Abstract
Aim: This study was conducted to determine the feasibility, safety, and clinical outcomes of the vaginal natural-orifice transluminal endoscopic surgery (vNOTES) approach in gynecology for obese patients. Methods: PubMed, Cochrane Library, and Google Scholar were searched, from inception to April 2025. A systematic review was performed following the PRISMA guidelines. Studies assessing the use of vNOTES for gynecological procedures in obese women were included. The quality of included articles was evaluated according to the Newcastle–Ottawa Scale. Results: The search yielded three retrospective cohort studies, one cross-sectional, and ten case series. The patients in the vNOTES group (n = 99) had statistically significant shorter operative times, reduced hospitalization, lower postoperative pain scores, fewer perioperative complications, and improved quality of life when compared to the laparoscopy group (n = 84). A study compared obese women to non-obese women undergoing vNOTES and found that operative times were longer in the obese group. Conversion to laparoscopy or laparotomy occurred in fewer than 5% of cases, and intraoperative and postoperative complication rates were low across all studies. Conclusions: vNOTES appears to be safe and potentially superior to other minimally invasive techniques. The small sample size of the case series and the lack of a sufficient number of comparative studies limit the strength of the conclusions.
1. Introduction
Gynecology encompasses a wide range of benign and malignant surgical conditions, which may present on either an emergency or elective basis. Access to the peritoneal cavity can be established via laparotomy, vaginal approach, conventional laparoscopy, and robotic-assisted techniques [1,2]. In contemporary clinical practice, the primary objective is to minimize perioperative morbidity and complication rates while optimizing cosmetic outcomes through minimally invasive methods.
The transvaginal approach offers several benefits comparable to conventional laparoscopy, such as shorter hospital stays, faster recovery, and reduced postoperative pain, while avoiding any abdominal incisions [1,3]. However, it manifests certain limitations compared to laparoscopic access, particularly regarding the extent of peritoneal cavity exploration [3]. Moreover, its feasibility is reduced in patients without pelvic organ prolapse or with significantly enlarged uteri. To combine the advantages of both vaginal and laparoscopic approaches, the vaginal natural-orifice transluminal endoscopy surgery (vNOTES) technique was developed [4]. vNOTES is a hybrid approach that allows access to the peritoneal cavity via a small posterior colpotomy through the vagina, a natural orifice, after which a multi-channel single-port device is introduced and a pneumoperitoneum is established. The procedure is then performed using standard laparoscopic instruments [5,6,7]. This approach combines all the well-documented benefits of minimally invasive surgery with the scarless advantage of a purely transvaginal entry [5].
Obesity, defined as a body mass index (BMI) greater than or equal to 30, according to the World Health Organization (WHO) affected one in eight individuals globally in 2022 [8]. It is a chronic disease with widespread systemic implications. In particular, in women, obesity is associated with infertility, abnormal uterine bleeding, endometrial hyperplasia, and increased endometrial cancer risk [9]. Obesity also significantly elevates the risk of perioperative complications, including vascular injury, hemorrhage, venous thromboembolism, and wound infections [10,11]. In laparoscopic surgery, the increased abdominal-wall thickness may impede the insertion and maneuverability of trocars and instruments, thereby prolonging operative time. When combined with the Trendelenburg position, this may contribute to substantial respiratory compromise [12].
The increasing prevalence of obesity and the perioperative challenges highlight the need for innovative, minimally invasive surgical techniques. This literature review aims to evaluate the role of the vNOTES approach in the management of gynecological surgical conditions in obese patients.
2. Methods
2.1. Protocol Registration
This review has been registered in PROSPERO, a database for prospectively registered systematic reviews. The registration number for this review is CRD420251055312.
2.2. Search Strategy
Two independent reviewers (AMK, CV) conducted a literature review using the Cochrane Central Register of Controlled Trials (CENTRAL), PubMed, and Google Scholar, covering the period from inception to April 2025. The search included Medical Subject Headings (MeSH) terms and the combination of the following terms: vaginal natural-orifice transluminal endoscopic surgery, obesity, overweight, and gynecology. The search was performed without using any filters.
