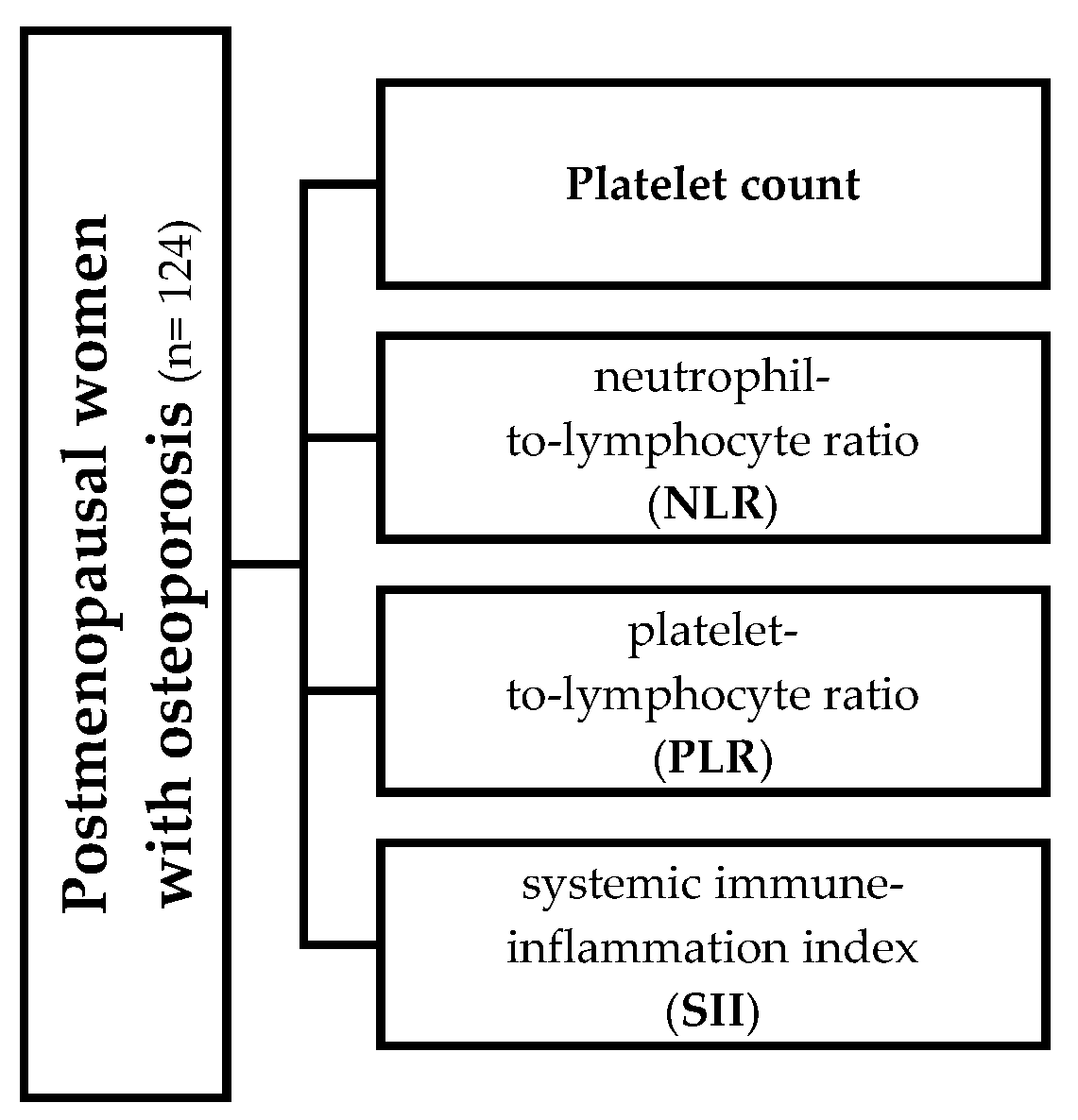
Exploring the Association Between Platelet Count, the Systemic Immune Inflammation Index, and Fracture Risk in Postmenopausal Women with Osteoporosis: A Cross-Sectional Study
Abstract
1. Introduction
2. Materials and Methods
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Lamichhane, A.P. Osteoporosis-an update. JNMA J. Nepal. Med. Assoc. 2005, 44, 60–66. [Google Scholar] [CrossRef] [PubMed]
- Baker-LePain, J.C.; Nakamura, M.C.; Lane, N.E. Effects of inflammation on bone: An update. Curr. Opin. Rheumatol. 2011, 23, 389–395. [Google Scholar] [CrossRef] [PubMed]
- Delmas, P.D. Clinical potential of RANKL inhibition for the management of postmenopausal osteoporosis and other metabolic bone diseases. J. Clin. Densitom. 2008, 11, 325–338. [Google Scholar] [CrossRef]
- Mazzaferro, S.; De Martini, N.; Rotondi, S.; Tartaglione, L.; Ureña-Torres, P.; Bover, J.; Pasquali, M.; ERA-EDTA Working Group on CKD-MBD. Bone, inflammation and chronic kidney disease. Clin. Chim. Acta. 2020, 506, 236–240. [Google Scholar] [CrossRef]
- Giannoudis, P.V.; Hak, D.; Sanders, D.; Donohoe, E.; Tosounidis, T.; Bahney, C. Inflammation, bone healing, and anti-inflammatory drugs: An update. J. Orthop. Trauma. 2015, 29 (Suppl. S12), S6–S9. [Google Scholar] [CrossRef]
- Semple, J.W.; Italiano, J.E., Jr.; Freedman, J. Platelets and the immune continuum. Nat. Rev. Immunol. 2011, 11, 264–274. [Google Scholar] [CrossRef]
- Silvagno, F.; De Vivo, E.; Attanasio, A.; Gallo, V.; Mazzucco, G.; Pescarmona, G. Mitochondrial localization of vitamin D receptor in human platelets and differentiated megakaryocytes. PLoS ONE 2010, 5, e8670. [Google Scholar] [CrossRef]
- Salari Sharif, P.; Abdollahi, M. The role of platelets in bone remodeling. Inflamm. Allergy Drug Targets 2010, 9, 393–399. [Google Scholar] [CrossRef] [PubMed]
- Kark, L.R.; Karp, J.M.; Davies, J.E. Platelet releasate increases the proliferation and migration of bone marrow-derived cells cultured under osteogenic conditions. Clin. Oral Implants Res. 2006, 17, 321–327. [Google Scholar] [CrossRef]
- Kim, J.; Kim, H.S.; Lee, H.S.; Kwon, Y.J. The relationship between platelet count and bone mineral density: Results from two independent population-based studies. Arch. Osteoporos. 2020, 15, 43. [Google Scholar] [CrossRef]
- Li, X.S.; Zhang, J.R.; Meng, S.Y.; Li, Y.; Wang, R.T. Mean platelet volume is negatively associated with bone mineral density in postmenopausal women. J. Bone Miner. Metab. 2012, 30, 660–665. [Google Scholar] [CrossRef]
- Yan, P.; Xu, Y.; Wan, Q.; Feng, J.; Yang, J.; Li, H.; Zhong, H.; Gao, C.; Zhang, Z. Impact of MPV and PDW on bone mineral density and their relationship with osteoporosis in Chinese patients with type 2 diabetes. Int. J. Clin. Exp. Med. 2018, 11, 2337–2349. [Google Scholar]
