The Role of Proximal Femoral Osteotomy for the Treatment of Avascular Necrosis: A Systematic Review of Clinical and Patient-Reported Outcomes
Abstract
1. Introduction
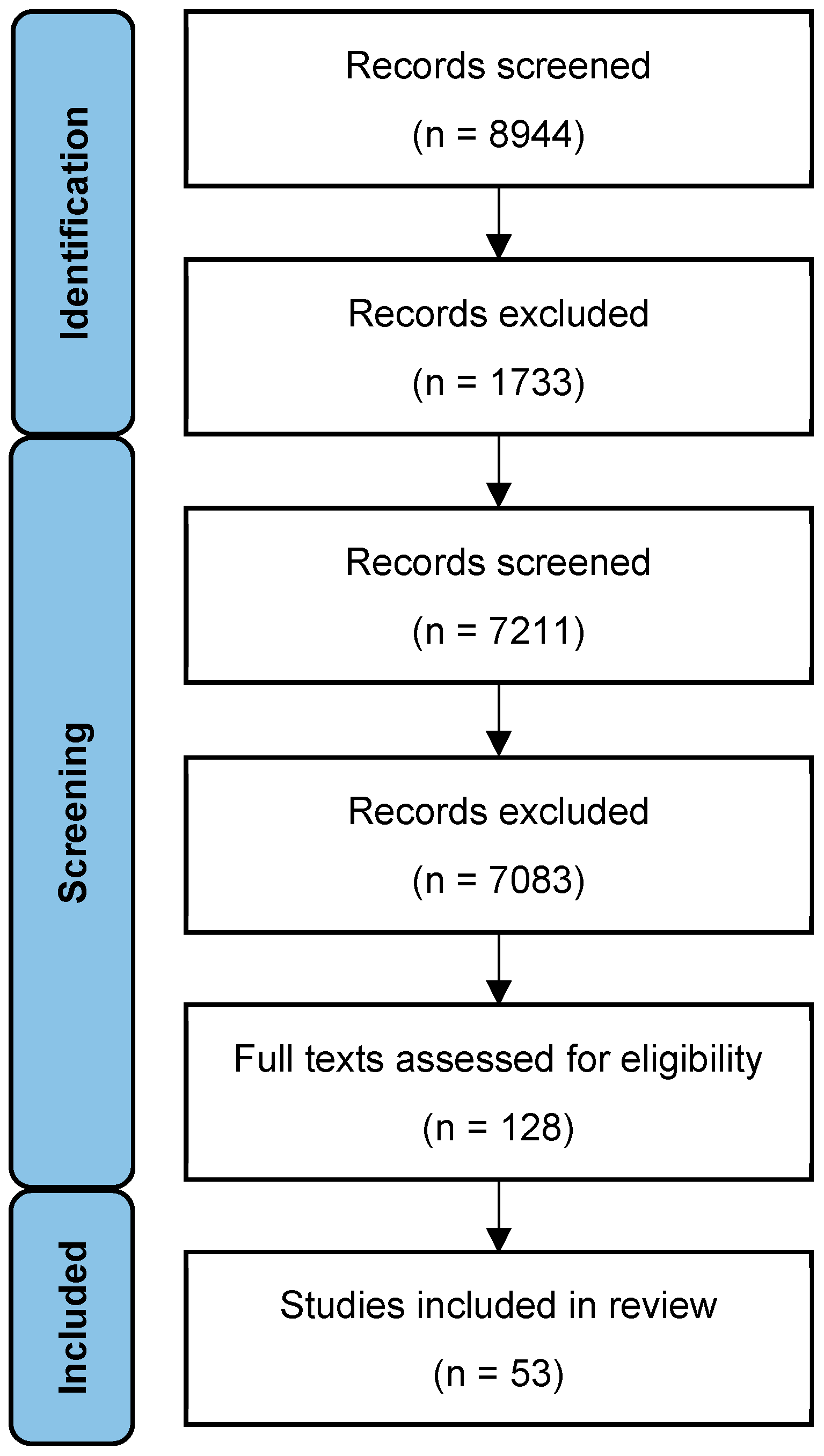
2. Materials and Methods
2.1. Outcome Measure
2.2. Literature Search
2.3. Criteria of Eligibility
2.4. Extraction of Data
2.5. Assessment of Risk of Bias
2.6. Data Synthesis and Analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| AVNFH | Avascular Necrosis of the Femoral Head |
| FWB | Full Weight Bearing |
| HHS | Harris Hip Score |
| IQR | Inter Quartile Range |
| NIH | National Institute for Health |
| MRI | Magnetic Resonance Imaging |
| NWB | Non-Weightbearing |
| OA | Osteoarthritis |
| PRISMA | Preferred Reporting Items for Systematic Reviews and Meta-Analysis |
| PROMS | Patient Reported Outcome Measures |
| PWB | Partial Weightbearing |
| THR | Total Hip Replacement |
References
- George, G.; Lane, J.M. Osteonecrosis of the Femoral Head. J. Am. Acad. Orthop. Surgeons. Glob. Res. Rev. 2022, 6, e21.00176. [Google Scholar] [CrossRef]
- Petek, D.; Hannouche, D.; Suva, D. Osteonecrosis of the femoral head: Pathophysiology and current concepts of treatment. EFORT Open Rev. 2019, 4, 85–97. [Google Scholar] [CrossRef]
- Yoon, B.-H.; Kim, T.-Y.; Shin, I.-S.; Lee, H.Y.; Lee, Y.J.; Koo, K.-H. Alcohol intake and the risk of osteonecrosis of the femoral head in Japanese populations: A dose-response meta-analysis of case-control studies. Clin. Rheumatol. 2017, 36, 2517–2524. [Google Scholar] [CrossRef]
- Mont, M.A.; Pivec, R.; Banerjee, S.; Issa, K.; Elmallah, R.K.; Jones, L.C. High-Dose Corticosteroid Use and Risk of Hip Osteonecrosis: Meta-Analysis and Systematic Literature Review. J. Arthroplast. 2015, 30, 1506–1512.e5. [Google Scholar] [CrossRef]
- Fukushima, W.; Fujioka, M.; Kubo, T.; Tamakoshi, A.; Nagai, M.; Hirota, Y. Nationwide epidemiologic survey of idiopathic osteonecrosis of the femoral head. Clin. Orthop. Relat. Res. 2010, 468, 2715–2724. [Google Scholar] [CrossRef]
- Matthews, A.; Davis, D.; Fish, M.; Stilston, D. Avascular Necrosis; StatPearls: Treasure Island, FL, USA, 2025. [Google Scholar]
- Zhang, Y.-Z.; Cao, X.-Y.; Li, X.-C.; Chen, J.; Zhao, Y.-Y.; Tian, Z.; Zheng, W. Accuracy of MRI diagnosis of early osteonecrosis of the femoral head: A meta-analysis and systematic review. J. Orthop. Surg. Res. 2018, 13, 167. [Google Scholar] [CrossRef]
- Atilla, B.; Bakırcıoğlu, S.; Shope, A.J.; Parvizi, J. Joint-preserving procedures for osteonecrosis of the femoral head. EFORT Open Rev. 2019, 4, 647–658. [Google Scholar] [CrossRef]
- Ancelin, D.; Reina, N.; Cavaignac, E.; Delclaux, S.; Chiron, P. Total hip arthroplasty survival in femoral head avascular necrosis versus primary hip osteoarthritis: Case-control study with a mean 10-year follow-up after anatomical cementless metal-on-metal 28-mm replacement. Orthop. Traumatol. Surg. Res. 2016, 102, 1029–1034. [Google Scholar] [CrossRef]
- Motomura, G. Femoral osteotomy for osteonecrosis of the femoral head. J. Jt. Surg. Res. 2023, 1, 2–8. [Google Scholar] [CrossRef]
- Quaranta, M.; Miranda, L.; Oliva, F.; Aletto, C.; Maffulli, N. Osteotomies for avascular necrosis of the femoral head. Br. Med. Bull. 2021, 137, 98–111. [Google Scholar] [CrossRef]
- Wilson, I.; Bohm, E.; Lübbeke, A.; Lyman, S.; Overgaard, S.; Rolfson, O.; W-Dahl, A.; Wilkinson, M.; Dunbar, M. Orthopaedic registries with patient-reported outcome measures. EFORT Open Rev. 2019, 4, 357–367. [Google Scholar] [CrossRef] [PubMed]
