Abstract
Background: Midfacial fractures are common outcomes of facial trauma. While younger individuals typically sustain these injuries through high-energy events like assaults and traffic or sports accidents, elderly patients increasingly present with fractures from low-energy mechanisms, primarily falls. Purpose: The aim of this study was to analyze age- and gender-specific patterns in midfacial fractures over a 10-year period, with emphasis on elderly individuals and low-energy trauma. Methods: A retrospective review was performed of proven midfacial fractures between 2013 and 2022 at the Department of Oral and Maxillofacial Surgery (University of Pécs, Hungary). The patients were stratified by age (<65 vs. ≥65 years) and gender. The variables included the injury mechanism, fracture localization, the dental status, hospitalization, and the presence of associated injuries. Bivariate analyses were performed, and the significance level was set to p < 0.05. Results: A total of 957 radiologically confirmed midfacial fracture cases were evaluated, of whom 344 (35.9%) were ≥65 years old. In the elderly group, females had a 19-fold higher risk for midfacial trauma than younger females (OR: 19.1, 95%CI: 9.30–39.21). In the older group, a fall was significantly the most frequent injury mechanism (OR: 14.5; 95%CI: 9.9–21.3), responsible for 89.5% of the cases, while hospitalization (OR: 0.36; 95%CI: 0.23–0.56) was less characteristic. Most of the fractures occurred in the zygomatic bone, in the zygomaticomaxillary complex, or in the anterior wall of the maxilla. Associated injuries in the elderly group included mostly lower limb injuries—particularly pertrochanteric femoral fractures in females—and upper limb injuries, with a slight male dominance. Conclusions: Low-energy falls are the primary cause of midfacial fractures in elderly patients, particularly in women. Tailored prevention and management strategies are essential for improving the outcomes in this growing demographic group.
1. Introduction
Midfacial fractures constitute a substantial portion of maxillofacial trauma and are traditionally linked to high-energy mechanisms such as interpersonal violence and road traffic accidents [1,2,3,4]. However, the increasing proportion of elderly individuals in the global population has led to a notable shift in the etiology and presentation of such injuries. In this demographic, low-energy trauma—particularly ground-level falls—has become the predominant cause [5,6,7].
Elderly patients present unique anatomical and physiological challenges in the context of facial trauma. Age-related osteopenia and osteoporosis, in conjunction with edentulism and diminished facial structural support, significantly increase the risk of a fracture from relatively minor impacts [8,9,10]. These changes not only alter fracture patterns, but also influence management strategies [11,12,13,14]. In many cases, conservative treatment is favored due to limited physiological reserves, comorbidities, and reduced functional and aesthetic expectations among older patients [6,15,16,17].
In addition to skeletal fragility, edentulism represents a key anatomical and functional risk factor in elderly patients who sustain midfacial trauma [8,10]. Tooth loss compromises the vertical dimension of occlusion and significantly alters maxillary and mandibular support, reducing the capacity of the masticatory system to absorb external forces. Consequently, even minor low-energy impacts may translate into the direct transmission of force to the midfacial bones, increasing the likelihood of a fracture.
Few studies have comprehensively addressed the intersection of the age, gender, and injury mechanism in midfacial trauma, particularly in Central and Eastern European populations [2,18]. Understanding these variables is critical for optimizing preventive strategies and tailoring therapeutic protocols to meet the specific needs of elderly patients [19,20].
The present study aimed to retrospectively analyze a 10-year cohort of patients with midfacial fractures in Hungary, at the University of Pécs, the Department of Oral and Maxillofacial Surgery. Emphasis was placed on identifying age- and gender-specific trends, with particular emphasis on the role of low-energy trauma and its implications for diagnoses, treatment planning, and resource allocation in geriatric care.
2. Materials and Methods
This retrospective cohort study was conducted at the Department of Oral and Maxillofacial Surgery, the University of Pécs, Hungary, and included patients diagnosed with midfacial fractures between January 2013 and December 2022. Patient data were retrieved from institutional electronic health records using ICD-10 diagnostic codes corresponding to midfacial fractures. Patients were included if they had radiologically (with CT) confirmed fractures involving the midfacial region (e.g., zygomatic complex, maxilla, frontal bone, orbital wall, Le Fort I–II–III, or naso-orbito-ethmoid (NOE) regionand when complete clinical documentation was available. Patients were excluded if they had incomplete medical records or when the fractures were limited to the mandible or nasal bone without midfacial involvement.
