Sex Differences in 24 H Blood Pressure in Night-Shift Workers
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design
2.2. Peripheral Blood Mononuclear Cell Isolation and Clock Gene Expression Analyses
2.3. Statistical Analyses
3. Results
3.1. Characteristics of the Study Population
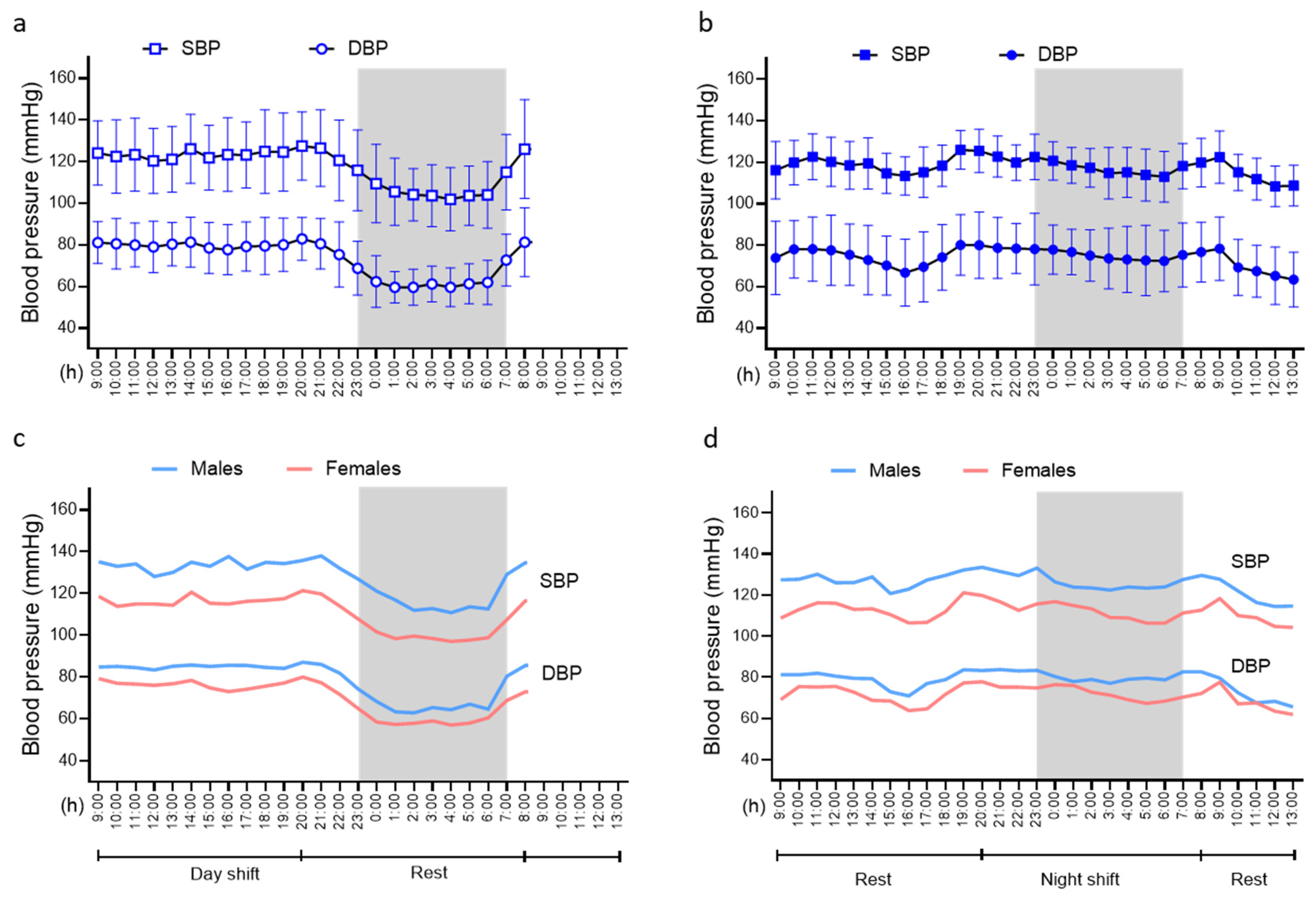
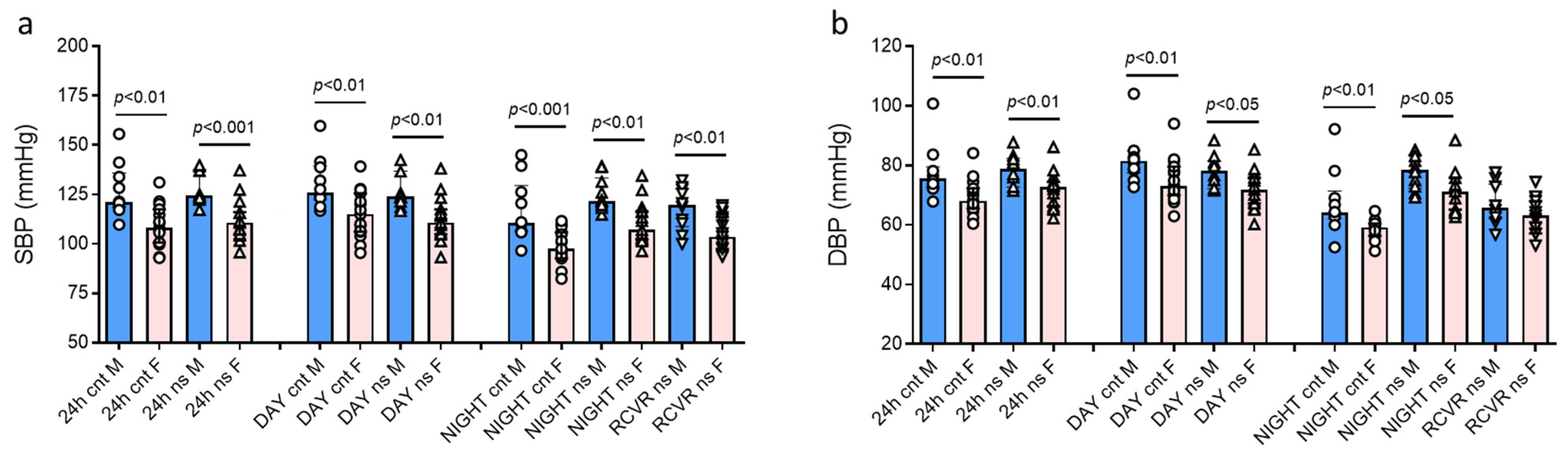
3.2. Blood Pressure Patterns and Levels in the Whole Study Population and According to Sex
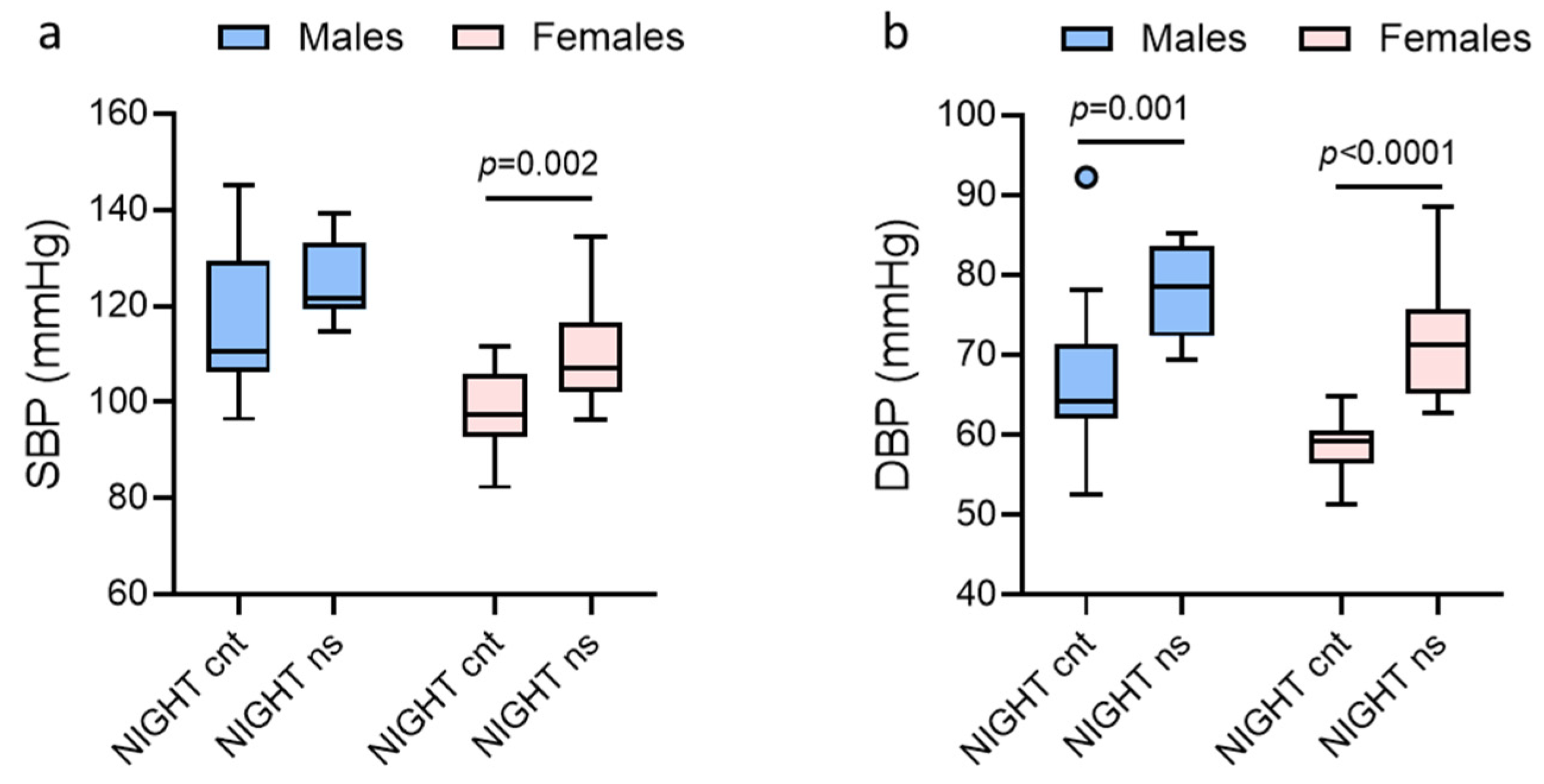
3.3. Paired Analysis of Blood Pressure at Night (Rest vs. Work) in Males and Females
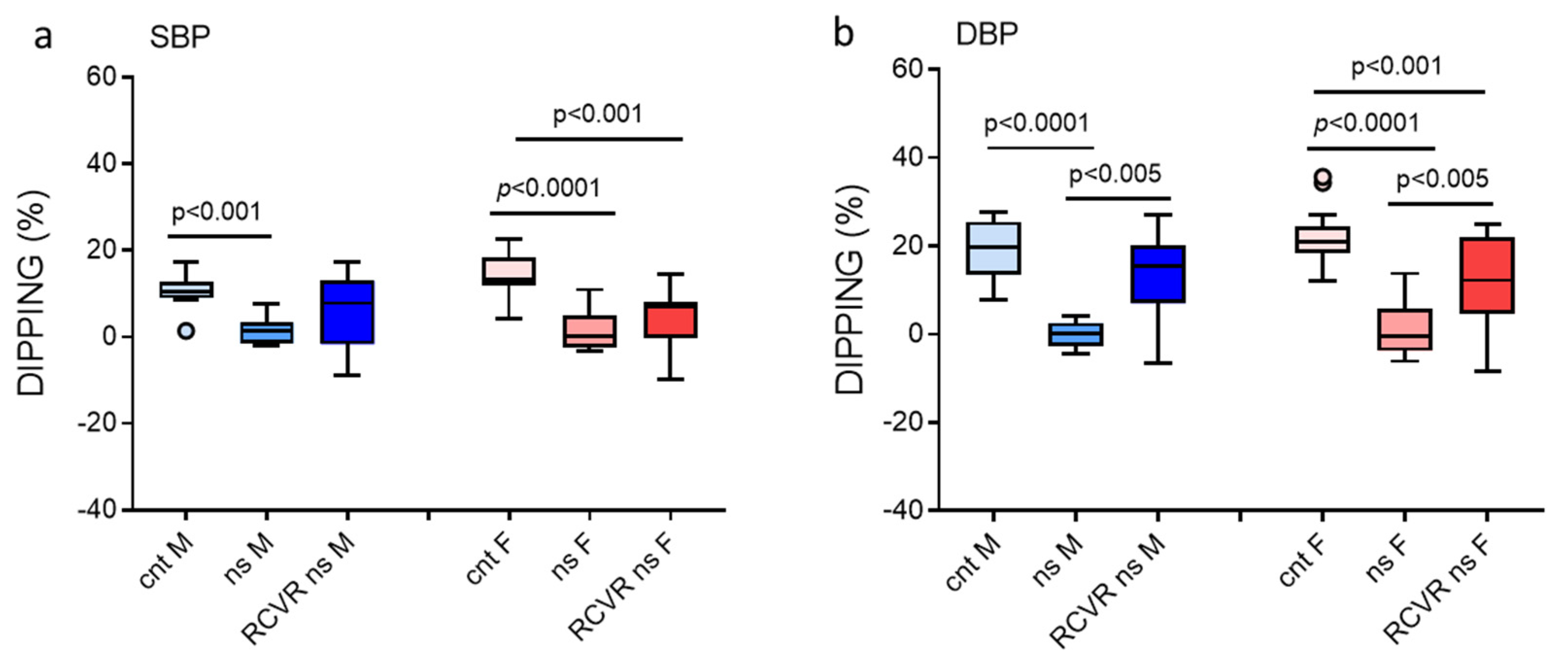
3.4. Blood Pressure Dippings in Males and Females
3.5. Circadian Rhythm Gene Expression in Males and Females
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Mauvais-Jarvis, F.; Bairey Merz, N.; Barnes, P.J.; Brinton, R.D.; Carrero, J.J.; DeMeo, D.L.; De Vries, G.J.; Epperson, C.N.; Govindan, R.; Klein, S.L.; et al. Sex and gender: Modifiers of health, disease, and medicine. Lancet 2020, 396, 565–582. [Google Scholar] [CrossRef]
- Shannon, G.; Jansen, M.; Williams, K.; Caceres, C.; Motta, A.; Odhiambo, A.; Eleveld, A.; Mannell, J. Gender equality in science, medicine, and global health: Where are we at and why does it matter? Lancet 2019, 393, 560–569. [Google Scholar] [CrossRef] [PubMed]
- Collaboration, N.C.D.R.F. Worldwide trends in hypertension prevalence and progress in treatment and control from 1990 to 2019: A pooled analysis of 1201 population-representative studies with 104 million participants. Lancet 2021, 398, 957–980. [Google Scholar] [CrossRef] [PubMed]
