Time Is Bone: Missed Opportunities for Secondary Prevention After a Hip Fracture
Abstract
1. Introduction
2. Material and Methods
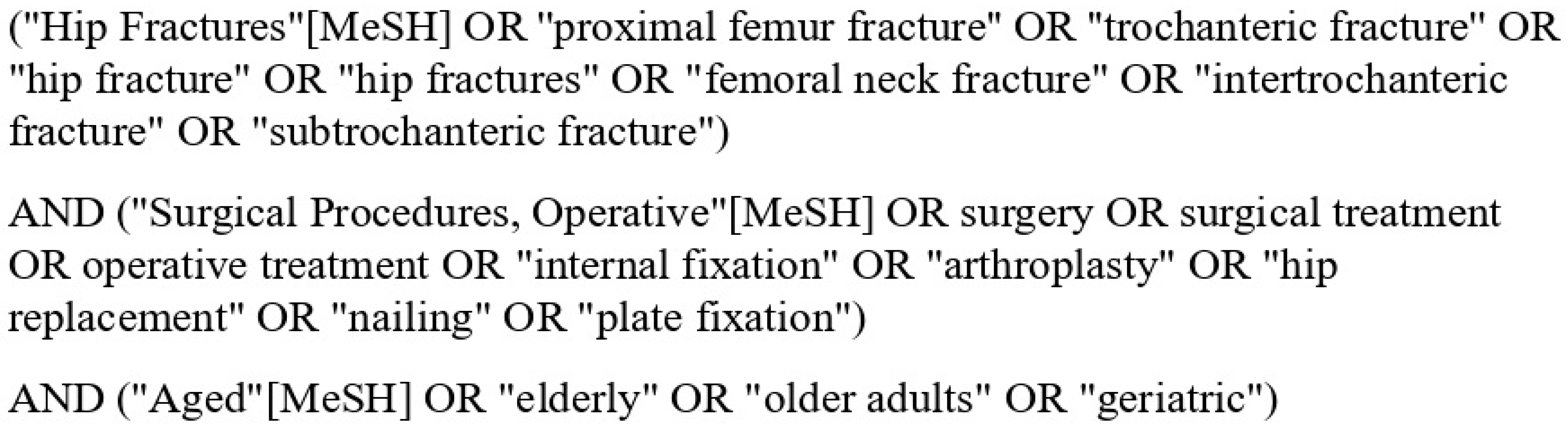
2.1. Search Strategy
2.2. Inclusion and Exclusion Criteria
2.3. Study Selection
2.4. Data Extraction
2.5. Data Synthesis and Analysis
3. Results
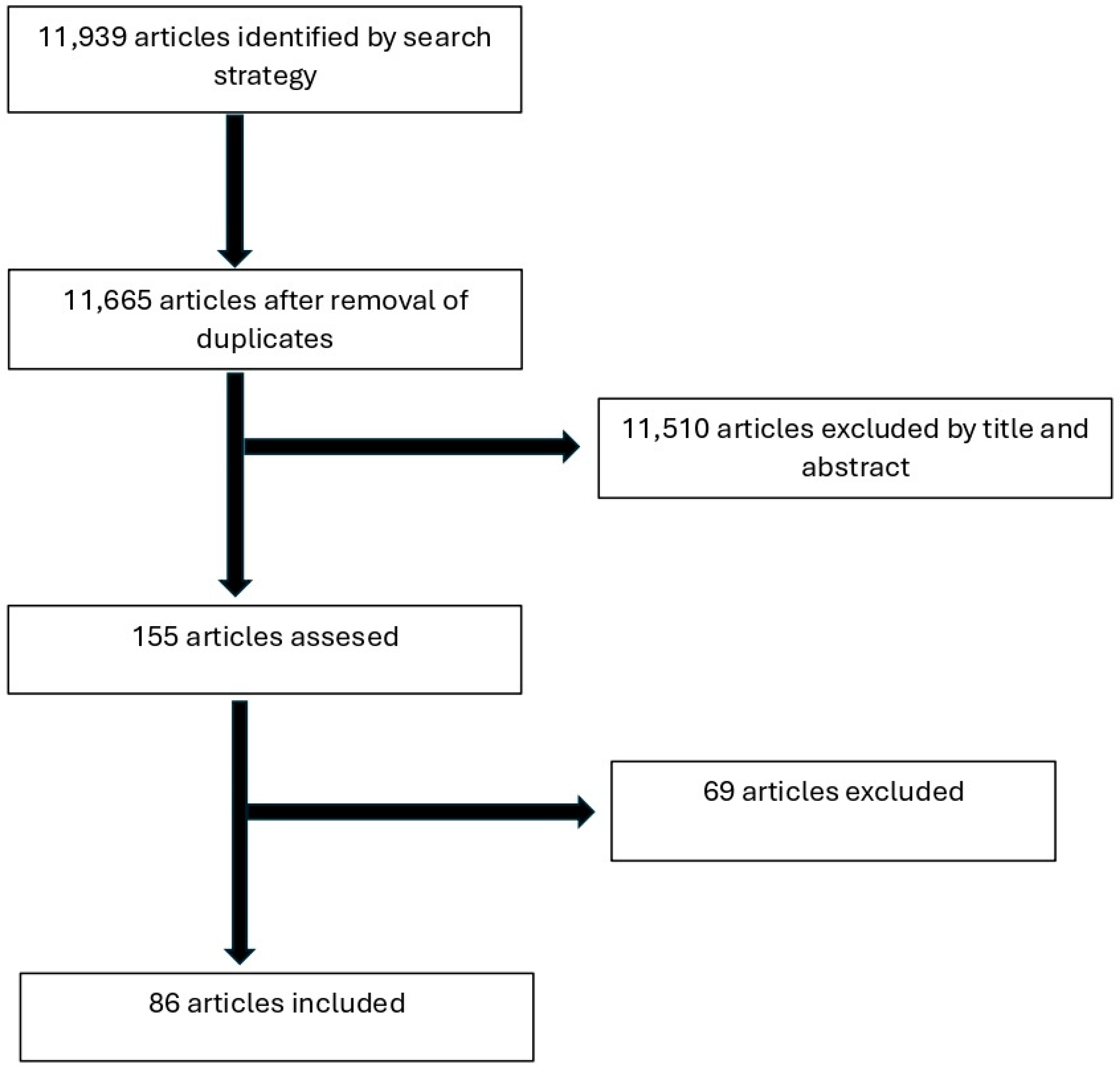
3.1. Flow and Characteristics of Included Studies
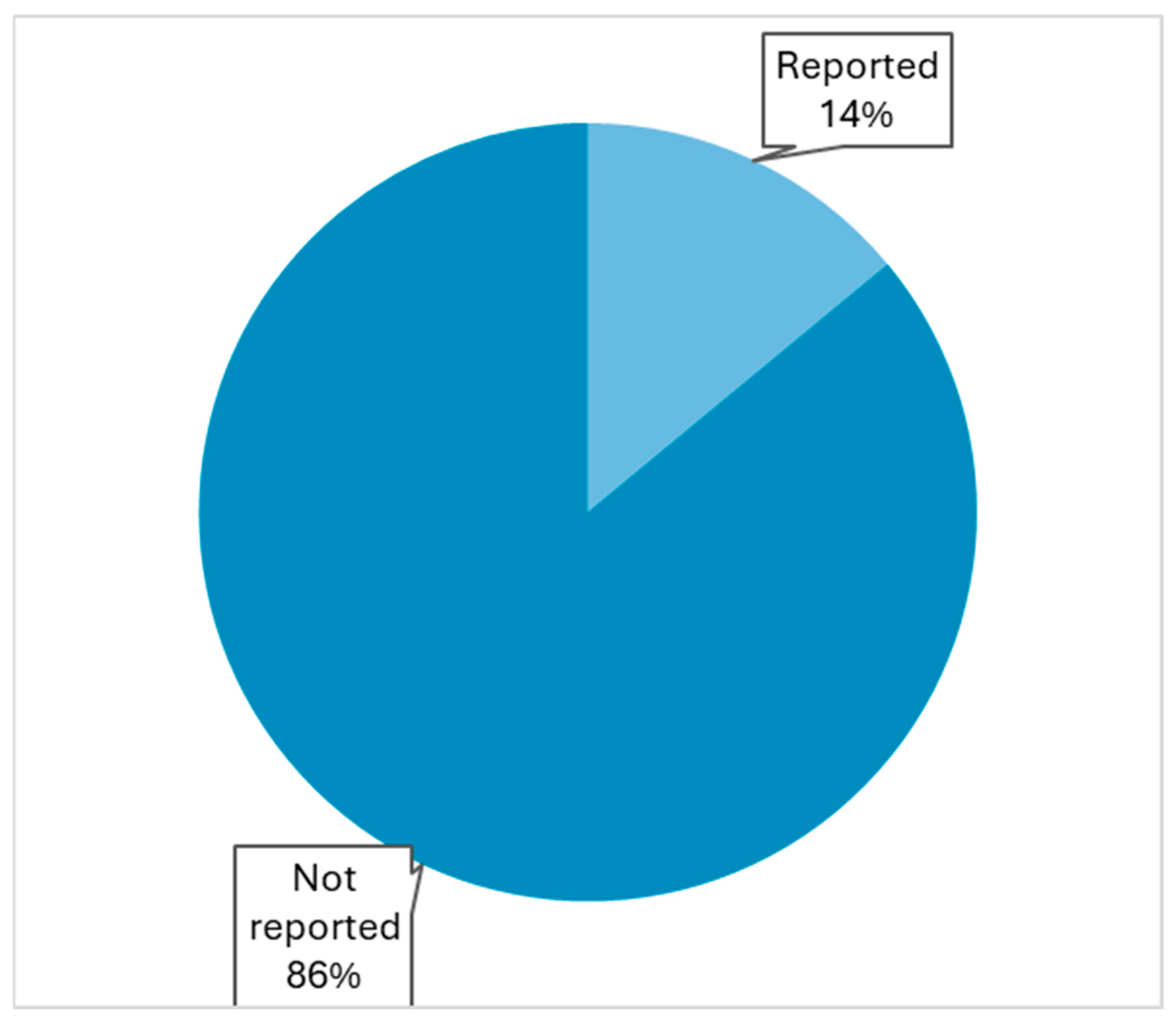
3.2. Reporting of Osteoporosis Management
3.3. Trends in Reporting
3.4. Non-Reporting Studies
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Data Availability Statement
Conflicts of Interest
References
- Adeyemi, A.; Delhougne, G. Incidence and Economic Burden of Intertrochanteric Fracture. JBJS Open Access 2019, 4, e0045. [Google Scholar] [CrossRef]
- Schermann, H.; Ashkenazi, I.; Graif, N.; Ogawa, T.; Morgan, S.; Ben Tov, T.; Khoury, A.; Warschawski, Y. Would giving priority in surgery timing to the oldest patients result in lower mortality? Int. Orthop. 2022, 46, 1701–1706. [Google Scholar] [CrossRef]
- Kim, S.C.; Kim, M.S.; Sanfélix-Gimeno, G.; Song, H.J.; Liu, J.; Hurtado, I.; Peiró, S.; Lee, J.; Choi, N.K.; Park, B.J.; et al. Use of osteoporosis medications after hospitalization for hip fracture: Across-national study. Am. J. Med. 2015, 128, 519–526.e1. [Google Scholar] [CrossRef]
- Matzkin, E.G.; DeMaio, M.; Charles, J.F.; Franklin, C.C. Diagnosis and Treatment of Osteoporosis: What Orthopaedic Surgeons Need to Know. J. Am. Acad. Orthop. Surg. 2019, 27, e902–e912. [Google Scholar] [CrossRef]
- McLellan, A.R.; Gallacher, S.J.; Fraser, M.; McQuillian, C. The fracture liaison service: Success of a program for the evaluation and management of patients with osteoporotic fracture. Osteoporos. Int. 2003, 14, 1028–1034. [Google Scholar] [CrossRef]
- Kanis, J.A.; Cooper, C.; Rizzoli, R.; Reginster, J.Y. Scientific Advisory Board of the European Society for Clinical and Economic Aspects of Osteoporosis (ESCEO) and the Committees of Scientific Advisors and National Societies of the International Osteoporosis Foundation (IOF) European guidance for the diagnosis and management of osteoporosis in postmenopausal women. Osteoporos. Int. 2019, 30, 3–44. [Google Scholar] [CrossRef]
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. BMJ 2021, 372, n71. [Google Scholar] [CrossRef] [PubMed]
- Abdallatif, A.G.; Sharma, A.; Mahmood, T.; Aslam, N. Complications and Outcomes of the Internal Fixation of Non-displaced Femoral Neck Fracture in Old Patients: A Two-Year Follow-Up. Cureus 2023, 15, e41391. [Google Scholar] [CrossRef] [PubMed]
- Adler, R.R.; Xiang, L.; Shah, S.K.; Clark, C.J.; Cooper, Z.; Mitchell, S.L.; Kim, D.H.; Hsu, J.; Sepucha, K.; Chunga, R.E.; et al. Hip Fracture Treatment and Outcomes Among Community-Dwelling People Living with Dementia. JAMA Netw. Open 2024, 7, e2413878. [Google Scholar] [CrossRef] [PubMed]
- Adulkasem, N.; Phinyo, P.; Khorana, J.; Pruksakorn, D.; Apivatthakakul, T. Prognostic Factors of 1-Year Postoperative Functional Outcomes of Older Patients with Intertrochanteric Fractures in Thailand: ARetrospective Cohort Study Int, J. Environ. Res. Public Health 2021, 18, 6896. [Google Scholar] [CrossRef] [PubMed]
- Andriollo, L.; Sangaletti, R.; Are, L.; Perticarini, L.; Benazzo, F.; Rossi, S.M.P. Uncemented hemiarthroplasty may have a role in the treatment of unstable intertrochanteric fractures in elderly patient. A survival complications and functional outcomes analysis. Int. J. Burns Trauma. 2023, 13, 126–135. [Google Scholar]
- Arraut, J.; Kurapatti, M.; Christensen, T.H.; Rozell, J.C.; Aggarwal, V.K.; Egol, K.A.; Schwarzkopf, R. Total hip arthroplasty for hip fractures in patients older than 80 years of age: A retrospective matched cohort study. Arch. Orthop. Trauma. Surg. 2023, 143, 1637–1642. [Google Scholar] [CrossRef]
- Barışhan, F.C.; Akesen, B.; Atıcı, T.; Durak, K.; Bilgen, M.S. Comparison of hemiarthroplasty and total hip arthroplasty in elderly patients with displaced femoral neck fractures. J. Int. Med. Res. 2018, 46, 2717–2730. [Google Scholar] [CrossRef]
- Bayon-Calatayud, M.; Benavente-Valdepeñas, A.M. Short-Term Outcomes of Interdisciplinary Hip Fracture Rehabilitation in Frail Elderly Inpatients. Rehabil. Res. Pract. 2018, 2018, 1708272. [Google Scholar] [CrossRef]
- Bi, C.; Zhao, Y.; Ma, Z.; Zhang, S. Comparison of Proximal Anti-Rotation Intramedullary Nail and Femoral Head Replacement for the Treatment of Femoral Intertrochanteric Fractures in Elderly Patients. Altern. Ther. Health Med. 2023, 29, 268–273. [Google Scholar]
- Bigoni, M.; Turati, M.; Leone, G.; Caminita, A.D.; D’Angelo, F.; Munegato, D.; Zatti, G. Internal fixation of intracapsular femoral neck fractures in elderly patients: Mortality and reoperation rate. Aging Clin. Exp. Res. 2020, 32, 1173–1178. [Google Scholar] [CrossRef] [PubMed]
- Blauth, M.; Joeris, A.; Rometsch, E.; Espinoza-Rebmann, K.; Wattanapanom, P.; Jarayabhand, R.; Poeze, M.; Wong, M.K.; Kwek, E.B.K.; Hegeman, J.H.; et al. Geriatric fracture centre vs. usual care after proximal femur fracture in older patients: What are the benefits? Results of a large international prospective multicentre study. BMJ Open 2021, 11, e039960. [Google Scholar] [CrossRef] [PubMed]
- Bűcs, G.; Dandé, Á.; Patczai, B.; Sebestyén, A.; Almási, R.; Nöt, L.G.; Wiegand, N. Bipolar hemiarthroplasty for the treatment of femoral neck fractures with minimally invasive anterior approach in elderly. Injury 2021, 52 (Suppl. 1), S37–S43. [Google Scholar] [CrossRef]
