Pulse Steroid Therapy for Severe Acute Respiratory Distress Syndrome: A Propensity Score-Matched Analysis
Abstract
1. Introduction
2. Materials and Methods
2.1. Setting
2.2. Data Collection
2.3. Patient Selection
2.4. Endpoints
2.5. Statistical Analysis
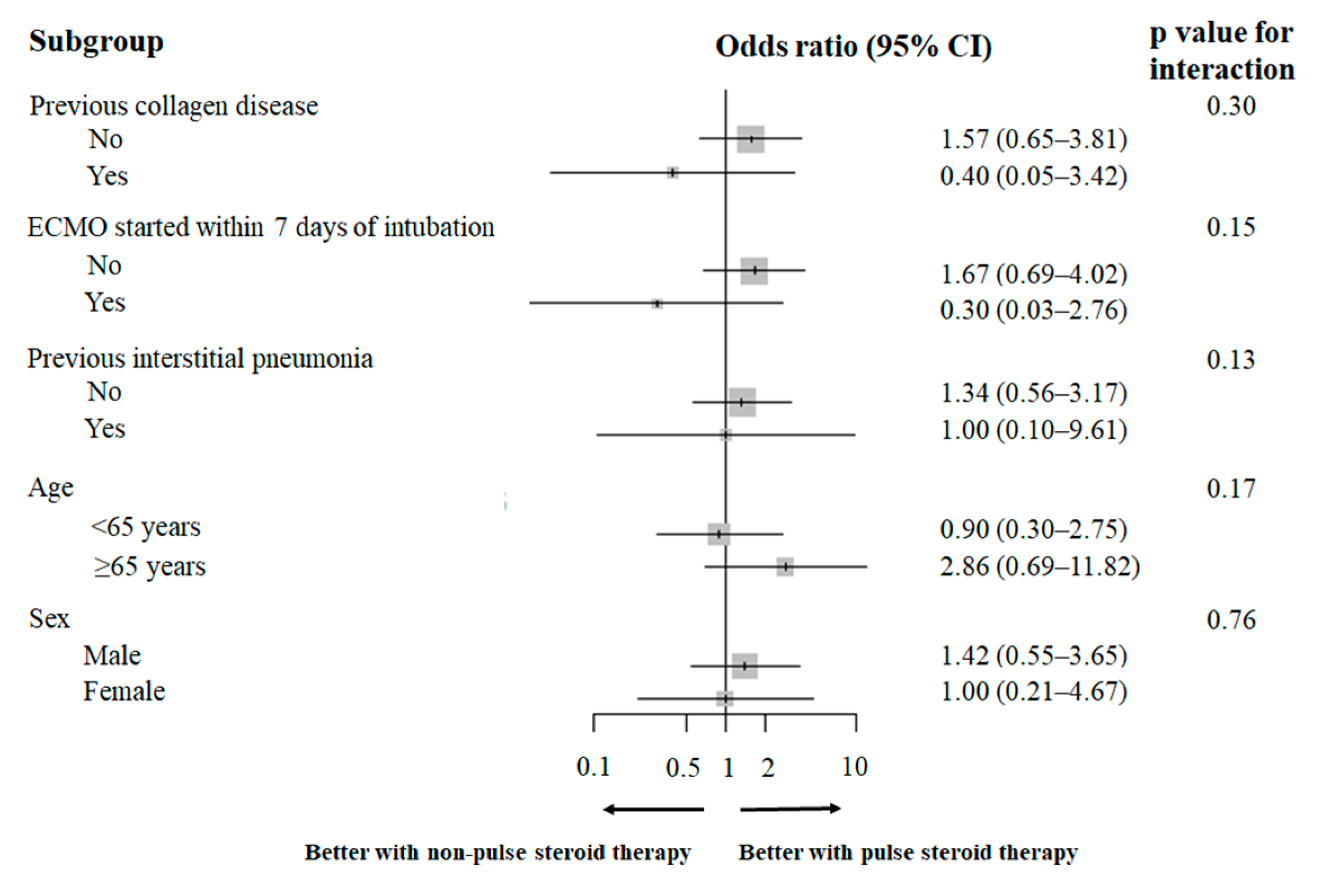
3. Results
3.1. Patients
3.2. Endpoints
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| ARDS | acute respiratory distress syndrome |
| BMI | body mass index |
| COVID-19 | coronavirus disease 2019 |
| COPD | chronic obstructive pulmonary disease |
| ECMO | extracorporeal membrane oxygenation |
| ECMOFDs | extracorporeal membrane oxygenation-free days |
| IQR | interquartile range |
| RESP | respiratory extracorporeal membrane oxygenation survival prediction |
| SOFA | Sequential Organ Failure Assessment |
| SD | standardized difference |
References
- Ranieri, V.M.; Rubenfeld, G.D.; Thompson, B.T.; Ferguson, N.D.; Caldwell, E.; Fan, E.; Camporota, L.; Slutsky, A.S. Acute respiratory distress syndrome: The Berlin Definition. JAMA 2012, 307, 2526–2533. [Google Scholar] [CrossRef] [PubMed]
- Bellani, G.; Laffey, J.G.; Pham, T.; Fan, E.; Brochard, L.; Esteban, A.; Gattinoni, L.; Van Haren, F.; Larsson, A.; McAuley, D.F.; et al. Epidemiology, patterns of care, and mortality for patients with acute respiratory distress syndrome in intensive care units in 50 countries. JAMA 2016, 315, 788–800. [Google Scholar] [CrossRef]
- Friedrichson, B.; Mutlak, H.; Zacharowski, K.; Piekarski, F. Insight into ECMO, mortality and ARDS: A nationwide analysis of 45,647 ECMO runs. Crit. Care 2021, 25, 38. [Google Scholar] [CrossRef]
- Ware, L.B.; Matthay, M.A. The acute respiratory distress syndrome. N. Engl. J. Med. 2000, 342, 1334–1349. [Google Scholar] [CrossRef]
- Briegel, J.; Jochum, M.; Gippner-Steppert, C.; Thiel, M. Immunomodulation in septic shock: Hydrocortisone differentially regulates cytokine responses. J. Am. Soc. Nephrol. 2001, 12 (Suppl. S17), S70–S74. [Google Scholar] [CrossRef]
- Kuperminc, E.; Heming, N.; Carlos, M.; Annane, D. Corticosteroids in ARDS. J. Clin. Med. 2023, 12, 3340. [Google Scholar] [CrossRef]
- Meduri, G.U.; Golden, E.; Freire, A.X.; Taylor, E.; Zaman, M.; Carson, S.J.; Gibson, M.; Umberger, R. Methylprednisolone infusion in early severe ARDS: Results of a randomized controlled trial. Chest 2007, 131, 954–963. [Google Scholar] [CrossRef]