2.3. Eligibility Criteria
Studies evaluating vNOTES for gynecological procedures in obese patients were reviewed based on their titles, abstracts, and full texts. Additionally, the references of all studies were examined for further citations.
Two reviewers (AMK, CV) independently assessed all articles to determine their eligibility for inclusion in the review process. This study focused on both retrospective and prospective observational studies. We excluded articles featuring non-gynecological procedures, reviews, Chinese-language manuscripts, and in vitro investigations.
This study follows the Preferred Reporting Items for Systematic Reviews and Meta-Analysis (PRISMA) guidelines [13]. Table S1a,b in the Supplementary Materials presents the comprehensive PRISMA 2020 Checklist.
2.4. Quality Assessment of the Included Studies
The Newcastle–Ottawa Scale (NOS) was used for the quality assessment of observational studies (case–control and cohort studies). A NOS score of 7 or higher indicated a low risk of bias. A score between 4 and 6 indicated a high risk of bias, whereas a score of 3 or lower indicated a very high risk of bias [14]. Disagreements regarding quality assessment were resolved through discussion with a third reviewer.
2.5. Data Extraction
Two authors (AMK, CV) independently extracted details, including the year of publication, hospital setting, study methodology, sample size, type of intervention, demographic characteristics, comorbidities, and outcomes. This study presents findings derived from both univariate and multivariate analyses.
3. Results
The relationship between the vNOTES approach in gynecological procedures and obesity was evaluated in four observational studies after a comprehensive literature review [15,16,17,18]. In addition, 10 case series provided further qualitative information about the clinical features of this condition [19,20,21,22,23,24,25,26,27,28]. Figure 1 presents the PRISMA flow diagram of the process of identification, screening, and selection of articles for inclusion in this analysis.
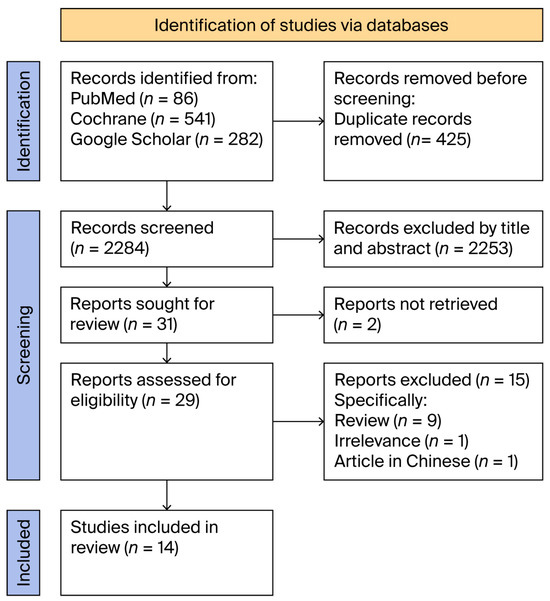
Figure 1.
Flow diagram of identification, screening, and inclusion of relevant studies.
3.1. Case Series
Table 1 presents data regarding ten case series with 324 obese patients who underwent vNOTES gynecological procedures. These studies were conducted in tertiary-care hospitals in Turkey, Belgium, Spain, Russia, Singapore, Australia, and Switzerland between 2017 and 2024. The patient demographics varied, with BMI ranging from 28.5 to 60 kg/m2 and mean ages between 36.2 and 74.5 years. The most common procedure performed was the vNOTES hysterectomy, often combined with bilateral salpingo-oophorectomy, primarily for treating early-stage endometrial cancer, endometrial hyperplasia, postmenopausal bleeding, or benign uterine conditions. The operative time ranged from 82 to 233 min, with fewer than 5% of patients requiring conversion to laparoscopy or laparotomy. Hemoglobin loss ranged from 0.3 to 2.4 g/dL, and the hospital stay was typically short, with most patients discharged within one to two days. Postoperative pain was minimal, with visual analog scale (VAS) scores ranging from 1.0 to 3.5 within 6 to 48 h. Intraoperative and postoperative complications were low across all studies, with notable events including bladder injury, ovarian vessel bleeding, and seroma formation.

