High Sensitive Cardiac Troponin-I (Hs-cTnI) Levels in Asymptomatic Hemodialysis Patients †
Abstract
1. Introduction
2. Methods
2.1. Study Population
2.2. Clinical Data and Study Outcome
2.3. Patients Follow-Up
2.4. Statement of Ethics
2.5. Statistical Analysis
3. Results
3.1. Dialysis Characteristics
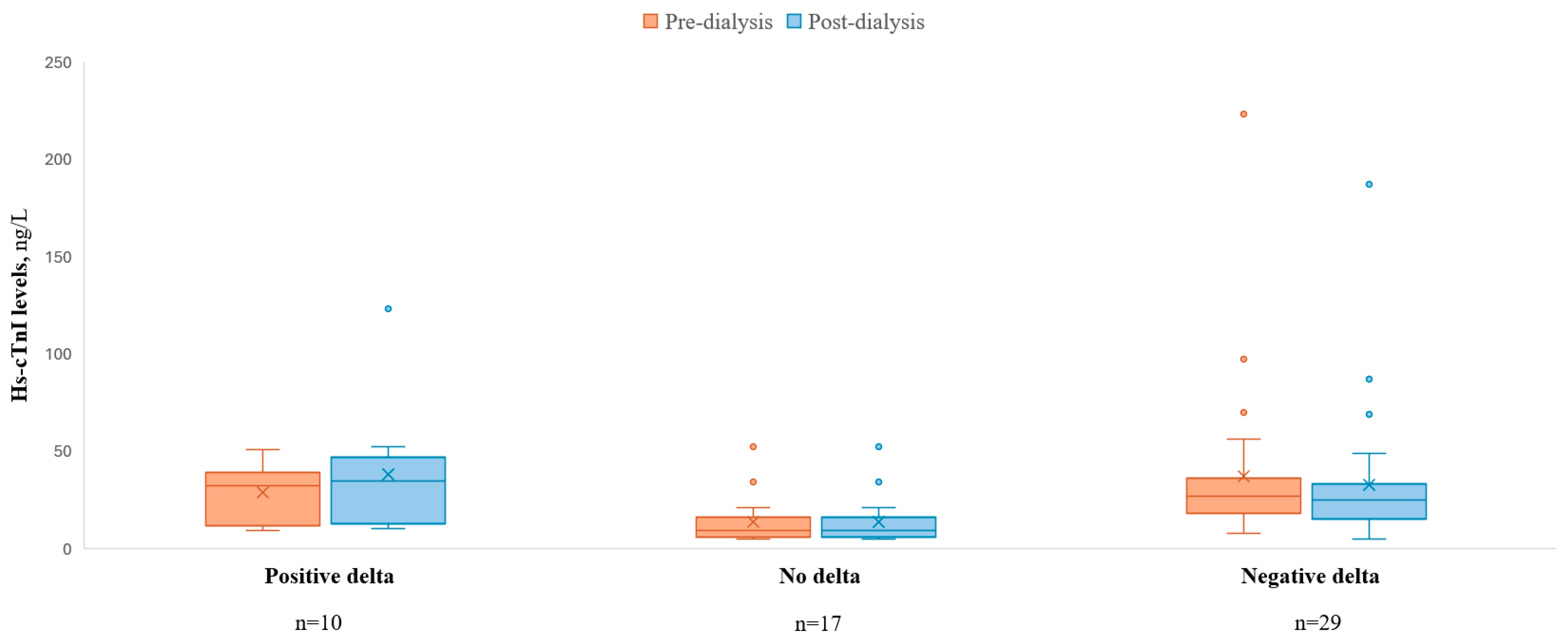
3.2. Hs-cTnI Levels
3.3. Hs-cTnI and “Gray Zone” Levels
3.4. Outcomes
4. Discussion
4.1. Baseline hs-TnI Level in Hemodialysis Patients
4.2. Hemodialysis Effect on the hs-TnI Levels
4.3. Clinical Associations
4.4. Diagnostic Challenges
4.5. Study Limitations
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Thygesen, K.; Alpert, J.S.; Jaffe, A.S.; Chaitman, B.R.; Bax, J.J.; Morrow, D.A.; White, H.D. Fourth Universal Definition of Myocardial Infarction. Circulation 2018, 138, e618–e651. [Google Scholar] [CrossRef]
- Krintus, M.; Kozinski, M.; Boudry, P.; Capell, N.E.; Köller, U.; Lackner, K.; Lefèvre, G.; Lennartz, L.; Lotz, J.; Herranz, A.M.; et al. European multicenter analytical evaluation of the Abbott ARCHITECT STAT high sensitive troponin i immunoassay. Clin. Chem. Lab. Med. 2014, 52, 1657–1665. [Google Scholar] [CrossRef]
- Tarapan, T.; Musikatavorn, K.; Phairatwet, P.; Takkavatakarn, K.; Susantitaphong, P.; Eiam-Ong, S.; Tiranathanagul, K. High sensitivity Troponin-I levels in asymptomatic hemodialysis patients. Ren. Fail. 2019, 41, 393–400. [Google Scholar] [CrossRef]
- Wongcharoen, W.; Chombandit, T.; Phrommintikul, A.; Noppakun, K. Variability of high-sensitivity cardiac troponin T and I in asymptomatic patients receiving hemodialysis. Sci. Rep. 2021, 11, 17334. [Google Scholar] [CrossRef]
- Lim, E.; Lee, M.-J. Optimal cut-off value of high-sensitivity troponin i in diagnosing myocardial infarction in patients with end-stage renal disease. Medicine 2020, 99, E18580. [Google Scholar] [CrossRef]
- Jakubiak, G.K. Cardiac Troponin Serum Concentration Measurement Is Useful Not Only in the Diagnosis of Acute Cardiovascular Events. J. Pers. Med. 2024, 14, 230. [Google Scholar] [CrossRef] [PubMed]
- Kampmann, J.D.; Hunderup, M.M.; Petersen, E.R.B.; Andersen, V.; Skovsted, T.A. Skovsted, High-sensitive troponin T, suPAR and Beta-2-microglobulin changes in concentration during hemodialysis. Scand. J. Clin. Lab. Investig. 2024, 84, 362–368. [Google Scholar] [CrossRef] [PubMed]
