Management and Outcomes of Non-Missile Penetrating Brain Injury Involving the Anterior Skull Base: A Case Report and Systematic Review
Abstract
1. Introduction
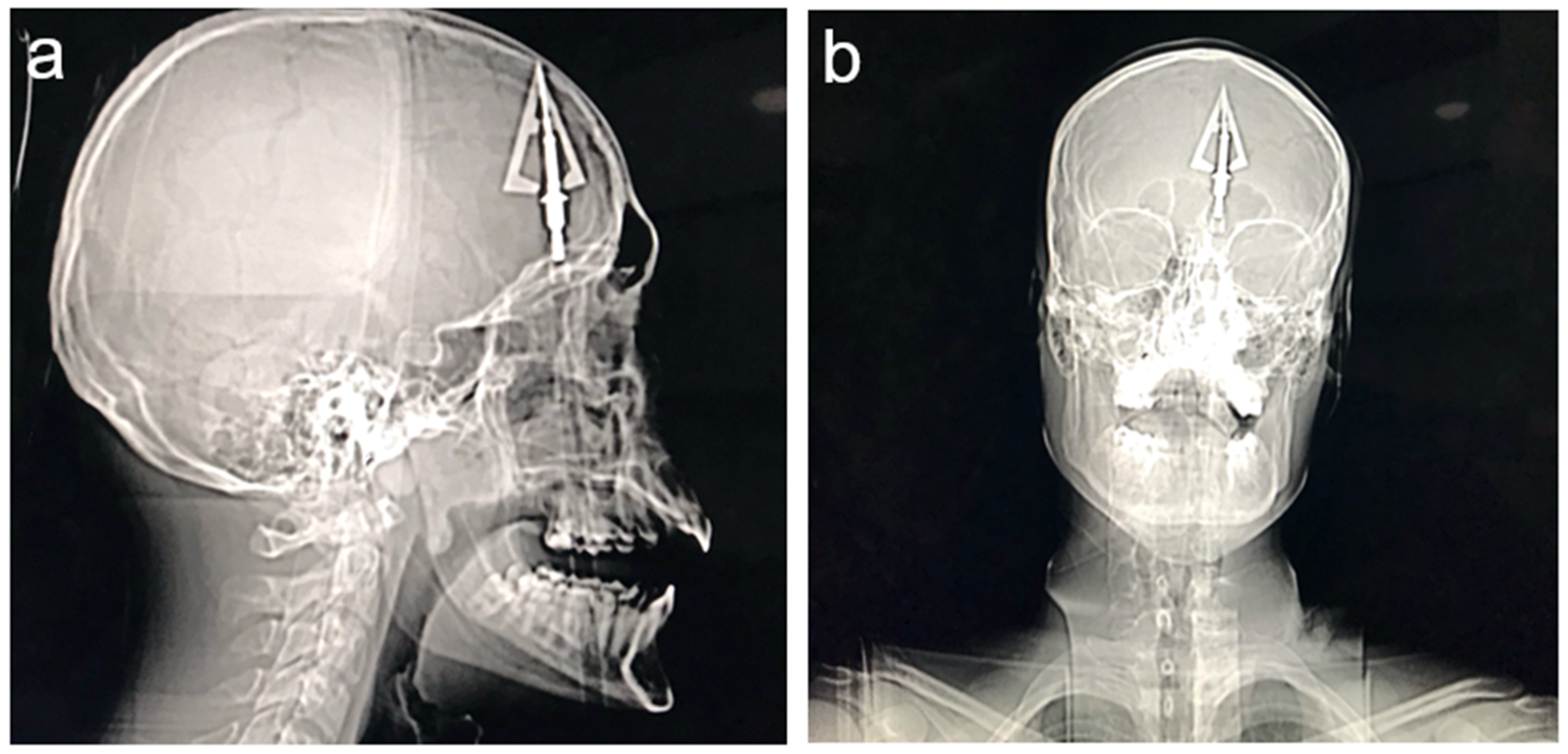
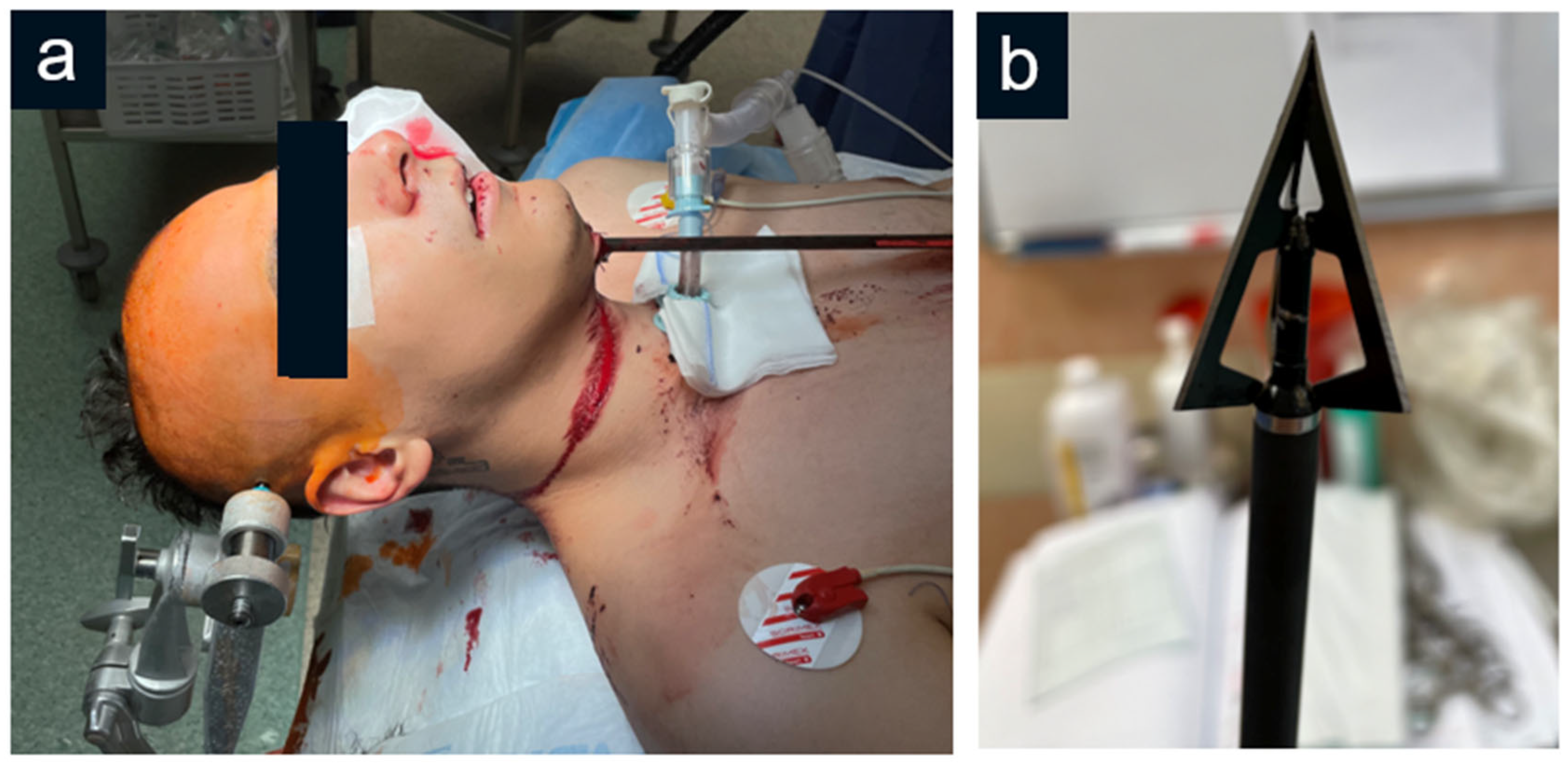
2. Case Description
2.1. Clinical Presentation
2.2. Surgical Procedure
2.3. Postoperative Course
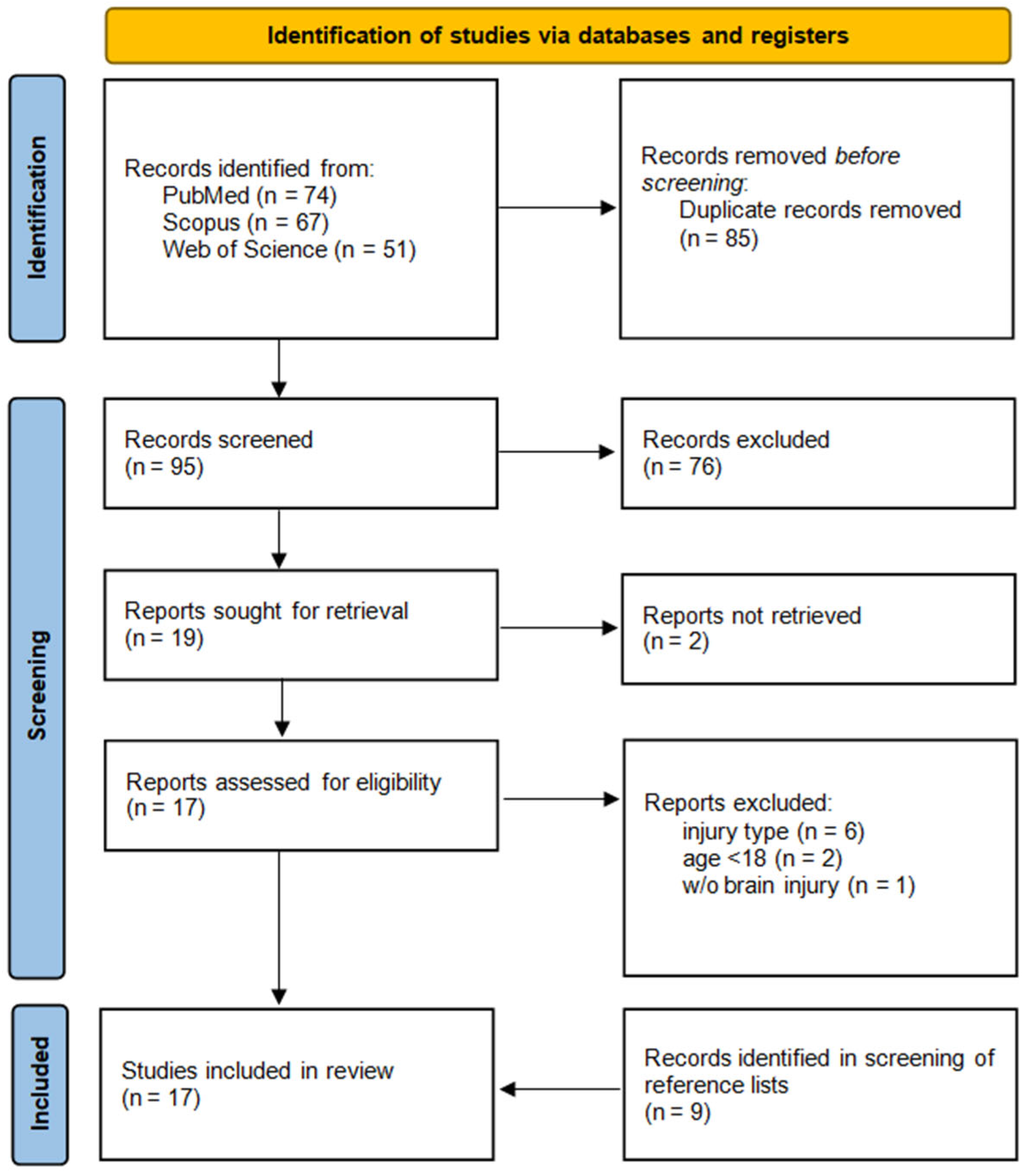
3. Systematic Literature Review
3.1. Materials and Methods
3.2. Results
3.2.1. Search Results
3.2.2. Characteristics of Included Articles
3.2.3. Quality Assessment of Included Articles
3.2.4. Characteristics of Patients with Non-Missile PBIs Involving the Anterior Skull Base
3.2.5. Management and Outcome
3.2.6. Complications
4. Discussion
5. Conclusions
Supplementary Materials
Funding
Data Availability Statement
Conflicts of Interest
References
- Skarupa, D.J.; Khan, M.; Hsu, A.; Madbak, F.G.; Ebler, D.J.; Yorkgitis, B.; Rahmathulla, G.; Alcindor, D.; Joseph, B. Trends in civilian penetrating brain injury: A review of 26,871 patients. Am. J. Surg. 2019, 218, 255–260. [Google Scholar] [CrossRef] [PubMed]
- Alao, T.; Munakomi, S.; Waseem, M. Penetrating Head Trauma. In StatPearls; StatPearls Publishing: Treasure Island, FL, USA, 2024. [Google Scholar]
- Zyck, S.; Toshkezi, G.; Krishnamurthy, S.; Carter, D.A.; Siddiqui, A.; Hazama, A.; Jayarao, M.; Chin, L. Treatment of Penetrating Nonmissile Traumatic Brain Injury. Case Series and Review of the Literature. World Neurosurg. 2016, 91, 297–307. [Google Scholar] [CrossRef] [PubMed]
- Young, L.; Rule, G.T.; Bocchieri, R.T.; Walilko, T.J.; Burns, J.M.; Ling, G. When physics meets biology: Low and high-velocity penetration, blunt impact, and blast injuries to the brain. Front. Neurol. 2015, 6, 89. [Google Scholar] [CrossRef] [PubMed]
- Kazim, S.F.; Shamim, M.S.; Tahir, M.Z.; Enam, S.A.; Waheed, S. Management of penetrating brain injury. J. Emergencies Trauma Shock 2011, 4, 395–402. [Google Scholar] [CrossRef]
- Harrington, B.M.; Gretschel, A.; Lombard, C.; Lonser, R.R.; Vlok, A.J. Complications, outcomes, and management strategies of non-missile penetrating head injuries. J. Neurosurg. 2020, 134, 1658–1666. [Google Scholar] [CrossRef]
- Di Ieva, A.; Audigé, L.; Kellman, R.M.; Shumrick, K.A.; Ringl, H.; Prein, J.; Matula, C. The Comprehensive AOCMF Classification: Skull Base and Cranial Vault Fractures—Level 2 and 3 Tutorial. Craniomaxillofac. Trauma Reconstr. 2014, 7 (Suppl. 1), 103–113. [Google Scholar] [CrossRef]
- Yellinek, S.; Cohen, A.; Merkin, V.; Shelef, I.; Benifla, M. Clinical significance of skull base fracture in patients after traumatic brain injury. J. Clin. Neurosci. 2016, 25, 111–115. [Google Scholar] [CrossRef]
- Zhang, D.; Chen, J.; Han, K.; Yu, M.; Hou, L. Management of Penetrating Skull Base Injury: A Single Institutional Experience and Review of the Literature. BioMed Res. Int. 2017, 2017, 2838167. [Google Scholar] [CrossRef]