Table 1.
Characteristics of the observational studies assessing vaginal natural-orifice transluminal endoscopic surgery (vNOTES) for gynecological procedures in obese patients.
3.2. Comparative Studies
Table 2 presents four comparative observational studies conducted between 2017 and 2024 in tertiary-care hospitals in China, France, and Turkey. Among these studies, three studies were designed as retrospective cohorts, while one was cross-sectional. A total of 99 obese patients who underwent vaginal natural-orifice transluminal endoscopic surgery (vNOTES) and 84 control patients who underwent multi-port laparoscopic surgery (MPLS) or total laparoscopic hysterectomy (TLH) were included in the analysis. Across all studies, vNOTES was associated with statistically significant shorter operative times and shorter hospital stays. Additionally, patients who underwent vNOTES experienced statistically significant lower postoperative pain scores at both 6 and 24 h. This group also demonstrated fewer perioperative complications and reported improved quality-of-life scores. Conversion to conventional laparoscopy was required in selected cases due to intraoperative difficulties or anatomical limitations. The number of conversions per study is summarized in Table 2, and the specific reasons are detailed in the corresponding footnotes. Notably, the demographic characteristics of patients in both groups did not show significant differences.

Table 2.
Characteristics of the case series assessing vaginal natural-orifice transluminal endoscopic surgery (vNOTES) for gynecological procedures in obese patients.
Bouchez et al. (2023) retrospectively compared 54 obese to 146 non-obese patients who had undergone vNOTES hysterectomy [16]. The results revealed that the obese patients had statistically significant longer operative times (p < 0.001) than the control group. Table 3 summarizes the risk-of-bias assessment for the included studies; one study was classified as low-risk (NOS score ≥ 7), while the remaining three were considered high-risk (NOS score < 7).

Table 3.
Quality assessment of observational studies assessing vaginal natural-orifice transluminal endoscopic surgery (vNOTES) for gynecological procedures in obese patients, according to the Newcastle–Ottawa Scale (NOS).
4. Discussion
In the present study, the aim was to evaluate the role of vNOTES in gynecologic procedures among obese patients through a comprehensive review of the current literature. A total of 14 studies comprising 477 patients who underwent vNOTES for either benign or malignant indications were included. The most commonly performed operation was vNOTES hysterectomy, frequently in combination with bilateral saplingo-oophorectomy. The technique was associated with low rates of intraoperative and postoperative complications and demonstrated statistically significant improvements in perioperative outcomes compared to traditional laparoscopic approaches.
Several studies have investigated the potential benefits of the vNOTES approach compared to alternative surgical techniques across all BMI categories. In a randomized controlled trial (RCT), Baekelandt et al. documented significantly shorter operative time, reduced hospital stays, and lower postoperative pain levels in the vNOTES hysterectomy group compared to the total laparoscopic hysterectomy (TLH) group [7]. Similarly, Kaya et al. reported comparable findings, although no statistically significant difference was observed between the two groups in terms of postoperative visual analog scale (VAS) scores [15]. Additionally, Nef et al. confirmed the safety and feasibility of the procedure in elderly patients, a distinct subgroup characterized by a high prevalence of comorbidities [29]. Finally, three systematic reviews concluded that while both vNOTES hysterectomy and TLH are equally effective for benign indications, vNOTES is associated with shorter operative time, decreased length of hospital stay, and lower intraoperative blood loss [30,31,32].