- Villar, J.; Ferrando, C.; Martínez, D.; Ambrós, A.; Muñoz, T.; Soler, J.A.; Aguilar, G.; Alba, F.; González-Higueras, E.; Conesa, L.A.; et al. Dexamethasone treatment for the acute respiratory distress syndrome: A multicentre, randomised controlled trial. Lancet Respir. Med. 2020, 8, 267–276. [Google Scholar] [CrossRef] [PubMed]
- Sinha, A.; Bagga, A. Pulse steroid therapy. Indian. J. Pediatr. 2008, 75, 1057–1066. [Google Scholar] [CrossRef] [PubMed]
- Nishikimi, M.; Ohshimo, S.; Fukumoto, W.; Hamaguchi, J.; Matsumura, K.; Fujizuka, K.; Hagiwara, Y.; Nakayama, R.; Bunya, N.; Maruyama, J.; et al. Chest CT findings in severe acute respiratory distress syndrome requiring V-V ECMO: J-CARVE registry. J. Intensive Care 2024, 12, 5. [Google Scholar] [CrossRef]
- Vincent, J.L.; Moreno, R.; Takala, J.; Willatts, S.; De Mendonça, A.; Bruining, H.; Reinhart, C.K.; Suter, P.M.; Thijs, L.G. The SOFA (Sepsis-related Organ Failure Assessment) score to describe organ dysfunction/failure. On behalf of the Working Group on Sepsis-Related Problems of the European Society of Intensive Care Medicine. Intensive Care Med. 1996, 22, 707–710. [Google Scholar] [CrossRef]
- Schmidt, M.; Bailey, M.; Sheldrake, J.; Hodgson, C.; Aubron, C.; Rycus, P.T.; Scheinkestel, C.; Cooper, D.J.; Brodie, D.; Pellegrino, V.; et al. Predicting survival after extracorporeal membrane oxygenation for severe acute respiratory failure. The Respiratory Extracorporeal Membrane Oxygenation Survival Prediction (RESP) score. Am. J. Respir. Crit. Care Med. 2014, 189, 1374–1382. [Google Scholar] [CrossRef] [PubMed]
- Kanda, Y. Investigation of the freely available easy-to-use software ‘EZR’ for medical statistics. Bone Marrow Transpl. 2013, 48, 452–458. [Google Scholar] [CrossRef]
- Ewald, H.; Raatz, H.; Boscacci, R.; Furrer, H.; Bucher, H.C.; Briel, M. Adjunctive corticosteroids for Pneumocystis jiroveci pneumonia in patients with HIV infection. Cochrane Database Syst. Rev. 2015, 2015, CD006150. [Google Scholar] [CrossRef]
- Bradley, B.; Branley, H.M.; Egan, J.J.; Greaves, M.S.; Hansell, D.M.; Harrison, N.K.; Hirani, N.; Hubbard, R.; Lake, F.; Millar, A.B.; et al. Interstitial lung disease guideline: The British Thoracic Society in collaboration with the Thoracic Society of Australia and New Zealand and the Irish Thoracic Society. Thorax 2008, 63 (Suppl. S5), v1–v58. [Google Scholar] [CrossRef] [PubMed]