- Kampmann, J.; Heaf, J.; Mogensen, C.B.; Pedersen, A.K.; Granhøj, J.; Mickley, H.; Brandt, F. Troponin Cut-Offs for Acute Myocardial Infarction in Patients with Impaired Renal Function—A Systematic Review and Meta-Analysis. Diagnostics 2022, 12, 276. [Google Scholar] [CrossRef]
- Snaedal, S.; Bárány, P.; Lund, S.H.; Qureshi, A.R.; Heimbürger, O.; Stenvinkel, P.; Löwbeer, C.; Szummer, K. High-sensitivity troponins in dialysis patients: Variation and prognostic value. Clin. Kidney J. 2021, 14, 1789–1797. [Google Scholar] [CrossRef] [PubMed]
- Kalaji, F.; Albitar, S. Predictive value of cardiac troponin T and I in hemodialysis patients. Saudi J. Kidney Dis. Transplant. 2012, 23, 939–945. [Google Scholar] [CrossRef]
- Skadberg, Ø.; Sandberg, S.; Røraas, T.; Petersen, P.H.; Sellevoll, H.; Svarstad, E.; Sæle, K.; Aakre, K.M. The variation in high sensitive cardiac troponin concentration during haemodialysis treatment is not similar to the biological variation observed in stable end stage renal disease patients. Scand. J. Clin. Lab. Investig. 2016, 76, 645–652. [Google Scholar] [CrossRef]
- Kumar, N.; Michelis, M.F.; DeVita, M.V.; Panagopoulos, G.; Rosenstock, J.L. Troponin I levels in asymptomatic patients on haemodialysis using a high-sensitivity assay. Nephrol. Dial. Transplant. 2011, 26, 665–670. [Google Scholar] [CrossRef] [PubMed]
- Assa, S.; Gansevoort, R.T.; Westerhuis, R.; Kobold, A.C.M.; Voors, A.A.; de Jong, P.E.; Bakker, S.J.L.; Franssen, C.F.M. Determinants and prognostic significance of an intra-dialysis rise of cardiac troponin I measured by sensitive assay in hemodialysis patients. Clin. Res. Cardiol. 2013, 102, 439–445. [Google Scholar] [CrossRef] [PubMed]
- Hasselbalch, R.B.; Alaour, B.; Kristensen, J.H.; Couch, L.S.; Kaier, T.E.; Nielsen, T.L.; Plesner, L.L.; Strandkjær, N.; Schou, M.; Rydahl, C.; et al. Hemodialysis and biomarkers of myocardial infarction a cohort study. Clin. Chem. Lab. Med. 2024, 62, 361–370. [Google Scholar] [CrossRef]
- Byrne, R.A.; Rossello, X.; Coughlan, J.J.; Barbato, E.; Berry, C.; Chieffo, A.; Claeys, M.J.; Dan, G.-A.; Dweck, M.R.; Galbraith, M.; et al. 2023 ESC Guidelines for the management of acute coronary syndromes. Eur. Heart J. 2023, 38, 3720–3826. [Google Scholar] [CrossRef]
- Januzzi, J.L.; Mahler, S.A.; Christenson, R.H.; Rymer, J.; Newby, L.K.; Body, R.; Morrow, D.A.; Jaffe, A.S. Recommendations for Institutions Transitioning to High-Sensitivity Troponin Testing: JACC Scientific Expert Panel. J. Am. Coll. Cardiol. 2019, 73, 1059–1077. [Google Scholar] [CrossRef]
