Polytetrafluoroethylene Isolation of the Periodontal Sulcus for Cementation of Full Veneer Restorations Using a Biologically Oriented Preparation Technique (BOPT): An In Vitro Study
Abstract
1. Introduction
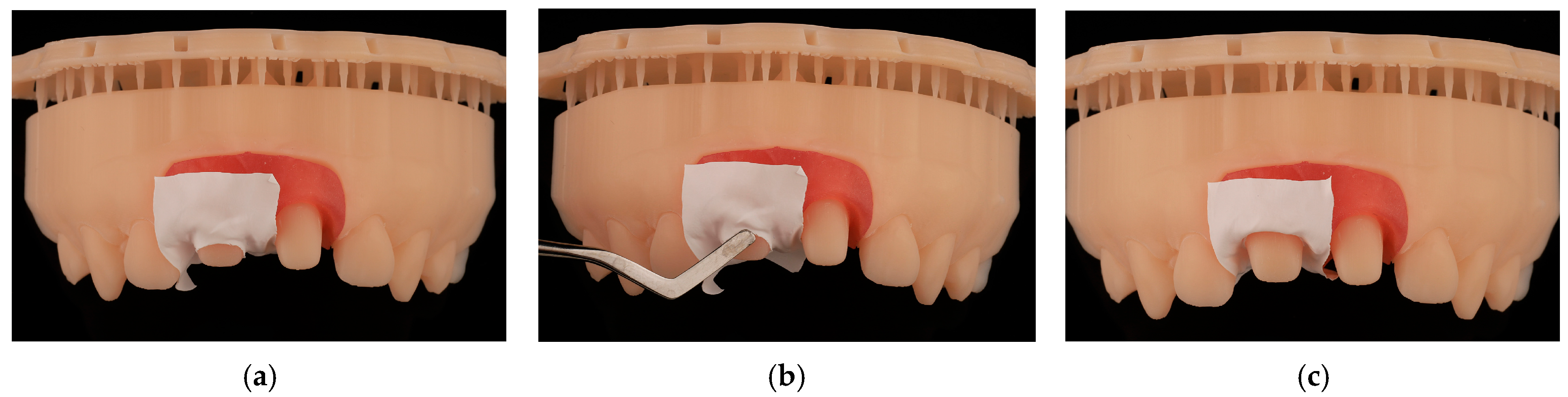
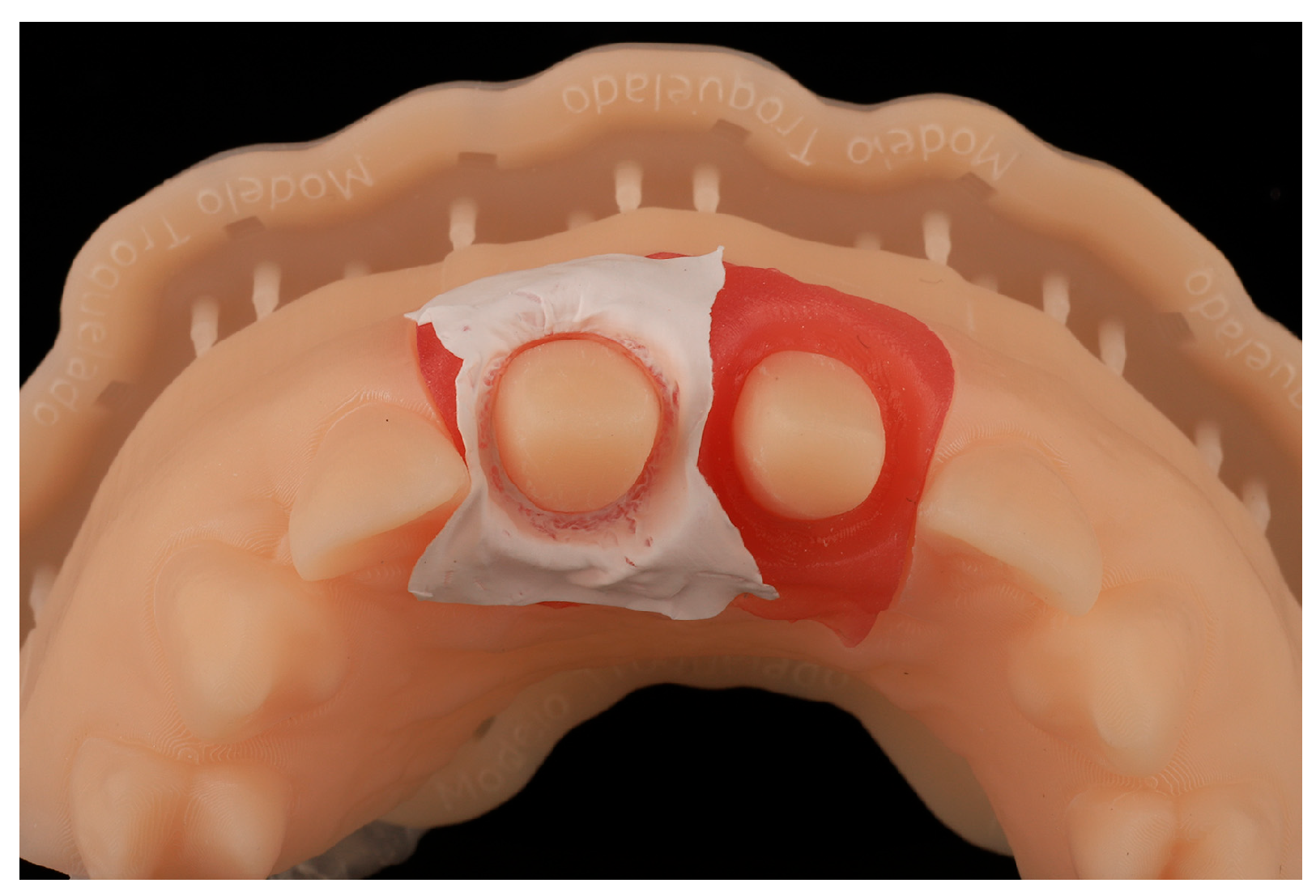