- Akbal, A.; Gokmen, F.; Gencer, M.; Inceer, B.S.; Komurcu, E. Mean platelet volume and platelet distribution width can be related to bone mineralization. Osteoporos. Int. 2014, 25, 2291–2295. [Google Scholar] [CrossRef] [PubMed]
- Ly, H.Q.; Kirtane, A.J.; Murphy, S.A.; Buros, J.; Cannon, C.P.; Braunwald, E.; Gibson, C.M. Association of platelet counts on presentation and clinical outcomes in ST-elevation myocardial infarction (from the TIMI trials). Am. J. Cardiol. 2006, 98, 1–5. [Google Scholar] [CrossRef]
- Samocha-Bonet, D.; Justo, D.; Rogowski, O.; Saar, N.; Abu-Abeid, S.; Shenkerman, G.; Shapira, I.; Berliner, S.; Tomer, A. Platelet counts and platelet activation markers in obese subjects. Mediat. Inflamm. 2008, 2008, 834153. [Google Scholar] [CrossRef]
- Osselaer, J.C.; Jamart, J.; Scheiff, J.M. Platelet distribution width for differential diagnosis of thrombocytosis. Clin. Chem. 1997, 43 Pt 1, 1072–1076. [Google Scholar] [CrossRef]
- Kim, J.Y.; Yoon, J.; Lim, C.S.; Choi, B.M.; Yoon, S.Y. Clinical significance of platelet-associated hematological parameters as an early supplementary diagnostic tool for sepsis in thrombocytopenic very-low-birth-weight infants. Platelets 2015, 26, 620–626. [Google Scholar] [CrossRef]
- Tamhane, U.U.; Aneja, S.; Montgomery, D.; Rogers, E.K.; Eagle, K.A.; Gurm, H.S. Association between admission neutrophil to lymphocyte ratio and outcomes in patients with acute coronary syndrome. Am. J. Cardiol. 2008, 102, 653–657. [Google Scholar] [CrossRef] [PubMed]
- Dong, C.H.; Wang, Z.M.; Chen, S.Y. Neutrophil to lymphocyte ratio predict mortality and major adverse cardiac events in acute coronary syndrome: A systematic review and meta-analysis. Clin. Biochem. 2018, 52, 131–136. [Google Scholar] [CrossRef]
- Templeton, A.J.; McNamara, M.G.; Šeruga, B.; Vera-Badillo, F.E.; Aneja, P.; Ocaña, A.; Leibowitz-Amit, R.; Sonpavde, G.; Knox, J.J.; Tran, B.; et al. Prognostic role of neutrophil-to-lymphocyte ratio in solid tumors: A systematic review and meta-analysis. J. Natl. Cancer Inst. 2014, 106, dju124. [Google Scholar] [CrossRef]
- Özturk, Z.A.; Yesil, Y.; Kuyumcu, M.E.; Bilici, M.; Özturk, N.; Yesil, N.K.; Özkaya, M.; Kısacık, B.; Kepekçi, Y.; Arıoğul, S. Inverse relationship between neutrophil lymphocyte ratio (NLR) and bone mineral density (BMD) in elderly people. Arch. Gerontol. Geriatr. 2013, 57, 81–85. [Google Scholar] [CrossRef]
- Yilmaz, H.; Uyfun, M.; Yilmaz, T.S.; Namuslu, M.; Inan, O.; Taskin, A.; Cakmak, M.; Bilgic, M.A.; Bavbek, N.; Akcay, A.; et al. Neutrophil-lymphocyte ratio may be superior to C-reactive protein for predicting the occurrence of postmenopausal osteoporosis. Endocr. Regul. 2014, 48, 25–33. [Google Scholar] [CrossRef] [PubMed]