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. BMJ 2021, 372, n71. [Google Scholar] [CrossRef]
- PROSPERO. Available online: https://www.crd.york.ac.uk/PROSPERO/view/CRD420251056765 (accessed on 24 July 2025).
- Ma, L.-L.; Wang, Y.-Y.; Yang, Z.-H.; Huang, D.; Weng, H.; Zeng, X.-T. Methodological quality (risk of bias) assessment tools for primary and secondary medical studies: What are they and which is better? Mil. Med. Res. 2020, 7, 7. [Google Scholar] [CrossRef]
- Kubo, Y.; Motomura, G.; Ikemura, S.; Hatanaka, H.; Utsunomiya, T.; Hamai, S.; Fujii, M.; Fukushi, J.-I.; Nakashima, Y. Effects of anterior boundary of the necrotic lesion on the progressive collapse after varus osteotomy for osteonecrosis of the femoral head. J. Orthop. Sci. 2020, 25, 145–151. [Google Scholar] [CrossRef]
- Kawano, K.; Motomura, G.; Ikemura, S.; Kubo, Y.; Fukushi, J.; Hamai, S.; Fujii, M.; Nakashima, Y. Long-term hip survival and factors influencing patient-reported outcomes after transtrochanteric anterior rotational osteotomy for osteonecrosis of the femoral head: A minimum 10-year follow-up case series. Mod. Rheumatol. 2020, 30, 184–190. [Google Scholar] [CrossRef]
- Kubo, Y.; Motomura, G.; Ikemura, S.; Sonoda, K.; Yamamoto, T.; Nakashima, Y. Factors influencing progressive collapse of the transposed necrotic lesion after transtrochanteric anterior rotational osteotomy for osteonecrosis of the femoral head. Orthop. Traumatol. Surg. Res. 2017, 103, 217–222. [Google Scholar] [CrossRef]
- Lee, Y.-K.; Park, C.H.; Ha, Y.-C.; Kim, D.-Y.; Lyu, S.-H.; Koo, K.-H. Comparison of Surgical Parameters and Results between Curved Varus Osteotomy and Rotational Osteotomy for Osteonecrosis of the Femoral Head. Clin. Orthop. Surg. 2017, 9, 160–168. [Google Scholar] [CrossRef]
- Morita, D.; Hasegawa, Y.; Okura, T.; Osawa, Y.; Ishiguro, N. Long-term outcomes of transtrochanteric rotational osteotomy for non-traumatic osteonecrosis of the femoral head. Bone Jt. J. 2017, 99-B, 175–183. [Google Scholar] [CrossRef]
- Kubo, Y.; Yamamoto, T.; Motomura, G.; Karasuyama, K.; Sonoda, K.; Iwamoto, Y. Patient-reported outcomes of femoral osteotomy and total hip arthroplasty for osteonecrosis of the femoral head: A prospective case series study. SpringerPlus 2016, 5, 1880. [Google Scholar] [CrossRef]
- Okura, T.; Hasegawa, Y.; Morita, D.; Osawa, Y.; Ishiguro, N. What factors predict the failure of curved intertrochanteric varus osteotomy for the osteonecrosis of the femoral head? Arch. Orthop. Trauma Surg. 2016, 136, 1647–1655. [Google Scholar] [CrossRef]
- Sonoda, K.; Yamamoto, T.; Motomura, G.; Nakashima, Y.; Yamaguchi, R.; Iwamoto, Y. Outcome of transtrochanteric rotational osteotomy for posttraumatic osteonecrosis of the femoral head with a mean follow-up of 12.3 years. Arch. Orthop. Trauma Surg. 2015, 135, 1257–1263. [Google Scholar] [CrossRef]
- Hamanishi, M.; Yasunaga, Y.; Yamasaki, T.; Mori, R.; Shoji, T.; Ochi, M. The clinical and radiographic results of intertrochanteric curved varus osteotomy for idiopathic osteonecrosis of the femoral head. Arch. Orthop. Trauma Surg. 2014, 134, 305–310. [Google Scholar] [CrossRef]
- Ito, H.; Tanino, H.; Yamanaka, Y.; Nakamura, T.; Takahashi, D.; Minami, A.; Matsuno, T. Long-term results of conventional varus half-wedge proximal femoral osteotomy for the treatment of osteonecrosis of the femoral head. J. Bone Jt. Surg. Br. Vol. 2012, 94-B, 308–314. [Google Scholar] [CrossRef]
- Ha, Y.-C.; Kim, H.J.; Kim, S.-Y.; Kim, K.-C.; Lee, Y.-K.; Koo, K.-H. Effects of age and body mass index on the results of transtrochanteric rotational osteotomy for femoral head osteonecrosis. J. Bone Jt. Surg. 2011, 93, 75–84. [Google Scholar] [CrossRef]