Patient data were retrospectively extracted from electronic medical records. All the data were fully anonymized in accordance with the General Data Protection Regulation (GDPR) prior to the analysis. The study variables included demographic characteristics (age, gender), the etiology of the injury (fall, traffic accident, assault, sports, other), fracture localization (i.e., the anatomical site of the fracture), and the hospitalization status (admitted to our maxillofacial institution, treated in external departments, or managed only on an outpatient basis). The analyzed variables further included the presence and location of associated injuries (e.g., head, upper/lower limb, trunk, orbital/nasal region) and the dental status of the elderly patient group. The dentition status was categorized as (i) patients with minor tooth loss and/or fixed dental prostheses (fewer than 3 teeth missing); (ii) patients with major tooth loss (more than 3 but fewer than 10 teeth missing); (iii) edentulous or partially edentulous patients with removable prostheses, and finally, (iv) completely edentulous patients without any prosthetic rehabilitation.
The patients then were stratified into two age groups: <65 years and ≥65 years, based on the World Health Organization (WHO)’s definition of elderly populations.
2.1. Ethical Approval
This study was approved by the Institutional Review Board of the University of Pécs (reference number: KK63973-1/2024). Due to the retrospective nature of the study, the requirement for informed consent was waived.
2.2. Statistical Analysis
Descriptive statistics were used to summarize the patient demographics and clinical characteristics. Categorical variables were analyzed with Pearson’s chi-square test, or Fisher’s exact test where appropriate (i.e., when the expected cell counts were below 5). MedCalc was used to compute univariate odds ratios [21]. A p-value < 0.05 was considered statistically significant. All the statistical analyses were performed using IBM SPSS Statistics, version 28.0 (IBM Corp., Armonk, NY, USA).
3. Results
3.1. Patient Demographics
A total of 957 patients with CT-confirmed midfacial fractures were included in this study. Of these, 620 were male and 337 were female. Among the patients under the age of 65 (n = 613), the majority were male (n = 477), while females constituted the majority (n = 201) in the elderly group (≥65 years; n = 344) (Figure 1). The mean age of the study population was 50.73 years (SD ± 24.82). Male patients had a mean age of 48.66 years (SD ± 20.69), whereas female patients were significantly older, with a mean age of 66.1 years (SD ± 19.1). Stratified by age, the <65-year subgroup had a mean age of 39.7 years (SD ± 14.0), while the ≥65-year group had a mean age of 77.41 years (SD ± 7.6).
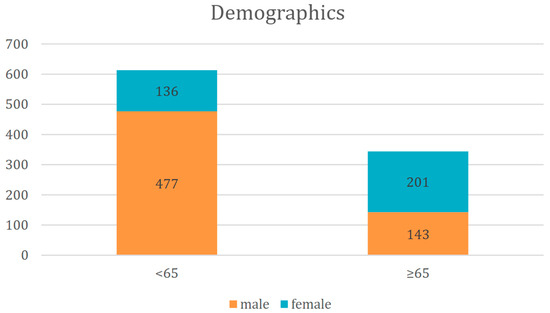
Figure 1.
Distribution of patients by age and gender.
3.2. Dental Status in the Elderly Population
In the ≥65-year-old patient group (n = 344), the dental status of the patients was as follows: 28 patients had minor tooth loss and/or fixed dental prostheses (8.1%); 114 patients had major tooth loss (33.1%); 92 patients were edentulous or partially edentulous, but had removable prostheses (26.7%); and 110 patients were completely edentulous without any prosthetic rehabilitation (32.0%). Midfacial fractures showed a ~16-times higher occurrence (OR: 16.05, 95%CI: 10.32–24.98, p < 0.001) in patients with total or subtotal tooth loss than in patients with only minor (<3 teeth missing) tooth loss. A further analysis regarding the correlation of the dental status with specific fracture patterns was not performed in the primary analysis due to inconsistent documentation and subgroup heterogeneity.
