Effect of Beveling Large Class II Cavities on the Enamel Marginal Quality of Direct Resin-Based Restorations
Abstract
1. Introduction
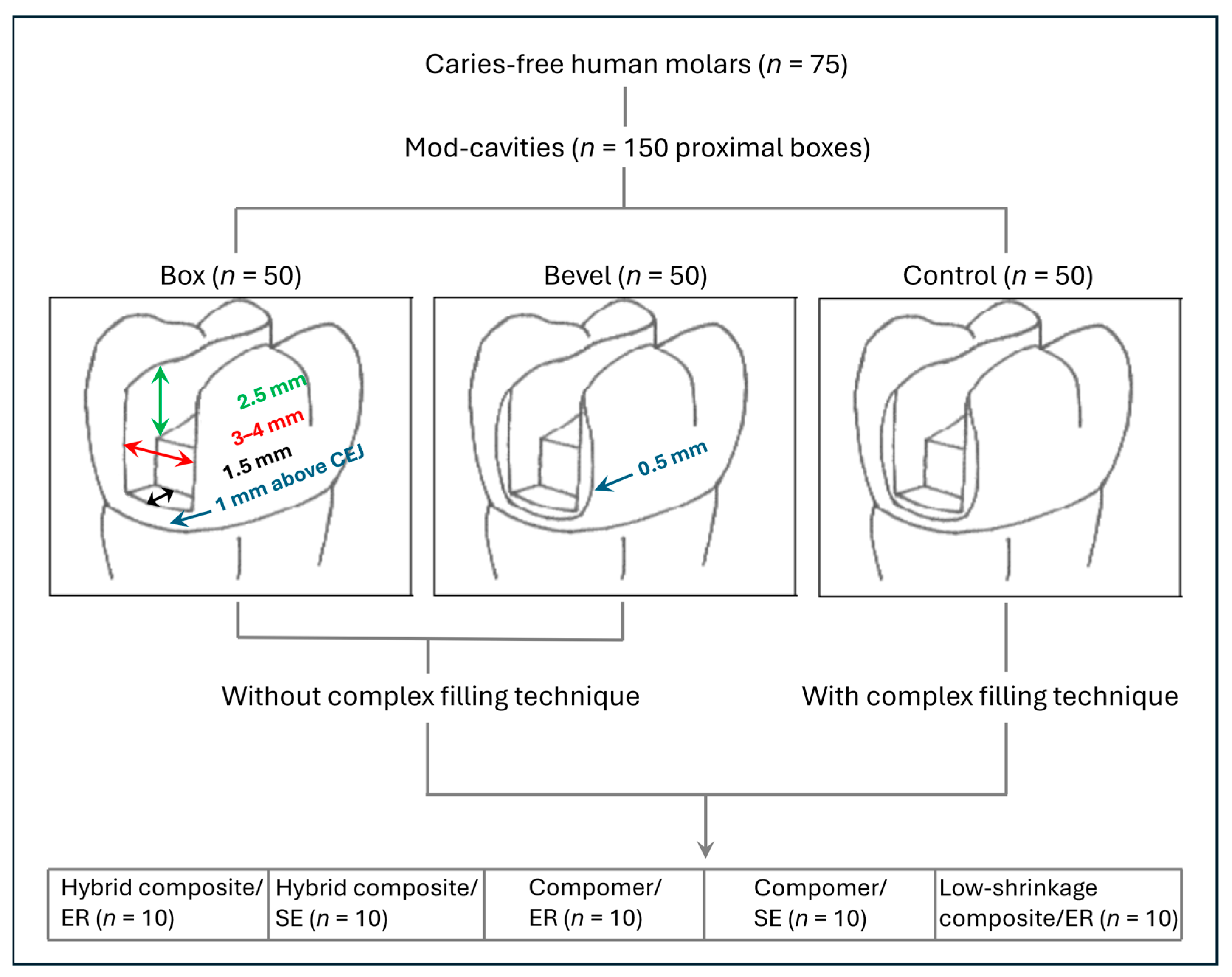
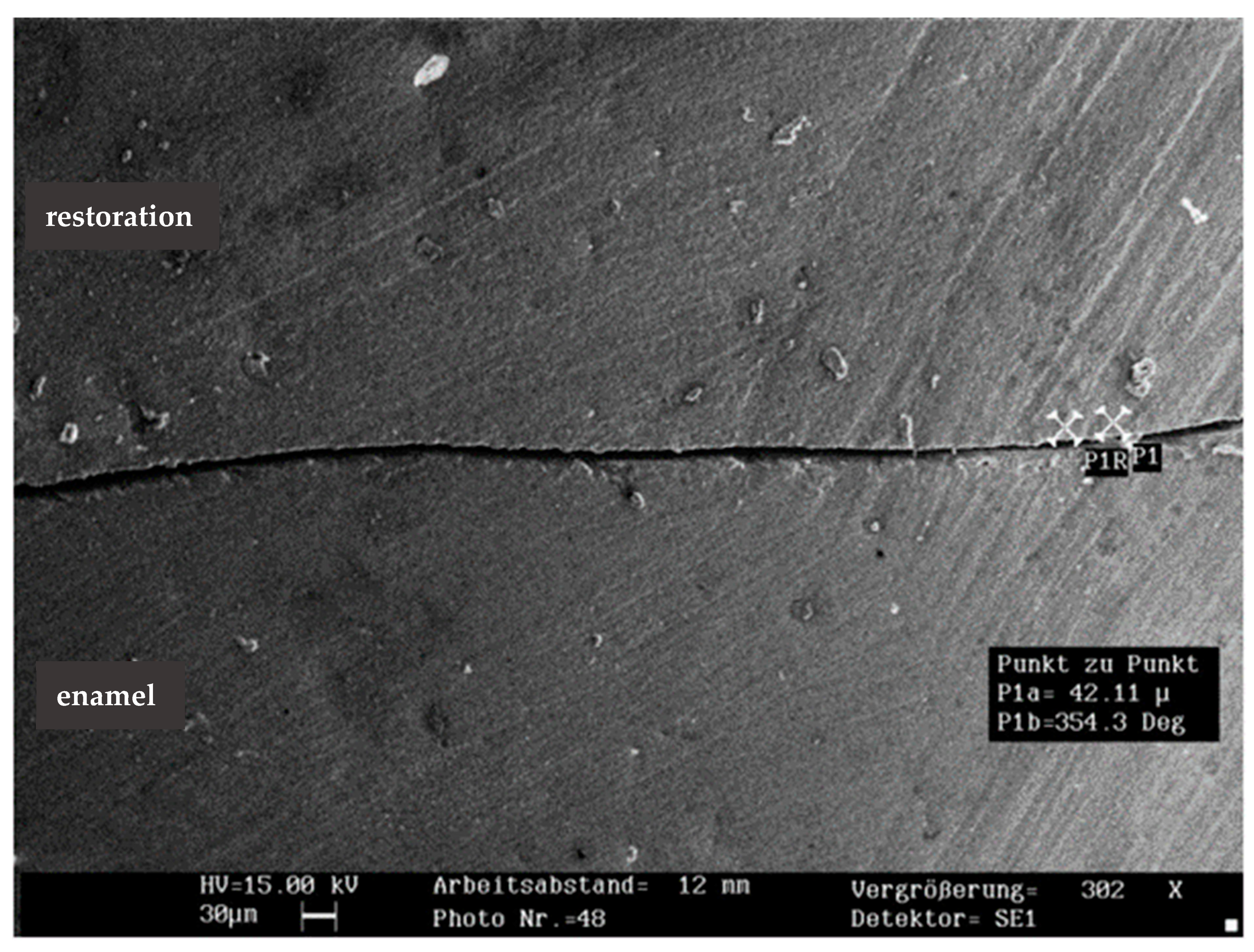
2. Materials and Methods
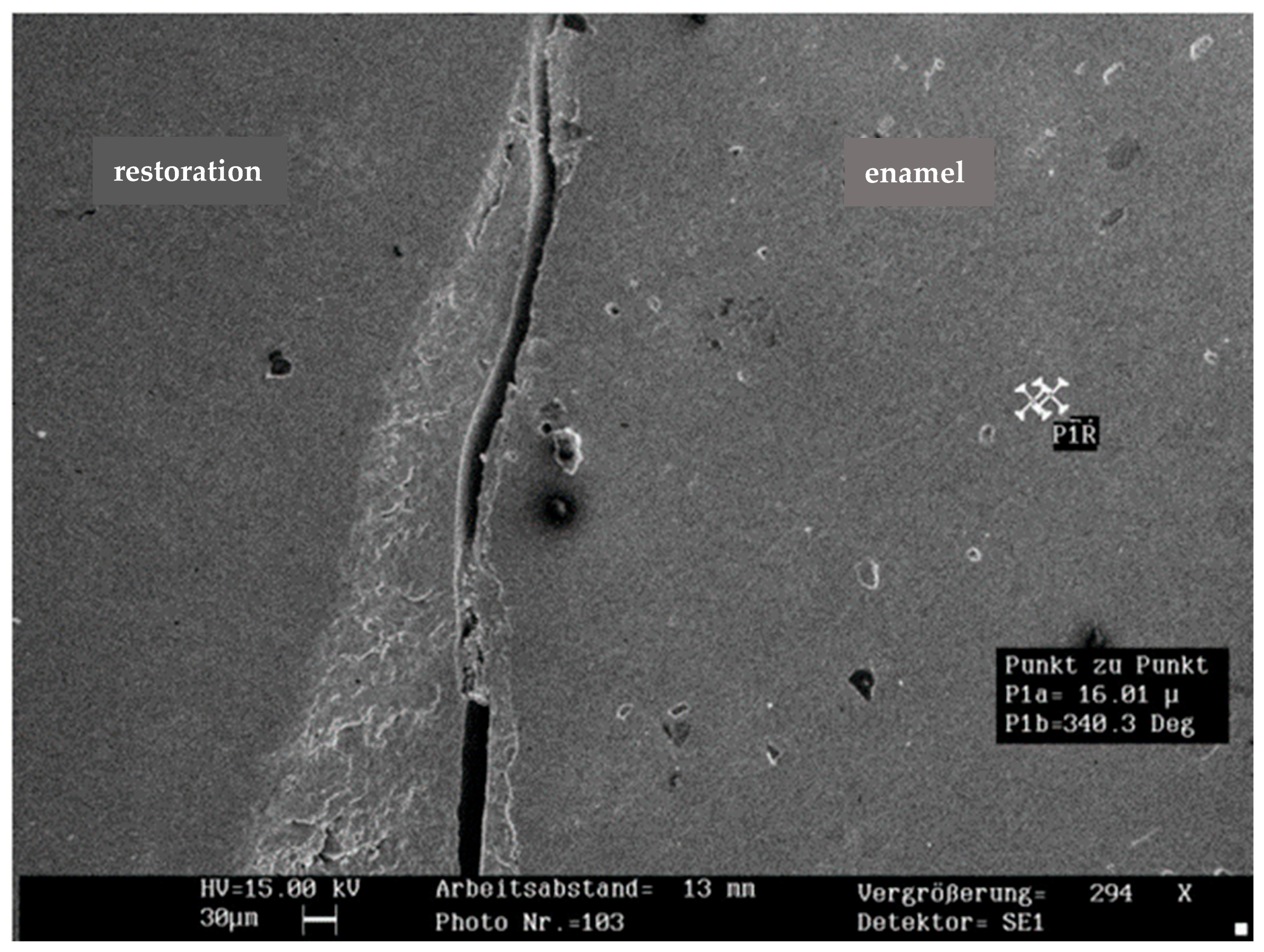
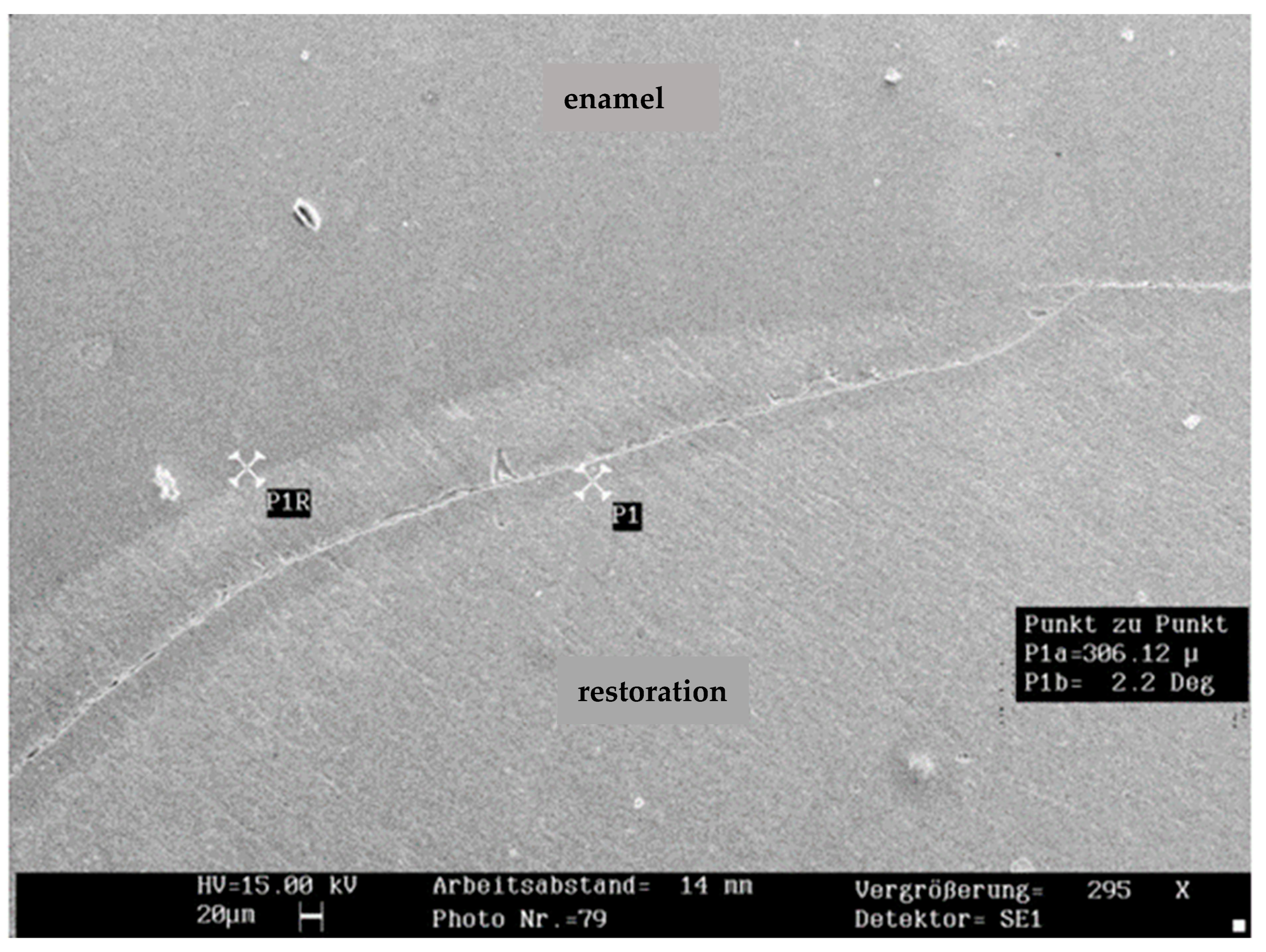
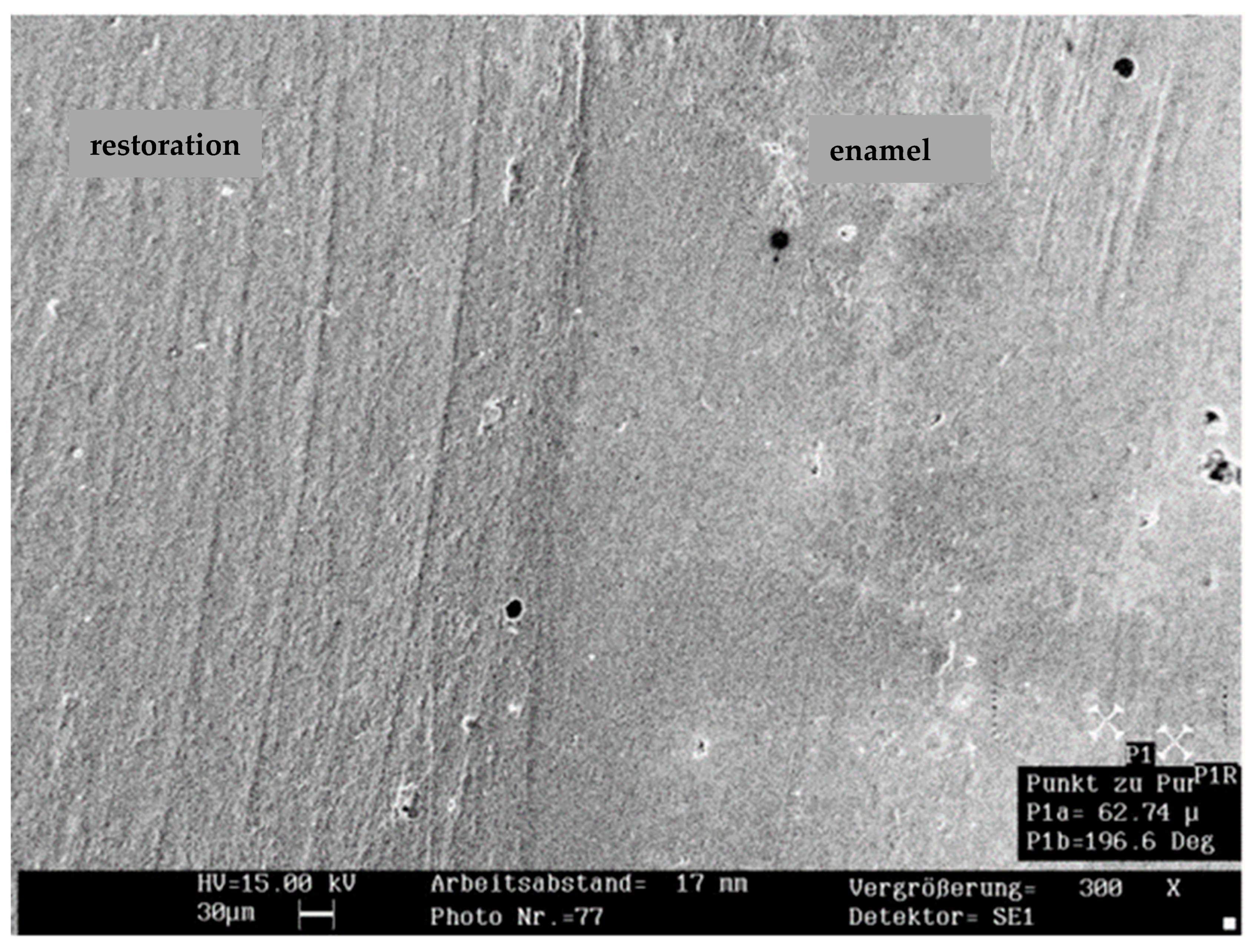
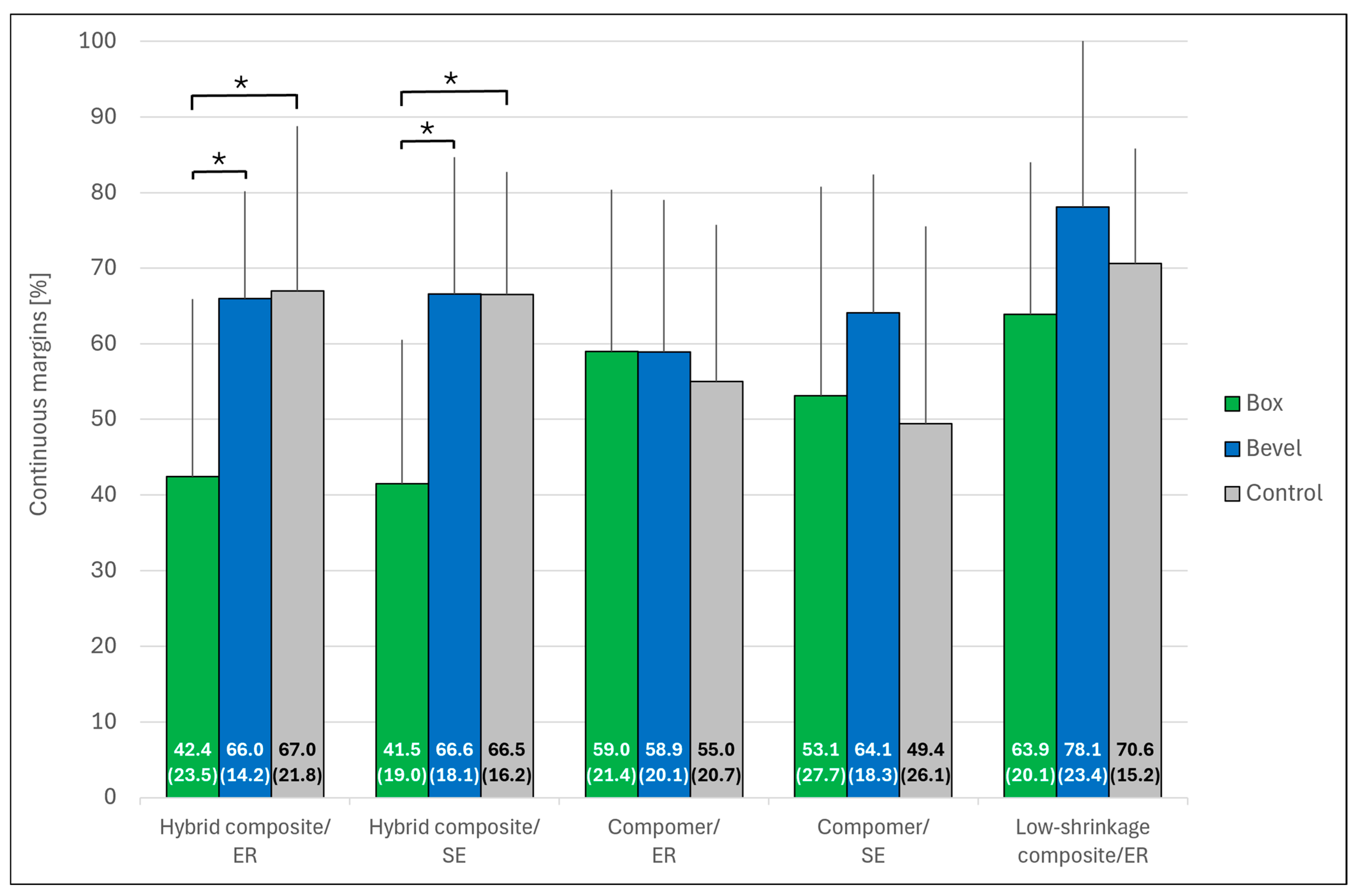
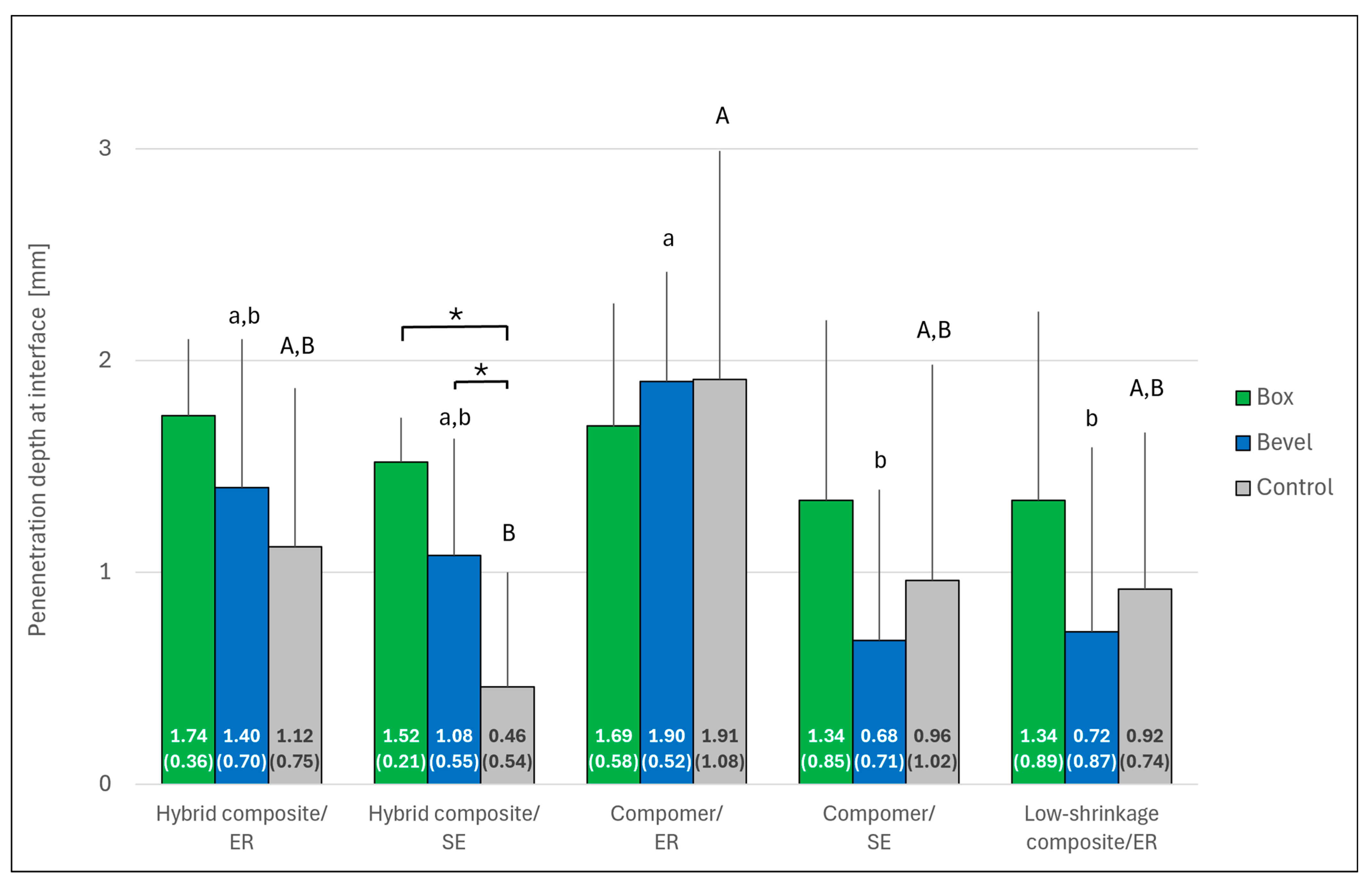
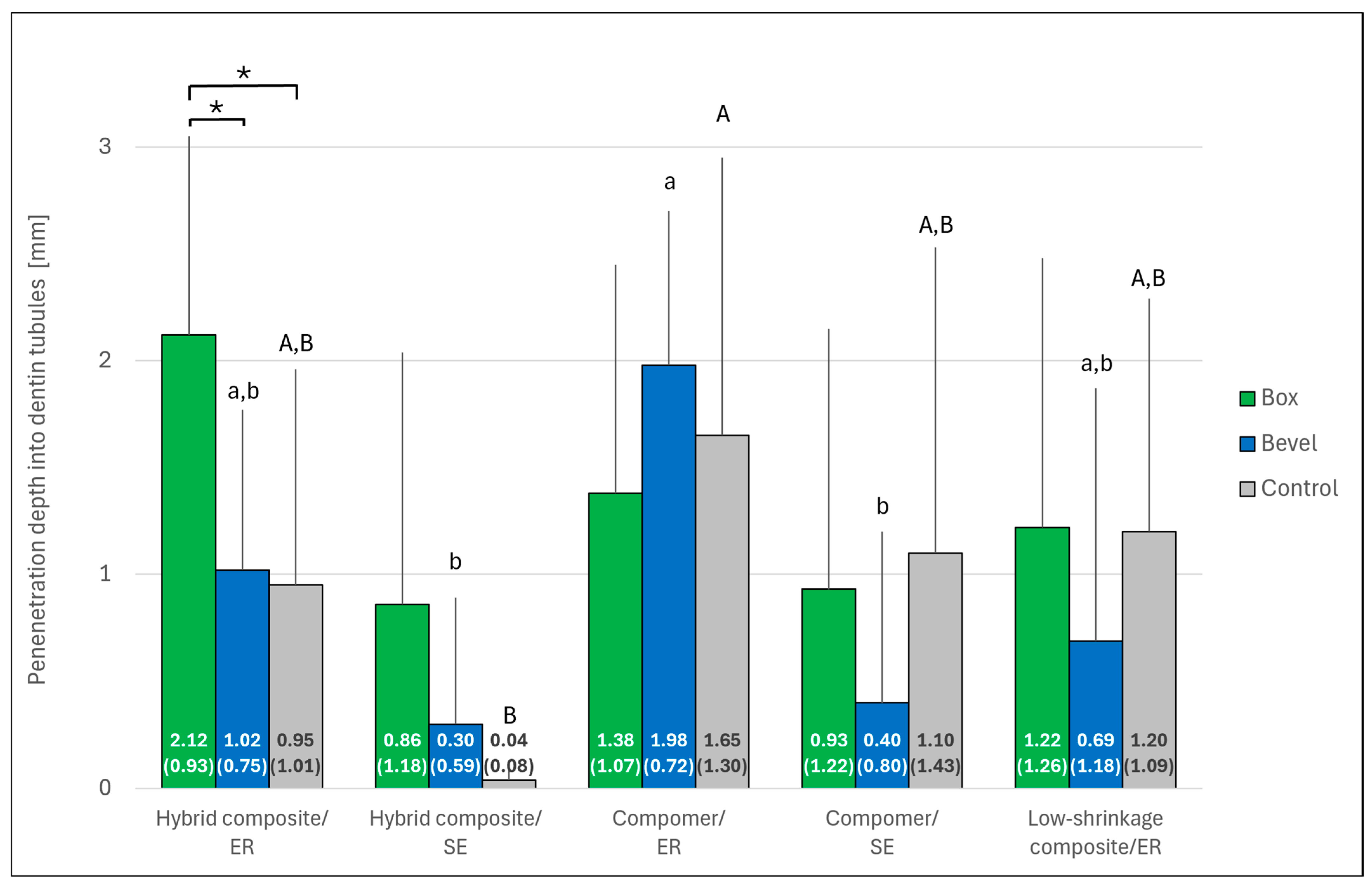
3. Results
4. Discussion
5. Clinical Relevance
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Demarco, F.F.; Cenci, M.S.; Montagner, A.F.; de Lima, V.P.; Correa, M.B.; Moraes, R.R.; Opdam, N.J.M. Longevity of composite restorations is definitely not only about materials. Dent. Mater. 2023, 39, 1–12. [Google Scholar] [CrossRef]
- Heintze, S.D.; Loguerico, A.D.; Hanzen, T.A.; Reis, A.; Rousson, V. Clinical efficacy of resin-based direct posterior restorations and glass-ionomer restorations—An updated meta-analysis of clinical outcome parameters. Dent. Mater. 2022, 38, e109–e135. [Google Scholar] [CrossRef]