- Motomura, G.; Yamamoto, T.; Suenaga, K.; Nakashima, Y.; Mawatari, T.; Ikemura, S.; Iwamoto, Y. Long-term outcome of transtrochanteric anterior rotational osteotomy for osteonecrosis of the femoral head in patients with systemic lupus erythematosus. Lupus 2010, 19, 860–865. [Google Scholar] [CrossRef]
- Biswal, S.; Hazra, S.; Yun, H.H.; Hur, C.Y.; Shon, W.Y. Transtrochanteric rotational osteotomy for nontraumatic osteonecrosis of the femoral head in young adults. Clin. Orthop. Relat. Res. 2009, 467, 1529–1537. [Google Scholar] [CrossRef]
- Yoon, T.R.; Abbas, A.A.; Hur, C.I.; Cho, S.G.; Lee, J.H. Modified transtrochanteric rotational osteotomy for femoral head osteonecrosis. Clin. Orthop. Relat. Res. 2008, 466, 1110–1116. [Google Scholar] [CrossRef]
- Sugioka, Y.; Yamamoto, T. Transtrochanteric posterior rotational osteotomy for osteonecrosis. Clin. Orthop. Relat. Res. 2008, 466, 1104–1109. [Google Scholar] [CrossRef]
- Seki, T.; Hasegawa, Y.; Masui, T.; Yamaguchi, J.; Kanoh, T.; Ishiguro, N.; Kawabe, K. Quality of life following femoral osteotomy and total hip arthroplasty for nontraumatic osteonecrosis of the femoral head. J. Orthop. Sci. 2008, 13, 116–121. [Google Scholar] [CrossRef]
- Ikemura, S.; Yamamoto, T.; Jingushi, S.; Nakashima, Y.; Mawatari, T.; Iwamoto, Y. Leg-length discrepancy after transtrochanteric curved varus osteotomy for osteonecrosis of the femoral head. J. Bone Jt. Surg. Br. Vol. 2007, 89-B, 725–729. [Google Scholar] [CrossRef]
- Atsumi, T.; Kajiwara, T.; Hiranuma, Y.; Tamaoki, S.; Asakura, Y. Posterior rotational osteotomy for nontraumatic osteonecrosis with extensive collapsed lesions in young patients. J. Bone Jt. Surg. 2006, 88, 42–47. [Google Scholar] [CrossRef]
- Nakamura, Y.; Kumazawa, Y.; Mitsui, H.; Toh, S.; Katano, H. Combined rotational osteotomy and vascularized iliac bone graft for advanced osteonecrosis of the femoral head. J. Reconstr. Microsurg. 2005, 21, 101–105. [Google Scholar] [CrossRef]
- Onodera, S.; Majima, T.; Abe, Y.; Ito, H.; Matsuno, T.; Minami, A. Transtrochanteric rotational osteotomy for osteonecrosis of the femoral head: Relation between radiographic features and secondary collapse. J. Orthop. Sci. 2005, 10, 367–373. [Google Scholar] [CrossRef]
- Rijnen, W.H.C.; Gardeniers, J.W.M.; Westrek, B.L.M.; Buma, P.; Schreurs, B.W. Sugioka’s osteotomy for femoral-head necrosis in young Caucasians. Int. Orthop. 2005, 29, 140–144. [Google Scholar] [CrossRef]
- Hisatome, T.; Yasunaga, Y.; Takahashi, K.; Ochi, M. Progressive collapse of transposed necrotic area after transtrochanteric rotational osteotomy for osteonecrosis of the femoral head induces osteoarthritic change. Arch. Orthop. Trauma Surg. 2004, 124, 77–81. [Google Scholar] [CrossRef]
- Langlais, F.; Fourastier, J.; Gédouin, J.E.; Ropars, M.; Lambotte, J.C.; Thomazeau, H. Can rotation osteotomy remain effective for more than ten years? Orthop. Clin. N. Am. 2004, 35, 345–351. [Google Scholar] [CrossRef] [PubMed]
- Sakano, S.; Hasegawa, Y.; Torii, Y.; Kawasaki, M.; Ishiguro, N. Curved intertrochanteric varus osteotomy for osteonecrosis of the femoral head. J. Bone Jt. Surg. Br. Vol. 2004, 86-B, 359–365. [Google Scholar] [CrossRef] [PubMed]
- Drescher, W.; Fürst, M.; Hahne, H.J.; Helfenstein, A.; Petersen, W.; Hassenpflug, J. Survival analysis of hips treated with flexion osteotomy for femoral head necrosis. J. Bone Jt. Surg. Br. Vol. 2003, 85-B, 969–974. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Fuchs, B.; Knothe, U.; Hertel, R.; Ganz, R. Femoral osteotomy and iliac graft vascularization for femoral head osteonecrosis. Clin. Orthop. Relat. Res. 2003, 412, 84–93. [Google Scholar] [CrossRef]