- Gerdts, E.; Sudano, I.; Brouwers, S.; Borghi, C.; Bruno, R.M.; Ceconi, C.; Cornelissen, V.; Dievart, F.; Ferrini, M.; Kahan, T.; et al. Sex differences in arterial hypertension. Eur. Heart J. 2022, 43, 4777–4788. [Google Scholar] [CrossRef]
- Ji, H.; Kim, A.; Ebinger, J.E.; Niiranen, T.J.; Claggett, B.L.; Bairey Merz, C.N.; Cheng, S. Sex Differences in Blood Pressure Trajectories Over the Life Course. JAMA Cardiol. 2020, 5, 19–26. [Google Scholar] [CrossRef]
- Ji, H.; Niiranen, T.J.; Rader, F.; Henglin, M.; Kim, A.; Ebinger, J.E.; Claggett, B.; Merz, C.N.B.; Cheng, S. Sex Differences in Blood Pressure Associations With Cardiovascular Outcomes. Circulation 2021, 143, 761–763. [Google Scholar] [CrossRef]
- Bidel, Z.; Nazarzadeh, M.; Canoy, D.; Copland, E.; Gerdts, E.; Woodward, M.; Gupta, A.K.; Reid, C.M.; Cushman, W.C.; Wachtell, K.; et al. Sex-Specific Effects of Blood Pressure Lowering Pharmacotherapy for the Prevention of Cardiovascular Disease: An Individual Participant-Level Data Meta-Analysis. Hypertension 2023, 80, 2293–2302. [Google Scholar] [CrossRef]
- Olivieri, O.; Pizzolo, F.; Ciacciarelli, A.; Corrocher, R.; Signorelli, D.; Falcone, S.; Blengio, G.S. Menopause not aldosterone-to-renin ratio predicts blood pressure response to a mineralocorticoid receptor antagonist in primary care hypertensive patients. Am. J. Hypertens. 2008, 21, 976–982. [Google Scholar] [CrossRef]
- Bager, J.E.; Manhem, K.; Andersson, T.; Hjerpe, P.; Bengtsson-Bostrom, K.; Ljungman, C.; Mourtzinis, G. Hypertension: Sex-related differences in drug treatment, prevalence and blood pressure control in primary care. J. Hum. Hypertens. 2023, 37, 662–670. [Google Scholar] [CrossRef]
- Lazaridis, A.; Malliora, A.; Gkaliagkousi, E. The Particularities of Arterial Hypertension in Female Sex: From Pathophysiology to Therapeutic Management. J. Clin. Med. 2025, 14, 3137. [Google Scholar] [CrossRef] [PubMed]
