Abstract
Background/Objectives: We sought to characterize the variance and overlap among definitions of Proximal Junctional Kyphosis (PJK) used in the adult spinal deformity (ASD) literature. PJK is defined as excess in PJK angle, a Cobb angle between the upper-instrumented vertebra (UIV) and a supra-adjacent vertebra (SAV), either one (UIV+1) or two (UIV+2) levels rostral of the UIV. No expert consensus exists for threshold angle or which SAV to use. Methods: A total of 116 thoracolumbar fusion patients ≥ 65 years old were reviewed. The UIV+1 and UIV+2 angles were measured. Six definitions of PJK from the literature were evaluated. These definitions were selected based on citation frequency, historical relevance, and accessibility through commonly used databases. Pearson’s Chi-squared and pairwise comparisons were performed to evaluate the distinctness and agreement rates among these definitions. Results: The six definitions of PJK were as follows: [PJK20] PJK angle ≥ 20° with UIV+2 as the (SAV), [PJK10] PJK angle ≥ 10° with a >10° change from pre-op with UIV+2 as the SAV, [PJK2SD] PJK angle > 2 standard deviations from average with UIV+1 as the SAV, [PJK10+10] PJK angle ≥ 10° with a >10° change from pre-op with UIV+1 as the SAV, [PJK15] PJK angle > 15° with UIV+1 as the SAV, and [PJK30] PJK angle > 30° with UIV+2 as the SAV, or displaced rod fracture, or reoperation within 2 years for junctional failure, pseudoarthrosis, or rod fracture. [PJK10] and [PJK2SD] were the most distinct definitions while [PJK20], [PJK10+10], [PJK15], and [PJK30] showed no significant pairwise differences. [PJK2SD] was stringent, while definition [PJK30] included unique diagnostic information not captured by other definitions. Conclusions: The use of [PJK20], [PJK10+10], [PJK15], or [PJK30] is recommended for consistency, with [PJK15] presenting the best balance. Stringent [PJK2SD] may be beneficial for identifying severe PJK, though with low sensitivity. Overall, PJK definitions must be standardized for the consistent reporting of clinical outcomes and research comparability.
1. Introduction
Adult spinal deformity (ASD) is a common spinal disorder that is projected to become increasingly prevalent in the future [1]. ASD may be brought about by multiple etiologies, including degenerative disease, iatrogenic causes (e.g., prior spinal surgery), or conditions such as ankylosing spondylitis [2]. Regardless of the cause, ASD often must be addressed via long-segment posterior pedicle screw and rod constructs. These surgeries can be quite effective in restoring proper alignment and promoting adequate fusion. However, extensive rigid constructs also carry the risk of complications, notably proximal junctional kyphosis (PJK), broadly defined as kyphosis that develops at the interface of the cranial end of the construct and the adjacent mobile segments [1,3,4]. The prevalence of PJK after surgery for ASD may lie between 20 and 40%, though some sources report rates as high as 61% [5,6,7,8].
While a global definition of PJK is consistent among publications, various authors have put forth different nuanced criteria [3,5,9,10]. In general, PJK is usually defined as an excess PJK angle, a Cobb angle formed between the upper-instrumented vertebra (UIV) and a supra-adjacent vertebra (SAV) either one (UIV+1) or two (UIV+2) vertebral levels above the UIV. Depending on the study, a Cobb angle of at least 10–20 degrees is required for the diagnosis of PJK [3,5,9,10]. Different cutoff values for PJK angle have been analyzed with respect to their prognostic value as predictors of postoperative pain, functional recovery, or the need for revision surgery [11,12,13]. Nonetheless, the results have not supported one strict definition of clinically significant PJK and no expert consensus currently exists as to the ideal magnitude to use for the PJK angle or which SAV should be used.
To that end, we used a large cohort of patients ≥ 65 years of age who underwent thoracolumbar fusions for ASD to better characterize the variance and overlap among multiple existing definitions of PJK used in the literature and to evaluate which definitions may be the most useful to compare across future studies.