- Pavlovčič, V.; Dolinar, D. Intertrochanteric osteotomy for osteonecrosis of the femoral head. Int. Orthop. 2002, 26, 238–242. [Google Scholar] [CrossRef][Green Version]
- Schneider, W.; Aigner, N.; Pinggera, O.; Knahr, K. Intertrochanteric osteotomy for avascular necrosis of the head of the femur. Survival probability of two different methods. J. Bone Jt. Surg. Br. Vol. 2002, 84, 817–824. [Google Scholar] [CrossRef]
- Gallinaro, P.; Massè, A. Flexion osteotomy in the treatment of avascular necrosis of the hip. Clin. Orthop. Relat. Res. 2001, 386, 79–84. [Google Scholar] [CrossRef]
- Koo, K.H.; Song, H.R.; Yang, J.W.; Yang, P.; Kim, J.R.; Kim, Y.M. Trochanteric rotational osteotomy for osteonecrosis of the femoral head. J. Bone Jt. Surg. Br. Vol. 2001, 83-B, 83–89. [Google Scholar] [CrossRef]
- Lengsfeld, M.; Schuler, P.; Griss, P. The long-term (8–12 years) results of valgus and lengthening osteotomy of the femoral neck. Arch. Orthop. Trauma Surg. 2001, 121, 201–204. [Google Scholar] [CrossRef] [PubMed]
- Nakai, T.; Masuhara, K.; Matsui, M.; Ohzono, K.; Ochi, T. Therapeutic effect of transtrochanteric rotational osteotomy and hip arthroplasty on quality of life of patients with osteonecrosis. Arch. Orthop. Trauma Surg. 2000, 120, 252–254. [Google Scholar] [CrossRef] [PubMed]
- Inao, S.; Ando, M.; Gotoh, E.; Matsuno, T. Minimum 10-year results of Sugioka’s osteotomy for femoral head osteonecrosis. Clin. Orthop. Relat. Res. 1999, 368, 141–148. [Google Scholar] [CrossRef]
- Atsumi, T.; Kuroki, Y. Modified Sugioka’s osteotomy: More than 130 degrees posterior rotation for osteonecrosis of the femoral head with large lesion. Clin. Orthop. Relat. Res. 1997, 334, 98–107. [Google Scholar] [CrossRef]
- Iwasada, S.; Hasegawa, Y.; Iwase, T.; Kitamura, S.; Iwata, H. Transtrochanteric rotational osteotomy for osteonecrosis of the femoral head. 43 patients followed for at least 3 years. Arch. Orthop. Trauma Surg. 1997, 116, 447–453. [Google Scholar] [CrossRef]
- Langlais, F.; Fourastier, J. Rotation osteotomies for osteonecrosis of the femoral head. Clin. Orthop. Relat. Res. 1997, 343, 110–123. [Google Scholar] [CrossRef]
- Mont, M.A.; Fairbank, A.C.; Krackow, K.A.; Hungerford, D.S. Corrective osteotomy for osteonecrosis of the femoral head. The Results of a Long-Term Follow-up Study*. J. Bone Jt. Surg. 1996, 78, 1032–1038. [Google Scholar] [CrossRef]
- Grigoris, P.; Safran, M.; Brown, I.; Amstutz, H.C. Long-term results of transtrochanteric rotational osteotomy for femoral head osteonecrosis. Arch. Orthop. Trauma Surg. 1996, 115, 127–130. [Google Scholar] [CrossRef]
- Dean, M.T.; Cabanela, M.E. Transtrochanteric anterior rotational osteotomy for avascular necrosis of the femoral head. Long-term results. J. Bone Jt. Surg. Br. Vol. 1993, 75-B, 597–601. [Google Scholar] [CrossRef]
- Sugano, N.; Takaoka, K.; Ohzono, K.; Matsui, M.; Saito, M.; Saito, S. Rotational osteotomy for non-traumatic avascular necrosis of the femoral head. J. Bone Jt. Surg. Br. Vol. 1992, 74-B, 734–739. [Google Scholar] [CrossRef] [PubMed]
- Sugioka, Y.; Hotokebuchi, T.; Tsutsui, H. Transtrochanteric anterior rotational osteotomy for idiopathic and steroid-induced necrosis of the femoral head. Indications and long-term results. Clin. Orthop. Relat. Res. 1992, 277, 111–120. [Google Scholar] [CrossRef]