- Omboni, S.; Khan, N.A.; Kunadian, V.; Olszanecka, A.; Schutte, A.E.; Mihailidou, A.S. Sex Differences in Ambulatory Blood Pressure Levels and Subtypes in a Large Italian Community Cohort. Hypertension 2023, 80, 1417–1426. [Google Scholar] [CrossRef] [PubMed]
- Toffoli, B.; Tonon, F.; Giudici, F.; Ferretti, T.; Ghirigato, E.; Contessa, M.; Francica, M.; Candido, R.; Puato, M.; Grillo, A.; et al. Preliminary Study on the Effect of a Night Shift on Blood Pressure and Clock Gene Expression. Int. J. Mol. Sci. 2023, 24, 9309. [Google Scholar] [CrossRef] [PubMed]
- Manohar, S.; Thongprayoon, C.; Cheungpasitporn, W.; Mao, M.A.; Herrmann, S.M. Associations of rotational shift work and night shift status with hypertension: A systematic review and meta-analysis. J. Hypertens. 2017, 35, 1929–1937. [Google Scholar] [CrossRef]
- Costello, H.M.; Gumz, M.L. Circadian Rhythm, Clock Genes, and Hypertension: Recent Advances in Hypertension. Hypertension 2021, 78, 1185–1196. [Google Scholar] [CrossRef]
- Tonon, F.; Tornese, G.; Giudici, F.; Nicolardi, F.; Toffoli, B.; Barbi, E.; Fabris, B.; Bernardi, S. Children With Short Stature Display Reduced ACE2 Expression in Peripheral Blood Mononuclear Cells. Front. Endocrinol. 2022, 13, 912064. [Google Scholar] [CrossRef]
- Wang, T.L.; Bryan, S.G.; Jeyabalan, A.; Facco, F.L.; Gandley, R.E.; Hubel, C.A.; Catov, J.M.; Hauspurg, A.K. Sleep Quality in Individuals with and without Persistent Postpartum Hypertension. Am. J. Perinatol. 2024, 41, 1113–1119. [Google Scholar] [CrossRef]