2. Materials and Methods
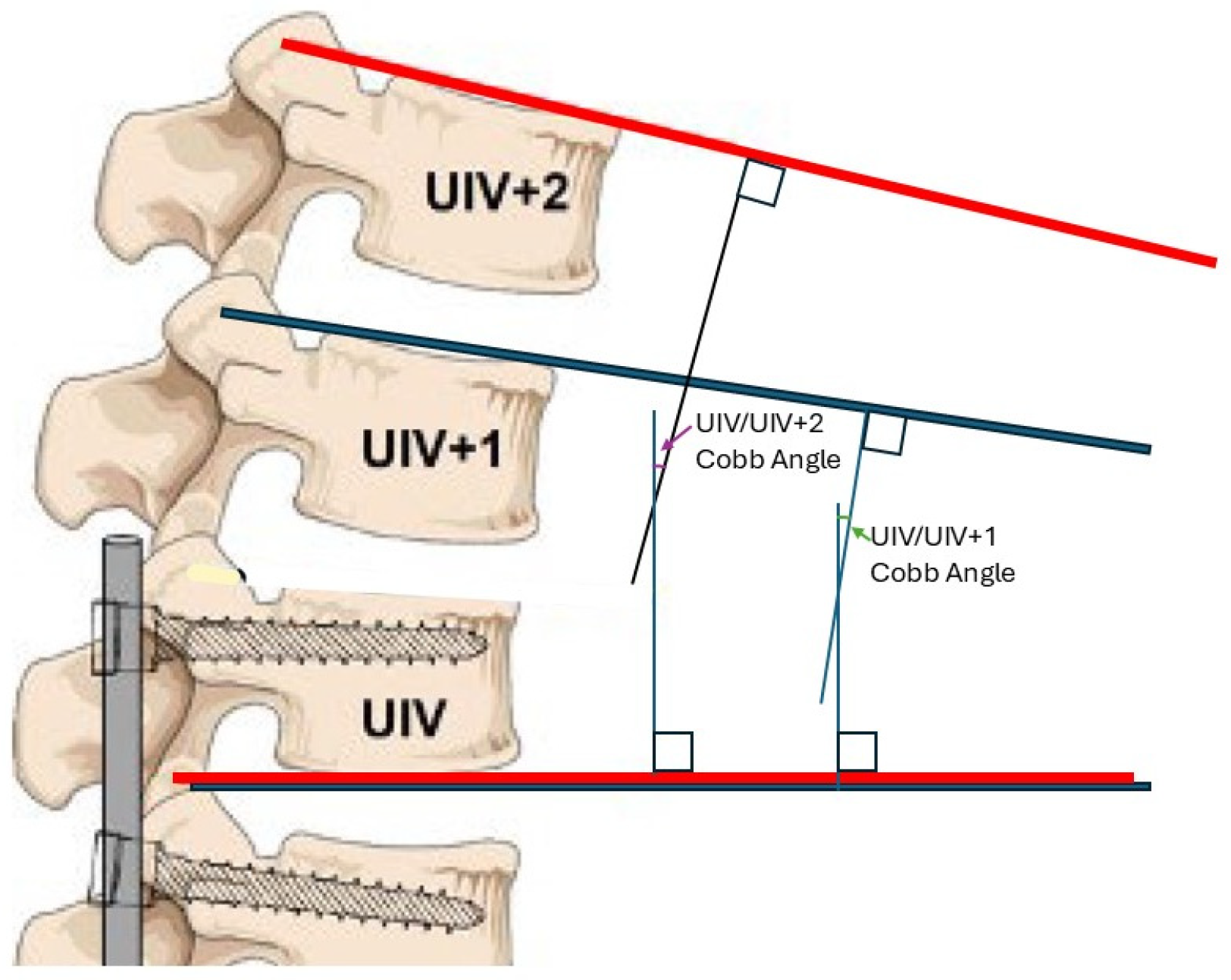
Radiographic and demographic data were collected for thoracolumbar fusion from an institutional database for patients ≥ 65 years old with a diagnosis of ASD. Patients who underwent fusion of at least three segments within the thoracolumbar region with pelvic fixation at the authors’ institution between 2014 and 2024 were included, while patients with missing radiographs for the required analysis were excluded. Preoperative and most recent follow-up (≥6 months postoperative) full-body scoliosis radiographs were exported from the patient’s electronic medical record (EMR). The upper instrumented vertebrae (UIV) for each patient were identified from intraoperative/postoperative imaging, and the Cobb angle was measured between the inferior endplate of the UIV and the superior endplate of the vertebrae immediately cranial to the UIV (UIV+1) (Figure 1, blue). A second Cobb angle was measured between the inferior endplate of the UIV and the superior endplate of the vertebrae two levels cranial to the UIV (UIV+2) (Figure 1, red) [14]. Angles were measured from both the preoperative and most recent follow-up radiographs.
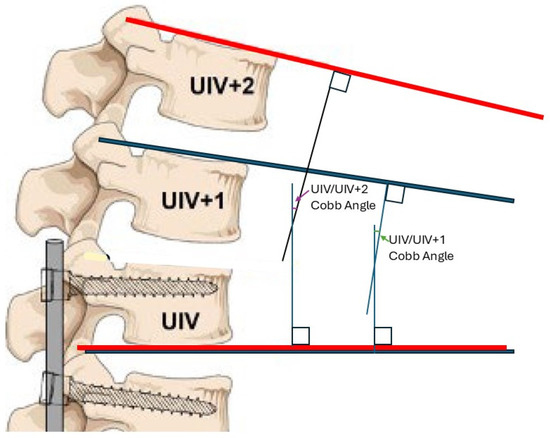
Figure 1.
Diagram of the Cobb angle between the upper instrumented vertebrae (UIV) and the UIV+1 (blue) or UIV+2 (red). Figure adapted from Boeckenfoerde et al. with permission per Creative Commons (CC BY) licensing guidelines [14].