- Melzer, C.; Boom, H.V.; Manz, P. Operative treatment of femoral head necrosis. Arch. Orthop. Trauma Surg. 1992, 111, 85–90. [Google Scholar] [CrossRef] [PubMed]
- Kinnard, P.; Lirette, R. The Borden and Gearen modification of the Sugioka transtrochanteric rotational osteotomy in avascular necrosis. A preliminary report. Clin. Orthop. Relat. Res. 1990, 255, 194–197. [Google Scholar] [CrossRef]
- Gottschalk, F. Indications and results of intertrochanteric osteotomy in osteonecrosis of the femoral head. Clin. Orthop. Relat. Res. 1989, 249, 219–222. [Google Scholar] [CrossRef]
- Jacobs, M.A.; Hungerford, D.S.; Krackow, K.A. Intertrochanteric osteotomy for avascular necrosis of the femoral head. J. Bone Jt. Surg. Br. Vol. 1989, 71-B, 200–204. [Google Scholar] [CrossRef]
- Maistrelli, G.; Fusco, U.; Avai, A.; Bombelli, R. Osteonecrosis of the hip treated by intertrochanteric osteotomy. A four- to 15-year follow-up. J. Bone Jt. Surg. Br. Vol. 1988, 70-B, 761–766. [Google Scholar] [CrossRef]
- Masuda, T.; Matsuno, T.; Hasegawa, I.; Kanno, T.; Ichioka, Y.; Kaneda, K. Results of transtrochanteric rotational osteotomy for nontraumatic osteonecrosis of the femoral head. Clin. Orthop. Relat. Res. 1988, 228, 69–74. [Google Scholar] [CrossRef]
- Saito, S.; Ohzono, K.; Ono, K. Joint-preserving operations for idiopathic avascular necrosis of the femoral head. Results of core decompression, grafting and osteotomy. J. Bone Jt. Surg. Br. Vol. 1988, 70-B, 78–84. [Google Scholar] [CrossRef]
- Eyb, R.; Kotz, R. The transtrochanteric anterior rotational osteotomy of Sugioka. Early and late results in idiopathic aseptic femoral head necrosis. Arch. Orthop. Trauma Surg. 1987, 106, 161–167. [Google Scholar] [CrossRef]
- Tooke, S.M.; Amstutz, H.C.; Hedley, A.K. Results of transtrochanteric rotational osteotomy for femoral head osteonecrosis. Clin. Orthop. Relat. Res. 1987, 224, 150–157. [Google Scholar] [CrossRef]
- Sugioka, Y. Transtrochanteric rotational osteotomy in the treatment of idiopathic and steroid-induced femoral head necrosis, Perthes’ disease, slipped capital femoral epiphysis, and osteoarthritis of the hip. Indications and results. Clin. Orthop. Relat. Res. 1984, 184, 12–23. [Google Scholar] [CrossRef]
- Imízcoz, J.L.; Villas, C.; Barredo, R.; Canadell, J. New plate for lateral translation in valgus intertrochanteric osteotomy (CUN plate). Arch. Orth. Traum. Surg. 1984, 103, 67–70. [Google Scholar] [CrossRef] [PubMed]
- Kotz, R. Avascular necrosis of the femoral head. A review of the indications and results of Sugioka’s transtrochanteric rotational osteotomy. Int. Orthop. 1981, 5, 53–58. [Google Scholar] [CrossRef] [PubMed]
- Mei, X.Y.; Gong, Y.J.; Safir, O.; Gross, A.; Kuzyk, P. Long-term outcomes of total hip arthroplasty in patients younger than 55 years: A systematic review of the contemporary literature. Can. J. Surg. 2019, 62, 249–258. [Google Scholar] [CrossRef]
- Karatas, M.E.; Kemah, B.; Soylemez, M.S.; Saglam, N. Mid-term survivorship and clinical results of cementless total hip arthroplasty for steroid-induced avascular necrosis. North. Clin. Istanb. 2024, 11, 219–224. [Google Scholar] [CrossRef]
- Salman, L.A.; Hantouly, A.T.; Khatkar, H.; Al-Ani, A.; Abudalou, A.; Al-Juboori, M.; Ahmed, G. The outcomes of total hip replacement in osteonecrosis versus osteoarthritis: A systematic review and meta-analysis. Int. Orthop. 2023, 47, 3043–3052. [Google Scholar] [CrossRef]
- Konarski, W.; Poboży, T.; Śliwczyński, A.; Kotela, I.; Krakowiak, J.; Hordowicz, M.; Kotela, A. Avascular Necrosis of Femoral Head—Overview and Current State of the Art. Int. J. Environ. Res. Public Heal. 2022, 19, 7348. [Google Scholar] [CrossRef]