- Chatterji, G.; Shukla, S.; Singhania, S.; Singh, M.P.; Mohanty, S.S.; Jaiswal, A.; Mishra, D. A Prospective Study Comparing the Functional Outcome of Bipolar Hemiarthroplasty Versus Total Hip Replacement in Elderly Patients with Fracture of the Neck of Femur. Cureus 2022, 14, e29529. [Google Scholar] [CrossRef] [PubMed]
- Civinini, R.; Paoli, T.; Cianferotti, L.; Cartei, A.; Boccaccini, A.; Peris, A.; Brandi, M.L.; Rostagno, C.; Innocenti, M. Functional outcomes and mortality in geriatric and fragility hip fractures-results of an integrated, multidisciplinary model experienced by the “Florence hip fracture unit”. Int. Orthop. 2019, 43, 187–192. [Google Scholar] [CrossRef]
- Dayama, A.; Olorunfemi, O.; Greenbaum, S.; Stone, M.E., Jr.; McNelis, J. Impact of frailty on outcomes in geriatric femoral neck fracture management: An analysis of national surgical quality improvement program dataset. Int. J. Surg. 2016, 28, 185–190. [Google Scholar] [CrossRef] [PubMed]
- Ekinci, Y.; Gürbüz, K.; Batın, S.; Kahraman, M.; Doğar, F.; Kaya Erten, Z. A multicenter intertrochanteric fracture study in the elderly: Hemiarthroplasty versus proximal femoral nailing. Jt. Dis. Relat. Surg. 2020, 31, 209–217. [Google Scholar] [CrossRef]
- Fernandez, M.A.; Achten, J.; Parsons, N.; Griffin, X.L.; Png, M.E.; Gould, J.; McGibbon, A.; Costa, M.L. WHiTE5 Investigators Cemented or Uncemented Hemiarthroplasty for Intracapsular Hip Fracture. N. Engl. J. Med. 2022, 386, 521–530. [Google Scholar] [CrossRef]
- Guo, J.; Dong, W.; Jin, L.; Yin, Y.; Zhang, R.; Hou, Z.; Zhang, Y. Treatment of basicervical femoral neck fractures with proximal femoral nail antirotation. J. Int. Med. Res. 2019, 47, 4333–4343. [Google Scholar] [CrossRef] [PubMed]
- Huang, J.; Shi, Y.; Pan, W.; Wang, Z.; Dong, Y.; Bai, Y.; Wang, A.; Zhao, Y.; Zheng, J.; Lian, H. Bipolar Hemiarthroplasty should not be selected as the primary option for intertrochanteric fractures in elderly patients. Sci. Rep. 2020, 10, 4840. [Google Scholar] [CrossRef]
- Garcia-Barreiro, G.; Huespe, I.; Llano, L.; Dozo, M.; Benchimol, J.A.; Rebecchi, P.; Taype, D.; Barla, J.; Sancineto, C.; Carabelli, G. Patients with trochanteric hip fractures and pre-existing osteoarthritis can be treated with nailing osteosynthesis without significant decrease in functional status. Injury 2023, 54 (Suppl. 6). [Google Scholar] [CrossRef]
- Gölge, U.H.; Pazarci, O.; Kılınç, S.; Nusran, G.; Kaymaz, B.; Göksel, F.; Kömürcü, E.; Bulut, O. The treatment of intertrochanteric fractures comparison of PFN and hemiarthroplasty 3-year mortality study. Acta Orthop. Belg. 2016, 82, 508–515. [Google Scholar]
- Iorio, R.; Iannotti, F.; Mazza, D.; Speranza, A.; Massafra, C.; Guzzini, M.; D’Arrigo, C.; Ferretti, A. Is dual cup mobility better than hemiarthroplasty in patients with dementia and femoral neck fracture? A randomized controlled trial. SICOT-J 2019, 5, 38. [Google Scholar] [CrossRef]
- Jonas, S.C.; Shah, R.; Al-Hadithy, N.; Norton, M.R.; Sexton, S.A.; Middleton, R.G. Displaced intracapsular neck of femur fractures in the elderly: Bipolar hemiarthroplasty may be the treatment of choice; a case control study. Injury 2015, 46, 1988–1991. [Google Scholar] [CrossRef]
- Ju, F.X.; Hou, R.X.; Xiong, J.; Shi, H.F.; Chen, Y.X.; Wang, J.F. Outcomes of Femoral Neck Fractures Treated with Cannulated Internal Fixation in Elderly Patients: A Long-Term Follow-Up Study. Orthop. Surg. 2020, 12, 809–818. [Google Scholar] [CrossRef] [PubMed]
- Karaali, E.; Çiloğlu, O. Metaphyseal vs. diaphyseal fixed-stem hemiarthroplasty in treating unstable intertrochanteric fractures in elderly patients. Ulus. Travma Acil Cerrahi Derg. 2021, 27, 104–108. [Google Scholar] [CrossRef]
- Kawai, M.; Tanji, A.; Nishijima, T.; Tateyama, K.; Yoda, Y.; Iizuka, A.; Kamata, Y.; Urabe, T. Association between time to surgery and 90-day mortality after hip fracture: A retrospective cohort study of 1734 cases. J. Orthop. Sci. 2018, 23, 987–991. [Google Scholar] [CrossRef] [PubMed]
- Khan, A.Q.; Mohammad, J.; Qamar, R.; Siddiqui, Y.S.; Sabir, A.B.; Abbas, M. Cemented unipolar or modular bipolar hemiarthroplasty for femoral neck fractures in elderly patients—Which is better? Int. J. Burn. Trauma 2021, 11, 447–455. [Google Scholar]
- Knauf, T.; Bücking, B.; Bargello, M.; Ploch, S.; Bliemel, C.; Knobe, M.; Ruchholtz, S.; Eschbach, D. Predictors of long-term survival after hip fractures?-5-year results of a prospective study in Germany. Arch. Osteoporos. 2019, 14, 40. [Google Scholar] [CrossRef] [PubMed]
- Koyuncu, Ş.; Altay, T.; Kayalı, C.; Ozan, F.; Yamak, K. Mechanical failures after fixation with proximal femoral nail and risk factors. Clin. Interv. Aging 2015, 10, 1959–1965. [Google Scholar] [CrossRef] [PubMed]
- Kusen, J.Q.; Schafroth, B.; Poblete, B.; van der Vet, P.C.R.; Link, B.C.; Wijdicks, F.J.G.; Babst, R.H.; Beeres, F.J.P. The implementation of a Geriatric Fracture Centre for hip fractures to reduce mortality and morbidity: An observational study. Arch. Orthop. Trauma. Surg. 2019, 139, 1705–1712. [Google Scholar] [CrossRef]
- Kusen, J.; van der Vet, P.; Wijdicks, F.J.; Houwert, M.; Dijkgraaf, M.; Hamaker, M.; Geraghty, O.; Verleisdonk, E.J.; van der Velde, D. Different approaches towards geriatric trauma care for hip fracture patients: An inter-hospital comparison. Eur. J. Trauma. Emerg. Surg. 2021, 47, 557–564. [Google Scholar] [CrossRef]
- Laubach, M.; Bläsius, F.M.; Volland, R.; Knobe, M.; Weber, C.D.; Hildebrand, F.; Pishnamaz, M. Internal fixation versus hip arthroplasty in patients with nondisplaced femoral neck fractures: Short-term results from a geriatric trauma registry. Eur. J. Trauma. Emerg. Surg. 2022, 48, 1851–1859. [Google Scholar] [CrossRef]
