Cross-Sectional Study of Variations in Cephalometric Parameters in Arab Orthodontic Patients with Skeletal Class I and II
Abstract
1. Introduction
2. Materials and Methods
2.1. Ethical Statement
2.2. Gender and Age Subgroups
- Males, and Females
- Age subgroups
- Combination of gender and age subgroups
2.3. Cephalometric Variables
- Sample size
2.4. Data Analysis
3. Results
3.1. Variations in Cephalogram Parameters
3.2. Variations in Cephalometric Parameters Within the Same Classification
3.2.1. Class I Occlusion
3.2.2. Class II Malocclusion
3.3. Calculated_ANB (i.e., ANB-ANB Individual)
3.4. Variations in Cephalometric Parameters Between Different Skeletal Classes
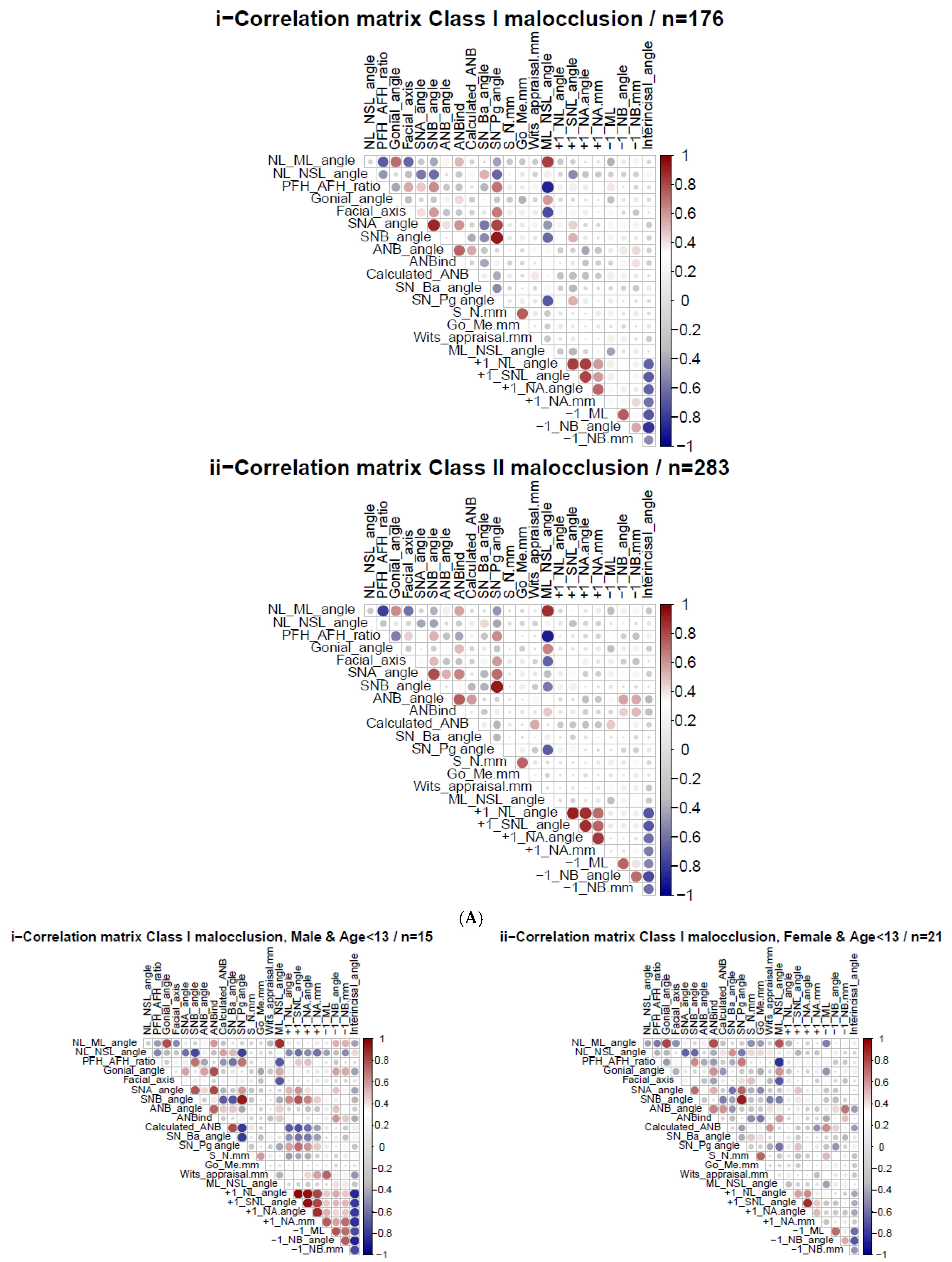
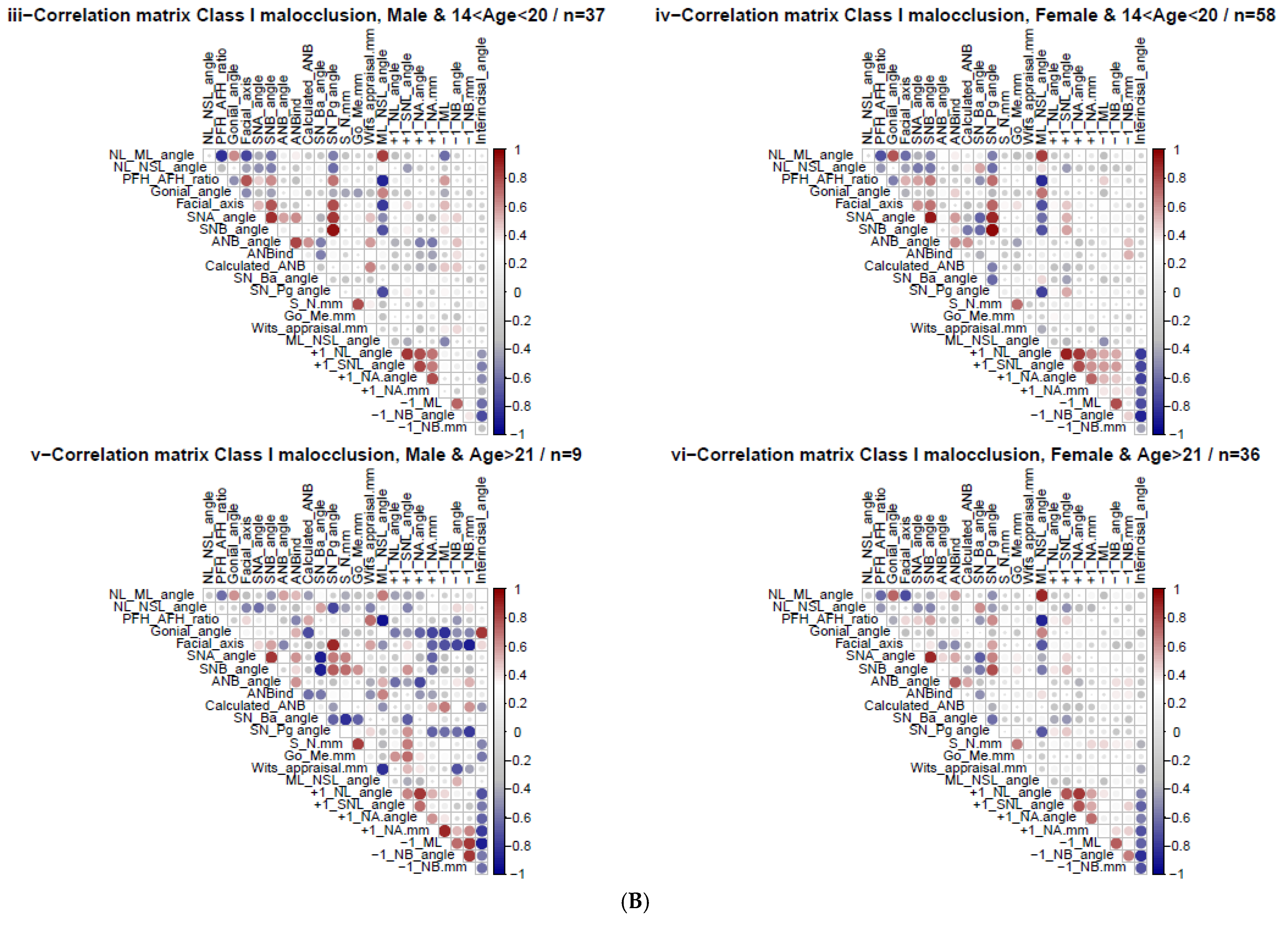
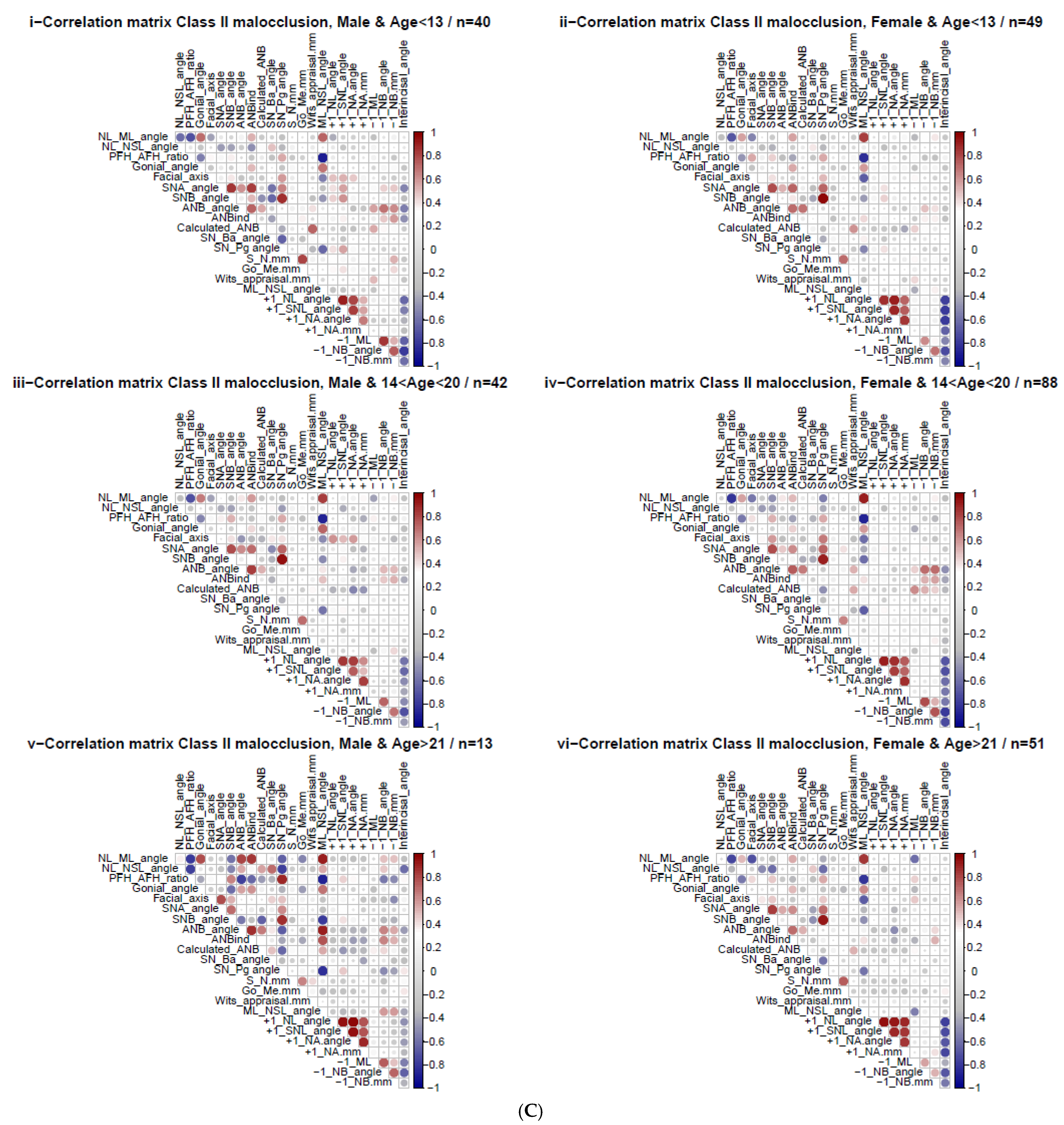
3.5. Heatmap Spearman Correlations: Calculated_ANB vs. Other Cephalometric Parameters
3.6. Heatmaps Spearman Correlations—Gender and Age Variation
3.7. Principal Component Analysis (PCA)
4. Discussion
4.1. Different Groups Comparisons
4.2. Calculated_ANB Correlation with Other Cephalometric Parameters
4.3. Results of Principal Component Analysis
4.4. Limitations
5. Conclusions and Future Research
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Gonçalves, F.M.; Taveira, K.V.M.; Araujo, C.M.; de Ravazzi, G.M.N.C.; Guariza Filho, O.; Zeigelboim, B.S.; Santos, R.S.; Stechman Neto, J. Association between atypical swallowing and malocclusions: A systematic review. Dent. Press J. Orthod. 2023, 27, e2221285. [Google Scholar] [CrossRef]
- Leavy, K.M.; Cisneros, G.J.; LeBlanc, E.M. Malocclusion and its relationship to speech sound production: Redefining the effect of malocclusal traits on sound production. Am. J. Orthod. Dentofac. Orthop. 2016, 150, 116–123. [Google Scholar] [CrossRef]
- Claudino, D.; Traebert, J. Malocclusion, dental aesthetic self-perception and quality of life in a 18 to 21 year-old population: A cross section study. BMC Oral Health. 2013, 13, 3. [Google Scholar] [CrossRef]