- Simank, H.-G.; Brocai, D.R.C.; Brill, C.; Lukoschek, M. Comparison of results of core decompression and intertrochanteric osteotomy for nontraumatic osteonecrosis of the femoral head using Cox regression and survivorship analysis. J. Arthroplast. 2001, 16, 790–794. [Google Scholar] [CrossRef]
- Triangga, A.F.R.; Magetsari, R.; Muhammad, H.; Putra, S.P.; Fazatamma, D.A.; Saraswati, P.A.; Huwaidi, A.F. A systematic review and meta-analysis of hip preservation osteotomy in osteonecrosis of femoral head. Int. J. Surg. Open 2024, 62, 160–170. [Google Scholar] [CrossRef]
- Kim, C.; Linsenmeyer, K.D.; Vlad, S.C.; Guermazi, A.; Clancy, M.M.; Niu, J.; Felson, D.T. Prevalence of radiographic and symptomatic hip osteoarthritis in an urban United States community: The Framingham osteoarthritis study. Arthritis Rheumatol. 2014, 66, 3013–3017. [Google Scholar] [CrossRef]
- HARRIS, W.H. Traumatic Arthritis of the Hip after Dislocation and Acetabular Fractures: Treatment by Mold Arthroplasty. An end-result study using a new method of result evaluation. J Bone Jt. Surg. Am. 1969, 51, 737–755. [Google Scholar] [CrossRef]
- McLean, J.M.; Cappelletto, J.; Clarnette, J.; Hill, C.L.; Gill, T.; Mandziak, D.; Leith, J. Normal population reference values for the Oxford and Harris Hip Scores—Electronic data collection and its implications for clinical practice. HIP Int. 2016, 27, 389–396. [Google Scholar] [CrossRef] [PubMed]
- Leiss, F.; Götz, J.S.; Maderbacher, G.; Meyer, M.; Reinhard, J.; Zeman, F.; Grifka, J.; Greimel, F. Excellent Functional Outcome and Quality of Life after Primary Cementless Total Hip Arthroplasty (THA) Using an Enhanced Recovery Setup. J. Clin. Med. 2021, 10, 621. [Google Scholar] [CrossRef] [PubMed]
- Kalairajah, Y.; Azurza, K.; Hulme, C.; Molloy, S.; Drabu, K.J. Health Outcome Measures in the Evaluation of Total Hip Arthroplasties—A Comparison Between the Harris Hip Score and the Oxford Hip Score. J. Arthroplast. 2005, 20, 1037–1041. [Google Scholar] [CrossRef] [PubMed]
- Söderman, P.; Malchau, H.; Herberts, P.; Zügner, R.; Regnér, H.; Garellick, G. Outcome after total hip arthroplasty: Part II. Disease-specific follow-up and the Swedish National Total Hip Arthroplasty Register. Acta Orthop. 2001, 72, 113–119. [Google Scholar] [CrossRef]
- Costa, M.L.; Achten, J.; Parsons, N.R.; Edlin, R.P.; Foguet, P.; Prakash, U.; Griffin, D.R.; Young Adult Hip Arthroplasty Team. Total hip arthroplasty versus resurfacing arthroplasty in the treatment of patients with arthritis of the hip joint: Single centre, parallel group, assessor blinded, randomised controlled trial. BMJ 2012, 344, e2147. [Google Scholar] [CrossRef]
- Lombardi, A.V.; Byrd, Z.O.; Berend, K.R.; Morris, M.J.; Adams, J.B.; Crawford, D.A. Mid-Term Survival of Total Hip Arthroplasty in Patients Younger Than 55-year-old. J. Arthroplast. 2022, 37, S517–S523. [Google Scholar] [CrossRef]
- Achten, J.; Parsons, N.R.; Edlin, R.P.; Griffin, D.R.; Costa, M.L. A randomised controlled trial of total hip arthroplasty versus resurfacing arthroplasty in the treatment of young patients with arthritis of the hip joint. BMC Musculoskelet. Disord. 2010, 11, 8. [Google Scholar] [CrossRef]
- Osawa, Y.; Seki, T.; Okura, T.; Takegami, Y.; Ishiguro, N.; Hasegawa, Y. Curved Intertrochanteric Varus Osteotomy vs Total Hip Arthroplasty for Osteonecrosis of the Femoral Head in Patients Under 50 Years Old. J. Arthroplast. 2020, 35, 1600–1605. [Google Scholar] [CrossRef]