- Xie, J.; Xie, J.; Xie, D.; Long, X. Left ventricular remodeling and its correlation with serum cardiac troponin I in patients with end-stage renal disease treated. Int. J. Artif. Organs 2024, 47, 380–387. [Google Scholar] [CrossRef] [PubMed]
- Ibrahim, L.; Yasin, K.; Abbas, L.; Ismael, Y.; Mousa, A.; Alkarajeh, M.; Hamdan, Z.; Nazzal, Z.; Sethi, Y. Exploring the relation between Interleukin-6 and high-sensitive cardiac troponin T in asymptomatic hemodialysis patient: A cross-sectional study. PLoS ONE 2024, 19, e0296965. [Google Scholar] [CrossRef]
- Löwbeer, C.; Stenvinkel, P.; Pecoits-Filho, R.; Heimbürger, O.; Lindholm, B.; Gustafsson, S.A.; Seeberger, A. Elevated cardiac troponin T in predialysis patients is associated with inflammation and predicts mortality. J. Intern. Med. 2003, 253, 153–160. [Google Scholar] [CrossRef]
- Kolland, M.; Amenitsch, J.; Schreiber, N.; Ginthör, N.; Schuller, M.; Riedl, R.; Rainer, P.P.; Schneditz, D.; Niedrist, T.; Eller, K.; et al. Changes in Cardiac Troponins During Hemodialysis Depend on Hemodialysis Membrane and Modality: A Randomized Crossover Trial; Oxford University Press: Oxford, UK, 2024. [Google Scholar] [CrossRef]
- Buchanan, C.; Mohammed, A.; Cox, E.; Köhler, K.; Canaud, B.; Taal, M.W.; Selby, N.M.; Francis, S.; McIntyre, C.W. Intradialytic cardiac magnetic resonance imaging to assess cardiovascular responses in a short-term trial of hemodiafiltration and hemodialysis. J. Am. Soc. Nephrol. 2017, 28, 1269–1277. [Google Scholar] [CrossRef]
- Ahn, S.; Kim, H.-K.; Lee, W.; Chun, S.; Min, W.-K. Effect of Outlier Elimination on the 99th Percentile Upper Reference Limits of High-Sensitivity Cardiac Troponin I Assays Based on a Strictly Selected Healthy Reference Population. Ann. Lab. Med. 2022, 42, 331–341. [Google Scholar] [CrossRef] [PubMed]
- Ji, M.; Moon, H.-W.; Hur, M.; Yun, Y.-M. Determination of high-sensitivity cardiac troponin I 99th percentile upper reference limits in a healthy Korean population. Clin. Biochem. 2016, 49, 10–11. [Google Scholar] [CrossRef] [PubMed]
- He, B.; Wang, K.; Xu, P.; Zhou, Q.; Xu, J. Determination of Age-And Sex-Specific 99th Percentile Upper Reference Limits for High-Sensitivity Cardiac Troponin I in Healthy Chinese Adults. Cardiology 2022, 147, 261–270. [Google Scholar] [CrossRef] [PubMed]
- Silva, R.E.; Santos, E.C.; Justino, P.B.; Santos, M.P.; Galdino, G.; Gonçalves, R.V.; Novaes, R.D. Cytokines and chemokines systemic levels are related to dialysis adequacy and creatinine clearance in patients with end-stage renal disease undergoing hemodialysis. Int. Immunopharmacol. 2021, 100, 108154. [Google Scholar] [CrossRef]