A PubMed search with key terms (“proximal junction* kyphosis” AND “definition”) and subsequent exploration of citations yielded 6 criteria for varying definitions of PJK based on different thresholds of the UIV to UIV+1 or UIV+2 Cobb angle [3,5,9,10,15,16]. These definitions were pragmatically selected based on expert opinion, incorporating factors such as citation counts, foundational influence, and prominence in standard database search results. A series of statistical tests were performed with R: A Language and Environment for Statistical Computing version 4.4.1 (CRAN, 2024). A Pearson’s Chi-squared test was performed among the different rates of PJK based on the definitions identified from the PubMed search. A subsequent pairwise comparison of proportions was performed to evaluate the distinctness of each individual definition’s rate in comparison to one another. Rate of agreement among PJK definitions were also analyzed in a pairwise fashion, followed by an evaluation of the proportion of PJK diagnoses that would also be diagnosed by additional criteria. Statistical significance was established by an alpha < 0.05, and 95% confidence intervals (95% CI) were calculated.
3. Results
A total of 116 patients met the inclusion criteria, 79 of whom were female (68.1%). The average age of the cohort was 70.9 ± 4.3 years, and the average BMI was 28.9 ± 5.4 (Table 1). Analysis of PJK definitions requiring identification of the UIV+2 decreased the total cohort to 111 patients due to visual obstruction of the UIV+2 vertebrae from either image cutoff or low resolution for 5 patients. For consistency, analysis of all PJK definitions were performed on the 111 eligible patients.

Table 1.
Descriptive statistics of demographics and characteristics of this study’s cohort.
The following six criteria for PJK were identified from the PubMed search: (1) PJK angle ≥ 20° with UIV+2 as the SAV; (2) PJK angle ≥ 10° with a >10° change from preoperative values with UIV+2 as the SAV; (3) PJK angle > 2 standard deviations from average with UIV+1 as the SAV; (4) PJK angle ≥ 10° with a >10° change from preoperative values with UIV+1 as the SAV; (5) PJK angle > 15° with UIV+1 as the SAV; and (6) PJK angle > 30° with UIV+2 as the SAV, displaced rod fracture, or reoperation within 2 years for junctional failure, pseudoarthrosis, or rod fracture (Table 2) [3,5,9,10,16]. These PJK definitions will henceforth be referred to as (1) PJK20, (2) PJK10, (3) PJK2SD, (4) PJK10+10, (5) PJK15, and (6) PJK30. PJK rates, by each definition, were (1) 20.7% (95% CI: 13.8–29.7%), (2) 36.9% (95% CI: 28.1–46.7%), (3) 3.6% (95% CI: 1.2–9.5%), (4) 23.4% (95% CI: 16.1–32.6%), (5) 15.3% (95% CI: 9.4–23.7%), and (6) 10.8% (95% CI: 6.0–18.5%).

Table 2.
Collection of PJK definitions, referenced studies, and rate of PJK within this study’s cohort per definition [3,5,9,10,16].
Pearson’s Chi-squared testing revealed significant variance among rates of PJK by criteria (p = 2.6 × 10−9, χ2 = 48.7, 95% CI: 0.83–12.8) with a Cramer’s V of 0.27 (95% CI: 0.18–0.34). Post hoc pairwise proportion testing with Holm p-value adjustment revealed 5 significantly distinct definition pairs and 10 non-significantly distinct pairs. The distinct pairs were PJK20&PJK2SD (p = 2.63 × 10−3, 95% CI: 0.088–0.25), PJK10&PJK2SD (p = 4.86 × 10−3, 95% CI: 0.24–0.43), PJK10&PJK15 (p = 2.80 × 10−8, 95% CI: 0.10–0.33), PJK10&PJK30 (p = 1.50 × 10−4, 95% CI: 0.15–0.37), and PJK2SD&PJK10+10 (p = 4.90 × 10−4, 95% CI: 0.11–0.28) (Table 3). In other words, the overall PJK rates for our cohort given by these distinct pairs were significantly different from each other. Meanwhile, the overall PJK rates given by every other pair were not significantly different.

Table 3.
Post hoc pairwise comparison of the various definitions with proportional difference (top) and Holm-adjusted p-values (bottom). Statistically significant distinct pairs of definitions are highlighted.
The pairwise agreements of the cohort classification as PJK positive or negative among these six definitions are shown in Table 4. These percentages represented the proportion of patients that were similarly diagnosed as having or not having PJK between the pair of definitions. The pairs with the greatest agreement were PJK10+10&PJK15 at 90.1% (95% CI: 82.6–94.7%), PJK2SD&PJK30 at 89.2% (95% CI: 81.5–94.0%), and PJK2SD&PJK15 at 88.3% (95% CI: 80.5–93.4%) (Table 4). Furthermore, PJK30, PJK2SD, and PJK15 had the greatest agreement with reoperation at 82.9% (95% CI: 74.3–89.1%), 79.3% (95% CI: 70.3–86.2%), and 71.2% (95% CI: 61.7–79.2%), respectively.