- Huart, J.; Persu, A.; Lengele, J.P.; Krzesinski, J.M.; Jouret, F.; Stergiou, G.S. Pathophysiology of the Nondipping Blood Pressure Pattern. Hypertension 2023, 80, 719–729. [Google Scholar] [CrossRef] [PubMed]
- Ohkubo, T.; Imai, Y.; Tsuji, I.; Nagai, K.; Watanabe, N.; Minami, N.; Kato, J.; Kikuchi, N.; Nishiyama, A.; Aihara, A.; et al. Relation between nocturnal decline in blood pressure and mortality. The Ohasama Study. Am. J. Hypertens. 1997, 10, 1201–1207. [Google Scholar] [CrossRef]
- Huang, R.C. The discoveries of molecular mechanisms for the circadian rhythm: The 2017 Nobel Prize in Physiology or Medicine. Biomed. J. 2018, 41, 5–8. [Google Scholar] [CrossRef]
- Cox, K.H.; Takahashi, J.S. Circadian clock genes and the transcriptional architecture of the clock mechanism. J. Mol. Endocrinol. 2019, 63, R93–R102. [Google Scholar] [CrossRef]
- Burt, V.L.; Whelton, P.; Roccella, E.J.; Brown, C.; Cutler, J.A.; Higgins, M.; Horan, M.J.; Labarthe, D. Prevalence of hypertension in the US adult population. Results from the Third National Health and Nutrition Examination Survey, 1988-1991. Hypertension 1995, 25, 305–313. [Google Scholar] [CrossRef]
- Benjamin, E.J.; Blaha, M.J.; Chiuve, S.E.; Cushman, M.; Das, S.R.; Deo, R.; de Ferranti, S.D.; Floyd, J.; Fornage, M.; Gillespie, C.; et al. Heart Disease and Stroke Statistics-2017 Update: A Report From the American Heart Association. Circulation 2017, 135, e146–e603. [Google Scholar] [CrossRef]
- Colafella, K.M.M.; Denton, K.M. Sex-specific differences in hypertension and associated cardiovascular disease. Nat. Rev. Nephrol. 2018, 14, 185–201. [Google Scholar] [CrossRef]
- Hernandez, I.; Delgado, J.L.; Diaz, J.; Quesada, T.; Teruel, M.J.; Llanos, M.C.; Carbonell, L.F. 17beta-estradiol prevents oxidative stress and decreases blood pressure in ovariectomized rats. Am. J. Physiol. Regul. Integr. Comp. Physiol. 2000, 279, R1599–R1605. [Google Scholar] [CrossRef]