- Allen, J. Acute eosinophilic pneumonia. Semin. Respir. Crit. Care Med. 2006, 27, 142–147. [Google Scholar] [CrossRef] [PubMed]
- Marie, I.; Hachulla, E.; Chérin, P.; Dominique, S.; Hatron, P.Y.; Hellot, M.F.; Devulder, B.; Herson, S.; Levesque, H.; Courtois, H. Interstitial lung disease in polymyositis and dermatomyositis. Arthritis Rheum. 2002, 47, 614–622. [Google Scholar] [CrossRef]
- RECOVERY Collaborative Group; Horby, P.; Lim, W.S.; Emberson, J.R.; Mafham, M.; Bell, J.L.; Linsell, L.; Staplin, N.; Brightling, C.; Ustianowski, A.; et al. Dexamethasone in hospitalized patients with COVID-19. N. Engl. J. Med. 2021, 384, 693–704. [Google Scholar] [CrossRef]
- De Pascale, G.; Bello, G.; Dell’Anna, A.M.; Montini, L.; Antonelli, M.; Moreno, G.; Rodriguez, A.; Martin-Loeches, I. Steroids and severe pneumonia. Ready for the winter? Discussion on “Corticosteroid treatment in critically ill patients with severe influenza pneumonia: A propensity score matching study”. Intensive Care Med. 2018, 44, 2319–2320. [Google Scholar] [CrossRef]
- Meduri, G.U.; Shih, M.C.; Bridges, L.; Martin, T.J.; El-Solh, A.; Seam, N.; Davis-Karim, A.; Umberger, R.; Anzueto, A.; Sriram, P.; et al. Low-dose methylprednisolone treatment in critically ill patients with severe community-acquired pneumonia. Intensive Care Med. 2022, 48, 1009–1023. [Google Scholar] [CrossRef]
- Ak, A.K.; Mantri, S.N. Lymphangitic Carcinomatosis; StatPearls: Treasure Island, FL, USA, 2024. [Google Scholar]
- Akasaka, K.; Tanaka, T.; Kitamura, N.; Ohkouchi, S.; Tazawa, R.; Takada, T.; Ichiwata, T.; Yamaguchi, E.; Hirose, M.; Arai, T.; et al. Outcome of corticosteroid administration in autoimmune pulmonary alveolar proteinosis: A retrospective cohort study. BMC Pulm. Med. 2015, 15, 88. [Google Scholar] [CrossRef]
- Shekar, K.; Roberts, J.A.; Mullany, D.V.; Corley, A.; Fisquet, S.; Bull, T.N.; Barnett, A.G.; Fraser, J.F. Increased sedation requirements in patients receiving extracorporeal membrane oxygenation for respiratory and cardiorespiratory failure. Anaesth. Intensive Care 2012, 40, 648–655. [Google Scholar] [CrossRef] [PubMed]
- Patel, J.S.; Kooda, K.; Igneri, L.A. A narrative review of the impact of extracorporeal membrane oxygenation on the pharmacokinetics and pharmacodynamics of critical care therapies. Ann. Pharmacother. 2023, 57, 706–726. [Google Scholar] [CrossRef] [PubMed]