Table 4.
Pairwise agreement among PJK definitions representing the percentage (95% CI) of patients diagnosed similarly between a pair of definitions. The three pairs with greatest agreement are highlighted.
Among patients with PJK according to a particular definition, the following percentages were identified as having PJK by at least one other definition: (PJK20) 91.3%, (PJK10) 78.0%, (PJK2SD) 100%, (PJK10+10) 88.5%, (PJK15) 100%, and (PJK30) 29.4%. The percentages of each definition’s PJK cohort that met criteria for additional PJK definitions are shown in Table 5.

Table 5.
Percentage of PJK positive patients meeting up to 5 additional PJK criteria.
4. Discussion
Discussions of PJK are of much interest in the spinal deformity literature. However, this condition is heterogeneously defined depending on the article and classification criteria used. In this study we used a large cohort of patients who underwent surgical correction of ASD to evaluate six different definitions of PJK identified in the current literature, each broadly cited and readily accessible among the prominent spinal deformity literature. We investigated which definition may encapsulate the most patients in our cohort to determine the definition that may be of most utility when comparing PJK among studies or for potential surgical decision-making. While we found that certain definitions of PJK captured similar patient subsets of our overall patient cohort, there were nevertheless significant differences between multiple criteria as to which patients would qualify as having PJK. In aggregate, our work demonstrates that comparison of results between studies that utilize distinct definitions of PJK may be difficult to interpret and of limited utility.
Only PJK definition PJK30 directly considered patient outcomes beyond imaging findings by integrating the need for reoperation or instrumentation failure [16]. Hence, we considered it the most clinically relevant definition for a symptomatic PJK. PJK30’s close relationship with patient function and greatest agreement with reoperation rates supported its use as a clinical benchmark for comparison with other definitions (Table 4).
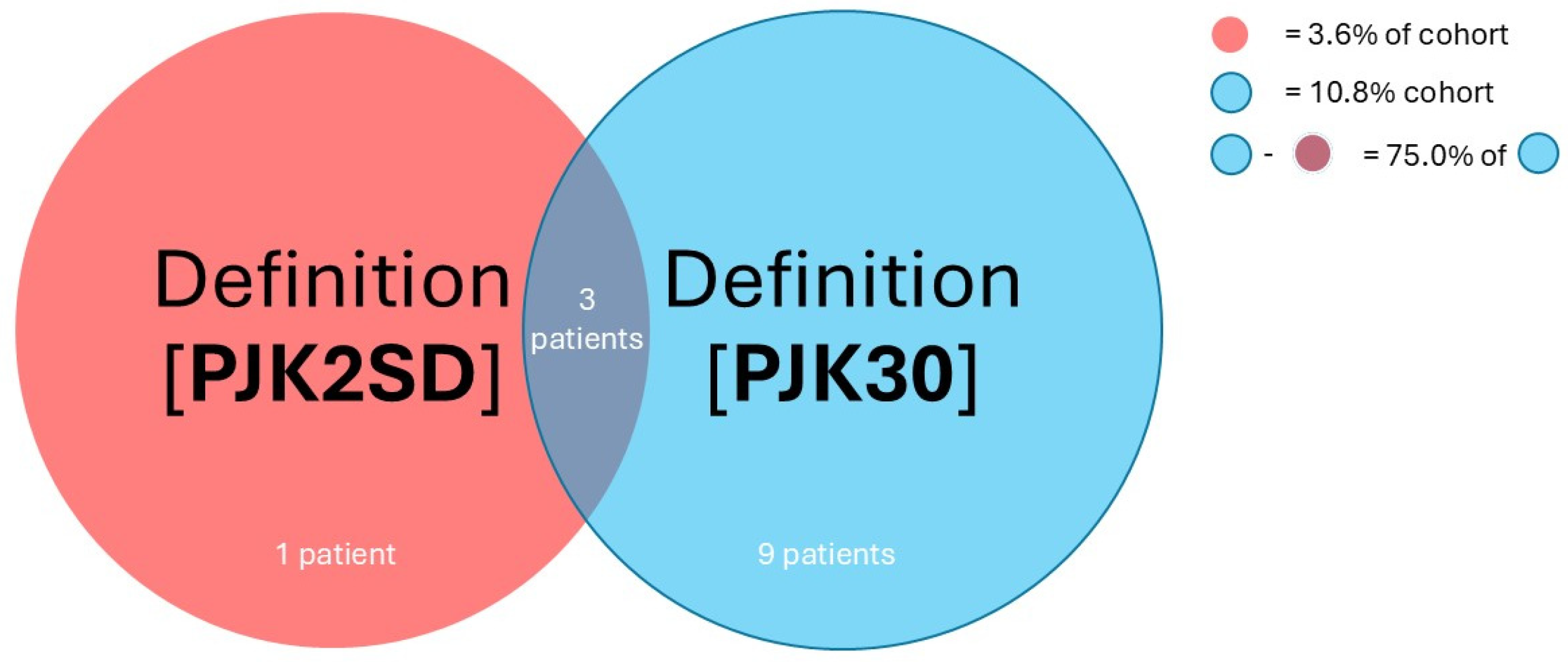
Considering the raw rate of PJK-positive patients in the same cohort, definition PJK2SD was the strictest for assigning PJK, while definition PJK10 was the most lenient among the six PJK definitions. The low rate of PJK for definition PJK2SD suggests that the dispersion of UIV/UIV+1 angles was functionally small to yield such a stringent diagnosis [9]. Notably, the tightness of distribution of this UIV/UIV+1 angle was relatively more extreme than the already conservative benchmark definition PJK30. This means that, in contrast to clinically relevant definition PJK30 (diagnosing 10.8% of the entire cohort), only 3.6% of the entire cohort experienced the kyphotic angle at the UIV varying outside expected ranges per definition PJK2SD. A conservative calculation, assuming all 3.6% of PJK patients per definition PJK2SD were also accounted for by definition PJK30, found that 66.7% of patients who experienced symptomatic PJK by definition PJK30 did not meet the threshold for definition PJK2SD. Considering that only 89.2% of positive or negative PJK diagnoses from definitions PJK2SD and PJK30 overlapped (Table 4), 75.0% of patients with symptomatic PJK (qualified by definition PJK30) were not accounted for by definition PJK2SD (Figure 2). It should be noted that definition PJK2SD was historically applied to adolescent scoliosis, which features a distinctly different clinical, biomechanical, and pathophysiologic picture than the degenerative ASD featured in our cohort [17].