- Zhu, D.; Chung, H.F.; Dobson, A.J.; Pandeya, N.; Giles, G.G.; Bruinsma, F.; Brunner, E.J.; Kuh, D.; Hardy, R.; Avis, N.E.; et al. Age at natural menopause and risk of incident cardiovascular disease: A pooled analysis of individual patient data. Lancet Public Health 2019, 4, e553–e564. [Google Scholar] [CrossRef]
- Tikellis, C.; Bernardi, S.; Burns, W.C. Angiotensin-converting enzyme 2 is a key modulator of the renin-angiotensin system in cardiovascular and renal disease. Curr. Opin. Nephrol. Hypertens. 2011, 20, 62–68. [Google Scholar] [CrossRef]
- Fabris, B.; Candido, R.; Bortoletto, M.; Toffoli, B.; Bernardi, S.; Stebel, M.; Bardelli, M.; Zentilin, L.; Giacca, M.; Carretta, R. Stimulation of cardiac apoptosis in ovariectomized hypertensive rats: Potential role of the renin-angiotensin system. J. Hypertens. 2011, 29, 273–281. [Google Scholar] [CrossRef]
- Tonon, F.; Candido, R.; Toffoli, B.; Tommasi, E.; Cortello, T.; Fabris, B.; Bernardi, S. Type 1 diabetes is associated with significant changes of ACE and ACE2 expression in peripheral blood mononuclear cells. Nutr. Metab. Cardiovasc. Dis. 2022, 32, 1275–1282. [Google Scholar] [CrossRef] [PubMed]
- Saksvik, I.B.; Bjorvatn, B.; Hetland, H.; Sandal, G.M.; Pallesen, S. Individual differences in tolerance to shift work--a systematic review. Sleep. Med. Rev. 2011, 15, 221–235. [Google Scholar] [CrossRef] [PubMed]
- Marquie, J.C.; Foret, J. Sleep, age, and shiftwork experience. J. Sleep. Res. 1999, 8, 297–304. [Google Scholar] [CrossRef] [PubMed]
