Changing Incidence, Aetiology and Outcomes of Prosthetic Joint Infections: A Population-Based Study in Iceland
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design, Sources of Data and Ethics Approval
2.2. Data Collection and Case Definitions
2.3. Epidemiology
2.4. Patient Involvement
2.5. Statistical Analysis
3. Results
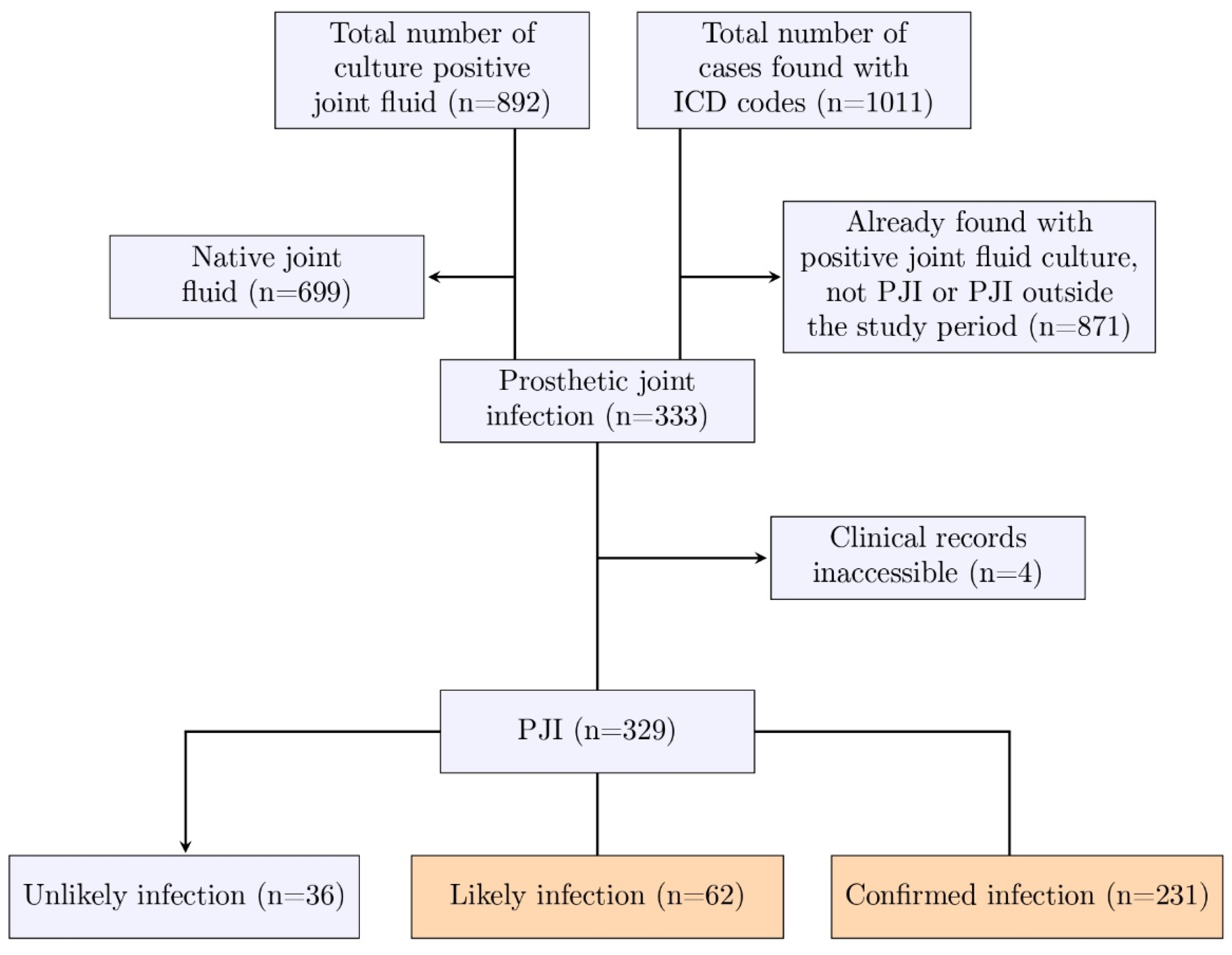
3.1. Identification of PJIs
3.2. Demographics and Clinical Characteristics
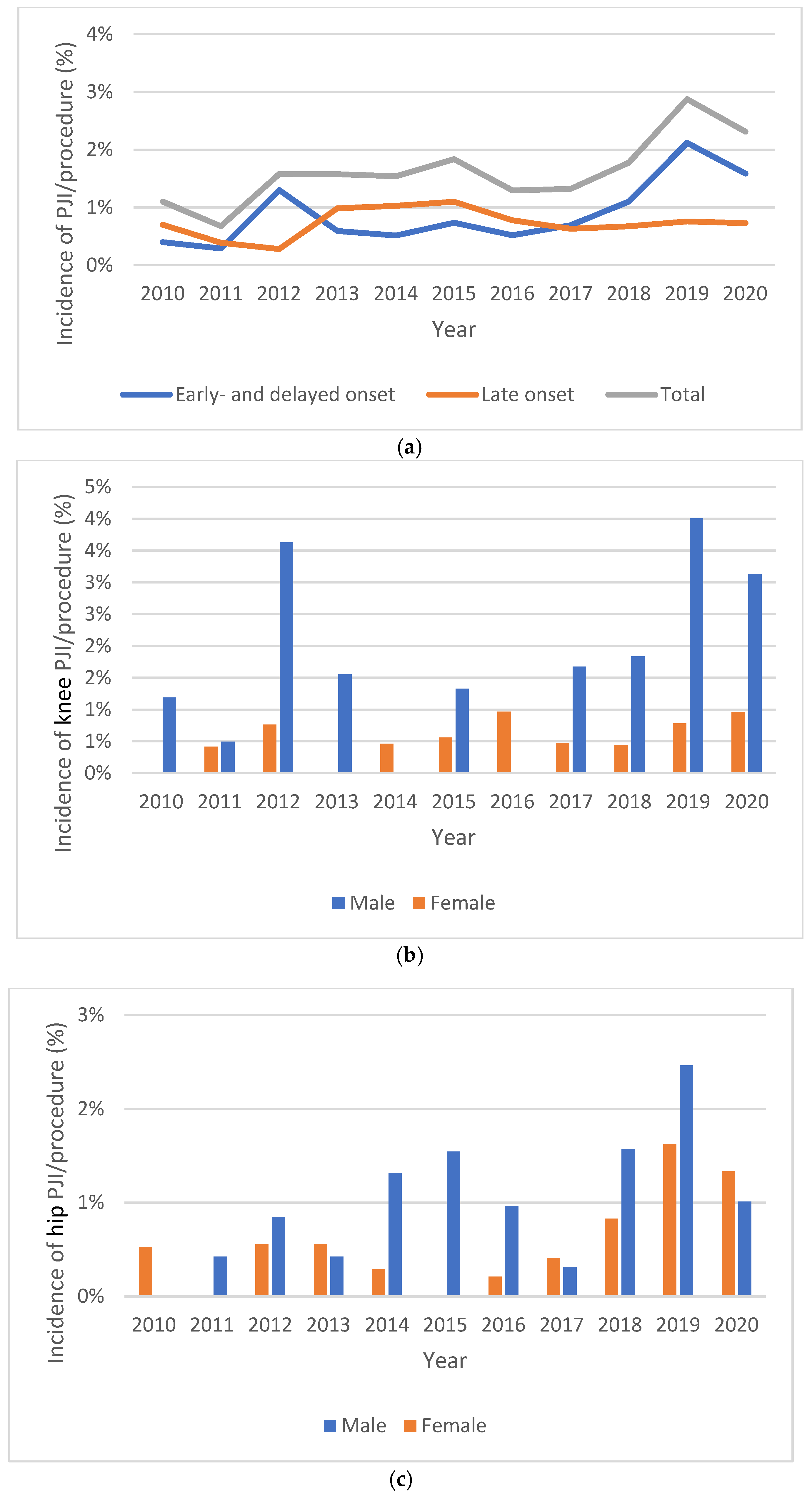
3.3. Incidence
3.4. Microbial Aetiology
3.5. Treatment and Outcome
4. Discussion
4.1. Clinical Characteristics
4.2. Diagnoses and Microbiology
4.3. Treatment Failure
4.4. Limitations
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| TJA | Total joint arthroplasty |
| PJI | Prosthetic joint infection |
| EBJIS | The European Bone and Joint Infection Society |
| DAIR | Debridement, antibiotics and implant retention |
| IRR | Incidence rate ratio |
| CoNS | Coagulase-negative staphylococcus |
| CN | Culture-negative |
| CP | Culture-positive |
References
- Kurtz, S.; Ong, K.; Lau, E.; Mowat, F.; Halpern, M. Projections of primary and revision hip and knee arthroplasty in the United States from 2005 to 2030. J. Bone Jt. Surg. Am. 2007, 89, 780–785. [Google Scholar] [CrossRef]
- Portillo, M.E.; Salvadó, M.; Sorli, L.; Alier, A.; Martínez, S.; Trampuz, A.; Gómez, J.; Puig, L.; Horcajada, J.P. Multiplex PCR of sonication fluid accurately differentiates between prosthetic joint infection and aseptic failure. J. Infect. 2012, 65, 541–548. [Google Scholar] [CrossRef]
- Ibrahim, M.S.; Twaij, H.; Haddad, F.S. Two-stage revision for the culture-negative infected total hip arthroplasty: A comparative study. Bone Jt. J. 2018, 100-B (Suppl. S1A), 3–8. [Google Scholar] [CrossRef]
- Akgün, D.; Müller, M.; Perka, C.; Winkler, T. The serum level of C-reactive protein alone cannot be used for the diagnosis of prosthetic joint infections, especially in those caused by organisms of low virulence. Bone Jt. J. 2018, 100-B, 1482–1486. [Google Scholar] [CrossRef]
- McNally, M.; Sousa, R.; Wouthuyzen-Bakker, M.; Chen, A.F.; Soriano, A.; Vogely, H.C.; Clauss, M.; Higuera, C.A.; Trebše, R. The EBJIS definition of periprosthetic joint infection. Bone Jt. J. 2021, 103-B, 18–25. [Google Scholar] [CrossRef]
- Sousa, R.; Ribau, A.; Alfaro, P.; Burch, M.A.; Ploegmakers, J.; McNally, M.; Clauss, M.; Wouthuyzen-Bakker, M.; Soriano, A. The European Bone and Joint Infection Society definition of periprosthetic joint infection is meaningful in clinical practice: A multicentric validation study with comparison with previous definitions. Acta Orthop. 2023, 94, 8–18. [Google Scholar] [CrossRef]