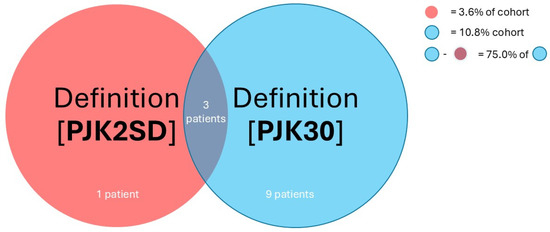
Figure 2.
Venn diagram illustration of the overlapping relationship between definition (3) PJK2SD and (6) PJK30, showing that 75.0% of PJK+ patients by (6) PJK30 are not accounted for by (3) PJK2SD.
A comparison of raw PJK rates from definitions PJK10 and PJK10+10, which differ only by usage of the UIV+1 or UIV+2 vertebrae as the cranial vertebrae in Cobb angle measurements, demonstrates that the use of definition PJK10+10, and thus the UIV+1 vertebrae, results in stricter criteria for PJK (Table 2) [3,10]. Again, if we were to use definition PJK30 as the standard for symptomatic PJK, the use of definition PJK10, or the UIV+2 vertebrae, could be interpreted as too lenient of a definition in comparison to use of definition PJK10+10, or UIV+1.
Closer evaluation of the pairwise overlap between definition PJK30 and either definitions PJK10 or PJK10+10 confirms that definition PJK10+10, or the use of the UIV+2, also diagnoses the PJK status of individual patients more similarly to that of definition PJK30 (Table 4). In fact, definition PJK10 had the least overlap with definition PJK30 compared to all other definitions, whereas definition PJK2SD, which used extreme deviations of PJK from average values, had the best overlap. This might suggest that, while definition PJK2SD is the strictest criteria for PJK, those who met the high threshold to be considered PJK positive by PJK2SD were more likely to require reoperation. However, definition PJK30 also includes a criterion for extreme PJK angle magnitude, which may confound this conclusion.
Chi-square testing with post hoc pairwise proportions analysis and p-value adjustment demonstrated that 10/15 (67%) definition pairs were not significantly different when evaluating overall cohort PJK rates (Table 3). Among the five distinct pairs, definitions PJK10 and PJK2SD were most common. Definition PJK10 was found to be too lenient and definition PJK2SD too strict based on raw PJK rates, which could explain why they was often statistically different from the other definitions and limited in practicality. Definitions PJK20, PJK10+10, PJK15, and PJK30 were not distinct from each other. These results suggest that definitions PJK10 and PJK2SD should be used with caution when consistency across studies is desired, while definitions PJK20, PJK10+10, PJK15, and PJK30 may be used more interchangeably.
From the evaluation of additional PJK criteria that were encompassed by each of the six definitions, as shown in Table 5, patients diagnosed as having PJK by definition PJK2SD would also be sufficiently diagnosed by most other definitions. In the context of definition PJK2SD’s stringent nature, this suggests that most other PJK definitions have sufficient coverage and that use of definition PJK2SD may be redundant. On the other end of the spectrum, the patients labeled PJK-positive by PJK30 were often not diagnosed by other PJK criteria. This finding further supports the utility of definition PJK30, including capturing unique information that is missed by the remaining PJK definitions.