- Rotenberg, L.; Portela, L.; Marcondes, W.B.; Moreno, C.; Nasciemento, C.P. Gender and diurnal sleep in night workers at Brazilian industry . Shift Work 21st Century Arb. Der Betrieblichen Prax. 2000, 305–309. [Google Scholar]
- Costello, H.M.; Eikenberry, S.A.; Cheng, K.Y.; Broderick, B.; Joshi, A.S.; Scott, G.R.; McKee, A.; Mendez, V.M.; Douma, L.G.; Crislip, G.R.; et al. Sex differences in the adrenal circadian clock: A role for BMAL1 in the regulation of urinary aldosterone excretion and renal electrolyte balance in mice. Am. J. Physiol. Ren. Physiol. 2025, 328, F1–F14. [Google Scholar] [CrossRef] [PubMed]
- Randler, C.; Engelke, J. Gender differences in chronotype diminish with age: A meta-analysis based on morningness/chronotype questionnaires. Chronobiol. Int. 2019, 36, 888–905. [Google Scholar] [CrossRef] [PubMed]
- Shim, J.; Fleisch, E.; Barata, F. Circadian rhythm analysis using wearable-based accelerometry as a digital biomarker of aging and healthspan. NPJ Digit. Med. 2024, 7, 146. [Google Scholar] [CrossRef] [PubMed]
- Vestergaard, J.M.; Dalboge, A.; Bonde, J.P.E.; Garde, A.H.; Hansen, J.; Hansen, A.M.; Larsen, A.D.; Harma, M.; Costello, S.; Bottcher, M.; et al. Night shift work characteristics and risk of incident coronary heart disease among health care workers: National cohort study. Int. J. Epidemiol. 2023, 52, 1853–1861. [Google Scholar] [CrossRef]
- Canto, J.G.; Rogers, W.J.; Goldberg, R.J.; Peterson, E.D.; Wenger, N.K.; Vaccarino, V.; Kiefe, C.I.; Frederick, P.D.; Sopko, G.; Zheng, Z.J.; et al. Association of age and sex with myocardial infarction symptom presentation and in-hospital mortality. JAMA 2012, 307, 813–822. [Google Scholar] [CrossRef]
