C. Endodontic Treatment Modalities for External Root Resorption Associated with Impacted Mandibular Third Molars. J. Endod. 1983, 9, 335–337. [Google Scholar] [CrossRef]
- Ahangari, Z.; Nasser, M.; Mahdian, M.; Fedorowicz, Z.; Marchesan, M.A. Interventions for the Management of External Root Resorption. Cochrane Database Syst. Rev. 2015, 11, CD008003. [Google Scholar] [CrossRef]
- Nagendrababu, V.; Chong, B.S.; McCabe, P.; Shah, P.K.; Priya, E.; Jayaraman, J.; Pulikkotil, S.J.; Setzer, F.C.; Sunde, P.T.; Dummer, P.M.H. PRICE 2020 Guidelines for Reporting Case Reports in Endodontics: A Consensus-based Development. Int. Endod. J. 2020, 53, 619–626. [Google Scholar] [CrossRef]
- Baensch, F.; Meißner, W.; Will, L.; Kunkel, M. Prevalence and Predictive Parameters of External Root Resorption Caused by Retained Wisdom Teeth. Clin. Oral Investig. 2024, 28, 583. [Google Scholar] [CrossRef]
- Dao, V.; Mallya, S.M.; Markovic, D.; Tetradis, S.; Chugal, N. Prevalence and Characteristics of Root Resorption Identified in Cone-Beam Computed Tomography Scans. J. Endod. 2023, 49, 144–154. [Google Scholar] [CrossRef] [PubMed]
- Ericson, S.; Kurol, P.J. Resorption of Incisors after Ectopic Eruption of Maxillary Canines: A CT Study. Angle Orthod. 2000, 70, 415–423. [Google Scholar] [CrossRef] [PubMed]
- Duncan, H.F.; Galler, K.M.; Tomson, P.L.; Simon, S.; El-Karim, I.; Kundzina, R.; Krastl, G.; Dammaschke, T.; Fransson, H.; Markvart, M.; et al. European Society of Endodontology Position Statement: Management of Deep Caries and the Exposed Pulp. Int. Endod. J. 2019, 52, 923–934. [Google Scholar] [CrossRef]
- AlRahabi, M.K. Evaluation of Complications of Root Canal Treatment Performed by Undergraduate Dental Students. Libyan J. Med. 2017, 12, 1345582. [Google Scholar] [CrossRef]
- Segura-Egea, J.J.; Cabanillas-Balsera, D.; Martín-González, J.; Cintra, L.T.A. Impact of Systemic Health on Treatment Outcomes in Endodontics. Int. Endod. J. 2023, 56, 219–235. [Google Scholar] [CrossRef]
- Moretto, C.; Kopper, P.M.P.; Münchow, E.A.; Scarparo, R.K. Association between Patient Age and Vital Pulp Therapy Outcomes: A Systematic Review and Meta-analysis of Prognostic Studies. Int. Endod. J. 2025, 58, 809–832. [Google Scholar] [CrossRef]
- Jepsen, K.; Dommisch, E.; Jepsen, S.; Dommisch, H. Vital Root Resection in Severely Furcation-involved Maxillary Molars: Outcomes after up to 7 Years. J. Clin. Periodontol. 2020, 47, 970–979. [Google Scholar] [CrossRef] [PubMed]
- Song, D.; Luo, Y.; Liu, X.; Hu, P.; Huang, D. Combined Micro-Apical Surgery and Vital Pulp Therapy in Mandibular Second Molars with External Root Resorption Caused by Impacted Teeth. Hua Xi Kou Qiang Yi Xue Za Zhi 2023, 41, 225–231. [Google Scholar] [CrossRef]
- Zhou, W.; Zheng, Q.; Tan, X.; Song, D.; Zhang, L.; Huang, D. Comparison of Mineral Trioxide Aggregate and IRoot BP Plus Root Repair Material as Root-End Filling Materials in Endodontic Microsurgery: A Prospective Randomized Controlled Study. J. Endod. 2017, 43, 1–6. [Google Scholar] [CrossRef] [PubMed]
- Xu, W.; Song, D.; Tan, X.; Zhang, L.; Huang, D. Vital Pulp Preservation Treatment in Mandibular Right First Molar with Vertical Root Fractures: A Case Report. Hua Xi Kou Qiang Yi Xue Za Zhi 2019, 37, 563–567. [Google Scholar] [CrossRef]
- Hermann, L.; Wenzel, A.; Schropp, L.; Matzen, L.H. Impact of CBCT on Treatment Decision Related to Surgical Removal of Impacted Maxillary Third Molars: Does CBCT Change the Surgical Approach? Dentomaxillofac. Radiol. 2019, 48, 20190209. [Google Scholar] [CrossRef] [PubMed]

| Visit | Diagnosis/Treatment | Observations |
|---|---|---|
| Initial visit | Anamnesis, clinical and radiographic examination (CBCT) | Mesio-inclined impacted upper third molars with resorption of the distal root of the adjacent second molars. |
| Extraction of the right third molar and rVPT of distal root of the upper right second molar | No significant complications. | |
| Second visit (1 month) | Extraction of the left third molar and rVPT of distal root of the upper left second molar | No significant complications. |
| 1-, 3-, 6- and 12-month follow-up | Heat and cold sensitivity tests | Pulp responding normally. Patient is asymptomatic. |
| 24-month follow-up | Heat and cold sensitivity tests; CBCT scan | Pulp responding normally. Patient is asymptomatic. Periadicular endogenous bone apposition observed in the CBCT. |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ambu, E.; Sanz, J.L.; Ghiretti, R.; Bellucci, F.; Gaeta, C.; Grandini, S.; Ghilotti, J.; Forner, L. Retrograde Vital Pulp Treatment in External Root Resorption Due to Third Molar Impaction: A Proof-of-Concept and Case Report. J. Clin. Med. 2025, 14, 5828. https://doi.org/10.3390/jcm14165828
Ambu E, Sanz JL, Ghiretti R, Bellucci F, Gaeta C, Grandini S, Ghilotti J, Forner L. Retrograde Vital Pulp Treatment in External Root Resorption Due to Third Molar Impaction: A Proof-of-Concept and Case Report. Journal of Clinical Medicine. 2025; 14(16):5828. https://doi.org/10.3390/jcm14165828
Chicago/Turabian StyleAmbu, Emanuele, José Luis Sanz, Roberto Ghiretti, Francesco Bellucci, Carlo Gaeta, Simone Grandini, James Ghilotti, and Leopoldo Forner. 2025. "Retrograde Vital Pulp Treatment in External Root Resorption Due to Third Molar Impaction: A Proof-of-Concept and Case Report" Journal of Clinical Medicine 14, no. 16: 5828. https://doi.org/10.3390/jcm14165828
APA StyleAmbu, E., Sanz, J. L., Ghiretti, R., Bellucci, F., Gaeta, C., Grandini, S., Ghilotti, J., & Forner, L. (2025). Retrograde Vital Pulp Treatment in External Root Resorption Due to Third Molar Impaction: A Proof-of-Concept and Case Report. Journal of Clinical Medicine, 14(16), 5828. https://doi.org/10.3390/jcm14165828