- Gerritsen, M.; Khawar, A.; Scheper, H.; van der Wal, R.; Schoones, J.; de Boer, M.; Nelissen, R.; Pijls, B. Modular component exchange and outcome of DAIR for hip and knee periprosthetic joint infection: A systematic review and meta-regression analysis. Bone Jt. Open. 2021, 2, 806–812. [Google Scholar] [CrossRef]
- Kunutsor, S.K.; Beswick, A.D.; Whitehouse, M.R.; Wylde, V.; Blom, A.W. Debridement, antibiotics and implant retention for periprosthetic joint infections: A systematic review and meta-analysis of treatment outcomes. J. Infect. 2018, 77, 479–488. [Google Scholar] [CrossRef]
- Brandt, C.M.; Sistrunk, W.W.; Duffy, M.C.; Hanssen, A.D.; Steckelberg, J.M.; Ilstrup, D.M.; Osmon, D.R. Staphylococcus aureus prosthetic joint infection treated with debridement and prosthesis retention. Clin. Infect. Dis. 1997, 24, 914–919. [Google Scholar] [CrossRef]
- Crockarell, J.R.; Hanssen, A.D.; Osmon, D.R.; Morrey, B.F. Treatment of infection with débridement and retention of the components following hip arthroplasty. J. Bone Jt. Surg. Am. 1998, 80, 1306–1313. [Google Scholar] [CrossRef]
- Scheper, H.; Gerritsen, L.M.; Pijls, B.G.; Van Asten, S.A.; Visser, L.G.; De Boer, M.G.J. Outcome of Debridement, Antibiotics, and Implant Retention for Staphylococcal Hip and Knee Prosthetic Joint Infections, Focused on Rifampicin Use: A Systematic Review and Meta-Analysis. Open Forum Infect. Dis. 2021, 8, ofab298. [Google Scholar] [CrossRef]
- Tornero, E.; Senneville, E.; Euba, G.; Petersdorf, S.; Rodriguez-Pardo, D.; Lakatos, B.; Ferrari, M.; Pilares, M.; Bahamonde, A.; Trebse, R.; et al. Characteristics of prosthetic joint infections due to Enterococcus sp. and predictors of failure: A multi-national study. Clin. Microbiol. Infect. 2014, 20, 1219–1224. [Google Scholar] [CrossRef]
- Bernaus, M.; Auñón-Rubio, Á.; Monfort-Mira, M.; Arteagoitia-Colino, I.; Martínez-Ros, J.; Castellanos, J.; Lamo-Espinosa, J.M.; Argüelles, F.; Veloso, M.; García, L.G.; et al. Risk Factors of DAIR Failure and Validation of the KLIC Score: A Multicenter Study of Four Hundred Fifty-Five Patients. Surg. Infect. 2022, 23, 280–287. [Google Scholar] [CrossRef]
- Nelson, S.B.; Pinkney, J.A.; Chen, A.F.; Tande, A.J. Periprosthetic Joint Infection: Current Clinical Challenges. Clin. Infect. Dis. 2023, 77, e34–e45. [Google Scholar] [CrossRef]
- Wouthuyzen-Bakker, M.; Sebillotte, M.; Lomas, J.; Taylor, A.; Palomares, E.B.; Murillo, O.; Parvizi, J.; Shohat, N.; Reinoso, J.C.; Sánchez, R.E.; et al. Clinical outcome and risk factors for failure in late acute prosthetic joint infections treated with debridement and implant retention. J. Infect. 2019, 78, 40–47. [Google Scholar] [CrossRef]
- Hvannberg, J.; Róbertsson, G.; Gestsson, J.; Ingvarsson, Þ. Knee arthroplasties performed at Akureyri University Hospital in the years 1983–2003. Læknablaðið 2005, 91, 739–746. [Google Scholar]