- Leonardsson, O.; Rolfson, O.; Rogmark, C. The surgical approach for hemiarthroplasty does not influence patient-reported outcome: A national survey of 2118 patients with one-year follow-up. Bone Joint J. 2016, 98-B, 542–547. [Google Scholar] [CrossRef]
- Li, H.; Wang, Q.; Dai, G.-G.; Peng, H. PFNA vs. DHS helical blade for elderly patients with osteoporotic femoral intertrochanteric fractures. Eur. Rev. Med. Pharmacol. Sci. 2018, 22, 1–7. [Google Scholar] [CrossRef]
- Liang, Y.; Liu, S.; Li, L.; Zhong, F. Proximal femoral nail antirotation versus external fixation for unstable intertrochanteric fractures in elderly patients: A randomized controlled trial. Medicine 2022, 101, e29384. [Google Scholar] [CrossRef]
- Liu, H.; Li, N.; Zhang, X.; He, L.; Li, D.; Li, Y.; Zhao, G.; Wu, X. Internal fixation versus hemiarthroplasty for displaced femoral neck fractures in the elderly: A cost-effectiveness analysis. Injury 2020, 51, 1346–1351. [Google Scholar] [CrossRef]
- Lu, Q.; Tang, G.; Zhao, X.; Guo, S.; Cai, B.; Li, Q. Hemiarthroplasty versus internal fixation in super-aged patients with undisplaced femoral neck fractures: A 5-year follow-up of randomized controlled trial. Arch. Orthop. Trauma. Surg. 2017, 137, 27–35. [Google Scholar] [CrossRef]
- MacLellan, C.; Faig, K.; Cooper, L.; Benjamin, S.; Shanks, J.; Flewelling, A.J.; Dutton, D.J.; McGibbon, C.; Bohnsack, A.; Wagg, J.; et al. Health Outcomes of Older Adults after a Hospitalization for a Hip Fracture. Can. Geriatr. J. 2024, 27, 290–298. [Google Scholar] [CrossRef]
- Mallick, A.; Jehan, S.; Omonbude, D. Outcome of surgery in neck of femur fracture patients with poor pre-fracture mobility. HIP Int. 2020, 30, 805–809. [Google Scholar] [CrossRef]
- Moaz, M.; Afgan, S.; Ahmad, I.; Ur Rehman, H.; Chishty, J.A.; Aslam, A.; Ibrahim, M. Cemented Modular Bipolar Hemiarthroplasty for Displaced Femoral Neck Fractures in the Elderly. Cureus 2024, 16, e74604. [Google Scholar] [CrossRef] [PubMed]
- Moore, J.; Berney, M.; Walsh, M.; Hurson, C.; Rowan, F.; Cleary, M.; Brent, L. Intracapsular hip fractures: A comparative study of cemented and uncemented hemiarthroplasties in the Irish hip fracture database. Surgeon 2024, 22, 276–280. [Google Scholar] [CrossRef]
- Morris, H.; Cameron, C.; Vanderboor, C.; Nguyen, A.; Londahl, M.; Harng Chong, Y.; Navarre, P. Hip fractures in the older adult: Orthopaedic and geriatric shared care model in Southland, New Zealand-a 5-year follow-up study. BMJ Open Qual. 2023, 12, e002242. [Google Scholar] [CrossRef] [PubMed]
- Mukka, S.; Sjöholm, P.; Aziz, A.; Eisler, T.; Kadum, B.; Krupic, F.; Morberg, P.; Sayed-Noor, A. A cohort study comparing internal fixation for undisplaced versus hip arthroplasty for displaced femoral neck fracture in the elderly: A pilot study for a clinical trial. Pilot Feasibility Stud. 2020, 6, 98. [Google Scholar] [CrossRef] [PubMed]
- Okano, I.; Sawada, T.; Kushima, N.; Tachibana, T.; Inagaki, K. Treatment with Helical Blade Cephalomedullary Nail for Two-Part Basicervical Proximal Femoral Fracture in Elderly Patients: A Retrospective Observational Study. Geriatr. Orthop. Surg. Rehabil. 2017, 8, 244–251. [Google Scholar] [CrossRef]
- Peddamadyam, S.; Arvind Kumar, B.; Arcot, R.V.K. Functional Outcomes of Primary Hemiarthroplasty for Unstable Intertrochanteric Fractures in the Elderly: A Prospective Observational Study. Cureus 2024, 16, e54892. [Google Scholar] [CrossRef]
- Prestmo, A.; Saltvedt, I.; Helbostad, J.L.; Taraldsen, K.; Thingstad, P.; Lydersen, S.; Sletvold, O. Who benefits from orthogeriatric treatment? Results from the Trondheim hip-fracture trial. BMC Geriatr. 2016, 16, 49. [Google Scholar] [CrossRef]
- Prieto-Alhambra, D.; Reyes, C.; Sainz, M.S.; González-Macías, J.; Delgado, L.G.; Bouzón, C.A.; Gañan, S.M.; Miedes, D.M.; Vaquero-Cervino, E.; Bardaji, M.F.B. In-hospital care, complications, and 4-month mortality following a hip or proximal femur fracture: The Spanish registry of osteoporotic femur fractures prospective cohort study. Arch. Osteoporos. 2018, 13, 96. [Google Scholar] [CrossRef] [PubMed]
- Ratanpal, A.; Kamath, K.R.; Salian, P.R.V.; Baliga, S.S.; Annappa, R.; Banerjee, S. Mortality and functional outcomes in elderly adults treated surgically by hemiarthroplasty for femoral neck fractures. SAGE Open Med. 2025, 13, 20503121241307264. [Google Scholar] [CrossRef] [PubMed]
- Regis, D.; Segalla, S.; Sandri, A.; Magnan, B. Cemented and uncemented stems for displaced femoral neck fracture in the elderly. Retrospective study with a minimum 1-year follow-up. Acta Biomed. 2023, 94, e2023146. [Google Scholar] [CrossRef]
- Sadeghi, C.; Prentice, H.A.; Okike, K.M.; Paxton, E.W. Treatment of Intertrochanteric Femur Fractures with Long versus Short Cephalomedullary Nails. Perm. J. 2020, 24, 19.229. [Google Scholar] [CrossRef]
- Salvesen, E.S.; Taraldsen, K.; Lønne, G.; Lydersen, S.; Lamb, S.E.; Opdal, K.; Saltvedt, I.; Johnsen, L.G. Characteristics and outcomes for hip fracture patients in an integrated orthogeriatric care model: A descriptive study of four discharge pathways with one-year follow-up. BMC Musculoskelet. Disord. 2025, 26, 184. [Google Scholar] [CrossRef]
- Sanderson-Jerome, C.; Hariharan, S. Outcome and Cost Evaluation of Hip Fractures in Elderly Patients at a Tertiary Care Hospital in the Caribbean. Cureus 2024, 16, e74586. [Google Scholar] [CrossRef]
- Schoeneberg, C.; Pass, B.; Volland, R.; Knobe, M.; Eschbach, D.; Ketter, V.; Lendemans, S.; Aigner, R. Four-month outcome after proximal femur fractures and influence of early geriatric rehabilitation: Data from the German Centres of Geriatric Trauma DGU. Arch. Osteoporos. 2021, 16, 68. [Google Scholar] [CrossRef]