- Aljuboori, Z.; McGrath, M.; Levitt, M.; Moe, K.; Chestnut, R.; Bonow, R. A case series of crossbow injury to the head highlighting the importance of an interdisciplinary management approach. Surg. Neurol. Int. 2022, 13, 60. [Google Scholar] [CrossRef]
- Aydin, S. Intracranial Penetrating Trauma Caused by Fishing Sinker. World Neurosurg. 2019, 129, 237–240. [Google Scholar] [CrossRef]
- Lan, Z.; Richard, S.; Ma, L.; Yang, C. Nonmissile anterior skull-base penetrating brain injury: Experience with 22 patients. Asian J. Neurosurg. 2018, 13, 742–748. [Google Scholar] [CrossRef] [PubMed]
- Asadullah, A.; Harmawan, E.W.; Prastikarunia, R.; Putra, G.H.; Kustono, H.; Utama, A.S.; Artha, K.S.A.; Apriawan, T.; Bajamal, A.H. Management of penetrating brain injury: A case report. Indones. J. Neurosurg. 2020, 3, 74–79. [Google Scholar] [CrossRef]
- Hyung, J.W.; Lee, J.J.; Lee, E.; Lee, M.H. Penetrating Orbitocranial Injuries in the Republic of Korea. Korean J. Neurotrauma 2023, 19, 314–323. [Google Scholar] [CrossRef] [PubMed]
- Li, X.S.; Yan, J.; Liu, C.; Luo, Y.; Liao, X.-S.; Yu, L.; Xiao, S.-W. Nonmissile Penetrating Head Injuries: Surgical Management and Review of the Literature. World Neurosurg. 2017, 98, 873.e9–873.e25. [Google Scholar] [CrossRef]
- Abdelhameid, A.K.; Saro, A. Non-missile penetrating brain injuries: Cases registry in Sohag University Hospital. Egypt. J. Neurosurg. 2019, 34, 24. [Google Scholar] [CrossRef]
- Del Castillo-Calcáneo, J.D.; Bravo-Angel, U.; Mendez-Olan, R.; Rodriguez-Valencia, F.; Valdés-García, J.; García-González, U.; Broc-Haro, G.G. Traumatic brain injury with a machete penetrating the dura and brain: Case report from southeast Mexico. Int. J. Surg. Case Rep. 2016, 23, 169–172. [Google Scholar] [CrossRef]
- De Holanda, L.F.; Pereira, B.J.A.; Holanda, R.R.; Neto, J.T.; de Holanda, C.V.M.; Filho, M.G.; de Oliveira, N.R.C.; de Oliveira, J.G. Neurosurgical Management of Nonmissile Penetrating Cranial Lesions. World Neurosurg. 2016, 90, 420–429. [Google Scholar] [CrossRef]
- Kondo, T.; Takahashi, M.; Kuse, A.; Morichika, M.; Nakagawa, K.; Tagawa, Y.; Taniguchi, T.; Taguchi, Y.; Fujiwara, T.; Tsuchiya, J.; et al. Autopsy Case of a Penetrating Wound to the Left Cerebral Hemisphere Caused by an Accidental Shooting with a Crossbow. Am. J. Forensic Med. Pathol. 2018, 39, 164–168. [Google Scholar] [CrossRef]
- Prasetyo, E.; Oley, M.C.; Sumual, V.; Faruk, M. Transorbital-penetrating intracranial injury due to a homemade metal arrow: A case report. Ann. Med. Surg. 2020, 57, 183–189. [Google Scholar] [CrossRef]
- Paramhans, D.; Shukla, S.; Batra, A.; Mathur, R.K. Successful removal of an impacted metallic arrowhead penetrating up to the brainstem. J. Emergencies Trauma Shock 2010, 3, 303. [Google Scholar] [CrossRef]
- Adamu, A.; Abdullahi, H.; Hasheem, M.G. Penetrating Arrow Injuries of the Head-and-Neck Region: Case Series and Review of Literature. Niger. Med. J. 2020, 61, 276–280. [Google Scholar] [CrossRef]