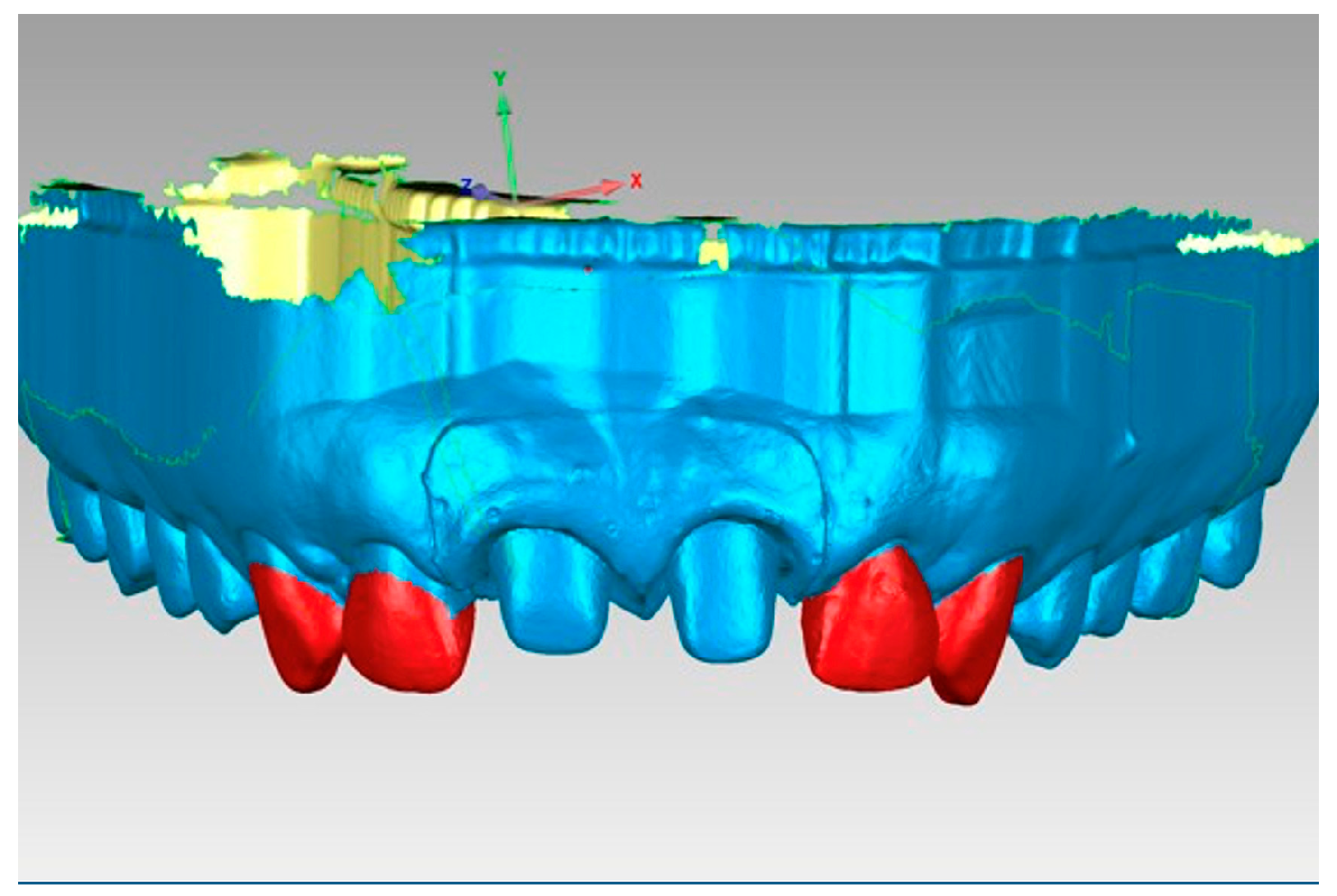
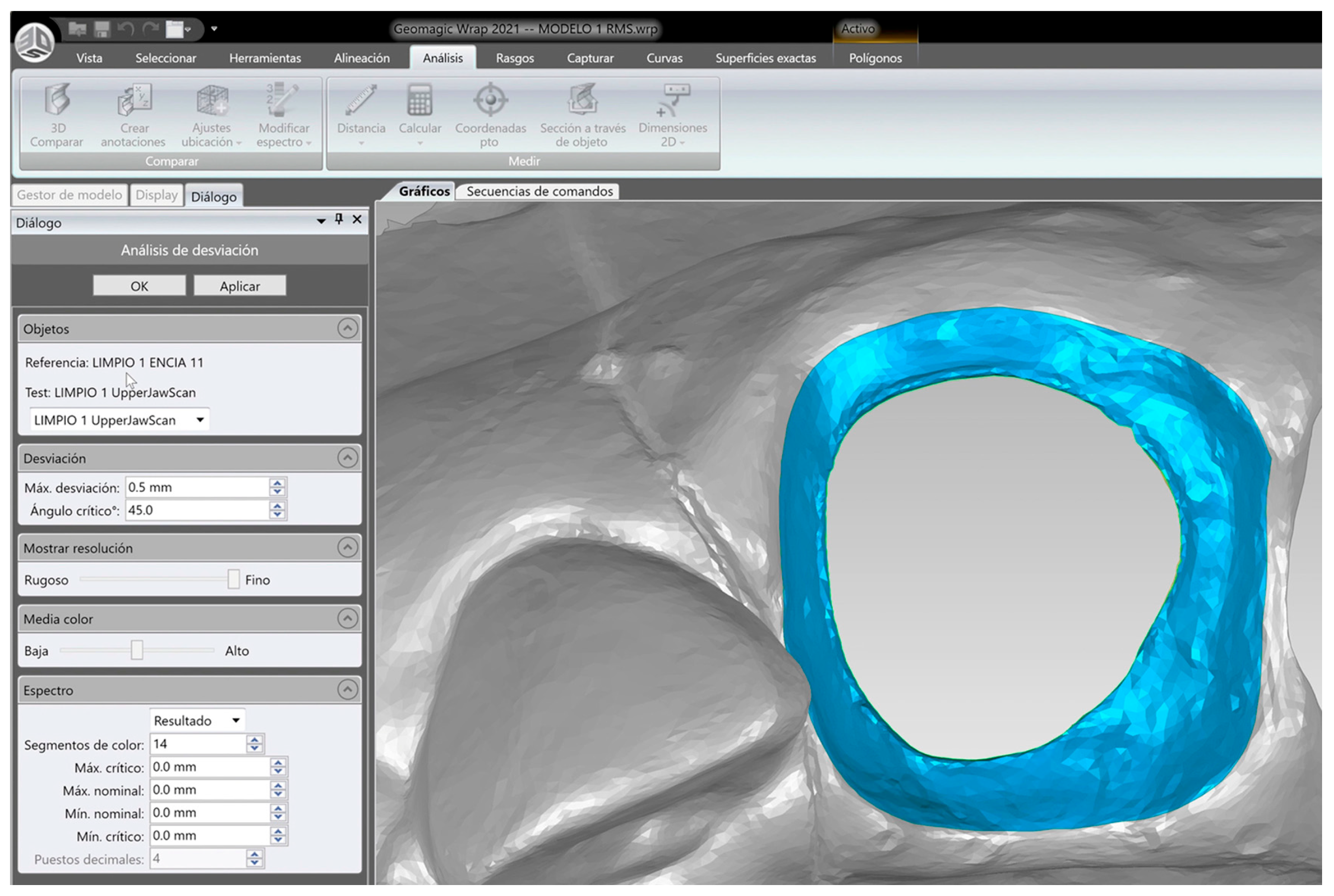
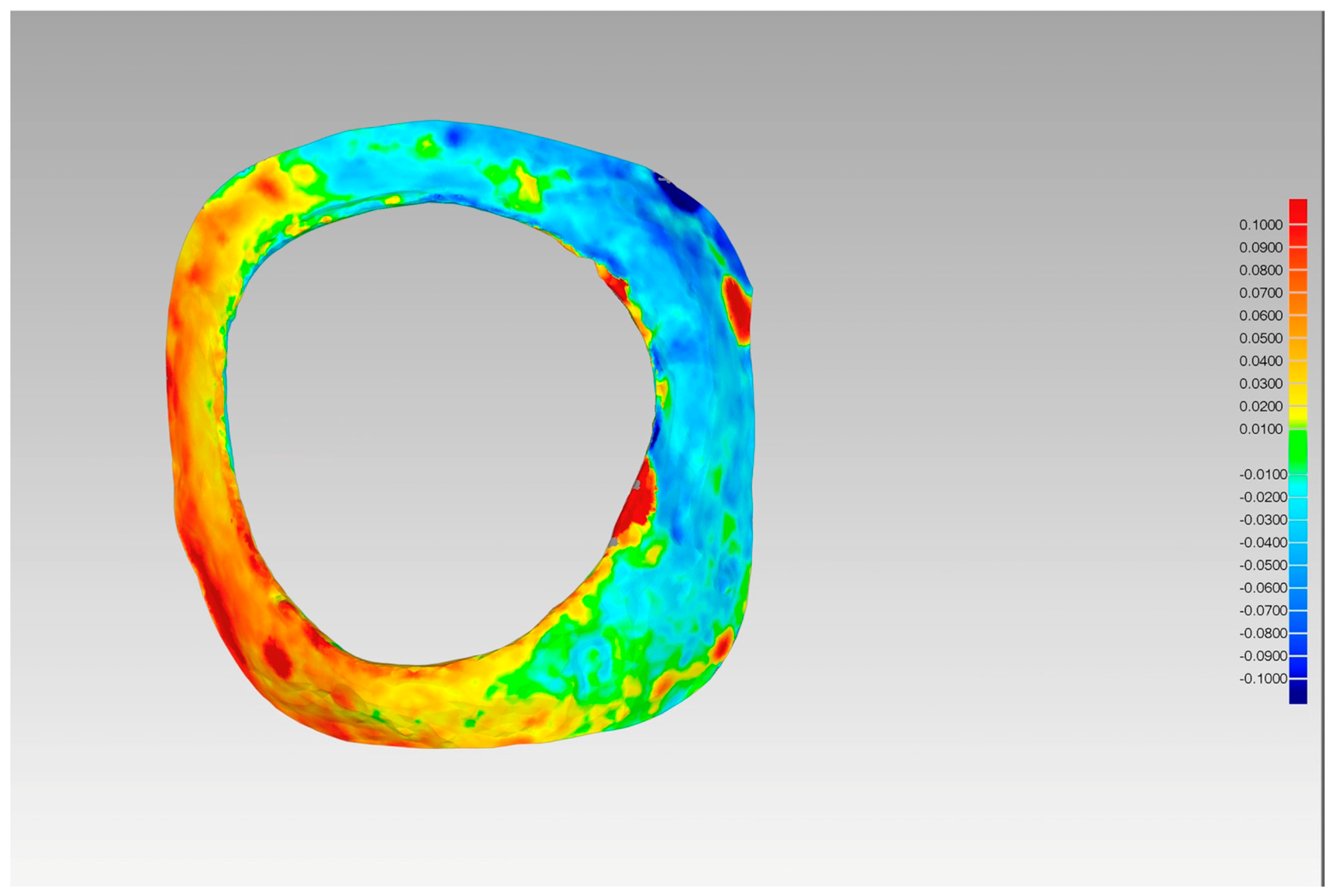