- Özdemir, S.; Ayaz, İ.; Çetin Tuncer, N.; Barutçugil, Ç.; Dündar, A. Evaluation of polymerization shrinkage, microhardness, and depth of cure of different types of bulk-fill composites. J. Esthet. Restor. Dent. 2025, 37, 1920–1929. [Google Scholar] [CrossRef]
- Soares, C.J.; Faria-E-Silva, A.L.; Rodrigues, M.P.; Vilela, A.B.F.; Pfeifer, C.S.; Tantbirojn, D.; Versluis, A. Polymerization shrinkage stress of composite resins and resin cements—What do we need to know? Braz. Oral Res. 2017, 31, e62. [Google Scholar] [CrossRef]
- Peutzfeldt, A.; Hug, T.; Wierichs, R.J. Bond strength and marginal adaptation of resin composites and correlations with clinical results. Dent. Mater. 2024, 40, 966–975. [Google Scholar] [CrossRef]
- Nedeljkovic, I.; De Munck, J.; Vanloy, A.; Declerck, D.; Lambrechts, P.; Peumans, M.; Teughels, W.; Van Meerbeek, B.; Van Landuyt, K.L. Secondary caries: Prevalence, characteristics, and approach. Clin. Oral Investig. 2020, 24, 683–691. [Google Scholar] [CrossRef]