- Schuijt, H.J.; Kusen, J.; van Hernen, J.J.; van der Vet, P.; Geraghty, O.; Smeeing, D.P.J.; van der Velde, D. Orthogeriatric Trauma Unit Improves Patient Outcomes in Geriatric Hip Fracture Patients. Geriatr. Orthop. Surg. Rehabil. 2020, 11, 2151459320949476. [Google Scholar] [CrossRef]
- Sun, M.; Zhang, X.; Wang, J.; Hong, Y.; Zhang, Y.; Wang, J.; Xu, D.; Yu, X.; Zhang, Y.; Zhu, H.; et al. Current status of postoperative care for elderly osteoporotic fracture patients in Jiangsu Province China: Amulticenter cross-sectional study. Int. J. Orthop. Trauma. Nurs. 2024, 55, 101136. [Google Scholar] [CrossRef] [PubMed]
- Sun, L.; Wang, C.; Zhang, M.; Li, X.; Zhao, B. The Surgical Timing and Prognoses of Elderly Patients with Hip Fractures: A Retrospective Analysis. Clin. Interv. Aging 2023, 18, 891–899. [Google Scholar] [CrossRef]
- Sun, M.; Liang, H.R.; Zhang, H.; Bai, T.; Xu, R.D.; Duan, S.Y.; Cai, Z.C. Surgical options for Evans-Jensen type IV intertrochanteric femur fractures in the elderly over 65: A comparison between total hip arthroplasty and proximal femoral nail antirotation. Front. Surg. 2024, 11, 1510094. [Google Scholar] [CrossRef] [PubMed]
- Solberg, L.B.; Vesterhus, E.B.; Hestnes, I.; Ahmed, M.V.; Ommundsen, N.; Westberg, M.; Frihagen, F. Comparing two different orthogeriatric models of care for hip fracture patients: An observational prospective cross-sectional study. BMJ Open Qual. 2023, 12, e002302. [Google Scholar] [CrossRef]
- Sniderman, J.; Vivekanantha, P.; Shah, A.; Safir, O.; Wolfstadt, J.; Kuzyk, P. Hemiarthroplasty for Unstable Intertrochanteric Hip Fractures: AMatched Cohort Study. J. Arthroplast. 2023, 38, 1522–1527. [Google Scholar] [CrossRef]
- Song, J.; Zhang, G.; Liang, J.; Bai, C.; Dang, X.; Wang, K.; He, C.; Liu, R. Effects of delayed hip replacement on postoperative hip function and quality of life in elderly patients with femoral neck fracture. BMC Musculoskelet. Disord. 2020, 21, 487. [Google Scholar] [CrossRef] [PubMed]
- Sundkvist, J.; Hulenvik, P.; Schmidt, V.; Jolbäck, P.; Sundfeldt, M.; Fischer, P.; Rogmark, C.; Juto, H.; Wolf, O.; Mukka, S. Basicervical femoral neck fractures: An observational study derived from the Swedish Fracture Register. Acta Orthop. 2024, 95, 250–255. [Google Scholar] [CrossRef]
- Tan, S.T.; Tan, W.P.; Jaipaul, J.; Chan, S.P.; Sathappan, S.S. Clinical outcomes and hospital length of stay in 2756 elderly patients with hip fractures: A comparison of surgical and non-surgical management. Singap. Med. J. 2017, 58, 253–257. [Google Scholar] [CrossRef]
- Chen, M.; Li, Y.; Yang, Y.; Zhuang, W. Analysis of the risk factors for contralateral refracture after hip fracture surgery in elderly individuals: A retrospective study. J. Orthop. Surg. Res. 2024, 19, 681. [Google Scholar] [CrossRef]
- Chen, C.H.; Huang, P.J.; Huang, H.T.; Lin, S.Y.; Wang, H.Y.; Fang, T.J.; Lin, Y.C.; Ho, C.J.; Lee, T.C.; Lu, Y.M.; et al. Impact of orthogeriatric care, comorbidity, and complication on 1-year mortality in surgical hip fracture patients: An observational study. Medicine 2019, 98, e17912. [Google Scholar] [CrossRef]
- Cho, H.M.; Lee, K. Clinical and Functional Outcomes of Treatment for Type A1 Intertrochanteric Femoral Fracture in Elderly Patients: Comparison of Dynamic Hip Screw and Proximal Femoral Nail Antirotation. Hip Pelvis 2016, 28, 232–242. [Google Scholar] [CrossRef]
- Lee, J.C.; Koo, K.; Wong, E.K.C.; Naqvi, R.; Wong, C.L. Impact of an orthogeriatric collaborative care model for older adults with hip fracture in a community hospital setting. Can. J. Surg. 2021, 64, E211–E217. [Google Scholar] [CrossRef]
- Chen, J.Y.; She, G.R.; Luo, S.M.; Wu, W.R.; Zhuang, T.F.; Huan, S.W.; Liu, N.; Zha, Z.G. Hemiarthroplasty compared with internal fixation for treatment of nondisplaced femoral neck fractures in elderly patients: A retrospective study. Injury 2020, 51, 1021–1024. [Google Scholar] [CrossRef]
- Takahashi, A.; Naruse, H.; Kitade, I.; Shimada, S.; Tsubokawa, M.; Kokubo, Y.; Matsumine, A. Functional outcomes after the treatment of hip fracture. PLoS ONE 2020, 15, e0236652. [Google Scholar] [CrossRef] [PubMed]
- Tian, R.H.; Zhang, Q.M.; Chu, F.L.; Li, X.Y.; Jiang, Z.; Han, L.; Sun, P.; Wang, H.B.; Chi, Y.L.; Wu, B. Comparison of two methods of locating proximal femoral nail anti-rotation in the treatment of femoral intertrochanteric fractures. J. Orthop. Surg. Res. 2020, 15, 108. [Google Scholar] [CrossRef] [PubMed]
- Tilaveridis, P.; Iliopoulos, E.; Georgoulas, P.; Drosos, G.; Ververidis, A.; Tilkeridis, K. Treating peri-trochanteric hip fractures with intramedullary nail, when a second anti-rotational screw is necessary? BMC Musculoskelet. Disord. 2023, 24, 787. [Google Scholar] [CrossRef] [PubMed]
- Tol, M.C.; van den Bekerom, M.P.; Sierevelt, I.N.; Hilverdink, E.F.; Raaymakers, E.L.; Goslings, J.C. Hemiarthroplasty or total hip arthroplasty for the treatment of a displaced intracapsular fracture in active elderly patients: 12-year follow-up of randomised trial. Bone Joint J. 2017, 99-B, 250–254. [Google Scholar] [CrossRef]
- Uzel, K.; Birinci, M.; Hakyemez, Ö.S.; Bostanci, B.; Bingöl, İ.; Öktem, U.; Ata, N.; Ülgü, M.M.; Birinci, Ş.; Karatosun, V. Comparison of Hemiarthroplasty, total hip arthroplasty, and internal fixation for hip fractures in patients over eighty years of age: Factors affecting mortality: A nationwide cohort study of fifty three thousand, four hundred and ninety five patients from Türkiye. Int. Orthop. 2025, 49, 729–736. [Google Scholar] [CrossRef]