- Huang, C.; Li, S. Association of blood neutrophil lymphocyte ratio in the patients with postmenopausal osteoporosis. Pak. J. Med. Sci. 2016, 32, 762–765. [Google Scholar] [CrossRef] [PubMed]
- Lee, S.H.; Ryu, S.Y.; Park, J.; Shin, M.H.; Han, M.A.; Choi, S.W. The relationship of neutrophil-lymphocyte ratio and platelet-lymphocyte ratio with bone mineral density in Korean postmenopausal women. Chonnam Med. J. 2019, 55, 150–155. [Google Scholar] [CrossRef]
- Eroglu, S.; Karatas, G. Platelet/lymphocyte ratio is an independent predictor for osteoporosis. Saudi Med. J. 2019, 40, 360–366. [Google Scholar] [CrossRef]
- Koseoglu, S.B. Bone loss & platelet-to-lymphocyte ratio. Biomark. Med. 2017, 11, 5–10. [Google Scholar]
- Fang, H.; Zhang, H.; Wang, Z.; Zhou, Z.; Li, Y.; Lu, L. Systemic immune-inflammation index acts as a novel diagnostic biomarker for postmenopausal osteoporosis and could predict the risk of osteoporotic fracture. J. Clin. Lab. Anal. 2020, 34, e23016. [Google Scholar] [CrossRef] [PubMed]
- Du, Y.N.; Chen, Y.J.; Zhang, H.Y.; Wang, X.; Zhang, Z.F. Inverse association between systemic immune-inflammation index and bone mineral density in postmenopausal women. Gynecol. Endocrinol. 2021, 37, 650–654. [Google Scholar] [CrossRef]
- Catalano, A.; Oliveri, C.; Natale, G.; Agostino, R.M.; Squadrito, G.; Gaudio, A.; Gembillo, G.; Marina, D.; Cernaro, V.; Longhitano, E.; et al. Renal function is associated with changes in bone mineral density in postmenopausal osteoporotic women treated with denosumab: Data from a retrospective cohort study. J. Clin. Med. 2024, 13, 6239. [Google Scholar] [CrossRef]
- Oliveri, C.; Xourafa, A.; Morabito, N.; Di Giovanni, A.; Lupo, E.; Basile, G.; Gaudio, A.; Catalano, A. Calf circumference predicts changes of bone mineral density in postmenopausal osteoporotic women receiving denosumab. Aging Clin. Exp. Res. 2025, 37, 141. [Google Scholar] [CrossRef] [PubMed]
- Cesari, M.; Pahor, M.; Lauretani, F.; Penninx, B.W.; Bartali, B.; Russo, R.; Cherubini, A.; Woodman, R.; Bandinelli, S.; Guralnik, J.M.; et al. Bone density and hemoglobin levels in older persons: Results from the InCHIANTI study. Osteoporos. Int. 2005, 16, 691–696. [Google Scholar] [CrossRef]
- Pepe, J.; Colangelo, L.; De Martino, V.; Occhiuto, M.; Iervolino, D.; Pasqualetti, P.; Minisola, S.; Cipriani, C. Study of the link between hematopoietic and skeletal systems in patients attending a referral center for osteoporosis. J. Endocrinol. Investig. 2023, 46, 2391–2397. [Google Scholar] [CrossRef]
- Zhu, H.; Li, Z.; Zhou, Y.; Zheng, R.; Diao, C.; Li, K.; Feng, Q.; Wang, D. Neutrophil-lymphocyte ratio as a risk factor for osteoporotic vertebrae fractures and femoral neck fractures. Medicine 2022, 101, e32125. [Google Scholar] [CrossRef]