- Gaengler, P.; Hoyer, I.; Montag, R. Clinical evaluation of posterior composite restorations: The 10-year report. J. Adhes. Dent. 2001, 3, 185–194. [Google Scholar]
- Lim, Z.E.; Duncan, H.F.; Moorthy, A.; McReynolds, D. Minimally invasive selective caries removal: A clinical guide. Br. Dent. 2023, 234, 233–240. [Google Scholar] [CrossRef] [PubMed]
- Reis, A.; Feitosa, V.P.; Chibinski, A.C.; Favoreto, M.W.; Gutierrez, M.F.; Loguercio, A.D. Biomimetic restorative dentistry: An evidence-based discussion of common myths. J. Appl. Oral Sci. 2024, 32, e20240271. [Google Scholar] [CrossRef] [PubMed]
- Van Meerbeek, B.; Yoshihara, K.; Van Landuyt, K.; Yoshida, Y.; Peumans, M. From Buonocore’s pioneering acid-etch technique to self-adhering restoratives. A status perspective of rapidly advancing dental adhesive technology. J. Adhes. Dent. 2020, 22, 7–34. [Google Scholar]
- Rathke, A.; Ostermeier, V.; Muche, R.; Haller, B. Reconsidering the double etching of enamel: Do self-etching primers contaminate phosphoric acid-etched enamel? J. Adhes. Dent. 2013, 15, 107–114. [Google Scholar] [PubMed]
- Schmidlin, P.R.; Wolleb, K.; Imfeld, T.; Gygax, M.; Lussi, A. Influence of beveling and ultrasound application on marginal adaptation of box-only Class II (slot) resin composite restorations. Oper. Dent. 2007, 32, 291–297. [Google Scholar] [CrossRef]
- Coelho-De-Souza, F.H.; Camacho, G.B.; Demarco, F.F.; Powers, J.M. Fracture resistance and gap formation of MOD restorations: Influence of restorative technique, bevel preparation and water storage. Oper. Dent. 2008, 33, 37–43. [Google Scholar] [CrossRef]
- Opdam, N.J.M.; Roeters, J.J.; Kujis, R.; Burgersdijk, R.C.W. Necessity of bevels for box only Class II composite restorations. J. Prosthet. Dent. 1998, 80, 274–279. [Google Scholar] [CrossRef]
- Hilton, T.J.; Ferracane, J.L. Cavity preparation factors and microleakage of Class II composite restorations filled at intraoral temperatures. Am. J. Dent. 1999, 12, 123–130. [Google Scholar]