- Begg, E.J.; Atkinson, H.C.; Gianarakis, N. The pharmacokinetics of corticosteroid agents. Med. J. Aust. 1987, 146, 37–41. [Google Scholar] [CrossRef] [PubMed]
- Yasir, M.; Goyal, A.; Sonthalia, S. Corticosteroid Adverse Effects; StatPearls: Treasure Island, FL, USA, 2024. [Google Scholar]
- Teijeiro-Paradis, R.; Gannon, W.D.; Fan, E. Complications associated with venovenous extracorporeal membrane oxygenation-what can go wrong. Crit. Care Med. 2022, 50, 1809–1818. [Google Scholar] [CrossRef]

| Variables | Unmatched Group | Matched Group | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| All Patients (n = 373) | Non-Pulse (n = 317) | Pulse (n = 56) | SD | p Value | All Patients (n = 96) | Non-Pulse (n = 48) | Pulse (n = 48) | SD | p Value | |
| Demographic factors and severity of illness | ||||||||||
| Age, median (IQR), years | 60 (51–67) | 60 (51–67) | 62.5 (52–67) | 0.06 | 0.711 | 62 (48.8–69.3) | 57 (45.8–70.3) | 63 (53.8–67.0) | 0.134 | 0.610 |
| male sex, n (%) | 283 (75.9) | 245 (77.3) | 38 (67.9) | 0.213 | 0.131 | 70 (72.9) | 35 (72.9) | 35 (72.9) | <0.001 | 1.000 |
| BMI, median (IQR) | 26 (22.8–30.5) | 26.2 (23.2–31.1) | 24.2 (21.5–27.0) | 0.461 | 0.002 | 24.6 (22.2–28.0) | 25.1 (21.4–28.3) | 24.6 (22.4–27.0) | 0.134 | 0.674 |
| Causes of ARDS, n (%) | 1.243 | - | 0.368 | 0.871 | ||||||
| COVID-19 | 217 (58.2) | 207 (65.3) | 10 (17.9) | 20 (20.8) | 10 (20.8) | 10 (20.8) | ||||
| Bacterial | 45 (12) | 31 (9.8) | 14 (25) | 23 (24) | 11 (22.9) | 12 (25.0) | ||||
| Extra-pulmonary | 20 (5.4) | 18 (5.7) | 2 (3.6) | 6 (6.3) | 4 (8.3) | 2 (4.2) | ||||
| Influenza | 10 (2.7) | 8 (2.5) | 2 (3.6) | 3 (3.1) | 1 (2.1) | 2 (4.2) | ||||
| Legionnaires | 5 (1.3) | 5 (1.6) | 0 (0) | 0 (0.0) | 0 (0) | 0 (0) | ||||
| Aspiration pneumonitis | 4 (1) | 3 (0.9) | 1 (1.8) | 2 (2.1) | 1 (2.1) | 1 (2.1) | ||||
| Trauma | 4 (1) | 3 (0.9) | 1 (1.8) | 2 (2.1) | 2 (4.2) | 0 (0.0) | ||||
| Drowning | 1 (4) | 1 (0.3) | 0 (0) | 0 (0.0) | 0 (0) | 0 (0.0) | ||||
| Unknown | 67 (18) | 41 (12.9) | 26 (46.4) | 40 (41.7) | 19 (39.6) | 21 (43.8) | ||||
| SOFA score, median (IQR) | 10 (8–12) | 9 (7–12) | 11 (8–12) | 0.273 | 0.042 | 11 (8–13) | 11 (8–13) | 11 (8–12) | 0.1 | 0.737 |
| RESP score, median (IQR) | 3 (1–4) | 3 (1–4) | 2 (0–4) | 0.111 | 0.300 | 2 (0–4) | 2 (0–4) | 2 (0–4) | 0.22 | 0.408 |