- Kang, Y.; Zhang, Z.; Zhao, X.; Zhang, Z.; Sheng, P.; Liao, W. Total hip arthroplasty for vascular necrosis of the femoral head in patients with systemic lupus erythematosus: A midterm follow-up study of 28 hips in 24 patients. Eur. J. Orthop. Surg. Traumatol. 2013, 23, 73–79. [Google Scholar] [CrossRef]
- Goh, E.L.; Boughton, O.R.; Donnelly, T.; Murphy, C.G.; Cashman, J.; Green, C. Do joint-preserving hip procedures compromise subsequent total hip arthroplasty? A meta-analysis of complications, functional outcome and survivorship. SICOT J. 2024, 10, 25. [Google Scholar] [CrossRef]
- Gallazzi, E.; Morelli, I.; Peretti, G.; Zagra, L. What Is the Impact of a Previous Femoral Osteotomy on THA? A Systematic Review. Clin. Orthop. Relat. Res. 2019, 477, 1176–1187. [Google Scholar] [CrossRef]
- Duncan, S.; Wingerter, S.; Keith, A.; Fowler, S.A.; Clohisy, J. Does Previous Osteotomy Compromise Total Hip Arthroplasty? A Systematic Review. J. Arthroplast. 2015, 30, 79–85. [Google Scholar] [CrossRef] [PubMed]



| Author | Year | Quality of Study | Risk of Bias |
|---|---|---|---|
| Kubo [16] | 2019 | Good | Low |
| Kawano [17] | 2018 | Good | Low |
| Kubo [18] | 2017 | Good | Low |
| Lee [19] | 2017 | Good | Low |
| Morita [20] | 2017 | Good | Low |
| Kubo [21] | 2016 | Good | Low |
| Okura [22] | 2016 | Good | Low |
| Sonoda [23] | 2015 | Fair | Moderate |
| Hamanishi [24] | 2014 | Fair | Moderate |
| Ito [25] | 2012 | Good | Low |
| Ha [26] | 2011 | Good | Low |
| Motomura [27] | 2010 | Good | Low |
| Biswal [28] | 2009 | Good | Low |
| Yoon [29] | 2008 | Good | Low |
| Sugioka [30] | 2008 | Good | Low |
| Seki [31] | 2008 | Fair | Moderate |
| Ikemura [32] | 2007 | Good | Low |
| Atsumi [33] | 2006 | Poor | High |
| Nakamura [34] | 2005 | Poor | High |
| Onodera [35] | 2005 | Fair | Moderate |
| Rijnen [36] | 2005 | Good | Low |
| Hisatome [37] | 2004 | Fair | Moderate |
| Langlais [38] | 2004 | Fair | Moderate |
| Sakano [39] | 2004 | Fair | Moderate |
| Drescher [40] | 2003 | Fair | Moderate |
| Fuchs [41] | 2003 | Fair | Moderate |
| Pavlovcic [42] | 2002 | Poor | High |
| Schneider [43] | 2002 | Fair | Moderate |
| Gallinaro [44] | 2001 | Poor | High |
| Koo [45] | 2001 | Good | Low |
| Lengsfeld [46] | 2001 | Fair | Moderate |
| Nakai [47] | 2000 | Poor | High |
| Inao [48] | 1999 | Fair | Moderate |
| Atsumi [49] | 1997 | Poor | High |
| Iwasada [50] | 1997 | Fair | Moderate |
| Langlais [51] | 1997 | Poor | High |
| Mont [52] | 1996 | Fair | Moderate |
| Grigoris [53] | 1995 | Fair | Moderate |
| Dean [54] | 1993 | Poor | High |
| Sugano [55] | 1992 | Fair | Moderate |
| Hotokebuchi [56] | 1992 | Poor | High |
| Melzer [57] | 1992 | Poor | High |
| Kinnard [58] | 1990 | Poor | High |
| Gottschalk [59] | 1989 | Poor | High |
| Jacobs [60] | 1989 | Poor | High |
| Maistrelli [61] | 1988 | Fair | Moderate |
| Masuda [62] | 1988 | Poor | High |
| Saito [63] | 1988 | Fair | Moderate |
| Eyb [64] | 1987 | Poor | High |
| Tooke [65] | 1987 | Fair | Moderate |
| Sugioka [66] | 1984 | Fair | Moderate |
| Imizcoz [67] | 1984 | Poor | High |
| Kotz [68] | 1981 | Poor | High |
| Aetiological Factor | N (%) |
|---|---|
| Steroid | 647 (34%) |
| Alcohol | 560 (29%) |
| Idiopathic | 407 (21%) |
| Trauma | 135 (7%) |
| Smoking | 54 (3%) |
| Hyperlipidemia | 49 (3%) |
| Pregnancy | 14 (<1%) |
| Congenital dislocation | 9 (<1%) |
| Perthes | 8 (<1%) |
| Heavy metal | 8 (<1%) |
| Fat embolism | 4 (<1%) |
| Caisson | 2 (<1%) |
| Systemic Lupus | 2 (<1%) |
| Diabetes | 2 (<1%) |
| Gout | 1 (<1%) |
| Radiation | 1 (<1%) |