- Meurer, J.C.; Rizzante, F.A.P.; Maenossono, R.M.; França, F.M.G.; Bombonatti, J.F.S.; Ishikiriama, S.K. Effect of cavosurface angle beveling on the exposure angle of enamel prisms in different cavity sizes. Microsc. Res. Tech. 2020, 83, 304–309. [Google Scholar] [CrossRef]
- Apel, Z.; Vafaeian, B.; Zarzecka, J.; Wuzinski, J.; Apel, D.B. Comparative analysis of various cavosurface margins in Class II restorations using 3D finite element method. Int. J. Numer. Methods Biomed. Eng. 2025, 41, e70041. [Google Scholar] [CrossRef] [PubMed]
- Dietrich, T.; Kraemer, M.; Lösche, G.M.; Roulet, J.F. Marginal integrity of large compomer Class II restorations with cervical margins in dentine. J. Dent. 2000, 28, 399–405. [Google Scholar] [CrossRef]
- Zaruba, M.; Wegehaupt, F.J.; Attin, T. Comparison between different flow application techniques: SDR vs flowable composite. J. Adhes. Dent. 2012, 15, 115–121. [Google Scholar]
- Hahn, B.; Haubitz, I.; Krug, R.; Krastl, G.; Soliman, S. Influence of matrix type on marginal gap formation of deep Class II bulk-fill composite restorations. Int. J. Environ. Res. Public Health 2022, 19, 4961. [Google Scholar] [CrossRef]
- Dietschi, D.; Askari, M.; Rossier, I.; Caseiro, L.; Krejci, I.; Leprince, J.G.; Di Bella, E.; Ardu, S. Marginal adaptation of in vitro Class II restorations made out of bulk or conventional composite using single- or multi-layered techniques. Materials 2023, 16, 6325. [Google Scholar] [CrossRef]
- Soliman, S.; Preidl, R.; Karl, S.; Hofmann, N.; Krastl, G.; Klaiber, B. Influence of cavity margin design and restorative material on marginal quality and seal of extended Class II resin composite restorations in vitro. J. Adhes. Dent. 2016, 18, 7–16. [Google Scholar]
- Isenberg, B.P.; Leinfelder, K.F. Efficacy of beveling posterior composite resin preparations. J. Esthet. Dent. 1990, 2, 70–73. [Google Scholar]