3.3. Etiology of Midfacial Fractures
Falls were the most common cause of injury among elderly patients (≥65 years), accounting for 89.5% of cases, in contrast to 37.1% in the younger group (<65 years). In the <65 cohort, assaults (32.2%) and traffic accidents (22.1%), i.e., non-fall causes, were predominant when considering the etiology (Table 1). The chi-square test confirmed that this age-related difference in trauma mechanisms was statistically significant (p < 0.001).

Table 1.
Distribution and odds ratios of injury mechanisms in patients aged <65 vs. ≥65 years.
3.4. Gender-Specific Injury Patterns
Across all age groups, fall-related fractures were significantly more frequent in females (76.9%) than in males (44.7%). In the elderly subgroup, 95.0% of the fractures in females and 81.8% in males resulted from falls (Figure 2). Falls were more common in individuals aged 65 and older (89.5%) compared to those under 65 (37.1%) (Figure 3). Conversely, traffic accidents (6.7% vs. 22.2%), sports-related injuries (0.3% vs. 6.9%), and assault-related injuries (3.2% vs. 32.3%) were more frequent in the younger age group (Figure 4). The association among gender, age, and the fall-related etiology was statistically significant (p < 0.001).
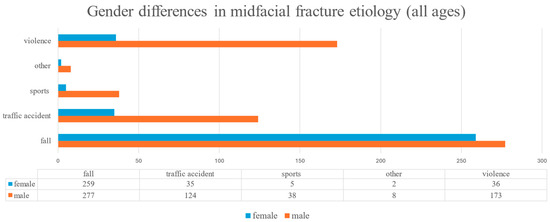
Figure 2.
Gender-specific distribution of midfacial fracture etiology across all age groups.
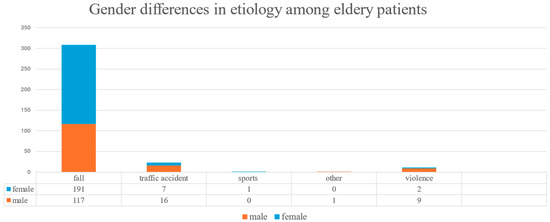
Figure 3.
Gender differences in midfacial fracture etiology among elderly patients (≥65 years).
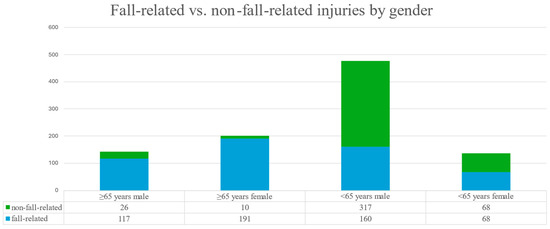
Figure 4.
Distribution of fall-related vs. non-fall-related injuries by gender and age group.
An age- and sex-stratified analysis revealed significant differences in the fall-related midfacial fracture risk. Elderly men (≥65 years) had a nearly 10-fold higher chance for such injuries compared to younger men (OR = 9.92, 95%CI: 5.60–14.20, p < 0.001). This age-related increase was even more pronounced in women, where elderly females had a 19-fold higher risk compared to younger females (OR = 19.1, 95% CI: 9.30–39.21, p < 0.001) (Table 2).

Table 2.
The correlation between gender, age, and fall-related injuries.
In terms of gender differences, elderly females had a more than four-times higher chance of experiencing a fall-related fracture than their male counterparts (OR = 4.24, 95% CI: 1.98–9.12, p = 0.001). Among younger patients, females also showed a nearly twofold increased risk compared to younger males (OR = 1.98, 95% CI: 1.35–2.92, p < 0.001) (Table 2). These findings emphasize that the female sex and an advanced age act synergistically, placing elderly women at the highest overall risk for fall-related midfacial fractures.
3.5. Hospitalization Patterns
Patients with fall-related injuries were much more likely to be treated as outpatients, while non-fall-related injuries were more often managed in a hospital setting (Figure 5). Outpatient cases were ~6.6 times more likely to present fall-related injuries compared to hospitalized patients (Table 3, Figure 5). On average, one in five patients from the younger patient group (<65 years and one in ten patients from the elderly group (≥65 years) were hospitalized in our maxillofacial department (p < 0.001) (Table 3). However, when considering all kinds of hospitalizations (including those in other departments), 27.6% of elderly patients (≥65 years) and 20.4% of younger patients (<65 years) were treated as inpatients. Overall, elderly individuals were ~1.5 times more likely to be treated as inpatients; however, this occurred significantly less frequently in the maxillofacial department. The average length of hospitalization was 2.4 ± 1.3 days in our maxillofacial surgery department; it was 9.2 ± 3.7 days in other (traumatology, neurology, intensive care) departments.