- Javidi, H.; Vettore, M.; Benson, P.E. Does orthodontic treatment before the age of 18 years improve oral health-related quality of life? A systematic review and meta-analysis. Am. J. Orthod. Dentofacial Orthop. 2017, 151, 644–655. [Google Scholar] [CrossRef]
- Ardani, I.G.A.W.; Heswari, D.; Alida, A. The correlation between Class I, II, III dental and skeletal malocclusion in ethnic Javanese: A cross sectional study. J. Int. Oral Health 2020, 12, 248. [Google Scholar] [CrossRef]
- Lone, I.M.; Zohud, O.; Midlej, K.; Awadi, O.; Masarwa, S.; Krohn, S.; Kirschneck, C.; Proff, P.; Watted, N.; Iraqi, F.A. Narrating the Genetic Landscape of Human Class I Occlusion: A Perspective-Infused Review. J. Pers. Med. 2023, 13, 1465. [Google Scholar] [CrossRef]
- Lone, I.M.; Zohud, O.; Midlej, K.; Proff, P.; Watted, N.; Iraqi, F.A. Skeletal Class II Malocclusion: From Clinical Treatment Strategies to the Roadmap in Identifying the Genetic Bases of Development in Humans with the Support of the Collaborative Cross Mouse Population. J. Clin. Med. 2023, 12, 5148. [Google Scholar] [CrossRef]
- Cenzato, N.; Nobili, A.; Maspero, C. Prevalence of dental malocclusions in different geographical areas: Scoping review. Dent. J. 2021, 9, 117. [Google Scholar] [CrossRef]
- Ghodasra, R.; Brizuela, M. Orthodontics, Malocclusion. In StatPearls; StatPearls Publishing: Treasure Island, FL, USA, 2024. [Google Scholar]
- Thomas, M. Orthodontics in the “art” of aesthetics. Int. J. Orthod. Milwaukee 2015, 26, 23–28. [Google Scholar]
- George, A.M.; Felicita, A.S.; Milling Tania, S.D.; Priyadharsini, J.V. Systematic review on the genetic factors associated with skeletal Class II malocclusion. Indian J. Dent. Res. 2021, 32, 399–406. [Google Scholar] [CrossRef]
- Steiner, C.C. Cephalometrics for you and me. Am. J. Orthod. 1953, 39, 729–755. [Google Scholar] [CrossRef]
- Fernandez, C.C.A.; Pereira, C.V.C.A.; Luiz, R.R.; Vieira, A.R.; De Castro Costa, M. Dental anomalies in different growth and skeletal malocclusion patterns. Angle Orthod. 2018, 88, 195–201. [Google Scholar] [CrossRef]