- De Pablo, P.; Cooper, M.S.; Buckley, C.D. Association between bone mineral density and C-reactive protein in a large population-based sample. Arthritis Rheum. 2012, 64, 2624–2631. [Google Scholar] [CrossRef]
- Wu, Z.J.; He, J.L.; Wei, R.Q.; Liu, B.; Lin, X.; Guan, J.; Lan, Y.B. Creactive protein and risk of fracture: A systematic review and doseresponse meta-analysis of prospective cohort studies. Osteoporos. Int. 2015, 26, 49–57. [Google Scholar] [CrossRef]
- Lin, C.C.; Li, T.C.; Liu, C.S.; Yang, C.W.; Lin, C.H.; Hsiao, J.H.; Meng, N.H.; Lin, W.Y.; Liao, L.N.; Li, C.I.; et al. Associations of TNF-alpha and IL-6 polymorphisms with osteoporosis through joint effects and interactions with LEPR gene in Taiwan: Taichung Community Health Study for Elders (TCHS-E). Mol. Biol. Rep. 2016, 43, 1179–1191. [Google Scholar] [CrossRef] [PubMed]
- Akbas, E.M.; Gungor, A.; Ozcicek, A.; Akbas, N.; Askin, S.; Polat, M. Vitamin D and inflammation: Evaluation with neutrophil-to-lymphocyte ratio and platelet-to-lymphocyte ratio. Arch. Med. Sci. 2016, 12, 721–727. [Google Scholar] [CrossRef]
- Elizondo-Montemayor, L.; Castillo, E.C.; Rodríguez-López, C.; Villarreal-Calderón, J.R.; Gómez-Carmona, M.; Tenorio-Martínez, S.; Nieblas, B.; García-Rivas, G. Seasonal Variation in Vitamin D in Association with Age, Inflammatory Cytokines, Anthropometric Parameters, and Lifestyle Factors in Older Adults. Mediat. Inflamm. 2017, 2017, 5719461. [Google Scholar] [CrossRef] [PubMed]
- Bellone, F.; Catalano, A.; Sottile, A.R.; Gaudio, A.; Loddo, S.; Corica, F.; Morabito, N. Early Changes of VEGF Levels After Zoledronic Acid in Women With Postmenopausal Osteoporosis: A Potential Role of Vitamin D. Front. Med. 2021, 8, 748438. [Google Scholar] [CrossRef] [PubMed]
- Atteritano, M.; Mirarchi, L.; Venanzi-Rullo, E.; Santoro, D.; Iaria, C.; Catalano, A.; Lasco, A.; Arcoraci, V.; Lo Gullo, A.; Bitto, A.; et al. Vitamin D Status and the Relationship with Bone Fragility Fractures in HIV-Infected Patients: A Case Control Study. Int. J. Mol. Sci. 2018, 19, 119. [Google Scholar] [CrossRef]
- Zhang, P.; Xu, Q.; Zhu, R. Vitamin D and allergic diseases. Front. Immunol. 2024, 15, 1420883. [Google Scholar] [CrossRef]
- Oteri, G.; Cicciù, M.; Peditto, M.; Catalano, A.; Loddo, S.; Pisano, M.; Lasco, A. Does Vitamin D3 Have an Impact on Clinical and Biochemical Parameters Related to Third Molar Surgery. J. Craniofac. Surg. 2016, 27, 469–476. [Google Scholar] [CrossRef] [PubMed]
- Hamza, F.N.; Daher, S.; Fakhoury, H.M.A.; Grant, W.B.; Kvietys, P.R.; Al-Kattan, K. Immunomodulatory Properties of Vitamin D in the Intestinal and Respiratory Systems. Nutrients 2023, 15, 1696. [Google Scholar] [CrossRef] [PubMed]