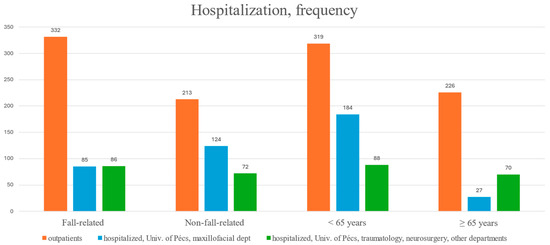
Figure 5.
Hospitalization status by age and trauma etiology.

Table 3.
Univariate odds ratios of the effect of injury mechanism and age on hospitalization.
3.6. Associated Injuries
Among 957 patients, detailed data on the localization of concomitant injuries were available for 75 individuals. Notably, all 75 cases with documented concomitant injuries were hospitalized in external departments of the University of Pécs, primarily in the traumatology, otorhinolaryngology, or neurosurgery units (Figure 6). These records allowed for subgroup analyses based on both sex and age. The injury patterns differed notably by both sex and age. Elderly patients (≥65 years) most frequently sustained lower limb injuries (n = 31), which were almost exclusively absent in the younger group (<65 years). Upper limb injuries were also more common among the elderly (n = 20 vs. n = 2), while head/brain and trunk injuries were relatively evenly distributed. Females experienced more lower limb injuries (n = 19) than males (n = 12), whereas males showed a slightly higher frequency of upper limb and trunk trauma.
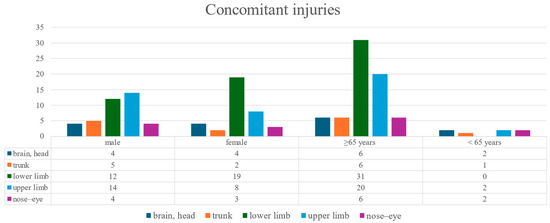
Figure 6.
Distribution of concomitant injuries by anatomical region and patient group.
We recorded only the most severe injury in polytraumatized patients; therefore, for example, we did not see associated lower limb injuries in the younger age group.
3.7. Fracture Localization in Elderly Fall Patients
Among elderly patients with fall-related injuries, the most frequently affected anatomical sites were the anterior maxillary wall (24.9%) the zygomaticomaxillary complex (17.9%), and the zygoma (17.9%). A statistically significant difference in fracture localization was found between elderly males and females (p = 0.047). Specifically, fractures involving the lateral maxillary wall (11.8% vs. 2.6%) and multiple maxillary walls (18.7% vs. 12.1%) were more frequent in women, while men had a higher proportion of zygomatic (24.1% vs. 17.6%) and zygomaticomaxillary (22.4% vs. 19.3%) fractures (Figure 7). These anatomical trends highlight the need for gender-sensitive diagnostic attention in geriatric trauma imaging.
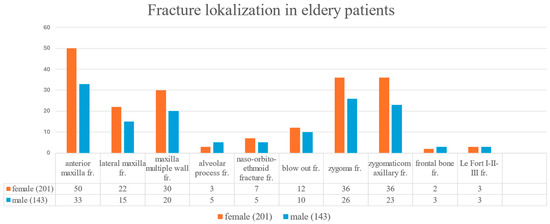
Figure 7.
Anatomical localization of midfacial fractures in elderly patients with fall-related injuries.