- Vasu, B.K.; Ramamurthi, K.P.; Rajan, S.; George, M. Geriatric Patients with Hip Fracture: Frailty and Other Risk Factors Affecting the Outcome. Anesth. Essays Res. 2018, 12, 546–551. [Google Scholar] [CrossRef]
- Yu, W.; Zhang, X.; Zhu, X.; Hu, J.; Liu, Y. A retrospective analysis of the InterTan nail and proximal femoral nail anti-rotation-Asia in the treatment of unstable intertrochanteric femur fractures in the elderly. J. Orthop. Surg. Res. 2016, 11, 10. [Google Scholar] [CrossRef]
- Wang, J.; Luo, H.; Wang, Q.; Zhu, X. Analysis of the Surgical Outcomes in Elderly Patients with Hip Fractures Combined with Hemiplegia. Clin. Interv. Aging 2022, 17, 1093–1098. [Google Scholar] [CrossRef]
- Viganò, M.; Pennestrì, F.; Listorti, E.; Banfi, G. Proximal hip fractures in 71,920 elderly patients: Incidence, epidemiology, mortality and costs from a retrospective observational study. BMC Public Health 2023, 23, 1963. [Google Scholar] [CrossRef]
- Wang, H.; Pan, L.; Li, B.; Ning, T.; Liang, G.; Cao, Y. Obese elderly patients with hip fractures may have better survival outcomes after surgery. Arch. Orthop. Trauma. Surg. 2023, 143, 4793–4803. [Google Scholar] [CrossRef]
- Wignadasan, W.; Najefi, A.; Dewhurst, M.; Fazal, M.A. Cemented Versus Uncemented Hemiarthroplasty for Displaced Intracapsular Neck of Femur Fractures in the Elderly: Outcomes and Costings. Indian J. Orthop. 2024, 58, 716–721. [Google Scholar] [CrossRef]
- Xu, X.; Hu, X.; Fei, L.; Shen, S. Analysis of elderly patients with inter-trochanteric fracture and failure of postoperative internal fixation. Technol. Health Care 2025, 33, 1917–1925. [Google Scholar] [CrossRef]
- Yan, T.-X.; Dong, S.-J.; Ning, B.; Zhao, Y.-C. Bipolar hip arthroplasty using conjoined tendon preserving posterior lateral approach in treatment of displaced femoral neck fractures. World J. Clin. Cases 2024, 12, 1076–1083. [Google Scholar] [CrossRef] [PubMed]
- Yin, Z.; Hu, Q.; Zhang, B.; Yi, J.; Zhang, H.; Yin, J. Comparison of surgical efficacy between direct anterior approach and posterolateral approach in the treatment of sarcopenia with femoral neck fractures. BMC Geriatr. 2024, 24, 1021. [Google Scholar] [CrossRef]
- Lee, Y.K.; Won, H.; Roa, K.R.U.; Ha, Y.C.; Koo, K.H. Bipolar hemiarthroplasty using microarc oxidation-coated cementless stem in patients with unstable intertrochanteric fracture. J. Orthop. Surg. 2019, 27, 2309499019847815. [Google Scholar] [CrossRef] [PubMed]
- Gilmore, C.; Mayne, A.; Goodland, C.; Cassidy, R.; MacDonnell, L.; Mogey, P.; Murphy, L.; Diamond, O. Early surgery improves survival after femoral fractures in the elderly: A retrospective review of 502 fragility fractures. Injury 2024, 55, 111275. [Google Scholar] [CrossRef] [PubMed]
- Roll, C.; Tittel, S.; Schäfer, M.; Burkhardt, J.; Kinner, B. Continuous improvement process: Ortho-geriatric co-management of proximal femoral fractures. Arch. Orthop. Trauma. Surg. 2019, 139, 347–354. [Google Scholar] [CrossRef]
- Zhou, X.; Chen, M.; Yu, W.; Han, G.; Ye, J.; Zhuang, J. Uncemented versus cemented total hip arthroplasty for displaced femoral neck fractures in elderly patients with osteoporosis: A retrospective analysis. J. Int. Med. Res. 2020, 48, 300060520944663. [Google Scholar] [CrossRef]
- Zhou, S.; Liu, J.; Zhen, P.; Shen, W.; Chang, Y.; Zhang, H.; Zhu, Q.; Li, X. Proximal femoral nail anti-rotation versus cementless bipolar hemiarthroplasty for unstable femoral intertrochanteric fracture in the elderly: A retrospective study. BMC Musculoskelet. Disord. 2019, 20, 500. [Google Scholar] [CrossRef] [PubMed]
- Park, J.-H.; Chung, Y.-Y.; Baek, S.-N.; Park, T.-G. Hemiarthroplasty through Direct Anterior Approach for Unstable Femoral Intertrochanteric Fractures in the Elderly: Analysis of Early Cases. Hip Pelvis 2022, 34, 79–86. [Google Scholar] [CrossRef] [PubMed]
- Cosman, F.; de Beur, S.J.; LeBoff, M.S.; Lewiecki, E.M.; Tanner, B.; Randall, S.; Lindsay, R. Clinician’s Guide to Prevention and Treatment of Osteoporosis. Osteoporos. Int. 2014, 25, 2359–2381. [Google Scholar] [CrossRef]
- Åkesson, K.E.; McGuigan, F.E.A. Closing the Osteoporosis Care Gap. Curr. Osteoporos. Rep. 2021, 19, 58–65. [Google Scholar] [CrossRef] [PubMed]
- Zhang, X.; Wang, Z.; Zhang, D.; Ye, D.; Zhou, Y.; Qin, J.; Zhang, Y. The prevalence and treatment rate trends of osteoporosis in postmenopausal women. PLoS ONE 2023, 18, e0290289. [Google Scholar] [CrossRef]
- Ross, B.J.; Lee, O.C.; Harris, M.B.; Dowd, T.C.; Savoie, F.H., 3rd; Sherman, W.F. Rates of Osteoporosis Management and Secondary Preventative Treatment After Primary Fragility Fractures. JBJS Open Access 2021, 6, e20.00142. [Google Scholar] [CrossRef]
- Akesson, K.; Marsh, D.; Mitchell, P.J.; McLellan, A.R.; Stenmark, J.; Pierroz, D.D.; Kyer, C.; Cooper, C.; IOF Fracture Working Group. Capture the Fracture: A Best Practice Framework and global campaign to break the fragility fracture cycle. Osteoporos. Int. 2013, 24, 2135–2152. [Google Scholar] [CrossRef]
- Van Camp, L.; Dejaeger, M.; Tournoy, J.; Gielen, E.; Laurent, M.R. Association of orthogeriatric care models with evaluation and treatment of osteoporosis: A systematic review and meta-analysis. Osteoporos. Int. 2020, 31, 2083–2092. [Google Scholar] [CrossRef]
- Yan, C.; Chen, Y.; Cao, J.; Fang, K.; Shao, L.; Luo, Y.; Yang, L. The effectiveness of fracture liaison services in patients with hip fractures: A systematic review and meta-analysis of randomized controlled trials. Heliyon 2023, 9, e20838. [Google Scholar] [CrossRef]