- Karger, B.; Sudhues, H.; Kneubuehl, B.P.; Brinkmann, B. Experimental arrow wounds: Ballistics and traumatology. J. Trauma: Inj. Infect. Crit. Care 1998, 45, 495–501. [Google Scholar] [CrossRef] [PubMed]
- Al-Alousi, H.M.; Al-Kubaisi, K.T.; Ismail, M.; Al-Ageely, T.A.; Abdulameer, A.O.; Aluaibi, S.A.; Al-Taie, R.H.; Hoz, S.S. Transbasal penetrating traumatic brain injury caused by a rifle rod: A case report. Surg. Neurol. Int. 2022, 13, 555. [Google Scholar] [CrossRef] [PubMed]
- Anwer, M.; Kumar, A.; Kumar, A.; Kumar, D.; Ahmed, F. Penetrating Sugarcane Injury to Brain via Orbit: A Case Report. Korean J. Neurotrauma 2024, 20, 52–56. [Google Scholar] [CrossRef] [PubMed]
- Vakil, M.T.; Singh, A.K. A review of penetrating brain trauma: Epidemiology, pathophysiology, imaging assessment, complications, and treatment. Emerg. Radiol. 2017, 24, 301–309. [Google Scholar] [CrossRef]
- Gökçek, C.; Erdem, Y.; Köktekir, E.; Karatay, M.; Bayar, M.A.; Edebali, N.; Kiliç, C. Intracranial foreign body. Turk Neurosurg. 2007, 17, 121–124. [Google Scholar]
- Gutiérrez-González, R.; Boto, G.R.; Rivero-Garvía, M.; Pérez-Zamarrón, Á.; Gómez, G. Penetrating brain injury by drill bit. Clin. Neurol. Neurosurg. 2008, 110, 207–210. [Google Scholar] [CrossRef]
- Luo, W.; Liu, H.; Hao, S.; Zhang, Y.; Li, J.; Liu, B. Penetrating brain injury caused by nail guns: Two case reports and a review of the literature. Brain Inj. 2012, 26, 1756–1762. [Google Scholar] [CrossRef]
- Harmon, L.A.; Haase, D.J.; Kufera, J.A.; Adnan, S.; Cabral, D.; Lottenberg, L.; Cunningham, K.W.; Bonne, S.; Burgess, J.; Etheridge, J.; et al. Infection after penetrating brain injury—An Eastern Association for the Surgery of Trauma multicenter study oral presentation at the 32nd annual meeting of the Eastern Association for the Surgery of Trauma, January 15–19, 2019, in Austin, Texas. J. Trauma Acute Care Surg. 2019, 87, 61–67. [Google Scholar] [CrossRef]
- Norman, G.; Atkinson, R.A.; Smith, T.A.; Rowlands, C.; Rithalia, A.D.; Crosbie, E.J.; Dumville, J.C. Intracavity lavage and wound irrigation for prevention of surgical site infection. Cochrane Database Syst. Rev. 2017, 2017, CD012234. [Google Scholar] [CrossRef]
- Sunshine, K.; Penuela, M.; Defta, D.; Herring, E.; Sajatovic, M.; Traeger, J.; Shammassian, B.H. Antibiotic Prophylaxis in Penetrating Brain Injury: A Systematic Review of the Literature. Neurosurgery 2020, 67 (Suppl. 1), 145. [Google Scholar] [CrossRef]
- Benzel, E.C.; Day, W.T.; Kesterson, L.; Willis, B.K.; Kessler, C.W.; Modling, D.; Hadden, T.A. Civilian craniocerebral gunshot wounds. Neurosurgery 1991, 29, 62–67. [Google Scholar] [CrossRef]
- Bayston, R.; de Louvois, J.; Brown, E.M.; Johnston, R.A.; Lees, P.; People, I.K. Use of antibiotics in penetrating craniocerebral injuries. Lancet 2000, 355, 1813–1817. [Google Scholar] [CrossRef]