- Iwamura, N.; Kidoguchi, S.; Asahi, N.; Takeda, I.; Matsuta, K.; Miyagi, K.; Iwano, M.; Miyazaki, R.; Kimura, H. Superiority of high sensitivity cardiac troponin I over NT-proBNP and adiponectin for 7-year mortality in stable patients receiving haemodialysis. Sci. Rep. 2024, 14, 11488. [Google Scholar] [CrossRef]
- Chen, M.; Gerson, H.; Eintracht, S.; Nessim, S.J.; MacNamara, E. Effect of Hemodialysis on Levels of High-Sensitivity Cardiac Troponin T. Am. J. Cardiol. 2017, 120, 2061–2064. [Google Scholar] [CrossRef]
- Hunderup, M.M.; Kampmann, J.D.; Kristensen, F.B.; Hafsund, M. The short-term effect of hemodialysis on the level of high-sensitive cardiac troponin T—A systematic review. Semin. Dial. 2024, 37, 110–116. [Google Scholar] [CrossRef]
- O’lOne, E.; Apple, F.S.; Burton, J.O.; Caskey, F.J.; Craig, J.C.; Defilippi, C.R.; Forfang, D.; Hicks, K.A.; Jha, V.; Mahaffey, K.W.; et al. Defining myocardial infarction in trials of people receiving hemodialysis: Consensus report from the SONG-HD MI Expert Working group. Kidney Int. 2023, 103, 1028–1037. [Google Scholar] [CrossRef]

| Total | |
|---|---|
| N = 56 | |
| Age (SD), years | 71.8 (±12.9) |
| Male (%) | 35 (62.5%) |
| BMI (SD) | 27.7 (±5.27) |
| HTN (%) | 51 (91.1%) |
| DLP (%) | 47 (83.9%) |
| DM (%) | 35 (62.5%) |
| Smoker † (%) (n = 54) | 13 (23.2%) |
| Prior CAD (%) | 25 (44.6%) |
| Prior PCI (%) | 19 (33.9%) |
| Prior CABG (%) | 7 (12.5%) |
| Stroke (%) | 15 (26.8%) |
| PAD (%) | 10 (17.9%) |
| CHF (%) | 27 (48.2%) |
| LVEF (%) (n = 54) | |
| ≥50% | 38 (70.4%) |
| 40–49% | 8 (14.8%) |
| <40% | 8 (14.8%) |
| PHT ¤ (%) (n = 55) | 26 (46.4%) |
| AF/AFL (%) | 23 (41.1%) |
| Anemia (%) | 53 (94.6%) |
| Malignancy † (%) | 8 (14.3%) |
| Total | |
|---|---|
| N = 56 | |
| Cause of ESRD † (%) | |
| DM | 22 (39.3%) |
| HTN | 9 (16.1%) |
| IgA nephropathy | 2 (3.6%) |
| FSGS | 3 (5.4%) |
| CRS | 4 (7.1%) |
| Amyloidosis | 1 (1.8%) |
| Vasculitis | 4 (7.1%) |
| PKD | 2 (3.6%) |
| GN | 2 (3.6%) |
| Lithium | 2 (3.6%) |
| MM | 1 (1.8%) |
| Uknown | 4 (7.1%) |
| Dialysis vintage (SD), months | 54.1 (±63.2) |
| Dialysis session duration (SD), hours | 3.65 (±0.409) |
| Type of solution (%) | |
| Standard | 41 (73.2%) |
| Low Ca | 10 (17.9%) |
| High Ca | 1 (1.8%) |
| Standard + KCl | 3 (5.4%) |
| Low Ca + KCl | 1 (1.8%) |
| Dry weight (SD), kg | 73.8 (±16.4) |
| Intradialytic weight gain (SD), kg | 1.42 (±2.72) |
| Target loss (SD), L | 2.63 (±0.980) |