- Jacobson, A. Application of the “Wits” appraisal. Am. J. Orthod. 1976, 70, 179–189. [Google Scholar] [CrossRef]
- Panagiotidis, G.; Witt, E. Der individualisierte ANB-Winkel. Fortschritte Kieferorthopädie 1977, 38, 408–416. [Google Scholar] [CrossRef]
- Järvinen, S. Floating norms for the ANB angle as guidance for clinical considerations. Am. J. Orthod. Dentofac. Orthop. 1986, 90, 383–387. [Google Scholar] [CrossRef]
- Järvinen, S. Relation of the Wits appraisal to the ANB angle: A statistical appraisal. Am. J. Orthod. Dentofac. Orthop. 1988, 94, 432–435. [Google Scholar] [CrossRef]
- Yen, C.H. The individualized ANB angle of Chinese adults. Gaoxiong Yi Xue Ke Xue Za Zhi 1990, 6, 449–453. [Google Scholar]
- Paddenberg, E.; Proff, P.; Kirschneck, C. Floating norms for individualising the ANB angle and the WITS appraisal in orthodontic cephalometric analysis based on guiding variables. J. Orofac. Orthop. 2023, 84, 10–18. [Google Scholar] [CrossRef]
- Trottman, A.; Elsbach, H.G. Comparison of malocclusion in preschool black and white children. Am. J. Orthod. Dentofac. Orthop. 1996, 110, 69–72. [Google Scholar] [CrossRef]
- Phelan, T.; Buschang, P.H.; Behrents, R.G.; Wintergerst, A.M.; Ceen, R.F.; Hernandez, A. Variation in Class II malocclusion: Comparison of Mexican mestizos and American whites. Am. J. Orthod. Dentofac. Orthop. 2004, 125, 418–425. [Google Scholar] [CrossRef]
- Alhammadi, M.S.; Halboub, E.; Fayed, M.S.; Labib, A.; El-Saaidi, C. Global distribution of malocclusion traits: A systematic review. Dent. Press J. Orthod. 2018, 23, 40.e1–40.e10. [Google Scholar] [CrossRef]
- Midlej, K.; Watted, N.; Awadi, O.; Masarwa, S.; Lone, I.M.; Zohud, O.; Paddenberg, E.; Krohn, S.; Kuchler, E.; Proff, P.; et al. Lateral cephalometric parameters among Arab skeletal classes II and III patients and applying machine learning models. Clin. Oral Investig. 2024, 28, 511. [Google Scholar] [CrossRef]