- Svansdóttir, S.; Einarsson, J.; Þorsteinsson, H. Úttekt á liðskiptaaðgerðum Klíníkurinnar Ármúla 2017–2021. Bachelor’s Thesis, University of Iceland, Reykjavík, Iceland, 2022. [Google Scholar]
- Zimmerli, W.; Trampuz, A.; Ochsner, P.E. Prosthetic-joint infections. N. Engl. J. Med. 2004, 351, 1645–1654. [Google Scholar] [CrossRef]
- Davis, J.S.; Metcalf, S.; Clark, B.; Robinson, J.O.; Huggan, P.; Luey, C.; McBride, S.; Aboltins, C.; Nelson, R.; Campbell, D.; et al. Predictors of Treatment Success After Periprosthetic Joint Infection: 24-Month Follow up From a Multicenter Prospective Observational Cohort Study of 653 Patients. Open Forum Infect Dis. 2022, 9, ofac048. [Google Scholar] [CrossRef]
- Wang, F.D.; Wang, Y.P.; Chen, C.F.; Chen, H.P. The incidence rate, trend and microbiological aetiology of prosthetic joint infection after total knee arthroplasty: A 13 years’ experience from a tertiary medical center in Taiwan. J. Microbiol. Immunol. Infect. 2018, 51, 717–722. [Google Scholar] [CrossRef]
- Pulido, L.; Ghanem, E.; Joshi, A.; Purtill, J.J.; Parvizi, J. Periprosthetic joint infection: The incidence, timing, and predisposing factors. Clin. Orthop. Relat. Res. 2008, 466, 1710–1715. [Google Scholar] [CrossRef]
- (MAC) MAC. Incidence and Predictors of Prosthetic Joint Infection Following Primary Total Knee Arthroplasty: A 15-Year Population-Based Cohort Study. J. Arthroplasty. 2022, 37, 367–372.e1. [Google Scholar] [CrossRef]
- (MAC) MAC. Risk Factors for Periprosthetic Joint Infection Following Primary Total Hip Arthroplasty: A 15-Year, Population-Based Cohort Study. J. Bone Jt. Surg. Am. 2020, 102, 503–509. [Google Scholar] [CrossRef]
- Zeng, Z.J.; Yao, F.M.; He, W.; Wei, Q.S.; He, M.C. Incidence of periprosthetic joint infection after primary total hip arthroplasty is underestimated: A synthesis of meta-analysis and bibliometric analysis. J. Orthop. Surg. Res. 2023, 18, 610. [Google Scholar] [CrossRef]
- Gundtoft, P.H.; Pedersen, A.B.; Schønheyder, H.C.; Overgaard, S. Validation of the diagnosis ‘prosthetic joint infection’ in the Danish Hip Arthroplasty Register. Bone Jt. J. 2016, 98-B, 320–325. [Google Scholar] [CrossRef]
- Lindgren, J.V.; Gordon, M.; Wretenberg, P.; Kärrholm, J.; Garellick, G. Validation of reoperations due to infection in the Swedish Hip Arthroplasty Register. BMC Musculoskelet. Disord. 2014, 15, 384. [Google Scholar] [CrossRef]
- Cortes-Penfield, N.; Krsak, M.; Damioli, L.; Henry, M.; Seidelman, J.; Hewlett, A.; Certain, L. How we approach suppressive antibiotic therapy (SAT) following debridement, antibiotics, and implant retention for prosthetic joint infection. Clin. Infect. Dis. 2023, 78, 188–198. [Google Scholar] [CrossRef]
- Moldovan, F. Role of Serum Biomarkers in Differentiating Periprosthetic Joint Infections from Aseptic Failures after Total Hip Arthroplasties. J. Clin. Med. 2024, 13, 5716. [Google Scholar] [CrossRef]