| MAP pre-dialysis (SD), mmHg | 91.1 (±16.0) |
| MAP post-dialysis (SD), mmHg | 84.7 (±13.2) |
| Delta MAP ¤ (SD), mmHg | 6.05 (±16.5) |
| Kt/V (SD) | 1.38 (±0.253) |
| Above Median (N = 28) | Below Median (N = 28) | p-Value | |
|---|---|---|---|
| Age (SD), years | 74.9 (±12.9) | 68.7 (±12.3) | 0.034 |
| PHT (%) (n = 55) | 17 (60.7%) | 9 (32.1%) | 0.076 |
| Creatinine pre-dialysis (SD), mg/dL | 6.52 (±1.56) | 7.87 (±2.27) | 0.019 |
| Creatinine post-dialysis (SD), mg/dL | 2.30 (±0.771) | 2.88 (±0.936) | 0.011 |
| Cause of ESRD † (%) | |||
| DM | 11 (39.3%) | 11 (39.3%) | 0.013 |
| HTN | 9 (32.1%) | 0 (0%) | |
| IGA nephropathy | 1 (3.6%) | 1 (3.6%) | |
| FSGS | 0 (0%) | 3 (10.7%) | |
| CRS | 2 (7.1%) | 2 (7.1%) | |
| Amyloidosis | 1 (3.6%) | 0 (0%) | |
| Vasculitis | 0 (0%) | 4 (14.3%) | |
| PKD | 0 (0%) | 2 (7.1%) | |
| GN | 0 (0%) | 2 (7.1%) | |
| Lithium | 2 (7.1%) | 0 (0%) | |
| MM | 0 (0%) | 1 (3.6%) | |
| Uknown | 2 (7.1%) | 2 (7.1%) | |
| Intradialytic weight gain (SD), kg | 1.38 (±0.932) | 1.47 (±3.77) | 0.03 |
| Target loss (SD), L | 2.43 (±0.920) | 2.83 (±1.01) | 0.047 |
| Number of hospitalizations (SD) | 1.11 (±1.45) | 0.536 (±0.999) | 0.0746 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Rabi, O.; Shavit, L.; Loutati, R.; Taha, L.; Karmi, M.; Brin, A.; Deeb, D.; Levi, N.; Fink, N.; Sabouret, P.; et al. High Sensitive Cardiac Troponin-I (Hs-cTnI) Levels in Asymptomatic Hemodialysis Patients. J. Clin. Med. 2025, 14, 5470. https://doi.org/10.3390/jcm14155470
Rabi O, Shavit L, Loutati R, Taha L, Karmi M, Brin A, Deeb D, Levi N, Fink N, Sabouret P, et al. High Sensitive Cardiac Troponin-I (Hs-cTnI) Levels in Asymptomatic Hemodialysis Patients. Journal of Clinical Medicine. 2025; 14(15):5470. https://doi.org/10.3390/jcm14155470
Chicago/Turabian StyleRabi, Ofir, Linda Shavit, Ranel Loutati, Louay Taha, Mohammad Karmi, Akiva Brin, Dana Deeb, Nir Levi, Noam Fink, Pierre Sabouret, and et al. 2025. "High Sensitive Cardiac Troponin-I (Hs-cTnI) Levels in Asymptomatic Hemodialysis Patients" Journal of Clinical Medicine 14, no. 15: 5470. https://doi.org/10.3390/jcm14155470
APA StyleRabi, O., Shavit, L., Loutati, R., Taha, L., Karmi, M., Brin, A., Deeb, D., Levi, N., Fink, N., Sabouret, P., Manassra, M., Qadan, A., Amro, M., Glikson, M., & Asher, E. (2025). High Sensitive Cardiac Troponin-I (Hs-cTnI) Levels in Asymptomatic Hemodialysis Patients. Journal of Clinical Medicine, 14(15), 5470. https://doi.org/10.3390/jcm14155470