- Lauretani, F.; Salvi, M.; Zucchini, I.; Testa, C.; Cattabiani, C.; Arisi, A.; Maggio, M. Relationship between Vitamin D and Immunity in Older People with COVID-19. Int. J. Environ. Res. Public Health 2023, 20, 5432. [Google Scholar] [CrossRef]
- De Martinis, M.; Allegra, A.; Sirufo, M.M.; Tonacci, A.; Pioggia, G.; Raggiunti, M.; Ginaldi, L.; Gangemi, S. Vitamin D Deficiency, Osteoporosis and Effect on Autoimmune Diseases and Hematopoiesis: A Review. Int. J. Mol. Sci. 2021, 22, 8855. [Google Scholar] [CrossRef]
- Xue, Y.; Bao, W.; Huang, W.; Zou, X.; Guo, Y. Relationship between neutrophil-to-lymphocyte ratio, monocyte-to-lymphocyte ratio, platelet-to-lymphocyte ratio and osteoporosis in postmenopausal type 2 diabetic patients: A retrospective study. Medicine 2024, 103, e40869. [Google Scholar] [CrossRef]
- Yin, W.; Li, X.; Zheng, S.; Lai, W.; Chen, C.; He, X.; Gong, K.; He, K.; Hu, S.; Zheng, J.; et al. Association of novel inflammatory markers with osteoporosis index in older spine osteoporosis patients: NHANES 1999-2018 cross-sectional study. Sci. Rep. 2025, 15, 9128. [Google Scholar] [CrossRef]
- Gaudio, A.; Xourafa, A.; Zanoli, L.; Rapisarda, R.; Catalano, A.; Signorelli, S.S.; Castellino, P. Early vascular ageing biomarkers in osteoporotic outpatients: A pilot study. Sci. Rep. 2020, 10, 19421. [Google Scholar] [CrossRef] [PubMed]
- Sharafi, M.H.; Nazari, A.; Cheraghi, M.; Souri, F.; Bakhshesh, M. The link between osteoporosis and cardiovascular diseases: A review of shared mechanisms, risk factors, and therapeutic approaches. Osteoporos. Int. 2025, 36, 1129–1142. [Google Scholar] [CrossRef] [PubMed]
- Gaudio, A.; Fiore, V.; Rapisarda, R.; Sidoti, M.H.; Xourafa, A.; Catalano, A.; Tringali, G.; Zanoli, L.; Signorelli, S.S.; Fiore, C.E. Sclerostin is a possible candidate marker of arterial stiffness: Results from a cohort study in Catania. Mol. Med. Rep. 2017, 15, 3420–3424. [Google Scholar] [CrossRef]
- Wani, K.; Sabico, S.; Veronese, N.; Al-Masri, A.A.; Al-Daghri, N.M. Ten-year atherosclerotic cardiovascular disease risk score in post-menopausal women with low bone mineral density. Aging Clin. Exp. Res. 2025, 37, 56. [Google Scholar] [CrossRef] [PubMed]
- Wang, Z.; Wang, R.; Ge, H.; Gu, Y.; Xian, S.; Yan, L.; Du, G.; Shen, Z.; Lv, S.; Zhan, H.; et al. The correlation between coagulation biomarkers, bone turnover markers, and bone mineral density in Chinese adults aged ≥ 50 years. Arch. Med. Sci. 2024, 20, 1854–1863. [Google Scholar] [CrossRef] [PubMed]



| Total Participants (n = 124) | |
|---|---|
| Age (yr) | 68.4 ± 9 |
| Menopausal age (yr) | 49.8 ± 2.4 |
| BMI (kg/m2) | 24.8 ± 5.8 |
| Bone mineral density | |
| L1-L4 BMD (gr/cm2) | 0.8 (0.77 to 0.82) |