| Author | Year | Country | Sample Size | Sex (Male:Female) | Mean Age | Type of Study | Outcomes of Interest | Level of Evidence | Osteoporosis Management |
|---|---|---|---|---|---|---|---|---|---|
| Abdalattif et al. [8] | 2023 | UK | 148 | 60:88 | 78.5 | Retrospective | Non-union and AVN incidence | III | NR |
| Adler et al. [9] | 2023 | USA | 33,142 | 9180:23,962 | 86.1 | Retrospective | Mortality, delirium, hospice services, SNF admission, nursing home admissions | III | NR |
| Adulkasem et al. [10] | 2021 | Thailand | 221 | 36:185 | 84 | Retrospective | Pre-injury New Mobility Score, score at the time of discharge, one year postoperative score | III | NR |
| Andriollo et al. [11] | 2023 | Italy | 86 | 20:86 | 87.4 | Retrospective | Charlson Comorbidity Index, Barthel index, Koval Grade, Mental Score, subsequent hospitalizations for surgical operations relating to the operated hip | III | NR |
| Arraut et al. [12] | 2022 | USA | 110 | 23:87 | Younger cohort: 67.69 Older cohort: 85.12 | Retrospective matched cohort | Discharge disposition, 90-days postoperative outcomes | III | NR |
| Barışhan et al. [13] | 2018 | Turkey | 38 | 13:25 | THA: 73.6 HA: 76.9 | Retrospective | Clinical outcomes and mortality | III | NR |
| Bayon-Calatayud et al. [14] | 2018 | Spain | 50 | 11:39 | 84.1 | Prospective cohort | Barthel score | II | NR |
| Bi et al. [15] | 2023 | China | 72 | 28:44 | 68.59 | Retrospective | Perioperative indicators, functional outcome (Harris hip score), complications one year postoperatively | III | NR |
| Bigoni et al. [16] | 2020 | Italy | 244 | 79:65 | 80 | Retrospective | Mortality rate, complications, reoperation rate | IV | NR |
| Blauth et al. [17] | 2021 | USA | 281 | 74:207 | Geriatric center: 81.9 Usual care: 83.9 | Prospective multicenter | Major adverse effects, mortality | II | NR |
| Bűcs et al. [18] | 2021 | Hungary | 94 | 35:59 | 79 | Prospective cohort | Perioperative indicators, mobilization, length of stay, functional outcome (Harris hip score) | II | NR |
| Chatterji et al. [19] | 2022 | India | 40 | 16:24 | THA: 70.28 HA: 68.5 | Prospective cohort | Functional outcome (Harris hip score) | II | NR |
| Chen et al. [73] | 2020 | China | 130 | 49:81 | HA: 78.3 IF: 75.1 | Retrospective cohort | Incidence of surgical complications and reoperation, mortality, hip joint function at the last follow-up, perioperative parameters | III | NR |
| Chen et al. [70] | 2019 | China | 313 | 92:221 | 77.6 | Retrospective cohort | 1-year mortality | III | NR |
| Chen et al [69] | 2024 | China | 458 | 121:276 | No fracture: 71 Contralateral hip fracture: 84 | Retrospective | Analysis of contralateral hip fracture risk factors | III | Administration of calcitriol and calcium |
| Cho et al. [71] | 2016 | China | 194 | 69:125 | DHS: 84.2 PFNA: 81 | Retrospective | Operative time, blood loss, walking ability, Barthel index, fracture union, proximal femur shortening, complications | III | BMD testing (DXA) |
| Civinini et al. [21] | 2019 | Italy | 677 | 210:467 | 84.5 | Prospective cohort | Mortality, return to daily activities, quality of life, adherence to re-fracture prevention programs | II | FLS, BMD testing and evaluation of fall and fracture within 3 months for 434 (66%) eligible patients, prescription of specific drugs and calcium ± vitamin D supplementation in 342 (78.8%) patients |
| Dayama et al. [21] | 2016 | USA | 3121 | 938:2183 | 77.34 | Retrospective registry study | 30-day morbidity and mortality | III | NR |
| Ekinci et al. [22] | 2020 | Turkey | 308 | 81:227 | BHA: 78.4 PFN: 77.7 | Prospective cohort | Singh Index, functional outcome (Harris hip score) | II | NR |
| Fernandez et al. [23] | 2023 | France | 181 | 40:41 | 82.5 | Retrospective cohort | Fixation failure rate at 3 and 6 months, quality of life, Parker mobility score, Harris hip score | III | NR |
| Guo et al. [24] | 2019 | China | 17 | 4:10 | 67.6 | Retrospective cohort | Fracture union, complications, functional outcome (Harris hip score) | III | NR |
| Huang et al. [25] | 2020 | China | 202 | 53:149 | 86 | Retrospective | Operative duration, blood loss, time of weight-bearing after operation, complications, functional outcome (Harris hip score) | III | NR |
| Garcia-Barreiro et al. [26] | 2023 | Argentina | 375 | 58:317 | 86.1 | Retrospective | Functional outcome (Parker mobility score) | III | NR |
| Gilmore et al. [89] | 2024 | UK | 502 | 137:335 | 80.1 | Retrospective | 30-day and 1-year mortality | III | NR |
| Gölge et al. [27] | 2016 | Turkey | 202 | 90:112 | HA: 78.6 PFN: 75.7 | Retrospective | Mortality | III | NR |
| Iorio et al. [28] | 2019 | Italy | 60 | 25:35 | HA: 83 THA: 82 | Prospective randomized | Dislocation rate at a minimum follow-up of 1 year, reoperation rate, time to surgery, surgical time, length of hospital stay, 30-day and 1-year mortality | I | NR |
| Jonas et al. [29] | 2015 | UK | 132 | 22:88 | HA: 79 THA: 78 | Retrospective | Functional outcome (Oxford Hip Score), quality of life (SF-36), complications | III | NR |
| Ju et al. [30] | 2020 | China | 73 | 16:57 | 68.22 | Retrospective | Necrosis of femoral head, functional outcome (Harris Hip score) | III | NR |
| Karaali et al. [31] | 2021 | Turkey | 129 | 44:85 | Metaphyseal fixed HA: 78 Diaphyseal fixed HA: 79 | Retrospective | 2-year functional outcome (Harris hip score, Parker Mobility Score), mortality | III | NR |
| Kawaji et al. [32] | 2015 | Japan | 42 | 9:33 | Asian IMHS: 78.4 Conv. IMHS:82.3 | Retrospective | Walking ability, complications | III | NR |
| Khan et al. [33] | 2021 | India | 88 | 43:45 | Unipolar group: 67.2 Bipolar group: 66.1 | Prospective randomized | Radiological outcome, functional outcome (Harris hip score) | I | NR |