Favorable outcomes associated with its application have positioned vNOTES as a valuable addition to the surgical field. Two separate meta-analyses by Steinemann et al. and Yang et al. reported lower postoperative pain scores, reduced rates of surgical-site infections, improved cosmetic outcomes, and shorter operative time and hospital stay with vNOTES compared to conventional laparoscopic approaches [32,33]. As a novel minimally invasive technique, vNOTES has attracted the interest of gynecologic oncologists. In this context, Lee et al. conducted a pilot study involving three patients, demonstrating the safety and feasibility of vNOTES for staging surgery in early endometrial cancer [34]. However, one of the main challenges in performing lymphadenectomy via vNOTES, compared to laparoscopic or robotic surgery, was the limited visualization of the retroperitoneal area and the lack of appropriate instruments for exposure and hemostasis [35,36]. This obstacle was addressed by Baekelandt et al., who described a new retroperitoneal vNOTES technique enabling sentinel lymph-node resection, and by Huber et al., who conducted a preliminary study with seven patients, showing the feasibility and safety of the method [37,38]. According to Deng et al. and Baekelandt et al., the application of vNOTES for the treatment of stage I endometrial cancer and identification of the sentinel lymph node appeared to be both safe and effective [38,39].
This study illustrated that the adoption of the vNOTES approach in obese patients yielded comparable outcomes to those observed in non-obese women when compared to conventional laparoscopy. Kaya et al. reported that the shorter operative time associated with vNOTES may have been attributable to easier access to the uterine pedicles and improved uterine manipulation. Furthermore, in obese patients, the increased amount of internal adipose tissue can hinder colpotomy and its closure during TLH. In contrast, with vNOTES, these steps are performed similarly to in a conventional vaginal hysterectomy [4]. Burnett et al. highlighted the easier handling of instruments during vNOTES procedures, as these did not need to traverse significant thickness of subcutaneous fat in obese patients undergoing laparoscopy [20]. Additionally, the retroperitoneal vNOTES approach eliminated the need for a steep Trendelenburg position and allowed for the use of lower pneumoperitoneum pressures, offering significant advantages in minimizing respiratory compromise in this patient subgroup [19,39]. Kale et al. and Kaya et al., in their respective analyses, attributed the reduced postoperative pain and decreased analgesic requirements associated with vNOTES to its scarless nature and the absence of abdominal-wall trauma or nerve injury. Consequently, these factors may have contributed to earlier patient mobilization and faster postoperative recovery [4,6].
The application of vNOTES in low-resource settings offers benefits, including quicker recovery and shorter hospital stays, which are valuable where healthcare structures are limited. However, success depends on the availability of surgical expertise and appropriate equipment. Efforts to expand vNOTES access should focus on training models and protocols adjusted to local constraints. As mentioned by Baekelandt et al. (2021), structured training and standardization are essential to ensure the reproducibility, safety, and adoption of this technique [40].
In addition, comparison between v-NOTES and vaginal hysterectomy remains of clinical interest. A recent systematic review and meta-analysis evaluated use of these two techniques in the general population [41]. However, there is limited evidence regarding these methods in obese patients. Since this review focuses on the outcomes of v-NOTES in individuals with obesity, it does not address this comparison. Future studies specifically designed to evaluate these two approaches in obese populations could provide additional clinical insights.
Although this study did not specifically analyze the learning curve associated with v-NOTES, it remains an important consideration, since adopting a new technique typically requires a period of skill development. Unfortunately, the current literature does not provide sufficient data to assess the learning curve, particularly regarding comparisons of operative times, complication rates, and procedural consistency during various phases of adoption. Future research that includes these factors could yield valuable insights.
It is important to acknowledge several limitations. There was a notable risk of publication and selection bias because this analysis primarily consisted of case series with small sample sizes, and the number of comparative studies that included a control group was limited. Additionally, heterogeneity existed among study designs, patient demographics, and surgical indications, which may impact the generalizability of the findings. Future research should prioritize large multicenter controlled trials that compare vNOTES with conventional methods and assess long-term outcomes, including recovery time and quality of life. Moreover, evidence-based studies are needed to better understand patient-reported outcomes, cost-effectiveness, and the learning curve for operators.
5. Conclusions
vNOTES appeared to be a promising minimally invasive surgical technique, especially in obese patients. While early outcomes are encouraging, the current evidence is limited due to small and heterogeneous studies. Future research should focus on large multicenter studies to validate these findings and determine the role of vNOTES in clinical practice.