- Wang, N.; Sun, Y.; Zhang, H.; Wang, B.; Chen, C.; Wang, Y.; Chen, J.; Tan, X.; Zhang, J.; Xia, F.; et al. Long-term night shift work is associated with the risk of atrial fibrillation and coronary heart disease. Eur. Heart J. 2021, 42, 4180–4188. [Google Scholar] [CrossRef]

| Target (GenBank Accession Number) | Primer Pair | Mature Transcript | Amplicon Size (bp) |
|---|---|---|---|
| BMAL1 (NM_001297719) | (F) 5′-TTACTGTGCTAAGGATGGCTG-3′ (R) 5′-GCCCTGAGAATGAGGTGTTTC-3′ | (F) 731–751 (R) 857–837 | 127 |
| CLOCK (NM_004898) | (F) 5′-CTACATTCACTCAGGACAGGC-3′ (R) 5′-GGCCCATAAGCATAGTACTAGG-3′ | (F) 2495–2515 (R) 2614–2593 | 120 |
| PER1 (NM_002616) | (F) 5′-CCTCCAGTGATAGCAACGG-3′ (R) 5′-ACCAGATGCACATCCTTACAG-3′ | (F) 1784–1802 (R) 1874–1854 | 91 |
| PER2 (NM_022817) | (F) 5′-GCCAGAGTCCAGATACCTTTAG-3′ (R) 5′-TGTGTCCACTTTCGAAGACTG-3′ | (F) 505–526 (R) 602–582 | 98 |
| PER3 (NM_001377275) | (F) 5′-CTGTCTCACTGTGGTTGAAAAG-3′ (R) 5′-TAGGTAACCCAGCAAAGGC-3′ | (F) 1063–1084 (R) 1207–1189 | 145 |
| CRY1 (NM_004075) | (F) 5′-TCCCGTCTGTTTGTGATTCG-3′ (R) 5′-TTAATAGCTGCGTCTCGTTCC-3′ | (F) 799–818 (R) 929–909 | 131 |
| CRY2 (NM_021117) | (F) 5′-TGGATAAGCACTTGGAACGG-3′ (R) 5′-AGAGACAACCAAAGCGCAG-3′ | (F) 735–754 (R) 854–836 | 120 |
| Variable | Entire Cohort (n = 25) | Males (n = 10) | Females (n = 15) | p Value | |
|---|---|---|---|---|---|
| Age | 33 (29–37) | 33 (31–36) | 31 (29–37) | 0.867 | |
| BMI | 22.6 (20.8–24.5) | 24.6 (22.0–26.9) | 22.1 (20.3–23.0) | 0.037 | |
| Physical activity | Yes (%) No (%) | 12 (48%) 13 (52%) | 3 (30%) 7 (70%) | 9 (60%) 6 (40%) | 0.226 |
| Medical conditions | Yes (%) No (%) | 3 (12%) 22 (88%) | 2 (20%) 8 (80%) | 1 (7%) 14 (93%) | 0.543 |
| Medication | Yes (%) No (%) | 5 (20%) 20 (80%) | 2 (20%) 8 (80%) | 3 (20%) 12 (80%) | 1 |