| Knauf et al. [34] | 2019 | Germany | 395 | 109:286 | 81 | Prospective | Mortality | II | NR |
| Koyuncu et al. [35] | 2015 | Turkey | 152 | 67:85 | 76 | Prospective | Clinical and radiological outcomes, complications | II | NR |
| Kusen et al. [36] | 2019 | Switzerland | 322 | 87:225 | 2013: 86 2016: 85 | Retrospective and prospective cohort | Peri-operative data, postoperative outcomes and complications | III | Osteoporosis screening, referral to general practitioner |
| Kusen et al. [37] | 2021 | Switzerland | 752 | 203:549 | 86 | Prospective cohort | Mortality, complications, time to surgical intervention, hospital length of stay | II | BMD testing (DEXA scan) |
| Laubach et al. [38] | 2021 | Germany | 1727 | 584:1143 | Internal fixation: 81 Arthroplasty: 83 | Retrospective | Μobility, residential status, reoperation rate, HRQoL, mortality | III | NR |
| Lee et al. [72] | 2021 | Canada | 212 | 49:163 | Preintervention group: 84 Postintervention group: 85 | Retrospective | Length of stay, incidence of delirium | III | Osteoporosis assessment, prescription of calcium and vitamin D |
| Lee et al. [88] | 2019 | South Korea | 234 | 49:185 | 80.6 | Prospective cohort | Clinical outcomes (Koval’s categories for walking ability), radiographic outcome | II | NR |
| Leonardsson et al. [39] | 2016 | Sweden | 2128 | 559:1569 | 85 | Retrospective | Quality of life, pain | III | NR |
| Li et al. [40] | 2018 | China | 43 | 17:26 | 76.5 | Retrospective | Functional outcome (Harris hip score), mobility (TUG test, Parker score | III | NR |
| Liang et al. [41] | 2022 | China | 87 | 32:55 | PFNA: 86.1 External fixation: 85.6 | Prospective randomized | Functional and radiographic outcomes, complications | I | NR |
| Liu et al. [42] | 2020 | China | 156 | 75:81 | HA: 78.1 Fixation: 76.2 | Prospective cohort | Quality of life, cost-effectiveness | II | NR |
| Lu et al. [43] | 2016 | China | 78 | 20:68 | Fixation: 85.85 HA: 86.24 | Prospective randomized | Operative outcome, hip functions | I | NR |
| MacLellan et al. [44] | 2024 | Canada | 659 | 193:489 | 82.8 | Retrospective | Length of stay, discharge location, mortality | III | NR |
| Mallick et al. [45] | 2019 | UK | 168 | 45:122 | 82 | Retrospective | Complications, mortality | III | NR |
| Moaz et al. [46] | 2024 | Pakistan | 102 | 56:46 | 65.4 | Prospective cohort | Functional outcome (Harris hip score) | II | NR |
| Moore et al. [47] | 2023 | Ireland | 7.109 | 2.203/4.906 | 81 | Retrospective registry study | Post-op mobility, 7-day and 14-day inpatient mortality, discharge destination | III | NR |
| Morris et al. [48] | 2023 | New Zealand | 181 | 46:135 | 2011 cohort: 84.2 2017 cohort: 82.6 | Retrospective | Length of stay, postoperative complications, 30-day and 1-year mortality | III | Assessment of risk factors, metabolic blood tests screening |
| Mukka et al. [49] | 2020 | Sweden | 235 | 75:160 | 83 | Prospective pilot study | Functional outcome (Harris hip score, WOMAC), pain (PNRS) | II | NR |
| Okano et al. [50] | 2017 | Japan | 16 | 2:14 | 86.9 | Retrospective | Implant-related complications | III | NR |
| Park et al. [93] | 2022 | Korea | 34 | 9:25 | 82.68 | Prospective cohort | Operation time, bleeding, time to walk, complications | II | NR |
| Peddamadyam et al. [51] | 2024 | India | 20 | 8:12 | 71.65 | Prospective cohort | Clinical outcome, complications | II | NR |
| Prestmo et al. [52] | 2015 | Norway | 397 | 104:293 | 83 | Prospective randomized study | Mobility at 4 months (SPPB) | I | NR |
| Prieto-Alhambra et al. [53] | 2018 | Spain | 997 | 232:765 | 83.6 | Prospective cohort | In-patient care, complications, and 4-month mortality | II | Osteoporosis not assessed for 23.6%, assessed but treatment unnecessary for 20.5%, 14.9% awaiting an osteoporosis clinical assessment, 3.2% discharged pending a DXA scan, prescription of anti-osteoporotic treatment at 21.4% |
| Ratanpai et al. [54] | 2025 | India | 110 | 37:73 | 71.3 | Prospective cohort | Functional outcome (modified Harris hip score and Oxford Hip Score), 1-year mortality | II | NR |
| Regis et al. [55] | 2023 | Italy | 139 | 41:98 | Uncemented HA: 80.1 Cemented HA: 84.3 | Retrospective cohort | Surgical time, overall perioperative complication rate | II | NR |
| Roll et al. [90] | 2018 | Germany | 1015 | 275:740 | 83.2 | Prospective cohort | Procedural and patient outcome parameters | II | NR |
| Sadeghi et al. [56] | 2020 | USA | 5526 | 1658:3868 | Long nail: 80.6 Short nail: 81.2 | Retrospective cohort | Risks of all-cause revision and revision for periprosthetic fracture | III | NR |
| Salvesen et al. [57] | 2025 | Norway | 398 | 116:282 | 83 | Prospective cohort | SPPB, EuroQol-5-dimension and5-level, Barthel index, Lawton and Brody Instrumental Activities of Daily Living, Lawton and Brody Self-Maintenance Scale, readmission and mortality | II | NR |
| Sanderson-Jerome [58] | 2024 | TTO | 30 | 13:17 | 82.0 | Prospective cohort | Time to surgery (lead time), complications by Clavien–Dindo score, hospital length of stay and mortality, and costs of hospitalization | II | NR |
| Schoenberg et al. [59] | 2021 | Germany | 9780 | 84.4 | Retrospective registry | Rate of readmission, rate of re-surgery, anti-osteoporotic therapy, housing, mortality, walking ability, and quality of life 120 days post-surgery | III | Initiation of anti-osteoporotic medication | |
| Schuijt et al. [60] | 2020 | Netherlands | 806 | 579 | 85 | Retrospective cohort | Postoperative complications, patient mortality, time spent at the emergency department, time to surgery, hospital length of stay | III | NR |