2. Materials and Methods
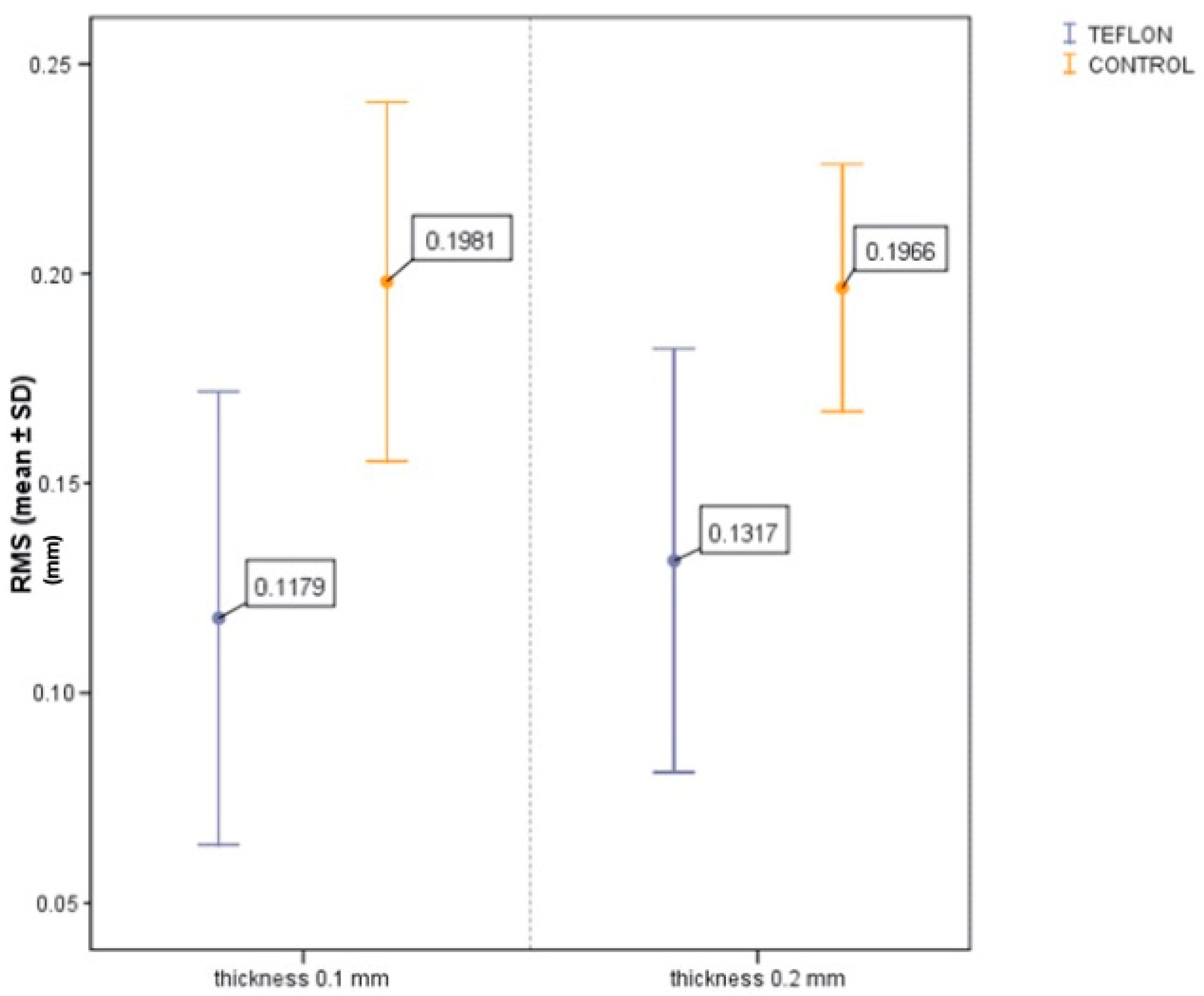
3. Results
4. Discussion
5. Conclusions
- PTFE tape is an effective alternative for relative isolation during BOPT cementation, significantly reducing excess cement in the gingival sulcus compared to no isolation.