- Kurtz, S.M.; Lau, E.C.; Son, M.S.; Chang, E.T.; Zimmerli, W.; Parvizi, J. Are We Winning or Losing the Battle with Periprosthetic Joint Infection: Trends in Periprosthetic Joint Infection and Mortality Risk for the Medicare Population. J. Arthroplast. 2018, 33, 3238–3245. [Google Scholar] [CrossRef]
- Gunnlaugsdóttir, S.L.; Erlendsdóttir, H.; Helgason, K.O.; Geirsson, Á.; Thors, V.; Guðmundsson, S.; Gottfreðsson, M. Native joint infections in Iceland 2003–2017: An increase in postarthroscopic infections. Ann. Rheum. Dis. 2022, 81, 132–139. [Google Scholar] [CrossRef]
- Mironenko, C.M.; Kapadia, M.; Donlin, L.; Figgie, M.; Carli, A.V.; Henry, M.; Goodman, S.M.; O Miller, A. Sex Differences in Prosthetic Joint Infection. Open Forum Infect. Dis. 2021, 8 (Suppl. S1), S229. [Google Scholar] [CrossRef]
- Lemaignen, A.; Bernard, L.; Marmor, S.; Ferry, T.; Grammatico-Guillon, L.; Astagneau, P. Epidemiology of complex bone and joint infections in France using a national registry: The CRIOAc network. J. Infect. 2021, 82, 199–206. [Google Scholar] [CrossRef]
- Casenaz, A.; Piroth, L.; Labattut, L.; Sixt, T.; Magallon, A.; Guilloteau, A.; Neuwirth, C.; Amoureux, L. Epidemiology and antibiotic resistance of prosthetic joint infections according to time of occurrence, a 10-year study. J. Infect. 2022, 85, 492–498. [Google Scholar] [CrossRef]
- Reisener, M.; Perka, C. Do Culture-Negative Periprosthetic Joint Infections Have a Worse Outcome Than Culture-Positive Periprosthetic Joint Infections? A Systematic Review and Meta-Analysis. Biomed. Res. Int. 2018, 2018, 6278012. [Google Scholar] [CrossRef]
- Browning, S.; Manning, L.; Metcalf, S.; Paterson, D.L.; Robinson, J.O.; Clark, B.; Davis, J.S. Characteristics and outcomes of culture-negative prosthetic joint infections from the Prosthetic Joint Infection in Australia and New Zealand Observational (PIANO) cohort study. J. Bone Jt. Infect. 2022, 7, 203–211. [Google Scholar] [CrossRef]
- Sigmund, I.K.; Ferry, T.; Sousa, R.; Soriano, A.; Metsemakers, W.J.; Clauss, M.; Trebse, R.; Wouthuyzen-Bakker, M. Debridement, antimicrobial therapy, and implant retention (DAIR) as curative strategy for acute periprosthetic hip and knee infections: A position paper of the European Bone & Joint Infection Society (EBJIS). J. Bone Jt. Infect. 2025, 10, 101–138. [Google Scholar] [CrossRef]
| Early Onset a (n = 92) | Delayed Onset a (n = 65) | Late Onset a (n = 136) | Overall (n = 293) | p-Value b | |
|---|---|---|---|---|---|
| Gender | |||||
| Male | 55 (59.8%) | 43 (66.2%) | 78 (57.4%) | 176 (60.1%) | 0.445 |
| Female | 37 (40.2%) | 22 (33.8%) | 58 (42.6%) | 117 (39.9%) | |
| EBJIS criteria | |||||
| Likely PJI | 19 (20.7%) | 14 (21.5%) | 29 (21.3%) | 62 (21.2%) | 1.000 |