| Murray lung injury score, median (IQR) | 13 (11–14) | 13 (11–14) | 13 (11–14) | 0.023 | 0.888 | 13 (11–14) | 13 (11–14) | 13 (11–14) | 0.047 | 0.673 |
| Intubation to ECMO start <7 days, n (%) | 310 (83.1) | 262 (82.6) | 48 (85.7) | 0.084 | 0.700 | 82 (85.4) | 42 (87.5) | 40 (83.3) | 0.118 | 0.770 |
| Neuromuscular blockers use before ECMO start, n (%) | 177 (47.5) | 153 (48.3) | 24 (42.9) | 0.109 | 0.472 | 39 (40.6) | 21 (43.8) | 18 (37.5) | 0.128 | 0.678 |
| Prone therapy before ECMO start, n (%) | 83 (22.3) | 79 (24.9) | 4 (7.1) | 0.499 | 0.003 | 7 (7.3) | 3 (6.2) | 4 (8.3) | 0.08 | 1.000 |
| Comorbidities, n (%) | ||||||||||
| Diabetes mellitus | 106 (28.4) | 94 (29.7) | 12 (21.4) | 0.189 | 0.261 | 19 (19.8) | 8 (16.7) | 11 (22.9) | 0.157 | 0.609 |
| Chronic kidney disease | 32 (8.6) | 27 (8.5) | 5 (8.9) | 0.015 | 1.000 | 7 (7.3) | 3 (6.2) | 4 (8.3) | 0.08 | 1.000 |
| Cerebrovascular accident | 32 (8.6) | 25 (7.9) | 5 (8.9) | 0.038 | 0.790 | 10 (10.4) | 5 (10.4) | 5 (10.4) | <0.001 | 1.000 |
| Asthma | 27 (7.2) | 22 (6.9) | 5 (8.9) | 0.074 | 0.578 | 8 (8.3) | 5 (10.4) | 3 (6.2) | 0.151 | 0.714 |
| COPD | 24 (6.4) | 20 (6.3) | 4 (7.1) | 0.033 | 0.770 | 5 (5.2) | 1 (2.1) | 4 (8.3) | 0.284 | 0.362 |
| Collagen disease | 29 (7.8) | 19 (6.0) | 10 (17.9) | 0.372 | 0.005 | 15 (15.6) | 8 (16.7) | 7 (14.6) | 0.057 | 1.000 |
| Ischemic heart disease | 21 (5.6) | 18 (5.7) | 3 (5.4) | 0.014 | 1.000 | 5 (5.2) | 2 (4.2) | 3 (6.2) | 0.09 | 1.000 |
| Interstitial pneumonia | 22 (5.9) | 15 (4.7) | 7 (12.5) | 0.28 | 0.032 | 12 (12.5) | 6 (12.5) | 6 (12.5) | <0.001 | 1.000 |
| Chronic heart failure | 15 (4) | 12 (3.8) | 3 (5.4) | 0.075 | 0.480 | 3 (3.1) | 0 (0) | 3 (6.2) | 0.365 | 0.242 |
| Lung cancer | 8 (2.1) | 7 (2.2) | 1 (1.8) | 0.03 | 1.000 | 3 (3.1) | 2 (4.2) | 1 (2.1) | 0.12 | 1.000 |
| Cirrhosis | 7 (1.9) | 3 (0.9) | 4 (7.1) | 0.319 | 0.011 | 4 (4.2) | 0 (0) | 4 (8.3) | 0.426 | 0.117 |
| Variables | Unmatched Group | Matched Group | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| All Patients (n = 373) | Non-Pulse (n = 317) | Pulse (n = 56) | SD | p Value | All Patients (n = 96) | Non-Pulse (n = 48) | Pulse (n = 48) | SD | p Value | |
| Laboratory data at ICU admission, median (IQR) | ||||||||||
| WBC, 109/L | 11.8 (8.3–17) | 11.7 (8.2–16.1) | 12.5 (9.5–19.8) | 0.221 | 0.111 | 13.6 (10.4–20.2) | 14.9 (11.5–20.8) | 12.5 (10.3–20.0) | 0.093 | 0.450 |