- A 0.1 mm PTFE thickness performs similarly to 0.2 mm in terms of cement control, with the added benefit of better subgingival adaptability and easier handling.
- Rubber dam isolation is not feasible in BOPT preparations due to the convergent, subgingival design; PTFE offers a practical solution in these cases.
- All crowns in this study were splinted to ensure consistent seating pressure, eliminating variability in cementation force and insertion angle.
- The PTFE isolation technique is clinically applicable, but it requires careful manipulation to avoid dislodgement and ensure precise adaptation to the sulcus.
- While the study focused on temporary cementation, the findings are also relevant for permanent cementation, where excess resin cement poses an even greater risk for periodontal inflammation.
- Further clinical studies are needed to confirm these findings under intraoral conditions, including the presence of saliva, gingival fluid, temperature fluctuations, and plaque.
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Romanini-Junior, J.C.; Kumagai, R.Y.; Ortega, L.F.; Rodrigues, J.A.; Cassoni, A.; Hirata, R.; Reis, A.F. Adhesive/silane application effects on bond strength durability to a lithium disilicate ceramic. J. Esthet. Restor. Dent. 2018, 30, 346–351. [Google Scholar] [CrossRef]
- Wang, Y.; Li, C.; Yuan, H.; Wong, M.C.; Zou, J.; Shi, Z.; Zhou, X. Rubber dam isolation for restorative treatment in dental patients. Cochrane Database Syst. Rev. 2016, 9, CD009858. [Google Scholar] [CrossRef]
- Agustín-Panadero, R.; Martín-de Llano, J.J.; Fons-Font, A.; Carda, C. Histological study of human periodontal tissue following biologically oriented preparation technique (BOPT). J. Clin. Exp. Dent. 2020, 12, 597–602. [Google Scholar] [CrossRef]
- Agustín-Panadero, R.; Loi, I.; Fons-Badal, C.; Laguna-Martos, M.; Llobell-Cortell, A.; Serra-Pastor, B. Periodontal Behavior of Full-Coverage Restorations Using a Biologically Oriented Preparation Technique (BOPT): A 10-Year Prospective Clinical Study. Int. J. Periodontics Restor. Dent. 2025, 11, 1–23. [Google Scholar] [CrossRef]
- Serra-Pastor, B.; Bustamante-Hernández, N.; Fons-Font, A.; Fernanda Solá-Ruíz, M.; Revilla-León, M.; Agustín-Panadero, R. Periodontal Behavior and Patient Satisfaction of Anterior Teeth Restored with Single Zirconia Crowns Using a Biologically Oriented Preparation Technique: A 6-Year Prospective Clinical Study. J. Clin. Med. 2021, 10, 3482. [Google Scholar] [CrossRef]
- Serra-Pastor, B.; Loi, I.; Fons-Font, A.; Solá-Ruíz, M.F.; Agustín-Panadero, R. Periodontal and prosthetic outcomes on teeth prepared with biologically oriented preparation technique: A 4-year follow-up prospective clinical study. J. Prosthodont. Res. 2019, 63, 415–420. [Google Scholar] [CrossRef]