- Paddenberg-Schubert, E.; Midlej, K.; Krohn, S.; Schröder, A.; Awadi, O.; Masarwa, S.; Lone, I.M.; Zohud, O.; Kirschneck, C.; Watted, N.; et al. Machine learning models for improving the diagnosing efficiency of skeletal class I and III in German orthodontic patients. Sci. Rep. 2025, 15, 12738. [Google Scholar] [CrossRef]
- Designing clinical research: An epidemiologic approach. Control. Clin. Trials 1989, 10, 125–126. [CrossRef]
- Nanda, A.; Mohapatra, B.B.; Mahapatra, A.P.K.; Mahapatra, A.P.K.; Mahapatra, A.P.K. Multiple comparison test by Tukey’s honestly significant difference (HSD): Do the confident level control type I error. Int. J. Stat. Appl. Math. 2021, 6, 59–65. [Google Scholar] [CrossRef]
- Korenius, T.; Laurikkala, J.; Juhola, M. On principal component analysis, cosine and Euclidean measures in information retrieval. Inf. Sci. 2007, 177, 4893–4905. [Google Scholar] [CrossRef]
- Salama, E.I.; Abuaffan, A.H. Cephalometric hard and soft tissue norms for sudanese adults. Orthod. J. Nepal 2016, 5, 28. [Google Scholar] [CrossRef]
- Drevensek, M.; Farcnik, F.; Vidmar, G. Cephalometric standards for Slovenians in the mixed dentition period. Eur. J. Orthod. 2006, 28, 51–57. [Google Scholar] [CrossRef]
- Deshmukh, N.; Pulluri, S.; Lavate, A.; Hoshing, S.; Ambarkar, S.; Shinde, S.; Chatla, K. Correlation of Cephalometric and Photographic Measurements in Different Skeletal Patterns. JMSCR 2022, 10, 80–88. [Google Scholar] [CrossRef]
- Pancherz, H.; Zieber, K.; Hoyer, B. Cephalometric characteristics of Class II division 1 and Class II division 2 malocclusions: A comparative study in children. Angle Orthod. 1997, 67, 111–120. [Google Scholar]
- Yoon, S.S.; Chung, C.-H. Comparison of craniofacial growth of untreated Class I and Class II girls from ages 9 to 18 years: A longitudinal study. Am. J. Orthod. Dentofac. Orthop. 2015, 147, 190–196. [Google Scholar] [CrossRef]
- Jan, A.; Bangash, A.A.; Shinwari, S. The Correlation between Wits and ANB Cephalometric Landmarks in Orthodontic Pateints. Pak. Armed Forces Med. J. 2017, 67, S267–S271. [Google Scholar]