- Aarabi, B. Causes of infections in penetrating head wounds in the Iran-Iraq War. Neurosurgery 1989, 25, 923. [Google Scholar] [CrossRef]
- Hakkarainen, T.W.; Dellinger, E.P.; Evans, H.L.; Farjah, F.; Farrokhi, E.; Steele, S.R.; Thirlby, R.; Flum, D.R. Comparative effectiveness of skin antiseptic agents in reducing surgical site infections: A report from the Washington State Surgical Care and Outcomes Assessment Program. J. Am. Coll. Surg. 2014, 218, 336–344. [Google Scholar] [CrossRef]
- Kaoutzanis, C.; Kavanagh, C.M.; Leichtle, S.W.; Welch, K.B.; Talsma, A.; Vandewarker, J.F.; Lampman, R.M.; Cleary, R.K. Chlorhexidine with isopropyl alcohol versus iodine povacrylex with isopropyl alcohol and alcohol- versus nonalcohol-based skin preparations: The incidence of and readmissions for surgical site infections after colorectal operations. Dis. Colon Rectum 2015, 58, 588–596. [Google Scholar] [CrossRef]
- Peel, T.N.; Watson, E.; Lee, S.J. Randomised Controlled Trials of Alcohol-Based Surgical Site Skin Preparation for the Prevention of Surgical Site Infections: Systematic Review and Meta-Analysis. J. Clin. Med. 2021, 10, 663. [Google Scholar] [CrossRef]
- Siddiqi, A.; Abdo, Z.E.; Rossman, S.R.; Kelly, M.A.; Piuzzi, N.S.; Higuera, C.A.; Schwarzkopf, R.; Springer, B.D.; Chen, A.F.; Parvizi, J. What Is the Optimal Irrigation Solution in the Management of Periprosthetic Hip and Knee Joint Infections? J. Arthroplast. 2021, 36, 3570–3583. [Google Scholar] [CrossRef]
- Severing, A.L.; Rembe, J.D.; Koester, V.; Stuermer, E.K. Safety and efficacy profiles of different commercial sodium hypochlorite/hypochlorous acid solutions (NaClO/HClO): Antimicrobial efficacy, cytotoxic impact and physicochemical parameters In Vitro. J. Antimicrob. Chemother. 2019, 74, 365–372. [Google Scholar] [CrossRef]
- Okunlola, A.I.; Adeolu, A.A.; Malomo, A.O.; Okunlola, C.K.; Shokunbi, M.T. Intra-operative wound irrigation with ceftriaxone does not reduce surgical site infection in clean neurosurgical procedures. Br. J. Neurosurg. 2021, 35, 766–769. [Google Scholar] [CrossRef]
- Loggini, A.; Vasenina, V.I.; Mansour, A.; Das, P.; Horowitz, P.M.; Goldenberg, F.D.; Kramer, C.; Lazaridis, C. Management of civilians with penetrating brain injury: A systematic review. J. Crit. Care 2020, 56, 159–166. [Google Scholar] [CrossRef]
- Yoneoka, Y.; Aizawa, N.; Nonomura, Y.; Ogi, M.; Seki, Y.; Akiyama, K. Traumatic Nonmissile Penetrating Transnasal Anterior Skull Base Fracture and Brain Injury with Cerebrospinal Fluid Leak: Intraoperative Leak Detection and an Effective Reconstruction Procedure for a Localized Skull Base Defect Especially After Coronavirus Disease 2019 Outbreak. World Neurosurg. 2020, 140, 166–172. [Google Scholar] [CrossRef]
- Khayat, M.A.; Khayat, H.; Alhantoobi, M.R.; Aljoghaiman, M.; Sommer, D.D.; Algird, A.; Guha, D. Traumatic penetrating head injury by crossbow projectiles: A case report and literature review. Surg. Neurol. Int. 2024, 15, 35. [Google Scholar] [CrossRef]