- Galli, F.; Deflorian, M.; Zucchelli, G.; Del Fabbro, M.; Testori, T. The biologically oriented preparation technique (BOPT) approach for preventing gingival recessions in fixed prosthodontics. A 5- to 13-year follow-up retrospective study. Int. J. Esthet. Dent. 2024, 19, 112–124. [Google Scholar]
- Sattar, M.M.; Patel, M.; Alani, A. Clinical applications of polytetrafluoroethylene (PTFE) tape in restorative dentistry. Br. Dent. J. 2017, 222, 151–158. [Google Scholar] [CrossRef]
- Loi, I.; Di Felice, A. Biologically oriented preparation technique (BOPT): A new approach for prosthetic restoration of periodontically healthy teeth. Eur. J. Esthet. Dent. 2013, 8, 10–23. [Google Scholar]
- Agustín-Panadero, R.; Solá-Ruíz, M.F. Vertical preparation for fixed prosthesis rehabilitation in the anterior sector. J. Prosthet. Dent. 2015, 114, 474–478. [Google Scholar] [CrossRef]
- Alani, A.; Bishop, K. Peri-implantitis. Part 2: Prevention and maintenance of peri-implant health. Br. Dent. J. 2014, 217, 289–297. [Google Scholar] [CrossRef]
- Roig-Vanaclocha, A.; Revilla-León, M.; Gómez-Polo, M.; Agustín-Panadero, R. Polytetrafluoroethylene relative isolation for adhesive cementation of dental restorations. J. Prosthet. Dent. 2024, 132, 26–30. [Google Scholar] [CrossRef]
- Kurian, N.; Varghese, K.G.; Wadhwa, S. A technique to avoid the entrapment of excess residual luting cement in soft-tissue irregularities underneath fixed dental prostheses by using polytetrafluoroethylene tape. J. Prosthet. Dent. 2023, 130, 271–272. [Google Scholar] [CrossRef]
- Araujo, E.; Perdigão, J. Anterior Veneer Restorations—An Evidence-based Minimal-Intervention Perspective. J. Adhes. Dent. 2021, 23, 91–110. [Google Scholar]
- Sirous, S.; Navadeh, A.; Ebrahimgol, S.; Atri, F. Effect of preparation design on marginal adaptation and fracture strength of ceramic occlusal veneers: A systematic review. Clin. Exp. Dent. Res. 2022, 8, 1391–1403. [Google Scholar] [CrossRef]
- Alghauli, M.A.; Alqutaibi, A.Y. 3D-printed intracoronal restorations, occlusal and laminate veneers: Clinical relevance, properties, and behavior compared to milled restorations; a systematic review and meta-analysis. J. Esthet. Restor. Dent. 2024, 36, 1153–1170. [Google Scholar] [CrossRef]
- Del Cisne Maldonado, K.; Espinoza, J.A.; Astudillo, D.A.; Delgado, B.A.; Bravo, W.D. Resistance of CAD/CAM composite resin and ceramic occlusal veneers to fatigue and fracture in worn posterior teeth: A systematic review. Dent. Med. Probl. 2024, 61, 417–426. [Google Scholar] [CrossRef]
- Badami, V.; Satya Priya, M.; Vijay, L.; Kethineni, H.; Akarapu, S.; Agarwal, S. Marginal Adaptation of Veneers: A Systematic Review. Cureus 2022, 14, e31885. [Google Scholar] [CrossRef]
- Djordjević, A.; Todić, J.; Simić, S.; Lazić, D.; Vlahović, Z.; Šubarić, L. The effect of different cementation techniques on the amount of remaining excess cement depending on the crown-abutment margin level. Vojn. Pregl. 2023, 80, 754–760. [Google Scholar] [CrossRef]