- Saad, A.; Saqib, N. Co-relation between ANB angle, Wits value and SNP plane angle. Pak. Oral. Dental. J. 2009, 29, 287–289. [Google Scholar]
- Ardani, I.G.A.W.; Sanjaya, M.L.; Sjamsudin, J. Cephalometric characteristic of skeletal class II malocclusion in javanese population at universitas airlangga dental hospital. Contemp. Clin. Dent. 2018, 9, S342–S346. [Google Scholar] [CrossRef]
- Gul-e-Erum; Fida, M. A comparison of cephalometric analyses for assessing sagittal jaw relationship. J. Coll. Physicians Surg. Pak. 2008, 18, 679–683. [Google Scholar]
- Moreno Uribe, L.M.; Ray, A.; Blanchette, D.R.; Dawson, D.V.; Southard, T.E. Phenotype-genotype correlations of facial width and height proportions in patients with Class II malocclusion. Orthod. Craniofac. Res. 2015, 18 (Suppl. S1), 100–108. [Google Scholar] [CrossRef]
- Dascalu, C.G.; Zegan, G. Statistical methods for variables space reduction in cephalometric studies. In Proceedings of the 2013 E-Health and Bioengineering Conference (EHB), Iasi, Romania, 21–23 November 2013; IEEE: New York, NY, USA, 2013; pp. 1–4. [Google Scholar]


| (A) | |||||||
| Skeletal Class I | |||||||
| Variable | N | Mean | Std. Dev. | Min | Pctl. 25 | Pctl. 75 | Max |
| Age | 157 | 18 | 6.2 | 8.2 | 14 | 21 | 48 |
| 0 < Age < 13 | 42(27%) | ||||||
| 14 < Age < 20 | 80 (51%) | ||||||
| Age > 21 | 35 (22%) | ||||||
| Female | 101 (64%) | ||||||
| Male | 56 (36%) | ||||||
| NL-ML angle | 157 | 30 | 6.2 | 13 | 26 | 34 | 46 |
| NL-NSL angle | 157 | 7.7 | 3.3 | −0.1 | 5.4 | 9.6 | 16 |
| PFH/AFH | 157 | 65 | 5 | 50 | 62 | 68 | 79 |
| Gonial angle | 157 | 132 | 7.6 | 113 | 128 | 138 | 155 |
| Facial axis | 157 | 88 | 4.3 | 77 | 85 | 91 | 102 |
| SNA angle | 157 | 83 | 3.8 | 75 | 80 | 85 | 94 |
| SNB angle | 157 | 78 | 3.3 | 68 | 75 | 80 | 85 |
| ANB angle | 157 | 5.1 | 1.5 | 2.2 | 4.1 | 6 | 9 |
| ANBind | 157 | 5.4 | 1.5 | 2.2 | 4.3 | 6.3 | 8.8 |