| Confirmed PJI | 73 (79.3%) | 51 (78.5%) | 107 (78.7%) | 231 (78.8%) | |
| Age (years) | |||||
| Median [IQR] | 69.1 [64.5–76.4] | 68.7 [62.9–75.9] | 71.0 [64.6–79.5] | 69.3 [64.3–77.4] | 0.165 |
| Primary vs. Revision arthroplasty | |||||
| Primary | 66 (71.7%) | 42 (64.6%) | 70 (51.5%) | 178 (60.8%) | 0.436 |
| Revision | 19 (20.7%) | 15 (23.1%) | 16 (11.8%) | 50 (17.1%) | |
| Missing | 7 (7.6%) | 8 (12.3%) | 50 (36.8%) | 65 (22.2%) | |
| Presentation type c | |||||
| Early postoperative | 45 (48.9%) | 0 (0%) | 0 (0%) | 45 (15.4%) | <0.001 |
| Late acute | 28 (30.4%) | 39 (60.0%) | 89 (65.4%) | 156 (53.2%) | |
| Chronic | 6 (6.5%) | 16 (24.6%) | 17 (12.5%) | 39 (13.3%) | |
| Late (Not classifiable) | 12 (13.0%) | 9 (13.8%) | 24 (17.6%) | 45 (15.4%) | |
| Missing | 1 (1.1%) | 1 (1.5%) | 6 (4.4%) | 8 (2.7%) | |
| Duration of symptoms (days) | |||||
| Median [IQR] | 5 [2–14] | 5 [2–33.5] | 3 [1–14] | 4.00 [1–14] | 0.147 |
| Infected joint | |||||
| Knee | 46 (50.0%) | 47 (72.3%) | 78 (57.4%) | 171 (58.4%) | 0.836 |
| Hip | 44 (47.8%) | 17 (26.2%) | 55 (40.4%) | 116 (39.6%) | 0.875 |
| Shoulder | 2 (2.2%) | 1 (1.5%) | 3 (2.2%) | 6 (2.0%) | 1.000 |
| Symptoms at admission to hospital (% of available data) d | |||||
| Joint pain | 68/92 (73.9%) | 63/65 (96.9%) | 128/136 (94.1%) | 259/293 (88.4%) | 0.008 |
| Swollen joint | 55/78 (70.5%) | 44/63 (69.8%) | 74/127 (58.3%) | 173/268 (64.6%) | 0.093 |
| Warm joint | 36/75 (48.0%) | 33/62 (53.2%) | 53/123 (43.1%) | 122/260 (46.9%) | 0.347 |
| Joint redness | 50/81 (61.7%) | 22/62 (35.5%) | 32/125 (25.6%) | 104/268 (38.8%) | <0.001 |
| Variables | IRR Adjusted | Confidence Interval | p-Value |
|---|---|---|---|
| PJI/procedure-person-years a | |||
| Gender (female vs. male) | 0.42 | [0.27–0.68] | <0.001 |
| Joint (knee vs. hip infection) | 1.37 | [0.90–2.22] | 0.169 |
| Period (2016–2020 vs. 2010–2015) | 1.82 | [1.11–2.82] | 0.012 |
| PJI/general population-person-years b | |||
| Gender (female vs. male) | 0.63 | [0.42–0.93] | 0.022 |
| Period (2012–2020 vs. 2003–2011) | 3.01 | [1.94–4.65] | <0.001 |
| Pathogen Isolate | Early Onset a (n = 92) | Delayed Onset a (n = 65) | Late Onset a (n = 136) | Total (n = 293) | p-Value b |
|---|---|---|---|---|---|
| Coagulase-negative staphylococci c | 39 (42.4%) | 19 (29.2%) | 30 (22.1%) | 88 (30.0%) | 0.004 |
| Staphylococcus aureus d | 24 (26.1%) | 13 (20.0%) | 39 (28.7%) | 76 (25.9%) | 0.259 |
| Streptococci e | 4 (4.3%) | 16 (24.6%) | 29 (21.3%) | 49 (16.7%) | 0.071 |
| Enterococci | 7 (7.6%) | 1 (1.5%) | 4 (2.9%) | 12 (4.1%) | 0.527 |
| Cutibacterium acnes | 1 (1.1%) | 4 (6.2%) | 3 (2.2%) | 8 (2.7%) | 0.729 |
| Candida species | 2 (2.2%) | 1 (1.5%) | 3 (2.2%) | 6 (2.0%) | 1.000 |
| Clostridium species | 3 (3.3%) | 0 (0%) | 1 (0.7%) | 4 (1.4%) | 0.220 |