Supplementary Materials
The following supporting information can be downloaded at: https://www.mdpi.com/article/10.3390/jcm14165713/s1, Table S1: (a) Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) 2020 Checklist. (b) Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) 2020 Abstracts Checklist.
Author Contributions
Conceptualization, S.A., D.D. and A.-M.K.; Methodology, A.-M.K., C.V. (Christos Vrysis), and D.Z.; Validation, E.K., I.S. and C.V. (Charalampos Voros); Formal Analysis, D.Z., A.G. and C.D.; Investigation, E.K., A.G. and I.S.; Resources, C.V. (Charalampos Voros) and C.D.; Data Curation, C.V. (Christos Vrysis) and N.G.; Writing—Original Draft Preparation, A.-M.K. and C.V. (Christos Vrysis); Writing—Review and Editing, N.G., G.T. and S.K.; Visualization, G.T., S.K. and T.G.; Supervision, T.G., S.A. and D.D. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Data Availability Statement
The data used in this study are available upon request.
Conflicts of Interest
The authors declare no conflicts of interest.
Abbreviations
The following abbreviations are used in this manuscript:
| vNOTES | vaginal natural-orifice transluminal endoscopic surgery |
| PRISMA | Preferred Reporting Items for Systematic Review and Meta-analysis |
| NOS | Newcastle–Ottawa Scale |
| TLH | total laparoscopic hysterectomy |
| BMI | body mass index |
| VAS | visual analog scale |
| RCT | randomized controlled trial |
| WHO | World Health Organization |
| SD | standard deviation |
References
- Pickett, C.M.; Seeratan, D.D.; Mol, B.W.J.; Nieboer, T.E.; Johnson, N.; Bonestroo, T.; Aarts, J.W. Surgical approach to hysterectomy for benign gynaecological disease. Cochrane Database Syst. Rev. 2023, 2023, CD003677. [Google Scholar] [CrossRef] [PubMed]
- Garry, R. Health economics of hysterectomy. Best Pract. Res. Clin. Obs. Gynaecol. 2005, 19, 451–465. [Google Scholar] [CrossRef]
- Baekelandt, J.; De Mulder, P.A.; Le Roy, I.; Mathieu, C.; Laenen, A.; Enzlin, P.; Weyers, S.; Mol, B.W.; Bosteels, J.J. Postoperative outcomes and quality of life following hysterectomy by natural orifice transluminal endoscopic surgery (NOTES) compared to laparoscopy in women with a non-prolapsed uterus and benign gynaecological disease: A systematic review and meta-analysis. Eur. J. Obstet. Gynecol. Reprod. Biol. 2017, 208, 6–15. [Google Scholar] [CrossRef]
- Kaya, C.; Yıldız, Ş.; Alay, İ.; Aslan, Ö.; Aydıner, İ.E.; Yaşar, L. The Comparison of Surgical Outcomes following Laparoscopic Hysterectomy and vNOTES Hysterectomy in Obese Patients. J. Investig. Surg. 2022, 35, 862–867. [Google Scholar] [CrossRef]
- Nesargikar, P.N.; Jaunoo, S.S. Natural orifice translumenal endoscopic surgery (N.O.T.E.S). Int. J. Surg. 2009, 7, 232–236. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Kale, A.; Sarıibrahim, B.; Başol, G. Hysterectomy and salphingoopherectomy by Transvaginal Natural Orifice Transluminal Endoscopic Surgery(NOTES): Turkish surgeons’ initial experience. Int. J. Surg. 2017, 47, 62–68. [Google Scholar] [CrossRef] [PubMed]