| Calculated_ANB (ANB − ANBind) | 157 | −0.26 | 0.59 | −1 | −0.8 | 0.1 | 1 |
| SN-Ba angle | 157 | 129 | 5.7 | 114 | 125 | 133 | 142 |
| SN-Pg angle | 157 | 78 | 3.7 | 67 | 76 | 80 | 89 |
| S-N (mm) | 157 | 63 | 7.2 | 39 | 58 | 66 | 88 |
| Go-Me (mm) | 157 | 60 | 6.3 | 46 | 56 | 63 | 82 |
| Wits appraisal (mm) | 157 | −3.3 | 2.6 | −9.1 | −5.3 | −1.5 | 3 |
| ML-NSL angle | 157 | 37 | 6.9 | 7.5 | 33 | 41 | 61 |
| +1/NL angle | 157 | 114 | 5.5 | 97 | 110 | 118 | 128 |
| +1/SNL angle | 157 | 105 | 10 | 11 | 101 | 111 | 125 |
| +1/NA angle | 157 | 24 | 5.6 | 2.8 | 20 | 27 | 40 |
| +1/NA (mm) | 157 | 3.4 | 2.1 | −2.3 | 2 | 5.1 | 8.6 |
| −1/ML (anatomic) | 157 | 93 | 6.7 | 77 | 89 | 98 | 111 |
| −1/NB angle | 157 | 28 | 6.3 | 8.5 | 24 | 32 | 47 |
| −1/NB (mm) | 157 | 5.6 | 2.4 | −1.4 | 3.9 | 7.4 | 12 |
| Interincisal angle | 157 | 124 | 9.8 | 102 | 118 | 129 | 154 |
| (B) | |||||||
| Skeletal Class II | |||||||
| Variable | N | Mean | Std. Dev. | Min | Pctl. 25 | Pctl. 75 | Max |
| Age | 237 | 17 | 6.5 | 6.8 | 13 | 21 | 44 |
| 0 < Age < 13 | 74 (31%) | ||||||
| 14 < Age < 20 | 107 (45%) | ||||||
| Age > 21 | 56 (24%) | ||||||
| Female | 162 (68%) | ||||||
| Male | 75 (32%) | ||||||
| NL-ML angle | 237 | 28 | 6.5 | 13 | 24 | 33 | 54 |
| NL-NSL angle | 237 | 8.3 | 3.6 | 1 | 6.1 | 10 | 42 |
| PFH/AFH | 237 | 65 | 5.3 | 50 | 62 | 69 | 79 |
| Gonial angle | 237 | 128 | 7.6 | 110 | 124 | 134 | 150 |
| Facial axis | 237 | 88 | 4.6 | 70 | 85 | 91 | 102 |
| SNA angle | 237 | 83 | 3.7 | 75 | 80 | 86 | 94 |
| SNB angle | 237 | 75 | 5.4 | 7.8 | 73 | 78 | 84 |
| ANB angle | 237 | 7.2 | 1.8 | 3.3 | 6 | 8.3 | 16 |
| ANBind | 237 | 5.3 | 1.6 | 1.6 | 4.1 | 6.4 | 10 |
| Calculated_ANB (ANB − ANBind) | 237 | 2 | 0.9 | 1.1 | 1.3 | 2.6 | 5.5 |
| SN-Ba angle | 237 | 130 | 5.3 | 119 | 126 | 133 | 147 |
| SN-Pg angle | 237 | 76 | 3.5 | 65 | 74 | 79 | 85 |
| S-N (mm) | 237 | 63 | 6.9 | 30 | 59 | 65 | 87 |
| Go-Me (mm) | 237 | 59 | 5.9 | 44 | 55 | 62 | 77 |
| Wits appraisal (mm) | 237 | −1.2 | 2.5 | −9.5 | −2.8 | 0.6 | 8.3 |