| Gauchers | 1 (<1%) |
| Chemotherapy | 1 (<1%) |
| Classification (Number of Studies) | N (%) |
|---|---|
| Ficat (20) | |
| Stage 1 Stage 2 Stage 3 Stage 4 | 30 (4%) 287 (35%) 475 (58%) 24 (3%) |
| Japanese Investigation Committee of Health and Welfare (9) | |
| Stage 1 Stage 2 Stage 3 Stage 4 | 1 (<1%) 68 (20%) 260 (77%) 7 (2%) |
| Type A Type B Type C Type D | 41 (10%) 27 (7%) 339 (83%) 0 (0%) |
| ARCO (5) | |
| Stage 1 Stage 2 Stage 3 Stage 4 | 0 (0%) 25 (11%) 182 (80%) 21 (9%) |
| Steinburg (2) | |
| Stage 1 Stage 2 Stage 3 Stage 4 | 0 (0%) 42 (51%) 35 (42%) 6 (7%) |
| JOA Hip Score (2) | |
| Stage 1 Stage 2 Stage 3 Stage 4 | 1 (<1%) 115 (34%) 148 (44%) 72 (21%) |
| Merle d’Aubigiune (1) | |
| Stage 1 Stage 2 Stage 3 | 2 (13%) 13 (81%) 1 (6%) |
| Not Recorded (14) |
| Osteotomy Details | N (%) |
|---|---|
| Osteotomy type | |
| Rotation Flexion Varus Valgus Flexion + Varus Flexion + Valgus Rotation + Varus Rotation + Valgus | 1534 (64%) 41 (2%) 440 (18%) 150 (6%) 120 (5%) 32 (1%) 40 (2%) 32 (1%) |
| Fixation type | |
| Screws Sliding hip screw Blade plate | 952 (40%) 765 (32%) 672 (28%) |
| Complication | N (%) |
|---|---|
| Delayed union | 42 (19%) |
| Fracture | 40 (18%) |
| Fixation failure | 33 (15%) |
| Non-union | 32 (15%) |
| Deformity | 28 (13%) |
| Deep infection | 21 (10%) |
| DVT/PE | 8 (4%) |
| Haematoma | 6 (3%) |
| Nerve injury | 4 (2%) |
| Surgical site infection | 4 (2%) |
| Poor wound healing | 1 (<1%) |
| Heterotopic ossification | 1 (<1%) |
| PROM (Number of Studies; Hips) | Outcome |
|---|---|
| Harris Hip Score (16; 745) [16,18,20,22,23,25,28,29,30,34,36,39,40,52,58,61] | |
| Pre-op Post-op Average change | 58.3 84.4 26.1 |
| Merle d’Aubigne Numeric Score (7; 418) [19,24,26,37,44,55,63] | |
| Pre-op Post-op Average change | 12.8 15.1 2.3 |
| Merle d’Aubigne Outcome Rating (6; 137) [33,37,38,41,46,51] | |
| Excellent Good Fair Poor | 61 (45%) 35 (26%) 18 (13%) 23 (17%) |
| Oxford Hip Score (2; 115) [17,21] | |
| Post-op score | 37.3 |
| UCLA Activity Scale (1; 95) [17] | |
| Post-op score | 5 |
| Pain Catastrophizing Score (1; 95) [17] | |
| Post-op score | 43 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Rodham, P.L.; Jido, J.T.; Bethell, H.; Giannoudis, V.P.; Panteli, M.; Kanakaris, N.K.; Giannoudis, P.V. The Role of Proximal Femoral Osteotomy for the Treatment of Avascular Necrosis: A Systematic Review of Clinical and Patient-Reported Outcomes. J. Clin. Med. 2025, 14, 5592. https://doi.org/10.3390/jcm14155592
Rodham PL, Jido JT, Bethell H, Giannoudis VP, Panteli M, Kanakaris NK, Giannoudis PV. The Role of Proximal Femoral Osteotomy for the Treatment of Avascular Necrosis: A Systematic Review of Clinical and Patient-Reported Outcomes. Journal of Clinical Medicine. 2025; 14(15):5592. https://doi.org/10.3390/jcm14155592
Chicago/Turabian StyleRodham, Paul L., Jamila Tukur Jido, Hannah Bethell, Vasileios P. Giannoudis, Michalis Panteli, Nikolaos K. Kanakaris, and Peter V. Giannoudis. 2025. "The Role of Proximal Femoral Osteotomy for the Treatment of Avascular Necrosis: A Systematic Review of Clinical and Patient-Reported Outcomes" Journal of Clinical Medicine 14, no. 15: 5592. https://doi.org/10.3390/jcm14155592
APA StyleRodham, P. L., Jido, J. T., Bethell, H., Giannoudis, V. P., Panteli, M., Kanakaris, N. K., & Giannoudis, P. V. (2025). The Role of Proximal Femoral Osteotomy for the Treatment of Avascular Necrosis: A Systematic Review of Clinical and Patient-Reported Outcomes. Journal of Clinical Medicine, 14(15), 5592. https://doi.org/10.3390/jcm14155592