- Baekelandt, J.; De Mulder, P.; Le Roy, I.; Mathieu, C.; Laenen, A.; Enzlin, P.; Weyers, S.; Mol, B.W.J.; Bosteels, J. Hysterectomy by transvaginal natural orifice transluminal endoscopic surgery versus laparoscopy as a day-care procedure: A randomised controlled trial. BJOG Int. J. Obstet. Gynaecol. 2019, 126, 105–113. [Google Scholar] [CrossRef]
- Emmerich, S.; Fryar, C.; Stierman, B.; Ogden, C. Obesity and Severe Obesity Prevalence in Adults: United States, August 2021–August 2023; CDC: Atlanta, GA, USA, 2024. [Google Scholar] [CrossRef]
- Kahan, S.; Winston, G. Addressing Obesity in Clinical Gynecology Practice. Clin. Obs. Gynecol. 2018, 61, 10–26. [Google Scholar] [CrossRef]
- Matanes, E.; Eisenberg, N.; Amajoud, Z.; Gupta, V.; Yasmeen, A.; Ismail, S.; Racovitan, F.; Raban, O.; Lau, S.; Salvador, S.; et al. Sentinel Lymph Node Sampling as an Alternative to Lymphadenectomy in Patients with Endometrial Cancer and Obesity. J. Obstet. Gynaecol. Can. 2021, 43, 1136–1144. [Google Scholar] [CrossRef]
- McMahon, M.D.; Scott, D.M.; Saks, E.; Tower, A.; Raker, C.A.; Matteson, K.A. Impact of Obesity on Outcomes of Hysterectomy. J. Minim. Invasive Gynecol. 2014, 21, 259–265. [Google Scholar] [CrossRef]
- Grieco, D.L.; Anzellotti, G.M.; Russo, A.; Bongiovanni, F.; Costantini, B.; D’iNdinosante, M.; Varone, F.; Cavallaro, F.; Tortorella, L.; Polidori, L.; et al. Airway Closure during Surgical Pneumoperitoneum in Obese Patients. Anesthesiology 2019, 131, 58–73. [Google Scholar] [CrossRef]
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. Int. J. Surg. 2021, 88, 105906. [Google Scholar] [CrossRef]
- Stang, A. Critical evaluation of the Newcastle-Ottawa scale for the assessment of the quality of nonrandomized studies in meta-analyses. Eur. J. Epidemiol. 2010, 25, 603–605. [Google Scholar] [CrossRef]
- Kaya, C.; Alay, I.; Cengiz, H.; Yıldız, G.O.; Baghaki, H.S.; Yasar, L. Comparison of hysterectomy cases performed via conventional laparoscopy or vaginally assisted natural orifice transluminal endoscopic surgery: A paired sample cross-sectional study. J. Obs. Gynaecol. 2021, 41, 434–438. [Google Scholar] [CrossRef] [PubMed]
- Bouchez, M.C.; Delporte, V.; Delplanque, S.; Leroy, M.; Vandendriessche, D.; Rubod, C.; Cosson, M.; Giraudet, G. vNOTES Hysterectomy: What about Obese Patients? J. Minim. Invasive Gynecol. 2023, 30, 569–575. [Google Scholar] [CrossRef] [PubMed]
- Wang, F.; Liu, Y.; Xing, Y.; Wang, D.; Bai, X.; Li, L.; Ma, C.; Sun, Y.; Bai, Y.; Wang, L. Clinical efficacy and safety study of vNOTES for benign ovarian tumors in obese patients. Sci. Rep. 2025, 15, 4609. [Google Scholar] [CrossRef]
- Matak, L.; Medić, F.; Sonicki, Z.; Matak, M.; Šimičević, M.; Baekelandt, J. Retrospective analysis between total laparoscopic and vNOTES hysterectomy in obese patients: Single-center study. Arch. Gynecol. Obs. 2024, 309, 2735–2740. [Google Scholar] [CrossRef] [PubMed]
- Mat, E.; Kale, A.; Gundogdu, E.C.; Basol, G.; Yildiz, G.; Usta, T. Transvaginal natural orifice endoscopic surgery for extremely obese patients with early-stage endometrial cancer. J. Obstet. Gynaecol. Res. 2021, 47, 262–269. [Google Scholar] [CrossRef]