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. BMJ 2021, 372, n71. [Google Scholar] [CrossRef]
| No. | Search Query |
|---|---|
| #1 | “Brain Injuries, Traumatic” [MeSH] OR “traumatic brain injur *” [tiab] OR “craniocerebral injur *” [tiab] OR “traumatic head injur *” [tiab] OR “neurotrauma *” [tiab] OR “cerebral injur *” [tiab] OR “brain injur *” [tiab] |
| #2 | “Wounds, Stab” [MeSH] OR “nonmissile” [tiab] OR “non-missile” [tiab] OR “non missile” [tiab] OR “stab injur *” [tiab] OR “stabbing” [tiab] OR “foreign bod *” [tiab] OR “stab *” [tiab] OR “Head Injuries, Penetrating” [MeSH] OR “penetrat *” [tiab] OR “penetrating brain injur *” [tiab] |
| #3 | “Cranial Fossa, Anterior” [MeSH] OR “anterior skull base” [tiab] OR “anterior skull-base” [tiab] OR “anterior cranial base” [tiab] OR “frontal base” [tiab] OR “frontal bone” [tiab] OR “ethmoid *” [tiab] OR “sphenoid *” [tiab] OR “anterior cranial fossa” [tiab] OR “skull * base” [tiab] OR “skull-base” [tiab] |
| #4 | #1 AND #2 AND #3 |
| Article No. | Authors | Year | Country | Case No. | Age | Gender | Mechanism | Injury Cause | Type of Injury | Type of Imaging | Type of Management | Other Specialists Assistance | Infection Prophylaxis | Outcome |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Current case | 2024 | Poland | 1 | 20 | M | suicide attempt | crossbow | transmental | CT | surgical | ENT surgeon | yes | olfactory dysfunction | |
| 1 | Khayat | 2024 | Canada | 2 | 31 | M | suicide attempt | crossbow | transmental | CT and CTA | surgical | ENT surgeon | not reported | no deficit |
| 2 | Anwer | 2024 | India | 3 | 32 | M | accidental | sugarcane | transorbital | CT | surgical | ophtalmologist | yes | loss of vision |
| 3 | Hyung | 2023 | Korea | 4 | 41 | F | accidental | tree branch | transnasal | CT | surgical | - | yes | no deficit |
| 5 | 60 | M | accidental | electric drill | transorbital | CT | non-operative | - | yes | no deficit | ||||
| 4 | Al-Alousi | 2022 | Iraq | 6 | 30 | M | accidental | rifle rod | transnasal | CT and plain radiographs | surgical | maxillofacial surgeon and ENT surgeon | yes | no deficit |
| 5 | Widodo | 2022 | Indonesia | 7 | 28 | M | accidental | wooden stick | transnasal | CT and plain radiographs | surgical | ENT surgeon | yes | no deficit |
| 6 | Gupta | 2022 | India | 8 | 24 | F | accidental | pressure cooker nozzle | transorbital | CT and plain radiographs | surgical | - | not reported | loss of vision |
| 7 | Aljuboori | 2022 | United States | 9 | 22 | M | suicide attempt | crossbow | transmental | CT, CTA, and DSA | surgical | ENT surgeon | not reported | n/r |
| 10 | 67 | M | suicide attempt | crossbow | transmental | CT, CTA, and DSA | surgical | ENT surgeon | not reported | n/r | ||||
| 11 | 36 | M | suicide attempt | crossbow | transmental | CT, MRI, CTA, and DSA | surgical | ENT surgeon | not reported | n/r | ||||