Overall, our findings suggest that definition PJK15 most optimally balances the clinical relevance of definition PJK30 while not yielding statistically different rates of PJK in our cohort. Additionally, definition PJK15 utilizes the UIV+1 vertebrae, which found greater agreement with definition PJK30 than when measuring the UIV+2 vertebrae. Definition PJK15 may also possibly identify PJK earlier than definition PJK30 because PJK15, which relies purely on imaging characteristics, is not contingent on the patient undergoing reoperation, allowing clinicians to identify early PJK that may not have yet progressed to such a degree to necessitate surgical intervention. That said, this hypothesis requires further validation in future studies that incorporate comprehensive clinical outcomes beyond just reoperation rates.
5. Limitations and Future Steps
This study has several limitations. First, its retrospective design inherently limits its ability to establish causal relationships between the definitions of PJK and outcomes such as reoperation rates. Secondly, data collection was performed at a single institution, which may reduce the generalizability of our findings to broader populations. Third, the exclusive focus on patients aged 65 and older may not reflect PJK dynamics in younger cohorts undergoing spinal surgeries. An age restriction was implemented for our cohort to focus analysis on elderly adults, who have a greater risk of developing PJK than younger adults [18,19,20,21,22]. Furthermore, younger adults tend to have distinct clinical presentations of ASD from older adults that cannot be fully accounted for by radiographic measurements, so their inclusion could have obscured our findings [2,23]. Another limitation is this study’s reliance on reoperation as a proxy for clinical outcomes. Certainly, other suboptimal clinical outcomes in the setting of PJK such as severe pain, reduced quality of life, decreased activity tolerance, or neurological symptoms could still prove distressing to patients who did not undergo reoperation for PJK. Similarly, patients could have instrumentation failure that received surgery without displaying any of these symptoms. Our reliance on reoperation as the sole surrogate for symptomatic PJK may potentially lead to incongruence between radiographic outcomes and patient-centered outcomes.
Furthermore, some definitions, such as PJK2SD, were historically applied to adolescent scoliosis, which presents distinct biomechanical and clinical characteristics compared to adult spinal deformity. These differences may limit the applicability of such definitions to the adult population examined in this study. Further studies should aim to validate these definitions prospectively in multi-institutional cohorts and consider broader clinical outcomes beyond reoperation to provide a more comprehensive understanding of PJK. Finally, it should be noted that no formal non-radiographic analysis was performed for definition PJK15 to definitively demonstrate its superiority in predicting clinical outcomes compared to other definitions (e.g., Delphi analysis). PJK15’s applicability was inferred from its statistical overlap with PJK30—a definition with intrinsic clinical outcome considerations—and this concept should be evaluated more thoroughly in future studies through consensus-building efforts as a next step towards definition standardization (e.g., Delphi analysis, Nominal Group Technique, or RAND/UCLA appropriateness method). Exploring whether different PJK definitions might be more appropriate for different patient subgroups (age, fusion length, and etiology) could further refine clinical decision-making.
6. Conclusions
This study highlights the variability in PJK definitions and their implications for clinical and radiographic outcomes. Clinically relevant, symptomatic PJK often does not correspond to larger deviations in PJK angle, underscoring the importance of definitions that align with patient outcomes. Among the definitions evaluated, PJK30 demonstrated itself to be the most clinically relevant with strong alignment to reoperation rates, thus making it a robust option for identifying symptomatic PJK. PJK15, while similar to PJK30, relies purely on radiographic criteria and thus offers the advantage of enabling the earlier diagnosis of PJK before clinical symptoms become apparent. In contrast, PJK20 and PJK10+10, though statistically viable, are limited by their reliance on UIV +2 measurements which are less practical than definitions that rely on UIV+1 due to the limited visibility or radiographic cutoff that may present when attempting to visualize a more rostral vertebra. These findings support the need for standardized PJK definitions that emphasize both clinical and radiographic relevance to improve consistency in research and surgical decision-making.
Author Contributions
Conceptualization, T.T.B. and C.A.M.; methodology, T.T.B.; software, T.T.B.; validation, T.T.B., K.J. and C.A.M.; formal analysis, T.T.B.; investigation, T.T.B., K.J., S.V. and M.R.-C.; resources, C.A.M.; data curation, T.T.B., K.J., S.V. and M.R.-C.; writing—original draft preparation, T.T.B., A.T.Y. and K.J.; writing—review and editing, T.T.B., K.J., A.T.Y., M.R.-C. and C.A.M.; visualization, T.T.B.; supervision, C.A.M.; project administration, C.A.M. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
This study was conducted in accordance with the Declaration of Helsinki and approved by the Institutional Review Board of Washington University in St. Louis (#202302010, 20 April 2025).
Informed Consent Statement
Patient consent was waived due to the retrospective nature of this study.