- Coelho-De-Souza, F.H.; Camargo, J.C.; Beskow, T.; Balestrin, M.D.; Klein-Júnior, C.A.; Demarco, F.F. A randomized double-blind clinical trial of posterior composite restorations with or without bevel: 1-year follow-up. J. Appl. Oral Sci. 2012, 20, 174–179. [Google Scholar] [CrossRef] [PubMed]
- Patanjali, S.; Arora, A.; Arya, A.; Grewal, M.S. An in vitro study of effect of beveling of enamel on microleakage and shear bond strength of adhesive systems in primary and permanent teeth. Int. J. Clin. Pediatr. Dent. 2019, 12, 205–210. [Google Scholar] [CrossRef] [PubMed]
- Swanson, T.K.; Feigal, R.J.; Tantbirojn, D.; Hodges, J.S. Effect of adhesive systems and bevel on enamel margin integrity in primary and permanent teeth. Pediatr. Dent. 2008, 30, 134–140. [Google Scholar]
- Central Ethical Review Committee. The (further) Use of Human Body Materials for the Purposes of Medical Research [in German]. 2003. Available online: www.zentrale-ethikkommission.de/fileadmin/user_upload/_old-files/downloads/pdf-Ordner/Zeko/Koerpermat-1.pdf (accessed on 28 June 2025).