| Sun et al. [62] | 2023 | China | 701 | 201:500 | Early surgery: 80.1 Late surgery: 79.56 | Retrospective | Quality of life, complications | III | NR |
| Sun et al. [61] | 2024 | China | 669 | 179:490 | 72.49 | Multicenter cross-sectional study | Current status of postoperative care for elderly osteoporotic fracture patient | II | Osteoporosis treatment for 303 (45.3%) patients after surgery |
| Sun et al. [63] | 2024 | China | 40 | 10:30 | ITF: 72.8 PFNA: 73.7 | Retrospective cohort | Surgical and rehabilitation data, functional outcome (Harris hip score), quality of life (SF-36), complications | III | NR |
| Solberg et al. [64] | 2023 | Norway | 516 | 146:370 | 84 | Prospective cohort | Comparison of two orthogeriatric care models | II | Treatment with anti-osteoporosis drugs in hospital: 70% |
| Sniderman et al. [65] | 2023 | Canada | 150 | 34:116 | HA: 83.2 ORIF: 84 | Retrospective cohort | Blood loss, complications | III | NR |
| Song et al. [66] | 2020 | China | 94 | 62:32 | Control group: 70.6 Delayed group: 73 | Prospective cohort | Functional outcome (Harris hip score), quality of life | II | NR |
| Sundkvist et al. [67] | 2024 | Sweden | 291 | 139:152 | 82 | Multicenter prospective cohort | Treatment failure, reoperations, mortality rate at 30 days, 90 days, and 1 year | II | NR |
| Tan et al. [68] | 2017 | Singapore | 2029 | 518:1511 | 78.8 | Retrospective | Complications, ambulatory status at discharge, length of hospital stay | III | NR |
| Takahashi et al. [74] | 2020 | Japan | 228 | 56:172 | 85 | Retrospective cohort | Patients’ ambulation ability before injury, at discharge, and 6 months after injury (Functional Ambulation Category), presurgical duration, length of hospital stay, time until beginning to walk using parallel bars, complications affecting treatment, mortality rate | III | NR |
| Tian et al. [75] | 2020 | China | 90 | 48:42 | 70.5 | Prospective cohort | Functional outcome (Harris hip score), complications | II | NR |
| Tilaveridis et al. [76] | 2023 | Greece | 118 | 82.7 | Prospective cohort | Radiographic outcome, complications | II | NR | |
| Tol et al. [77] | 2017 | Netherlands | 252 | 47:205 | 81.1 | Prospective randomized | Functional outcome, (modified Harris hip score), postoperative complications, intra-operative data | I | NR |
| Uzel et al. [78] | 2024 | Turkey | 53,495 | 35.841:17.654 | 86 | Retrospective registry | Complication, mortality | III | NR |
| Vasu et al. [79] | 2018 | India | 60 | 34:26 | Prospective cohort | Association of modified frailty index (MFI) with 90-day mortality | II | NR | |
| Vigano et al. [82] | 2023 | Italy | 79,120 | 17,040:54,877 | 84 | Retrospective registry | Fracture incidence, epidemiology, mortality, cost | III | NR |
| Wang et al. [83] | 2023 | China | 644 | 174:470 | 81.66 | Retrospective | 1-year mortality, major complications, and AKI by BMI category | III | NR |
| Wang et al. [82] | 2022 | China | 761 | 247:514 | 81.23 | Retrospective | Length of hospital stay, postoperative complications, 30-day and one-year mortalities, one-year functional status | III | NR |
| Wignadasan et al. [84] | 2024 | UK | 335 | 105:224 | Cemented: 84.7 Uncemented: 85.9 | Retrospective | Length of hospital stay, discharge destination, morbidity, mortality, theater time, cost | III | NR |
| Xu et al. [85] | 2025 | China | 300 | 161:139 | 85.88 | Prospective cohort | Fracture reduction, Harris hip score at 1 and 6 months after surgery, failure of internal fixation | II | NR |
| Yan et al. [86] | 2024 | China | 80 | 23:57 | 80.5 | Retrospective | Torn conjoined tendons, dislocation and complication rate | III | NR |
| Yin et al. [87] | 2024 | China | 141 | 50:91 | DAA: 73.98 PLA: 76.72 | Retrospective | Hospitalization days, VAS score, Harris hip score at one month and six months, incidence of complications, revision rate, one-year survival rate, patient satisfaction | III | NR |
| Yu et al. [80] | 2016 | China | 117 | 67:80 | PFNA-II: 74.2 IT group: 75.2 | Prospective | Intraoperative variables, postoperative complications | II | NR |
| Zhou et al. [91] | 2020 | China | 224 | 114:110 | 68.52 | Prospective cohort | Functional outcome (Harris hip score), rates of revision, loosening, periprosthetic fracture, dislocation | II | NR |
| Zhou et al. [92] | 2019 | China | 108 | 63:45 | 75.3 | Prospective cohort | Operation time, intraoperative bleeding, immobilization duration, hospitalization time, Harris hip score, postoperative complications | II | BMD testing (DXA), initiation of alendronate and vitamin D3 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Daskalakis, I.I.; Bastian, J.D.; Tosounidis, T.H. Time Is Bone: Missed Opportunities for Secondary Prevention After a Hip Fracture. J. Clin. Med. 2025, 14, 5816. https://doi.org/10.3390/jcm14165816
Daskalakis II, Bastian JD, Tosounidis TH. Time Is Bone: Missed Opportunities for Secondary Prevention After a Hip Fracture. Journal of Clinical Medicine. 2025; 14(16):5816. https://doi.org/10.3390/jcm14165816
Chicago/Turabian StyleDaskalakis, Ioannis I., Johannes D. Bastian, and Theodoros H. Tosounidis. 2025. "Time Is Bone: Missed Opportunities for Secondary Prevention After a Hip Fracture" Journal of Clinical Medicine 14, no. 16: 5816. https://doi.org/10.3390/jcm14165816
APA StyleDaskalakis, I. I., Bastian, J. D., & Tosounidis, T. H. (2025). Time Is Bone: Missed Opportunities for Secondary Prevention After a Hip Fracture. Journal of Clinical Medicine, 14(16), 5816. https://doi.org/10.3390/jcm14165816