4. Discussion
One of the central aims of this study was to identify demographic patterns in fall-related midfacial fractures. Table 4 was included to provide a structured overview of these patterns by age and gender. Importantly, it not only summarizes the findings of the present study, but also places them in context with relevant data from the international literature. This comparison helps to interpret the synergistic effects of an advanced age and the female sex as combined risk factors in midfacial trauma etiology. This retrospective analysis confirms that low-energy falls are the leading cause of midfacial fractures in elderly patients, especially among women. The disproportionately high incidence in females aged ≥65 may be attributed to several interrelated factors, including osteoporosis [1,4,6], edentulism [8,13], and a generally higher fall risk [13,20]. Demographic factors may also contribute in Hungary; women over the age of 65 outnumber men by nearly 1.5 to 1 [22], which likely influences the gender distribution observed in fall-related injuries. These findings align with previous studies emphasizing the vulnerability of the aging midface due to a reduced bone density and diminished structural resilience [8,13,14,20].

Table 4.
Overview of age- and gender-specific patterns of fall-related midfacial fractures, as supported by findings in the present study and the relevant literature.
The fracture pattern in elderly patients differed markedly from that of younger individuals, with zygomatic and anterior maxillary wall fractures being most prevalent following falls [6,8,10,13,16]. In contrast, high-energy etiologies such as traffic accidents and interpersonal violence were more typical in the under-65 group [2,3,18]. The strong gender disparity in injury mechanisms—with women experiencing a higher rate of fall-related fractures—underscores the need for gender-sensitive prevention efforts.
The hospitalization rates were notably lower in elderly patients, and conservative management was more commonly employed in fall-related cases. This likely reflects both the low-impact nature of the trauma and a more cautious therapeutic approach, balancing surgical risks with expected functional benefits [6,15]. These trends echo findings in the maxillofacial trauma literature that advocate for individualized, age-adapted treatment plans in geriatric patients [3,5,23].
Our data also revealed that associated injuries—particularly to the lower extremities—are more common in elderly and female patients, suggesting the need for multidisciplinary trauma assessments and care [7,19]. The high prevalence of comorbidities and polypharmacy in this age group further reinforces the importance of integrating geriatric expertise into trauma management protocols [5,6,17,24]. Notably, international studies from Africa, India, Malaysia, and Poland have reported contrasting findings, with significantly fewer elderly patients and fall-related cases among midfacial fracture populations. This highlights the influence of differing demographic structures, healthcare access, and injury mechanisms across countries [9,14,18,19].
Table 4 summarizes the demographic characteristics of the studies referenced in the present analysis. Notably, in the reviewed literature as well as in our own data, fall-related midfacial fractures were typically associated with older age groups, further supporting the age-dependent nature of this trauma mechanism. Beyond surgical considerations, dental rehabilitation in elderly patients with midfacial trauma poses unique challenges. Age-related edentulism and a reduced bone quality often render even significant occlusal disturbances clinically less relevant, especially when the maxilla is involved [12,17]. Unlike mandibular trauma, maxillary fractures rarely result in complex prosthetic dilemmas due to the anatomical and functional characteristics of the upper arch [1,6,8,10]. However, a poor bone quality frequently contraindicates the use of dental implants [8], and the generally lower demand for advanced prosthetic care among elderly Hungarian patients compared to their Western European counterparts further reduces the clinical imperative for aggressive rehabilitation.
5. Limitations
This study has several limitations. First, its retrospective and single-center design may limit generalizability. Second, only the most severe associated injury was recorded in polytraumatized patients, which likely underestimates the total burden of trauma. Lastly, although the dentition status was documented in part, the data were incomplete and heterogeneous, which precluded a meaningful subgroup analysis regarding its influence on fracture patterns.
6. Conclusions
Midfacial fractures in elderly patients are predominantly the result of low-energy falls and often do not necessitate surgical intervention or hospitalization. The presence of comorbidities and elevated perioperative risks frequently supports a conservative treatment approach. Demographic factors—particularly a higher proportion of elderly women—appear to influence injury patterns. Recognizing these age- and gender-specific trauma profiles is essential for developing individualized care strategies and for avoiding overtreatment, particularly in cases where dental rehabilitation is unlikely to yield substantial functional or quality-of-life benefits due to anatomical limitations or socioeconomic constraints.
Author Contributions
Conceptualization, E.O.; methodology, E.O. and J.S.; formal analysis, L.M.; investigation, E.O.; data curation, E.O.; resources, J.S.; writing—original draft preparation, E.O. and Z.N.; writing—review and editing, J.S.; visualization, L.M.; supervision, J.S. and L.O.; project administration, E.O. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
This study was approved by the Regional and Institutional Research Ethics Committee of the University of Pécs (reference number: KK63973-1/2024, date of approval: 10 January 2024).