- Tjan, A.H.; Bergh, B.H.; Lidner, C. Effect of various incremental techniques on the marginal adaptation of class II composite resin restorations. J. Prosthet. Dent. 1992, 67, 62–66. [Google Scholar] [CrossRef] [PubMed]
- ISO. Dental Materials—Testing of Adhesion to Tooth Structure; Technical Specification: 2003; No. 11405. Available online: https://cdn.standards.iteh.ai/samples/31486/30aec144f6404fba864b3a908380037a/ISO-TS-11405-2003.pdf (accessed on 28 June 2025).
- Heintze, S.D. Clinical relevance of tests on bond strength, microleakage and marginal adaptation. Dent. Mater. 2013, 29, 59–84. [Google Scholar] [CrossRef]
- Wang, C.; Xu, J.; Xu, J.; Deng, S.; Fu, B.; Zhang, L. Effect of the prism-interprisms three-dimension spatial microstructure on the enamel bond strength. BMC Oral Health 2023, 23, 855. [Google Scholar] [CrossRef]
- Van Dijken, J.W.V.; Lindberg, A. A 15-year randomized controlled study of a reduced shrinkage stress resin composite. Dent. Mater. 2015, 31, 1150–1158. [Google Scholar] [CrossRef]
- Pummer, A.; Cieplik, F.; Nikolić, M.; Buchalla, W.; Hiller, K.A.; Schmalz, G. Longevity of posterior composite and compomer restorations in children placed under different types of anesthesia: A retrospective 5-year study. Clin. Oral Investig. 2020, 24, 141–150. [Google Scholar] [CrossRef] [PubMed]
- Lund, R.G.; Piva, E.; de Moura, F.R.; Demarco, F.F.; de Oliveira Lima, J.; Cardoso, P.E.C. Two-year clinical wear performance of two polyacid-modified resin composites (compomers) in posterior treatment teeth. Braz. J. Oral Sci. 2008, 25, 1539–1542. [Google Scholar]
- Frankenberger, R.; Friedrich, K.; Dudek, M.C.; Winter, J.; Krämer, N.; Roggendorf, M.J. Influence of proximal-cervical undermined enamel areas on marginal quality and enamel integrity of laboratory and CAD/CAM ceramic inlays and partial crowns. J. Funct. Biomater. 2025, 16, 82. [Google Scholar] [CrossRef] [PubMed]
| Restorative Material | Brand Name (Manufacturer; LOT No.) | Adhesive (Manufacturer; LOT No.) | Adhesive Application | Mode |
|---|---|---|---|---|
| Micro hybrid composite | Spectrum TPH (Dentsply Sirona, Konstanz, Germany; 0204000776) | Prime & Bond NT (Dentsply Sirona, Konstanz, Germany; 0204000566) | Apply etchant for 30 s (enamel) and 15 s (dentin). Rinse and gently air dry. Apply adhesive for 20 s. Gently air blow. Light cure for 20 s * | ER |
| Adper Prompt L-Pop (3M, Seefeld, Germany; 132885) | Activate blister. Apply adhesive and rub for 15 s. Gently air blow. Light cure for 10 s * | SE | ||
| Compomer | Dyract Posterior (Dentsply Sirona, Konstanz, Germany; 0206001456) | Prime & Bond NT | Apply etchant for 30 s (enamel) and 15 s (dentin). Rinse and gently air dry. Apply adhesive for 20 s. Gently air blow. Light cure for 20 s * | ER |
| Adper Prompt L-Pop | Activate blister, apply adhesive and rub for 15 s. Gently air blow. Light cure for 10 s * | SE | ||
| Low-shrinkage composite | InTen-S (Ivoclar, Schaan, Liechtenstein; E00484) | Excite (Ivoclar, Schaan, Liechtenstein; E51015) | Apply etchant for 30 s (enamel) and 15 s (dentin). Rinse and gently air dry. Apply adhesive and rub for 10 s. Gently air blow. Light cure for 10 s ** | ER |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Rathke, A.; Frehse, H.; Selinka, A. Effect of Beveling Large Class II Cavities on the Enamel Marginal Quality of Direct Resin-Based Restorations. J. Clin. Med. 2025, 14, 5649. https://doi.org/10.3390/jcm14165649
Rathke A, Frehse H, Selinka A. Effect of Beveling Large Class II Cavities on the Enamel Marginal Quality of Direct Resin-Based Restorations. Journal of Clinical Medicine. 2025; 14(16):5649. https://doi.org/10.3390/jcm14165649
Chicago/Turabian StyleRathke, Andreas, Henry Frehse, and Anne Selinka. 2025. "Effect of Beveling Large Class II Cavities on the Enamel Marginal Quality of Direct Resin-Based Restorations" Journal of Clinical Medicine 14, no. 16: 5649. https://doi.org/10.3390/jcm14165649
APA StyleRathke, A., Frehse, H., & Selinka, A. (2025). Effect of Beveling Large Class II Cavities on the Enamel Marginal Quality of Direct Resin-Based Restorations. Journal of Clinical Medicine, 14(16), 5649. https://doi.org/10.3390/jcm14165649