| 8 | Yoneoka | 2020 | Japan | 12 | 65 | M | accidental | garden pole | transnasal | CT | non-operative | - | yes | no deficit |
| 9 | Prasetyo | 2020 | Indonesia | 13 | 28 | M | accidental | metal arrow | transorbital | CT, CTA, and plain radiographs | surgical | ophtalmologist | yes | loss of vision |
| 10 | Asadullah | 2020 | Indonesia | 14 | 43 | M | violence | wooden stick | transorbital | CT and CTA | surgical | ophtalmologist | yes | impaired vision |
| 15 | 18 | M | accidental | fish bullet | transorbital | CT and CTA | surgical | ophtalmologist | yes | no deficit | ||||
| 16 | 36 | M | accidental | fish bullet | transorbital | CT | surgical | - | yes | no deficit | ||||
| 11 | Aydin | 2019 | Turkey | 17 | 37 | M | accidental | fishing sinker | transorbital | CT | surgical | - | not reported | right hemiparesis |
| 12 | Lan | 2018 | China | 18 | 51 | M | accidental | wooden stick | transorbital | CT and MRI | surgical | - | yes | no deficit |
| 19 | 22 | M | violence | metal rod | transorbital | CT and MRI | surgical | - | yes | no deficit | ||||
| 20 | 30 | M | accidental | wooden stick | transorbital | CT and MRI | surgical | - | yes | no deficit | ||||
| 21 | 40 | M | violence | wooden stick | transorbital | CT and MRI | surgical | - | yes | no deficit | ||||
| 22 | 29 | M | accidental | wooden stick | transorbital | CT and MRI | surgical | - | yes | right oculomotor palsy | ||||
| 23 | 32 | M | violence | knife | transorbital | CT and MRI | surgical | - | yes | right oculomotor palsy | ||||
| 24 | 31 | M | accidental | chopstick | transorbital | CT and MRI | surgical | - | yes | right abducens palsy | ||||
| 25 | 44 | M | accidental | wooden stake | transorbital | CT, MRI, and CTA | surgical | - | yes | no deficit | ||||
| 26 | 43 | M | accidental | bamboo stick | transorbital | CT, MRI | surgical | - | yes | no deficit | ||||
| 27 | 32 | M | violence | nail | transorbital | CT and MRI | non-operative | - | yes | no deficit | ||||
| 28 | 42 | M | accidental | wooden stick | transorbital | CT and MRI | surgical | - | yes | no deficit | ||||
| 29 | 23 | M | violence | pool cue | transorbital | CT and MRI | surgical | - | yes | loss of vision | ||||
| 30 | 41 | M | accidental | wooden stick | transnasal | CT and MRI | surgical | - | yes | loss of vision | ||||
| 31 | 22 | M | accidental | tree twig | transorbital | CT and MRI | surgical | - | yes | left oculomotor palsy | ||||
| 32 | 51 | M | accidental | tree twig | transorbital | CT and MRI | surgical | - | yes | no deficit | ||||
| 13 | Zhang | 2017 | China | 33 | 75 | F | accidental | bamboo stick | transorbital | CT, MRI, and DSA | surgical | - | yes | no deficit |
| 34 | 42 | M | accidental | electric drill | transorbital | CT | non-operative | - | yes | no deficit | ||||
| 35 | 29 | M | accidental | screw | transorbital | CT | surgical | - | yes | oculomotor nerve injury and impaired vision | ||||