| Corynebacterium species | 2 (2.2%) | 0 (0%) | 2 (1.5%) | 4 (1.4%) | 1.000 |
| Gram-negative bacteria | 5 (5.4%) | 0 (0%) | 5 (3.7%) | 10 (3.4%) | 0.738 |
| Escherichia coli | 1 (1.1%) | 0 (0%) | 4 (2.9%) | 5 (1.7%) | |
| Proteus mirabilis | 2 (2.2%) | 0 (0%) | 1 (0.7%) | 3 (1.0%) | |
| Klebsiella pneumoniae | 1 (1.1%) | 0 (0%) | 0 (0%) | 1 (0.3%) | |
| Pseudomonas aeruginosa | 1 (1.1%) | 0 (0%) | 0 (0%) | 1 (0.3%) | |
| Other pathogen | 2 (2.2%) | 3 (4.6%) | 4 (2.9%) | 9 (3.1%) | 0.756 |
| Polymicrobial f | 22 (23.9%) | 7 (10.8%) | 9 (6.6%) | 38 (13.0%) | 0.003 |
| Culture-negative | 3 (3.3%) | 8 (12.3%) | 16 (11.8%) | 27 (9.2%) | 0.229 |
| Pathogen Isolate | Early Postoperative (n = 45) | Late Acute (n = 156) | Chronic (n = 39) | Late (Not Classifiable) (n = 45) | Total (n = 285) b | p-Value c |
|---|---|---|---|---|---|---|
| Coagulase-negative staphylococci d | 15 (33.3%) | 33 (21.2%) | 19 (48.7%) | 20 (44.4%) | 87 (30.5%) | <0.001 |
| Staphylococcus aureus | 12 (26.7%) | 52 (33.3%) | 4 (10.3%) | 6 (13.3%) | 74 (26.0%) | <0.001 |
| Streptococci e | 1 (2.2%) | 36 (23.1%) | 2 (5.1%) | 10 (22.2%) | 49 (17.2%) | 0.504 |
| Enterococci | 6 (13.3%) | 5 (3.2%) | 0 (0%) | 1 (2.2%) | 12 (4.2%) | 0.119 |
| Cutibacterium acnes | 0 (0%) | 2 (1.3%) | 6 (15.4%) | 0 (0%) | 8 (2.8%) | 0.009 |
| Candida species | 1 (2.2%) | 2 (1.3%) | 1 (2.6%) | 1 (2.2%) | 5 (1.8%) | 0.634 |
| Clostridium species | 1 (2.2%) | 2 (1.3%) | 0 (0%) | 1 (2.2%) | 4 (1.4%) | 1.000 |
| Corynebacterium species | 1 (2.2%) | 1 (0.6%) | 0 (0%) | 2 (4.4%) | 4 (1.4%) | 0.827 |
| Gram-negative bacteria | 5 (11.1%) | 4 (2.6%) | 0 (0%) | 0 (0%) | 9 (3.2%) | 0.110 |
| Escherichia coli | 1 (2.2%) | 3 (1.9%) | 0 (0%) | 0 (0%) | 4 (1.4%) | |
| Proteus mirabilis | 2 (4.4%) | 1 (0.6%) | 0 (0%) | 0 (0%) | 3 (1.1%) | |
| Klebsiella pneumoniae | 1 (2.2%) | 0 (0%) | 0 (0%) | 0 (0%) | 1 (0.4%) | |
| Pseudomonas aeruginosa | 1 (2.2%) | 0 (0%) | 0 (0%) | 0 (0%) | 1 (0.4%) | |
| Other pathogen | 2 (4.4%) | 3 (1.9%) | 1 (2.6%) | 3 (6.7%) | 9 (3.2%) | 0.488 |
| Polymicrobial f | 17 (37.8%) | 13 (8.3%) | 5 (12.8%) | 3 (6.7%) | 38 (13.3%) | 0.302 |
| Culture-negative | 1 (2.2%) | 16 (10.3%) | 6 (15.4%) | 1 (2.2%) | 24 (8.4%) | 1.000 |
| DAIR (n = 147) | Antibiotics without Curative Surgery b (n = 27) | Two-Stage (n = 60) | Overall (n = 234) | p-Value | |
|---|---|---|---|---|---|
| Gender | |||||
| Male | 93 (63.3%) | 16 (59.3%) | 33 (55.0%) | 142 (60.7%) | 0.536 |
| Female | 54 (36.7%) | 11 (40.7%) | 27 (45.0%) | 92 (39.3%) | |
| Age (years) | |||||
| Median [IQR] | 69.7 [64.1–77.4] | 69.7 [63.3–74.1] | 67.2 [62.0–73.6] | 68.8 [63.6–76.2] | 0.150 |
| Infected joint, n (%) | |||||
| Knee | 89 (60.5%) | 18 (66.7%) | 36 (60.0%) | 143 (61.1%) | 0.818 |
| Hip | 55 (37.4%) | 8 (29.6%) | 24 (40.0%) | 87 (37.2%) | 0.648 |