Informed Consent Statement
Due to the retrospective nature of the study and the use of anonymized medical records, the requirement for informed consent was waived by the ethics committee.
Data Availability Statement
The raw data supporting the conclusions of this article will be made available by the authors on request.
Acknowledgments
The authors thank the Department of Radiology and the hospital archives team for their valuable assistance in data collection and management.
Conflicts of Interest
The authors declare no conflicts of interest related to this study.
References
- Atisha, D.M.; Burr, T.V.R.; Allori, A.C.; Puscas, L.; Erdmann, D.; Marcus, J.R. Facial Fractures in the Aging Population. Plast. Reconstr. Surg. 2016, 137, 39–49. [Google Scholar] [CrossRef]
- Brucoli, M.; Boffano, P.; Romeo, I.; Corio, C.; Benech, A.; Ruslin, M.; Forouzanfar, T.; Starch-Jensen, T.; Rodríguez-Santamarta, T.; de Vicente, J.S.; et al. Management of Maxillofacial Trauma in the Elderly: A European Multicenter Study. Dent. Traumatol. 2020, 36, 241–246. [Google Scholar] [CrossRef]
- Ogura, I.; Hirahara, N.; Muraoka, H.; Fukuda, T. Characteristics of Maxillofacial Fractures in Elderly Patients Compared with Young Patients. Int. J. Oral-Med. Sci. 2016, 15, 10–16. [Google Scholar] [CrossRef]
- Kloss, F.R.; Stigler, R.G.; Brandstätter, A.; Tuli, T.; Rasse, M.; Laimer, K.; Hächl, O.L.; Gassner, R. Complications Related to Midfacial Fractures: Operative Versus Non-Surgical Treatment. Int. J. Oral Maxillofac. Surg. 2011, 40, 33–37. [Google Scholar] [CrossRef]
- Bettschen, D.; Kronenberg, J.; Kruse, A.; Rücker, M.; Wanner, G.A.; Rücker, M. Epidemiology of maxillofacial trauma in elderly patients receiving oral anticoagulant or antithrombotic medication: A Swiss retrospective study. BMC Emerg. Med. 2024, 24, 39. [Google Scholar] [CrossRef]
- Yovev, T.; Burnic, A.; Kniha, K.; Knobe, M.; Hölzle, F.; Modabber, A. Surgical Management of Facial Fractures in Geriatric Patients. J. Craniofac. Surg. 2021, 32, 2082–2086. [Google Scholar] [CrossRef] [PubMed]
- Liu, F.C.; Halsey, J.N.; Oleck, N.C.; Lee, E.S.; Granick, M.S. Facial Fractures as a Result of Falls in the Elderly: Concomitant Injuries and Management Strategies. Craniomaxillofac. Trauma Reconstr. 2019, 12, 45–53. [Google Scholar] [CrossRef]
- Giacomin, M.; De Conto, F.; Siqueira, S.P.; Signori, P.H.; Eidt, J.M.S.; Sawazaki, R. Elderly patients with facial trauma: A ten-year review. Rev. Bras. Geriatr. Gerontol. 2017, 20, 618–623. [Google Scholar] [CrossRef]
- Agarwal, S.; Krishnan, M.; Arularasan, G.; Lakshmanan, S. Single Institutional Experience of Geriatric Maxillofacial Trauma Patients: A Retrospective Study. J. Korean Assoc. Oral Maxillofac. Surg. 2025, 51, 102–107. [Google Scholar] [CrossRef] [PubMed]
- Carvalho Filho, M.A.M.; Saintrain, M.V.L.; Dos Anjos, R.E.S.; Pinheiro, S.S.; Cardoso, L.C.P.; Moizan, J.A.H.; de Aguiar, A.S.W. Prevalence of Oral and Maxillofacial Trauma in Elders Admitted to a Reference Hospital in Northeastern Brazil. PLoS ONE 2015, 10, e0135813. [Google Scholar] [CrossRef]