| Femur neck BMD (gr/cm2) | 0.62 (0.6 to 0.62) |
| Osteoporosis [n (%)] | 60 (48.4) |
| Osteopenia [n (%)] | 64 (51.6) |
| 10-yr probability of fracture | |
| Major osteoporotic (%) | 16 (14 to 18) |
| Hip fracture (%) | 5.4 (2.25 to 6.6) |
| Platelet count and indices | |
| Platelet count | 239,000 (230,000 to 251,016) |
| Mean Platelet Volume (MPV) (fL) | 10.2 (9.92 to 10.40) |
| Platelet Distribution Width (PDW) (%) | 16.1 (16.00 to 16.20) |
| Plateletcrit (PCT) (%) | 0.246 (0.23 to 0.26) |
| Platelet Large Cell Coefficient (P-LCC) (mm2) | 62,500 (59,000 to 73,652.35) |
| Platelet Large Cell Ratio (P-LCR) (%) | 27.35 (25.33 to 28.76) |
| Red blood cells (mm2) | 4511.921 ± 495.914 |
| White blood cells (mm2) | 7.241 ± 3.190 |
| Neutrophils (%) | 62 ± 9.7 |
| Lymphocytes (%) | 29.8 ± 9.3 |
| Inflammation markers | |
| Neutrophil-to-Lymphocyte Ratio (NLR) | 2.1 (1.875 to 2.250) |
| Platelet-to-Lymphocyte Ratio (PLR) | 132.12 (123.98 to 144.26) |
| Systemic immune inflammation index (SII) | 48.997 (45.473 to 55.480) |
| Vitamin D status | |
| 25(OH)D (ng/mL) | 42.3 ± 15.5 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Oliveri, C.; Xourafa, A.; Agostino, R.M.; Corigliano, V.; Botindari, A.; Gaudio, A.; Morabito, N.; Allegra, A.; Catalano, A. Exploring the Association Between Platelet Count, the Systemic Immune Inflammation Index, and Fracture Risk in Postmenopausal Women with Osteoporosis: A Cross-Sectional Study. J. Clin. Med. 2025, 14, 5453. https://doi.org/10.3390/jcm14155453
Oliveri C, Xourafa A, Agostino RM, Corigliano V, Botindari A, Gaudio A, Morabito N, Allegra A, Catalano A. Exploring the Association Between Platelet Count, the Systemic Immune Inflammation Index, and Fracture Risk in Postmenopausal Women with Osteoporosis: A Cross-Sectional Study. Journal of Clinical Medicine. 2025; 14(15):5453. https://doi.org/10.3390/jcm14155453
Chicago/Turabian StyleOliveri, Cecilia, Anastasia Xourafa, Rita Maria Agostino, Valentina Corigliano, Antonino Botindari, Agostino Gaudio, Nunziata Morabito, Alessandro Allegra, and Antonino Catalano. 2025. "Exploring the Association Between Platelet Count, the Systemic Immune Inflammation Index, and Fracture Risk in Postmenopausal Women with Osteoporosis: A Cross-Sectional Study" Journal of Clinical Medicine 14, no. 15: 5453. https://doi.org/10.3390/jcm14155453
APA StyleOliveri, C., Xourafa, A., Agostino, R. M., Corigliano, V., Botindari, A., Gaudio, A., Morabito, N., Allegra, A., & Catalano, A. (2025). Exploring the Association Between Platelet Count, the Systemic Immune Inflammation Index, and Fracture Risk in Postmenopausal Women with Osteoporosis: A Cross-Sectional Study. Journal of Clinical Medicine, 14(15), 5453. https://doi.org/10.3390/jcm14155453