Data Availability Statement
The data used for this study were obtained from electronic medical records from Barnes-Jewish Hospital (St. Louis, MO) and contain protected health information. Due to institutional policies and patient confidentiality regulations, these data are not publicly available. Data access is restricted to approved researchers in compliance with ethical and regulatory requirements. Please contact Washington University’s Institutional Review Board for further information on data access.
Acknowledgments
Washington University School of Medicine’s Dean’s Medical Student Research Fellowship for the MPHS Yearlong Research Program.
Conflicts of Interest
The authors declare no conflicts of interest. CAM is a consultant for Kuros, Augmedics, SMAIO, Baxter Health, and SI-Bone. The research conducted to acquire the results of this study were not funded with any grants.
Abbreviations
The following abbreviations are used in this manuscript:
| ASD | Adult Spinal Deformity |
| PJK | Proximal Junctional Kyphosis |
| UIV | Upper Instrumented Vertebra |
| SAV | Supra-adjacent Vertebra |
| EMR | Electronic Medical Record |
| BMI | Body Mass Index |
| SD | Standard Deviation |
| CI | Confidence Interval |
References
- Kim, H.J.; Iyer, S. Proximal Junctional Kyphosis. JAAOS-J. Am. Acad. Orthop. Surg. 2016, 24, 318–326. [Google Scholar] [CrossRef]
- Diebo, B.G.; Shah, N.V.; Boachie-Adjei, O.; Zhu, F.; Rothenfluh, D.A.; Paulino, C.B.; Schwab, F.J.; Lafage, V. Adult spinal deformity. Lancet 2019, 394, 160–172. [Google Scholar] [CrossRef]
- Bridwell, K.H.; Lenke, L.G.; Cho, S.K.; Pahys, J.M.; Zebala, L.P.; Dorward, I.G.; Cho, W.; Baldus, C.; Hill, B.W.; Kang, M.M. Proximal junctional kyphosis in primary adult deformity surgery: Evaluation of 20 degrees as a critical angle. Neurosurgery 2013, 72, 899–906. [Google Scholar] [CrossRef] [PubMed]
- Sardar, Z.M.; Kim, Y.; Lafage, V.; Rand, F.; Lenke, L.; Klineberg, E. State of the art: Proximal junctional kyphosis-diagnosis, management and prevention. Spine Deform. 2021, 9, 635–644. [Google Scholar] [CrossRef] [PubMed]
- Glattes, R.C.; Bridwell, K.H.; Lenke, L.G.; Kim, Y.J.; Rinella, A.; Edwards, C., 2nd. Proximal junctional kyphosis in adult spinal deformity following long instrumented posterior spinal fusion: Incidence, outcomes, and risk factor analysis. Spine 2005, 30, 1643–1649. [Google Scholar] [CrossRef] [PubMed]
- Kim, H.J.; Lenke, L.G.; Shaffrey, C.I.; Van Alstyne, E.M.; Skelly, A.C. Proximal junctional kyphosis as a distinct form of adjacent segment pathology after spinal deformity surgery: A systematic review. Spine 2012, 37 (Suppl. S22), S144–S164. [Google Scholar] [CrossRef]
- Lee, J.H.; Kim, J.U.; Jang, J.S.; Lee, S.H. Analysis of the incidence and risk factors for the progression of proximal junctional kyphosis following surgical treatment for lumbar degenerative kyphosis: Minimum 2-year follow-up. Br. J. Neurosurg. 2014, 28, 252–258. [Google Scholar] [CrossRef]
- Yagi, M.; King, A.B.; Boachie-Adjei, O. Incidence, risk factors, and natural course of proximal junctional kyphosis: Surgical outcomes review of adult idiopathic scoliosis. Minimum 5 years of follow-up. Spine 2012, 37, 1479–1489. [Google Scholar] [CrossRef]
- Helgeson, M.D.; Shah, S.A.; Newton, P.O.; Clements, D.H., III; Betz, R.R.; Marks, M.C.; Bastrom, T. Evaluation of proximal junctional kyphosis in adolescent idiopathic scoliosis following pedicle screw, hook, or hybrid instrumentation. Spine 2010, 35, 177–181. [Google Scholar] [CrossRef]
- Lonner, B.S.; Newton, P.; Betz, R.; Scharf, C.; O’Brien, M.; Sponseller, P.; Lenke, L.; Crawford, A.; Lowe, T.; Letko, L.; et al. Operative management of Scheuermann’s kyphosis in 78 patients: Radiographic outcomes, complications, and technique. Spine 2007, 32, 2644–2652. [Google Scholar] [CrossRef]