- Burnett, A.F.; Pitman, T.C.; Baekelandt, J.F. vNOTES (vaginal natural orifice transluminal surgery) gynecologic procedures in morbidly and super-morbidly obese women: Five year experience. Arch. Gynecol. Obs. 2023, 309, 565–570. [Google Scholar] [CrossRef] [PubMed]
- Altintas, M.M.; Kuru, B.; Küçük, H.F.; Kaya, S.; Mat, E.; Cevik, A. Concurrent hysterectomy and umbilical hernia repair via transvaginal notes among morbidly obese patients. Clin. Exp. Obs. Gynecol. 2022, 49, 30. [Google Scholar] [CrossRef]
- Guevara, R.; Ortega, C.; Fernandez-Gonzalez, S.; Barahona, M.; Martinez, J.M.; Perez, S.; Torrejón-Becerra, J.C.; Castilla, M.; Alemany, J.; Cañizares, A.; et al. 191 VNOTES feasibility in the surgical treatment of endometrial cancer: A case series. Int. J. Gynecol. Cancer 2024, 34, A162. [Google Scholar] [CrossRef]
- Kale, A.; Mat, E.; Başol, G.; Gündoğdu, E.C.; Aboalhasan, Y.; Yildiz, G.; Kuru, B.; Kale, E.; Usta, T.; Altıntaş, M.; et al. A New and Alternative Route: Transvaginal Natural Orifice Transluminal Endoscopic Scarless Surgery (vaginal natural orifice transluminal endoscopic surgery) for Class 2 and Class 3 Obese Patients Suffering from Benign and Malignant Gynecologic Pathologies. Surg. Innov. 2022, 29, 730–741. [Google Scholar] [CrossRef] [PubMed]
- Kapurubandara, S.; Baekelandt, J.; Laws, P.; King, J. Adoption of vaginally assisted natural orifice transluminal endoscopic surgery for hysterectomy: A single tertiary experience. Aust. N. Z. J. Obstet. Gynaecol. 2025, 65, 77–84. [Google Scholar] [CrossRef]
- Matak, L.; Šimičević, M.; Dukić, B.; Matak, M.; Baekelandt, J. vNOTES surgical staging for endometrial carcinoma in overweight patients: A case series. Arch. Gynecol. Obs. 2024, 309, 2829–2832. [Google Scholar] [CrossRef] [PubMed]
- Ng, W.; Lim, N.; Ang, J.X.; Wong, Y.W.Y.; Nadarajah, R. Transvaginal natural orifice transluminal endoscopic surgery hysterectomy in patients with body mass index >50: An Asian experience. J. Obstet. Gynaecol. Res. 2024, 50, 2153–2157. [Google Scholar] [CrossRef]
- Hurni, Y.; Simonson, C.; Di Serio, M.; Lachat, R.; Bodenmann, P.; Seidler, S.; Huber, D. Feasibility and safety of vNOTES for gynecological procedures in obese patients. J. Gynecol. Obs. Hum. Reprod. 2023, 52, 102687. [Google Scholar] [CrossRef]
- Musin, I.I.; Berg, E.A.; Yashchuk, A.G.; Murtazina, G.K.; Ovsiuk, D.N.; Gimaeva, Z.T. Vaginal natural orifice transluminal endoscopic total hysterectomy (vNOTES). Gynecol. Obstet. Clin. Med. 2024, 4, e000015. [Google Scholar] [CrossRef]
- Nef, J.; Hurni, Y.; Simonson, C.; Fournier, I.; Di Serio, M.; Lachat, R.; Bodenmann, P.; Seidler, S.; Huber, D. Safety and efficacy of transvaginal natural orifice endoscopic surgery (vNOTES) for gynecologic procedures in the elderly: A case series of 119 consecutive patients. Eur. J. Obstet. Gynecol. Reprod. Biol. 2025, 308, 23–28. [Google Scholar] [CrossRef]
- Housmans, S.; Noori, N.; Kapurubandara, S.; Bosteels, J.J.A.; Cattani, L.; Alkatout, I.; Deprest, J.; Baekelandt, J. Systematic Review and Meta-Analysis on Hysterectomy by Vaginal Natural Orifice Transluminal Endoscopic Surgery (vNOTES) Compared to Laparoscopic Hysterectomy for Benign Indications. J. Clin. Med. 2020, 9, 3959. [Google Scholar] [CrossRef]