| 36 | 40 | M | accidental | hot projective oil paint | transorbital | CT and MRI | surgical | - | yes | loss of vision | ||||
| 14 | Li | 2017 | China | 37 | 34 | M | accidental | metal rod | transmental | CT and CTA | surgical | ENT surgeon | yes | loss of vision |
| 38 | 52 | M | accidental | metal rod | transorbital | CT, CTA, and DSA | surgical | - | yes | coma | ||||
| 15 | Chowdhury | 2016 | Bangladesh | 39 | 45 | M | violence | bamboo stick | transorbital | CT and plain radiographs | surgical | - | not reported | loss of vision |
| 16 | Tewari | 2015 | India | 40 | 35 | M | accidental | metal rod | transorbital | plain radiographs | surgical | - | yes | ptosis |
| 17 | Sweeney | 2011 | United States | 41 | 31 | M | suicide attempt | knife | transmental | CT and CTA | surgical | ENT surgeon | not reported | no deficit |
| No. | Author | Year | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 |
|---|---|---|---|---|---|---|---|---|---|---|
| 1 | Khayat | 2024 | Yes | Yes | Yes | Yes | Yes | Unclear | Yes | Yes |
| 2 | Anwer | 2024 | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Unclear |
| 3 | Hyung | 2023 | Yes | No | Yes | Yes | No | Unclear | Yes | Yes |
| 4 | Al-Alousi | 2022 | Yes | Yes | Yes | Yes | No | Yes | Yes | No |
| 5 | Widodo | 2022 | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| 6 | Gupta | 2022 | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| 7 | Aljuboori | 2022 | Yes | Yes | Yes | Yes | Yes | No | Yes | Yes |
| 8 | Yoneoka | 2020 | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| 9 | Prasetyo | 2020 | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| 10 | Asadullah | 2020 | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| 11 | Aydin | 2019 | Yes | No | Yes | Yes | Unclear | Yes | Yes | No |
| 12 | Lan | 2018 | Yes | Unclear | Yes | Yes | Yes | Yes | Yes | Unclear |
| 13 | Zhang | 2017 | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| 14 | Li | 2017 | Yes | No | Yes | Yes | Yes | Yes | Yes | Yes |
| 15 | Chowdhury | 2016 | Yes | Yes | Yes | Yes | Yes | Yes | Yes | No |
| 16 | Tewari | 2015 | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Unclear |
| 17 | Sweeney | 2011 | Yes | No | Yes | Yes | Yes | Yes | Yes | Yes |
| Variable | n (%) | |||
|---|---|---|---|---|
| Total, n = 41 | Transorbital, n = 29 | Transmental, n = 7 | Transnasal, n = 5 | |
| Age (years) | 37.4 ± 13.1 | 37.5 ± 12.5 | 34.4 ± 15.5 | 41.0 ± 14.7 |
| Gender | ||||
| Male | 38 (92.7%) | 27 (93.1%) | 7 (100.0%) | 4 (80.0%) |
| Female | 3 (7.3%) | 2 (6.9%) | 0 (0.0%) | 1 (20.0%) |
| Mechanism of injury | ||||
| Accident | 28 (68.3%) | 22 (75.9%) | 1 (14.3%) | 5 (100.0%) |
| Violence | 7 (17.1%) | 7 (24.1%) | 0 (0.0%) | 0 (0.0%) |
| Suicide attempt | 6 (14.6%) | 0 (0.0%) | 6 (85.7%) | 0 (0.0%) |
| Neurological function on admission | ||||
| Intact | 30 (73.2%) | 20 (69.0%) | 7 (85.7%) | 4 (80.0%) |
| Impaired | 11 (26.8%) | 9 (31.0%) | 1 (14.3%) | 1 (20.0%) |