| Platelet count, 109/L | 190 (121–264) | 189 (126–260) | 192 (104–284) | 0.117 | 0.787 | 190 (105–281) | 161 (102–251) | 198 (123–288) | 0.22 | 0.206 |
| CRP, mg/dL | 10.6 (4.3–19) | 10.4 (4.2–18.4) | 12.4 (4.8–21.1) | 0.185 | 0.233 | 12.2 (6.0–20.6) | 10.9 (6.1–20.2) | 12.5 (5.6–20.7) | 0.022 | 0.826 |
| D-dimer, μg/mL | 5.9 (2.5–16) | 5.5 (2.3–15.3) | 9.6 (4.3–32.1) | 0.115 | 0.028 | 8.5 (3.8–30.1) | 7.9 (3.4–26.1) | 9.4 (4.2–33.8) | 0.17 | 0.575 |
| Arterial gas data before starting ECMO | ||||||||||
| pH | 7.32 (7.22–7.39) | 7.33 (7.23–7.39) | 7.3 (7.2–7.4) | 0.017 | 0.777 | 7.32 (7.21–7.39) | 7.32 (7.23–7.38) | 7.31 (7.21–7.39) | 0.061 | 0.834 |
| PaO2, mmHg | 72.9 (60–89.6) | 72.9 (60–87.5) | 73 (59.5–90.4) | 0.029 | 0.954 | 69.8 (59.0–91.1) | 70.4 (58.7–93.3) | 69.6 (60.0–89.8) | 0.022 | 0.783 |
| PaCO2, mmHg | 50 (41–64.5) | 50 (41–63) | 49.2 (41–64.6) | 0.084 | 0.887 | 49.4 (41.0–64.6) | 49.0 (41.0–62.4) | 50.1 (40.8–65.1) | 0.163 | 0.703 |
| HCO3−, mmol/L | 26 (22.1–29) | 26 (22–29) | 26 (22.8–30.6) | 0.093 | 0.528 | 25.7 (22.4–30.2) | 25.0 (21.3–29.0) | 26.0 (22.7–31.0) | 0.205 | 0.234 |
| Other therapeutic intervention, n (%) | ||||||||||
| Steroid therapy | 3.053 | - | 2.944 | <0.001 | ||||||
| Dexamethasone | 173 (46.4) | 173 (54.6) | 0 (0) | 13 (13.5) | 13 (27.1) | 0 (0) | ||||
| Methylprednisolone | 112 (30) | 56 (17.7) | 56 (100) | 57 (59.4) | 9 (18.8) | 48 (100) | ||||
| Hydrocortisone | 31 (8.3) | 41 (12.9) | 0 (0) | 13 (13.5) | 13 (27.1) | 0 (0) | ||||
| Prednisolone | 37 (9.9) | 37 (11.7) | 0 (0) | 12 (12.5) | 12 (25.0) | 0 (0) | ||||
| Betamethasone | 10 (2.7) | 10 (3.2) | 0 (0) | 1 (1.0) | 1 (2.1) | 0 (0) | ||||
| RRT | 139 (37.3) | 118 (37.2) | 21 (37.5) | 0.006 | 1.000 | 40 (41.7) | 24 (50.0) | 16 (33.3) | 0.343 | 0.147 |
| Prone therapy | 137 (36.7) | 127 (40.1) | 10 (17.9) | 0.505 | 0.001 | 18 (18.8) | 11 (22.9) | 7 (14.6) | 0.215 | 0.433 |
| Neuromuscular blockers use | 237 (63.5) | 206 (65) | 31 (55.4) | 0.198 | 0.178 | 58 (60.4) | 32 (66.7) | 26 (54.2) | 0.258 | 0.297 |
| Drug Name | Number (%) | Dose (mg) |
|---|---|---|
| Hydrocortisone | 13 (27.1) | |
| 8 | 200 | |
| 2 | 300 | |
| 1 | 100 | |
| 1 | 60 | |
| 1 | 44 | |
| Dexamethasone | 13 (27.1) | |
| 7 | 6.6 | |
| 3 | 20 | |
| 2 | 7 | |
| 1 | 6 | |
| Prednisolone | 12 (25.0) | |