| ML-NSL angle | 237 | 36 | 7.2 | 4.6 | 32 | 40 | 63 |
| +1/NL angle | 237 | 113 | 7.6 | 91 | 108 | 119 | 135 |
| +1/SNL angle | 237 | 105 | 8.3 | 78 | 99 | 110 | 124 |
| +1/NA angle | 237 | 21 | 12 | −121 | 17 | 27 | 42 |
| +1/NA (mm) | 237 | 2.9 | 2.3 | −2.8 | 1.2 | 4.4 | 9.2 |
| −1/ML (anatomic) | 237 | 97 | 9.3 | 9.5 | 92 | 102 | 120 |
| −1/NB angle | 237 | 29 | 7 | 6.8 | 25 | 33 | 50 |
| −1/NB (mm) | 237 | 5.6 | 2.6 | −0.5 | 3.8 | 7.4 | 12 |
| Interincisal angle | 237 | 122 | 11 | 100 | 114 | 129 | 163 |
| (A) | |||||
| Parameter | Group A _ Group B | Difference | Lower CI | Upper CI | Adj. p Value |
| NL-ML angle | I_Male-I_Female | −2.11 | −4.12 | −0.10 | 0.04 |
| PFH/AFH | I_Male-I_Female | 2.56 | 0.34 | 4.77 | 0.02 |
| PFH/AFH | I_Male_14 < Age < 20-I_Female_0 < Age < 13 | 4.03 | 0.26 | 7.80 | 0.03 |
| ANBind | I_Male-I_Female | −0.51 | −1.00 | −0.02 | 0.04 |
| SN-Ba | I_Male_14 < Age < 20-I_Female_14 < Age < 20 | −3.96 | −7.66 | −0.26 | 0.03 |
| S-N (mm) | I_Male-I_Female | 3.43 | 0.47 | 6.38 | 0.02 |
| S-N (mm) | I_Male_14 < Age < 20-I_Female_0 < Age < 13 | 7.03 | 0.98 | 13.09 | 0.01 |
| Go Me (mm) | I_Male-I_Female | 2.16 | 0.12 | 4.20 | 0.04 |
| Wits appraisal | I_Male-I_Female | 1.01 | 0.15 | 1.86 | 0.02 |
| ML-NSL angle | I_Male-I_Female | −3.04 | −6.08 | −0.01 | 0.05 |
| (B) | |||||
| Parameter | Group A _ Group B | Difference | Lower CI | Upper CI | Adj. p value |
| NL-ML angle | II_Age > 21-II_14 < Age < 20 | 4.21 | 1.24 | 7.18 | 0.00 |
| NL-ML angle | II_Female_Age > 21-II_Female_14 < Age < 20 | 4.43 | 0.48 | 8.38 | 0.01 |
| PFH/AFH | II_Age > 21-II_14 < Age < 20 | −2.66 | −5.09 | −0.24 | 0.02 |
| PFH/AFH | II_14 < Age < 20-II_0 < Age < 13 | 1.98 | 0.11 | 3.85 | 0.03 |
| PFH/AFH | II_Female_14 < Age < 20-II_Female_0 < Age < 13 | 3.08 | 0.23 | 5.93 | 0.03 |
| PFH/AFH | II_Female_Age > 21-II_Female_14 < Age < 20 | −2.95 | −5.81 | −0.08 | 0.04 |
| Gonial angle | II_14 < Age < 20-II_0 < Age < 13 | −3.01 | −5.68 | −0.34 | 0.02 |