| Years of work | 7 (2–10) | 7 (5–9) | 4 (2–11) | 0.636 | |
| Working position | Attending (%) Resident (%) | 13 (52%) 12 (48%) | 4 (40%) 6 (60%) | 9 (60%) 6 (40%) | 0.428 |
| Day shift steps | 7720 (6504–11,062) | 6940 (5881–12,191) | 8000 (6944–10,307) | 0.591 | |
| Night shift/month | 1.2 (1–2) | 1.2 (1–2) | 1.2 (1–2) | 1 | |
| Night-shift calls | 17.5 (13–20) | 18 (11.5–20) | 17.5 (15–19) | 0.893 | |
| Night-shift admissions | 8.5 (6–10) | 8 (6–9) | 9 (6.5–10) | 0.567 | |
| Night-shift steps | 6660 (5785–7822) | 7414 (6521–8291) | 6436 (5603–7369) | 0.209 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Toffoli, B.; Berti, S.; Pitteri, I.; Contessa, M.; Tonon, F.; Defendi, R.; Grillo, A.; Fabris, B.; Bernardi, S. Sex Differences in 24 H Blood Pressure in Night-Shift Workers. J. Clin. Med. 2025, 14, 5728. https://doi.org/10.3390/jcm14165728
Toffoli B, Berti S, Pitteri I, Contessa M, Tonon F, Defendi R, Grillo A, Fabris B, Bernardi S. Sex Differences in 24 H Blood Pressure in Night-Shift Workers. Journal of Clinical Medicine. 2025; 14(16):5728. https://doi.org/10.3390/jcm14165728
Chicago/Turabian StyleToffoli, Barbara, Silvia Berti, Ilaria Pitteri, Matilde Contessa, Federica Tonon, Rebecca Defendi, Andrea Grillo, Bruno Fabris, and Stella Bernardi. 2025. "Sex Differences in 24 H Blood Pressure in Night-Shift Workers" Journal of Clinical Medicine 14, no. 16: 5728. https://doi.org/10.3390/jcm14165728
APA StyleToffoli, B., Berti, S., Pitteri, I., Contessa, M., Tonon, F., Defendi, R., Grillo, A., Fabris, B., & Bernardi, S. (2025). Sex Differences in 24 H Blood Pressure in Night-Shift Workers. Journal of Clinical Medicine, 14(16), 5728. https://doi.org/10.3390/jcm14165728