- Hassanzadeh, H.; Gupta, S.; Jain, A.; El Dafrawy, M.H.; Skolasky, R.L.; Kebaish, K.M. Type of Anchor at the Proximal Fusion Level Has a Significant Effect on the Incidence of Proximal Junctional Kyphosis and Outcome in Adults After Long Posterior Spinal Fusion. Spine Deform. 2013, 1, 299–305. [Google Scholar] [CrossRef] [PubMed]
- Kim, H.J.; Bridwell, K.H.; Lenke, L.G.; Park, M.S.; Ahmad, A.; Song, K.-S.; Piyaskulkaew, C.; Hershman, S.; Fogelson, J.; Mesfin, A. Proximal junctional kyphosis results in inferior SRS pain subscores in adult deformity patients. Spine 2013, 38, 896–901. [Google Scholar] [CrossRef] [PubMed]
- Kim, H.J.; Bridwell, K.H.; Lenke, L.G.; Park, M.S.; Song, K.S.; Piyaskulkaew, C.; Chuntarapas, T. Patients with proximal junctional kyphosis requiring revision surgery have higher postoperative lumbar lordosis and larger sagittal balance corrections. Spine 2014, 39, E576–E580. [Google Scholar] [CrossRef] [PubMed]
- Boeckenfoerde, K.; Schulze Boevingloh, A.; Gosheger, G.; Bockholt, S.; Lampe, L.P.; Lange, T. Risk Factors of Proximal Junctional Kyphosis in Adolescent Idiopathic Scoliosis-The Spinous Processes and Proximal Rod Contouring. J. Clin. Med. 2022, 11, 6098. [Google Scholar] [CrossRef]
- Hyun, S.J.; Lee, B.H.; Park, J.H.; Kim, K.J.; Jahng, T.A.; Kim, H.J. Proximal Junctional Kyphosis and Proximal Junctional Failure Following Adult Spinal Deformity Surgery. Korean J. Spine 2017, 14, 126–132. [Google Scholar] [CrossRef]
- Hills, J.; Mundis, G.M.; Klineberg, E.O.; Smith, J.S.; Line, B.; Gum, J.L.; Protopsaltis, T.S.; Hamilton, D.K.; Soroceanu, A.; Eastlack, R.; et al. The T4-L1-Hip Axis: Sagittal Spinal Realignment Targets in Long-Construct Adult Spinal Deformity Surgery: Early Impact. J. Bone Jt. Surg. Am. 2024, 106, e48. [Google Scholar] [CrossRef]
- Petrosyan, E.; Fares, J.; Ahuja, C.S.; Lesniak, M.S.; Koski, T.R.; Dahdaleh, N.S.; El Tecle, N.E. Genetics and pathogenesis of scoliosis. N. Am. Spine Soc. J. 2024, 20, 100556. [Google Scholar] [CrossRef]
- Lafage, R.; Beyer, G.; Schwab, F.; Klineberg, E.; Burton, D.; Bess, S.; Kim, H.J.; Smith, J.; Ames, C.; Hostin, R.; et al. Risk Factor Analysis for Proximal Junctional Kyphosis After Adult Spinal Deformity Surgery: A New Simple Scoring System to Identify High-Risk Patients. Glob. Spine J. 2020, 10, 863–870. [Google Scholar] [CrossRef]
- Kim, Y.J.; Bridwell, K.H.; Lenke, L.G.; Glattes, C.R.; Rhim, S.; Cheh, G. Proximal junctional kyphosis in adult spinal deformity after segmental posterior spinal instrumentation and fusion: Minimum five-year follow-up. Spine 2008, 33, 2179–2184. [Google Scholar] [CrossRef]
- Kim, Y.J.; Bridwell, K.H.; Lenke, L.G.; Rhim, S.; Cheh, G. Sagittal thoracic decompensation following long adult lumbar spinal instrumentation and fusion to L5 or S1: Causes, prevalence, and risk factor analysis. Spine 2006, 31, 2359–2366. [Google Scholar] [CrossRef]
- O’Leary, P.T.; Bridwell, K.H.; Lenke, L.G.; Good, C.R.; Pichelmann, M.A.; Buchowski, J.M.; Kim, Y.J.; Flynn, J.B. Risk factors and outcomes for catastrophic failures at the top of long pedicle screw constructs: A matched cohort analysis performed at a single center. Spine 2009, 34, 2134–2139. [Google Scholar] [CrossRef]
- Naresh-Babu, J.; Kwan, K.Y.H.; Wu, Y.; Yilgor, C.; Alanay, A.; Cheung, K.M.C.; Polly, D.W.; Park, J.-B.; Ito, M.; Lenke, L.G.; et al. AO Spine Adult Spinal Deformity Patient Profile: A Paradigm Shift in Comprehensive Patient Evaluation in Order to Optimize Treatment and Improve Patient Care. Glob. Spine J. 2023, 13, 1490–1501. [Google Scholar] [CrossRef] [PubMed]
- Bess, S.; Boachie-Adjei, O.; Burton, D.; Cunningham, M.; Shaffrey, C.; Shelokov, A.; Hostin, R.; Schwab, F.; Wood, K.; Akbarnia, B. Pain and disability determine treatment modality for older patients with adult scoliosis, while deformity guides treatment for younger patients. Spine 2009, 34, 2186–2190. [Google Scholar] [CrossRef] [PubMed]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).