| Shoulder | 3 (2.0%) | 1 (3.7%) | 0 (0%) | 4 (1.7%) | 0.411 |
| Zimmerli classification | |||||
| Early onset | 77 (52.4%) | 5 (18.5%) | 8 (13.3%) | 90 (38.5%) | <0.001 |
| Delayed onset | 26 (17.7%) | 9 (33.3%) | 14 (23.3%) | 49 (20.9%) | 0.161 |
| Late onset | 44 (29.9%) | 13 (48.1%) | 38 (63.3%) | 95 (40.6%) | <0.001 |
| Duration of symptoms (days) | |||||
| Median [IQR] | 4 [2–13.5] | 2 [1–10.5] | 7 [1–95] | 4 [1–14] | 0.021 |
| Missing | 5 (3.4%) | 0 (0%) | 1 (1.7%) | 6 (2.6%) | |
| Pathogen isolate, n (%) | |||||
| Coagulase-negative staphylococci c | 45 (30.6%) | 8 (29.6%) | 22 (36.7%) | 75 (32.1%) | 0.671 |
| Staphylococcus aureus | 42 (28.6%) | 7 (25.9%) | 8 (13.3%) | 57 (24.4%) | 0.045 |
| Streptococci d | 27 (18.4%) | 4 (14.8%) | 8 (13.3%) | 39 (16.7%) | 0.704 |
| Enterococci | 7 (4.8%) | 0 (0%) | 2 (3.3%) | 9 (3.8%) | 0.779 |
| Cutibacterium acnes | 0 (0%) | 1 (3.7%) | 5 (8.3%) | 6 (2.6%) | 0.002 |
| Candida species | 3 (2.0%) | 0 (0%) | 0 (0%) | 3 (1.3%) | 0.695 |
| Clostridium species | 3 (2.0%) | 0 (0%) | 1 (1.7%) | 4 (1.7%) | - |
| Corynebacterium species | 3 (2.0%) | 0 (0%) | 1 (1.7%) | 4 (1.7%) | 1.000 |
| Gram-negative bacteria | 5 (3.4%) | 0 (0%) | 2 (3.3%) | 7 (3.0%) | 1.000 |
| Escherichia coli | 2 (1.4%) | 0 (0%) | 1 (1.7%) | 3 (1.3%) | - |
| Proteus mirabilis | 1 (0.7%) | 0 (0%) | 1 (1.7%) | 2 (0.9%) | - |
| Klebsiella pneumoniae | 1 (0.7%) | 0 (0%) | 0 (0%) | 1 (0.4%) | - |
| Pseudomonas aeruginosa | 1 (0.7%) | 0 (0%) | 0 (0%) | 1 (0.4%) | |
| Other | 4 (2.7%) | 2 (7.4%) | 3 (5.0%) | 9 (3.8%) | 0.440 |
| Polymicrobial | 26 (17.7%) | 3 (11.1%) | 7 (11.7%) | 36 (15.4%) | 0.529 |
| Culture-negative | 8 (5.4%) | 5 (18.5%) | 8 (13.3%) | 21 (9.0%) | 0.026 |
| Treatment Success (n = 161) | Treatment Failure (n = 98) | Overall (n = 259) a | p-Value b | |
|---|---|---|---|---|
| Gender | ||||
| Male | 98 (60.9%) | 58 (59.2%) | 156 (60.2%) | 0.968 |
| Female | 63 (39.1%) | 40 (40.8%) | 103 (39.8%) | |
| Age (years) | ||||
| Median [IQR] | 68.8 [64.6–75.5] | 68.8 [62.9–78.0] | 68.8 [64.1–76.2] | 0.914 |
| Joint affected | ||||
| Knee | 96 (59.6%) | 53 (54.1%) | 149 (57.5%) | 0.512 |
| Hip | 59 (36.6%) | 45 (45.9%) | 104 (40.2%) | 0.210 |
| Shoulder | 6 (3.7%) | 0 (0%) | 6 (2.3%) | 0.086 |
| Zimmerli classification | ||||
| Early onset | 53 (32.9%) | 37 (37.8%) | 90 (34.7%) | 0.897 |
| Delayed onset | 39 (24.2%) | 20 (20.4%) | 59 (22.8%) | |
| Late onset | 69 (42.9%) | 41 (41.8%) | 110 (42.5%) | |
| Duration of symptoms (days) | ||||
| Median [IQR] | 4 [1–17.8] | 5 [1–14] | 5 [1–16] | 0.871 |
| Missing | 3 (1.9%) | 4 (4.1%) | 7 (2.7%) | |
| Pathogen isolate | ||||
| Coagulase-negative staphylococci c | 49 (30.4%) | 35 (35.7%) | 84 (32.4%) | 0.423 |
| Staphylococcus aureus | 33 (20.5%) | 30 (30.6%) | 63 (24.3%) | 0.082 |
| Streptococci d | 31 (19.3%) | 9 (9.2%) | 40 (15.4%) | 0.027 |