| GCS on admission (reported data) | n = 37 | n = 26 | n = 6 | n = 5 |
| 15 | 20 (54.1%) | 10 (38.5%) | 6 (100.0%) | 4 (80.0%) |
| Below 15 | 17 (45.9%) | 16 (61.5%) | 0 (0.0%) | 1 (20.0%) |
| Variable | n (%) | |||
|---|---|---|---|---|
| Total, n = 41 | Transorbital, n = 29 | Transmental, n = 7 | Transnasal, n = 5 | |
| Imaging | ||||
| Plain radiographs | 6 (14.6%) | 4 (13.8%) | 0 (0.0%) | 2 (40.0%) |
| CT | 40 (97.6%) | 28 (96.6%) | 7 (100.0%) | 5 (100.0%) |
| MRI | 18 (43.9%) | 16 (55.2%) | 1 (14.3%) | 1 (20.0%) |
| DSA | 5 (12.2%) | 2 (6.9%) | 3 (42.8%) | 0 (0.0%) |
| CTA | 11 (26.8%) | 5 (17.2%) | 6 (85.7%) | 0 (0.0%) |
| Type of treatment | ||||
| Operative | 37 (90.2%) | 26 (89.7%) | 7 (100.0%) | 4 (80.0%) |
| Non-operative | 4 (9.8%) | 3 (10.3%) | 0 (0.0%) | 1 (20.0%) |
| Antimicrobial prophylaxis | 33 (80.5%) | 27 (93.1%) | 1 (14.3%) | 5 (100.0%) |
| Operative field irrigation with antibiotics/antiseptics | 2 (4.9%) | 1 (3.4%) | 1 (14.3%) | 0 (0.0%) |
| Antiseizure prophylaxis (reported data) | n = 7 | n = 5 | n = 1 | n = 1 |
| Phenytoin | 2 (28.6%) | 2 (40.0%) | 0 (0.0%) | 0 (0.0%) |
| Sodium valproate | 2 (28.6%) | 1 (20.0%) | 1 (100.0%) | 0 (0.0%) |
| Not specified | 3 (42.8%) | 2 (40.0%) | 0 (0.0%) | 1 (100.0%) |
| Outcome at last follow-up (reported data) | n = 38 | n = 29 | n = 5 | n = 4 |
| Neurologically intact | 20 (52.6%) | 14 (48.3%) | 4 (80.0%) | 2 (50.0%) |
| Persisted deficit | 18 (47.4%) | 15 (51.7%) | 1 (20.0%) | 2 (50.0%) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Czyżewski, W.; Szymoniuk, M.; Litak, J.; Kura, K.; Kuś-Budzyńska, K.; Dryla, A.; Baj, J.; Torres, K.; Staśkiewicz, G. Management and Outcomes of Non-Missile Penetrating Brain Injury Involving the Anterior Skull Base: A Case Report and Systematic Review. J. Clin. Med. 2025, 14, 5731. https://doi.org/10.3390/jcm14165731
Czyżewski W, Szymoniuk M, Litak J, Kura K, Kuś-Budzyńska K, Dryla A, Baj J, Torres K, Staśkiewicz G. Management and Outcomes of Non-Missile Penetrating Brain Injury Involving the Anterior Skull Base: A Case Report and Systematic Review. Journal of Clinical Medicine. 2025; 14(16):5731. https://doi.org/10.3390/jcm14165731
Chicago/Turabian StyleCzyżewski, Wojciech, Michał Szymoniuk, Jakub Litak, Krzysztof Kura, Klaudia Kuś-Budzyńska, Aleksandra Dryla, Jacek Baj, Kamil Torres, and Grzegorz Staśkiewicz. 2025. "Management and Outcomes of Non-Missile Penetrating Brain Injury Involving the Anterior Skull Base: A Case Report and Systematic Review" Journal of Clinical Medicine 14, no. 16: 5731. https://doi.org/10.3390/jcm14165731
APA StyleCzyżewski, W., Szymoniuk, M., Litak, J., Kura, K., Kuś-Budzyńska, K., Dryla, A., Baj, J., Torres, K., & Staśkiewicz, G. (2025). Management and Outcomes of Non-Missile Penetrating Brain Injury Involving the Anterior Skull Base: A Case Report and Systematic Review. Journal of Clinical Medicine, 14(16), 5731. https://doi.org/10.3390/jcm14165731