| 3 | 80 | |
| 3 | 60 | |
| 2 | 30 | |
| 1 | 90 | |
| 1 | 70 | |
| 1 | 40 | |
| 1 | 20 | |
| Methylprednisolone | 9 (18.8) | |
| 3 | 80 | |
| 2 | 40 | |
| 1 | 500 | |
| 1 | 160 | |
| 1 | 88 | |
| 1 | 50 | |
| Betamethasone | 1 (2.0) | |
| 1 | 16 |
| Variable | Unmatched Group | Matched Group | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Non-Pulse (n = 317) | Pulse (n = 56) | OR | 95%CI | p Value | Non-Pulse (n = 48) | Pulse (n = 48) | OR | 95%CI | p Value | |
| All-cause hospital mortality, n (%) | 109 (34.4) | 23 (41.1) | 0.75 | 0.41–1.41 | 0.36 | 23 (47.9) | 20 (41.7) | 1.28 | 0.53–3.12 | 0.68 |
| ECMOFDs on 28 days, median (IQR), days | 15 (0–20) | 11 (0–18) | 0.24 | 3 (0–17) | 9.5 (0–17.3) | 0.69 | ||||
| Adverse events | ||||||||||
| Blood culture positive, n (%) | 99 (31.2) | 5 (8.9) | 0.22 | 0.07–0.56 | <0.001 | 11 (22.9) | 5 (10.4) | 0.39 | 0.09–1.37 | 0.17 |
| Intracranial bleeding, n (%) | 10 (3.2) | 1 (1.8) | 0.56 | 0.01–4.07 | 1 | 2 (4.2) | 1 (2.1) | 0.49 | 0.01–9.77 | 1 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kawano, Y.; Maruyama, J.; Nishikimi, M.; Arima, H.; Irie, Y.; Morimoto, S.; Muranishi, K.; Nakashio, M.; Nakamura, Y. Pulse Steroid Therapy for Severe Acute Respiratory Distress Syndrome: A Propensity Score-Matched Analysis. J. Clin. Med. 2025, 14, 5547. https://doi.org/10.3390/jcm14155547
Kawano Y, Maruyama J, Nishikimi M, Arima H, Irie Y, Morimoto S, Muranishi K, Nakashio M, Nakamura Y. Pulse Steroid Therapy for Severe Acute Respiratory Distress Syndrome: A Propensity Score-Matched Analysis. Journal of Clinical Medicine. 2025; 14(15):5547. https://doi.org/10.3390/jcm14155547
Chicago/Turabian StyleKawano, Yasumasa, Junichi Maruyama, Mitsuaki Nishikimi, Hisatomi Arima, Yuhei Irie, Shinichi Morimoto, Kentaro Muranishi, Maiko Nakashio, and Yoshihiko Nakamura. 2025. "Pulse Steroid Therapy for Severe Acute Respiratory Distress Syndrome: A Propensity Score-Matched Analysis" Journal of Clinical Medicine 14, no. 15: 5547. https://doi.org/10.3390/jcm14155547
APA StyleKawano, Y., Maruyama, J., Nishikimi, M., Arima, H., Irie, Y., Morimoto, S., Muranishi, K., Nakashio, M., & Nakamura, Y. (2025). Pulse Steroid Therapy for Severe Acute Respiratory Distress Syndrome: A Propensity Score-Matched Analysis. Journal of Clinical Medicine, 14(15), 5547. https://doi.org/10.3390/jcm14155547