| Enterococci | 5 (3.1%) | 5 (5.1%) | 10 (3.9%) | 0.509 |
| Cutibacterium acnes | 7 (4.3%) | 1 (1.0%) | 8 (3.1%) | 0.265 |
| Candida species | 2 (1.2%) | 4 (4.1%) | 6 (2.3%) | 0.202 |
| Clostridium species | 3 (1.9%) | 1 (1.0%) | 4 (1.5%) | 1.000 |
| Corynebacterium species | 0 (0%) | 4 (4.1%) | 4 (1.5%) | 0.038 |
| Gram-negative bacteria | 6 (3.7%) | 3 (3.1%) | 9 (3.5%) | 0.714 |
| Escherichia coli | 4 (2.5%) | 0 (0%) | 4 (1.5%) | |
| Proteus mirabilis | 1 (0.6%) | 2 (2.0%) | 3 (1.2%) | |
| Klebsiella pneumoniae | 1 (0.6%) | 0 (0%) | 1 (0.4%) | |
| Pseudomonas aeruginosa | 0 (0%) | 1 (1.0%) | 1 (0.4%) | |
| Other pathogen | 5 (3.1%) | 3 (3.1%) | 8 (3.1%) | 0.732 |
| Polymicrobial | 17 (10.6%) | 21 (21.4%) | 38 (14.7%) | 0.036 |
| Culture-negative | 20 (12.4%) | 3 (3.1%) | 23 (8.9%) | 0.028 |
| First treatment after diagnosis of PJI e | ||||
| DAIR | 79 (49.1%) | 68 (69.4%) | 147 (56.8%) | 0.001 |
| Two-stage | 52 (32.3%) | 7 (7.1%) | 59 (22.9%) | <0.001 |
| One-stage | 8 (5.0%) | 7 (7.1%) | 15 (5.8%) | 0.637 |
| Antibiotics without curative surgery | 13 (8.1%) | 14 (14.3%) | 27 (10.4%) | 0.160 |
| Girdlestone | 6 (3.7%) | 1 (1.0%) | 7 (2.7%) | 0.261 |
| Arthrodesis | 2 (1.2%) | 0 (0%) | 2 (0.8%) | 0.529 |
| Amputation | 1 (0.6%) | 0 (0%) | 1 (0.4%) | 1.000 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Haraldsdóttir, I.; Gunnlaugsdóttir, S.L.; Kristjánsson, D.F.; Erlendsdóttir, H.; Helgason, K.O.; Gudbrandsson, E.Þ.; Sigurdardóttir, B.; Gottfredsson, M. Changing Incidence, Aetiology and Outcomes of Prosthetic Joint Infections: A Population-Based Study in Iceland. J. Clin. Med. 2025, 14, 5289. https://doi.org/10.3390/jcm14155289
Haraldsdóttir I, Gunnlaugsdóttir SL, Kristjánsson DF, Erlendsdóttir H, Helgason KO, Gudbrandsson EÞ, Sigurdardóttir B, Gottfredsson M. Changing Incidence, Aetiology and Outcomes of Prosthetic Joint Infections: A Population-Based Study in Iceland. Journal of Clinical Medicine. 2025; 14(15):5289. https://doi.org/10.3390/jcm14155289
Chicago/Turabian StyleHaraldsdóttir, Ingunn, Signy Lea Gunnlaugsdóttir, Dagur Fridrik Kristjánsson, Helga Erlendsdóttir, Kristján Orri Helgason, Elías Þór Gudbrandsson, Bryndís Sigurdardóttir, and Magnús Gottfredsson. 2025. "Changing Incidence, Aetiology and Outcomes of Prosthetic Joint Infections: A Population-Based Study in Iceland" Journal of Clinical Medicine 14, no. 15: 5289. https://doi.org/10.3390/jcm14155289
APA StyleHaraldsdóttir, I., Gunnlaugsdóttir, S. L., Kristjánsson, D. F., Erlendsdóttir, H., Helgason, K. O., Gudbrandsson, E. Þ., Sigurdardóttir, B., & Gottfredsson, M. (2025). Changing Incidence, Aetiology and Outcomes of Prosthetic Joint Infections: A Population-Based Study in Iceland. Journal of Clinical Medicine, 14(15), 5289. https://doi.org/10.3390/jcm14155289