- Chaccour, C.; Giannini, A.; Golia D’Augè, T.; Ayed, A.; Allahqoli, L.; Alkatout, I.; Laganà, A.S.; Chiantera, V.; D’ORia, O.; Sleiman, Z. Hysterectomy Using Vaginal Natural Orifice Transluminal Endoscopic Surgery Compared with Classic Laparoscopic Hysterectomy: A New Advantageous Approach? A Systematic Review on Surgical Outcomes. Gynecol. Obs. Investig. 2023, 88, 187–196. [Google Scholar] [CrossRef]
- Yang, E.; Nie, D.; Li, Z. Comparison of Major Clinical Outcomes Between Transvaginal NOTES and Traditional Laparoscopic Surgery: A Systematic Review and Meta-analysis. J. Surg. Res. 2019, 244, 278–290. [Google Scholar] [CrossRef]
- Steinemann, D.C.; Müller, P.C.; Probst, P.; Schwarz, A.; Büchler, M.W.; Müller-Stich, B.P.; Linke, G.R. Meta-analysis of hybrid natural-orifice transluminal endoscopic surgery versus laparoscopic surgery. Br. J. Surg. 2017, 104, 977–989. [Google Scholar] [CrossRef]
- Lee, C.L.; Wu, K.Y.; Tsao, F.Y.; Huang, C.-Y.; Han, C.-M.; Yen, C.-F.; Huang, K.-G. Natural orifice transvaginal endoscopic surgery for endometrial cancer. Gynecol. Minim. Invasive Ther. 2014, 3, 89–92. [Google Scholar] [CrossRef]
- Oh, S.H.; Park, S.J.; Lee, E.J.; Yim, G.W.; Kim, H.S. Pelvic lymphadenectomy by vaginal natural orifice transluminal endoscopic surgery (vNOTES) for early-stage endometrial cancer. Gynecol. Oncol. 2019, 153, 211–212. [Google Scholar] [CrossRef] [PubMed]
- Tantitamit, T.; Lee, C.L. Application of Sentinel Lymph Node Technique to Transvaginal Natural Orifices Transluminal Endoscopic Surgery in Endometrial Cancer. J. Minim. Invasive Gynecol. 2019, 26, 949–953. [Google Scholar] [CrossRef] [PubMed]
- Huber, D.; Hurni, Y. Sentinel Node Biopsy for Endometrial Cancer by Retroperitoneal Transvaginal Natural Orifice Transluminal Endoscopic Surgery: A Preliminary Study. Front. Surg. 2022, 9, 907548. [Google Scholar] [CrossRef]
- Baekelandt, J.F. New Retroperitoneal Transvaginal Natural Orifice Transluminal Endoscopic Surgery Approach to Sentinel Node for Endometrial Cancer: A Demonstration Video. J. Minim. Invasive Gynecol. 2019, 26, 1231–1232. [Google Scholar] [CrossRef]
- Deng, L.; Liu, Y.; Yao, Y.; Deng, Y.; Tang, S.; Sun, L.; Wang, Y. Efficacy of vaginal natural orifice transluminal endoscopic sentinel lymph node biopsy for endometrial cancer: A prospective multicenter cohort study. Int. J. Surg. 2023, 109, 2996–3002. [Google Scholar] [CrossRef]
- Baekelandt, J.; Kapurubandara, S. Benign Gynaecological procedures by vaginal Natural Orifice Transluminal Endoscopic Surgery (vNOTES): Complication data from a series of 1000 patients. Eur. J. Obstet. Gynecol. Reprod. Biol. 2021, 256, 221–224. [Google Scholar] [CrossRef]
- Marchand, G.J.; Ulibarri, H.; Arroyo, A.; Blanco, M.; Herrera, D.G.; Hamilton, B.; Ruffley, K.; Azadi, A. Systematic review and meta-analysis of vaginal natural orifice transluminal endoscopic surgery hysterectomy versus vaginal hysterectomy for benign indications. AJOG Glob. Rep. 2024, 4, 100355. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).