- Meisgeier, A.; Pienkohs, S.; Dürrschnabel, F.; Moosdorf, L.; Neff, A. Epidemiologic Trends in Maxillofacial Trauma Surgery in Germany—Insights from the National DRG Database 2005–2022. J. Clin. Med. 2024, 13, 4438. [Google Scholar] [CrossRef]
- Chávez Serna, E.; Iñigo-Arroyo, F. Management of Facial Fractures in the Elderly Patient: Experience of the Orthognathic Surgery and Facial Trauma Clinic of the Gea González Hospital. J. Am. Coll. Surg. 2021, 233, e161–e162. [Google Scholar] [CrossRef]
- Stay, E.; Maschka, D. Falls in elderly people that result in facial injuries. Br. J. Oral Maxillofac. Surg. 2003, 41, 138–142. [Google Scholar] [CrossRef]
- Béogo, R.; Coulibaly, T.A.; Traoré, I.; Mabika, B.D.D.; Zoma, E. Facial Fractures in the Elderly: Epidemiology and Outcome in 103 Patients. Int. J. Clin. Oral Maxillofac. Surg. 2019, 4, 48–51. [Google Scholar] [CrossRef]
- Kokko, L.L.; Puolakkainen, T.; Suominen, A.; Snäll, J.; Thorén, H. Are the Elderly with Maxillofacial Injuries at Increased Risk of Associated Injuries? Br. J. Oral Maxillofac. Surg. 2022, 60, 387–392. [Google Scholar] [CrossRef]
- Kerschbaum, M.; Lang, S.; Henssler, L.; Ernstberger, A.; Alt, V.; Pfeifer, C.; Worlicek, M.; Popp, D. Influence of Oral Anticoagulation and Antiplatelet Drugs on Outcome of Elderly Severely Injured Patients. J. Clin. Med. 2021, 10, 1649. [Google Scholar] [CrossRef]
- Pagin, M.; Mabire, C.; Cotton, M.; Zingg, T.; Carron, P.N. Retrospective Analysis of Geriatric Major Trauma Patients Admitted in the Shock Room of a Swiss Academic Hospital: Characteristics and Prognosis. J. Clin. Med. 2020, 9, 1343. [Google Scholar] [CrossRef] [PubMed]
- Michalak, P.; Wyszyńska-Pawelec, G.; Szuta, M.; Hajto-Bryk, J.; Zapała, J.; Zarzecka, J.K. Fractures of the Craniofacial Skeleton in the Elderly: Retrospective Studies. Int. J. Environ. Res. Public Health 2021, 18, 11219. [Google Scholar] [CrossRef] [PubMed]
- Royan, S.J.; Hamid, A.L.; Kovilpillai, F.J.; Junid, N.Z.; Wan Mustafa, W.M. A Prospective Study on Elderly Patients with Facial Fractures in a Developing Country. Gerodontology 2008, 25, 124–128. [Google Scholar] [CrossRef] [PubMed]
- Kannus, P.; Niemi, S.; Parkkari, J. Rising incidence of fall-induced maxillofacial injuries among older adults. Aging Clin. Exp. Res. 2016, 28, 1127–1131. [Google Scholar] [CrossRef]
- MedCalc Software Ltd. Odds Ratio Calculator. Available online: https://www.medcalc.org/calc/odds_ratio.php (accessed on 18 June 2025).
- Klinger, A.; Monostori, J.; Spéder, Z. Demográfiai Atlasz—Magyarország népessége térben és időben; Központi Statisztikai Hivatal (KSH): Budapest, Hungary, 2021; Available online: https://www.ksh.hu/interaktiv/demoevk2023/terkepek/terkepek.html (accessed on 27 July 2025).
- Rahimpour, A.; Baxter, J.; Giangrosso, G.; Murphy, A.; Bown, P.; Denning, D.A.; Ray, P.; Rahman, B. Age-Related Patterns of Traumatic Facial Fractures in the Appalachian Tri-state Area: A Five-Year Retrospective Study. Cureus 2024, 16, e62090. [Google Scholar] [CrossRef] [PubMed]
- Atinga, A.; Shekkeris, A.; Fertleman, M.; Batrick, N.; Kashef, E.; Dick, E. Trauma in the Elderly Patient. Br. J. Radiol. 2018, 91, 20170739. [Google Scholar] [CrossRef] [PubMed]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).