- Schuh, P.L.; Wachtel, H.; Bolz, W.; Maischberger, C.; Schenk, A.; Kühn, M. “Teflon tape technique”: Synergy between isolation and lucidity. Quintessence Int. 2019, 50, 488–493. [Google Scholar]
- Kuşçu, S.; Hayran, Y. Selection of Cement Materials and Isolation Techniques for the Effective Removal of Residual Cement in the Cementation. Clin. Implant. Dent. Relat. Res. 2025, 27, e70040. [Google Scholar] [CrossRef]
- Thimmappa, M.; Bhatia, M.; Somani, P.; Kumar, D.R.V. Comparative evaluation of three noninvasive gingival displacement systems: An in vivo study. J. Indian Prosthodont. Soc. 2018, 18, 122–130. [Google Scholar] [CrossRef]
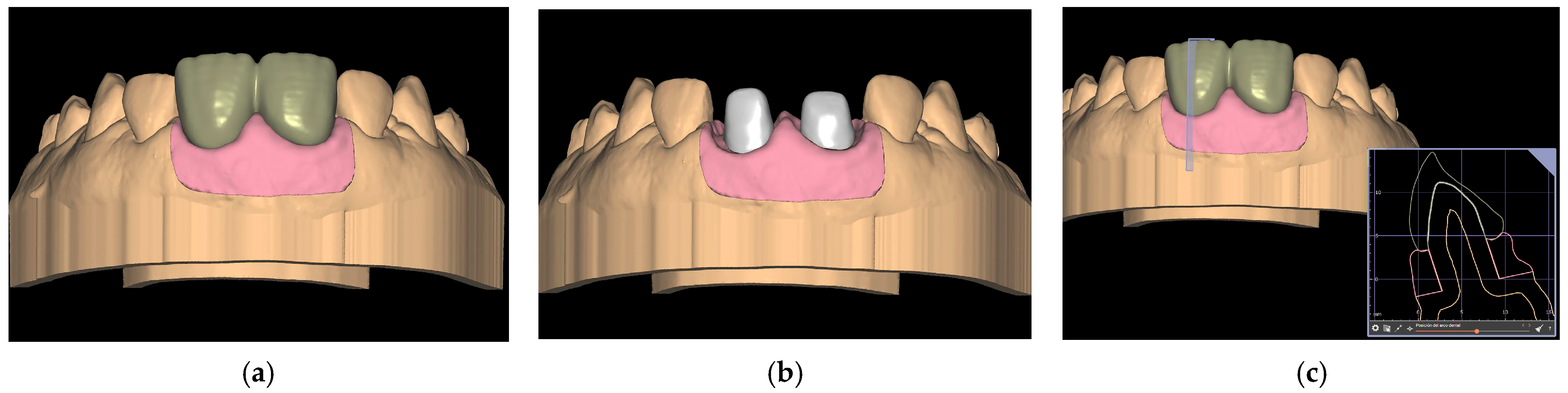
- Agustín-Panadero, R.; Loi, I.; Fernández-Estevan, L.; Chust, C.; Rech-Ortega, C.; Pérez-Barquero, J.A. Digital protocol for creating a virtual gingiva adjacent to teeth with subgingival dental preparations. J. Prosthodont. Res. 2020, 64, 506–514. [Google Scholar] [CrossRef]
- Papaspyridakos, P.; Chen, Y.W.; Alshawaf, B.; Kang, K.; Finkelman, M.; Chronopoulos, V.; Weber, H.P. Digital workflow: In vitro accuracy of 3D printed casts generated from complete-arch digital implant scans. J. Prosthet. Dent. 2020, 124, 589–593. [Google Scholar] [CrossRef]










Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Mañes, J.F.; Tripodi, F.; Pérez-Barquero, J.A.; Serra-Pastor, B.; Roig-Vanaclocha, A.; Maneiro-Lojo, J.; Loi, I.; Agustín-Panadero, R. Polytetrafluoroethylene Isolation of the Periodontal Sulcus for Cementation of Full Veneer Restorations Using a Biologically Oriented Preparation Technique (BOPT): An In Vitro Study. J. Clin. Med. 2025, 14, 5305. https://doi.org/10.3390/jcm14155305
Mañes JF, Tripodi F, Pérez-Barquero JA, Serra-Pastor B, Roig-Vanaclocha A, Maneiro-Lojo J, Loi I, Agustín-Panadero R. Polytetrafluoroethylene Isolation of the Periodontal Sulcus for Cementation of Full Veneer Restorations Using a Biologically Oriented Preparation Technique (BOPT): An In Vitro Study. Journal of Clinical Medicine. 2025; 14(15):5305. https://doi.org/10.3390/jcm14155305
Chicago/Turabian StyleMañes, José Félix, Federica Tripodi, Jorge Alonso Pérez-Barquero, Blanca Serra-Pastor, Ana Roig-Vanaclocha, Jesús Maneiro-Lojo, Ignazio Loi, and Rubén Agustín-Panadero. 2025. "Polytetrafluoroethylene Isolation of the Periodontal Sulcus for Cementation of Full Veneer Restorations Using a Biologically Oriented Preparation Technique (BOPT): An In Vitro Study" Journal of Clinical Medicine 14, no. 15: 5305. https://doi.org/10.3390/jcm14155305
APA StyleMañes, J. F., Tripodi, F., Pérez-Barquero, J. A., Serra-Pastor, B., Roig-Vanaclocha, A., Maneiro-Lojo, J., Loi, I., & Agustín-Panadero, R. (2025). Polytetrafluoroethylene Isolation of the Periodontal Sulcus for Cementation of Full Veneer Restorations Using a Biologically Oriented Preparation Technique (BOPT): An In Vitro Study. Journal of Clinical Medicine, 14(15), 5305. https://doi.org/10.3390/jcm14155305