| Gonial angle | II_Age > 21-II_14 < Age < 20 | 3.37 | 0.46 | 6.28 | 0.02 |
| Facial axis | II_Age > 21-II_0 < Age < 13 | −2.50 | −4.75 | −0.24 | 0.02 |
| Facial axis | II_Age > 21-II_14 < Age < 20 | −2.42 | −4.52 | −0.32 | 0.01 |
| Facial axis | II_Female_Age > 21-II_Female_14 < Age < 20 | −3.00 | −5.79 | −0.21 | 0.02 |
| Facial axis | II_Female_Age > 21-II_Female_14 < Age < 20 | −3.00 | −5.49 | −0.50 | 0.01 |
| Facial axis | II_Male_0 < Age < 13-II_Female_Age > 21 | 3.17 | 0.07 | 6.27 | 0.04 |
| SNB angle | II_14 < Age < 20-II_0 < Age < 13 | 2.00 | 0.08 | 3.91 | 0.04 |
| SN-Pg angle | II_14 < Age < 20-II_0 < Age < 13 | 1.31 | 0.09 | 2.52 | 0.03 |
| SN-Pg angle | II_Age > 21-II_14 < Age < 20 | −1.60 | −2.93 | −0.28 | 0.01 |
| S-N (mm) | II_Male-II_Female | 2.35 | 0.49 | 4.22 | 0.01 |
| S-N (mm) | II_Male_0 < Age < 13-II_Female_14 < Age < 20 | 4.39 | 0.18 | 8.60 | 0.04 |
| ML-NSL angle | II_Age > 21-II_14 < Age < 20 | 3.99 | 0.68 | 7.31 | 0.01 |
| ML-NSL angle | II_Female_Age > 21-II_Female_14 < Age < 20 | 4.38 | 0.47 | 8.29 | 0.02 |
| +1/NA angle | II_14 < Age < 20-II_0 < Age < 13 | −5.29 | −9.62 | −0.95 | 0.01 |
| +1/NA angle | II_Male_14 < Age < 20-II_Female_0 < Age < 13 | −9.97 | −17.57 | −2.37 | 0.00 |
| +1/NA angle | II_Male_14 < Age < 20-II_Male_0 < Age < 13 | −9.27 | −17.59 | −0.96 | 0.01 |
| +1/NA (mm) | II_14 < Age < 20-II_0 < Age < 13 | −1.27 | −2.23 | −0.32 | 0.00 |
| +1/NA (mm) | II_Age > 21-II_0 < Age < 13 | −1.01 | −1.96 | −0.06 | 0.03 |
| −1/ML (anatomic) | II_Female_14 < Age < 20-II_Female_0 < Age < 13 | 5.34 | 0.19 | 10.48 | 0.03 |
| (C) | |||||
| Parameter | Group A _ Group B | Difference | Lower CI | Upper CI | Adj. p value |
| Calculated_ANB | II_Male-I_Female | 2.24 | 1.93 | 2.55 | 0 |
| Calculated_ANB | II_Female-I_Male | 2.17 | 1.85 | 2.48 | 0 |
| Calculated_ANB | II_Male-I_Male | 2.12 | 1.76 | 2.48 | 0 |
| Calculated_ANB | II_0 < Age < 13-I_0 < Age < 13 | 2.24 | 1.81 | 2.68 | 0 |
| Calculated_ANB | II_14 < Age < 20-I_0 < Age < 13 | 2.18 | 1.76 | 2.59 | 0 |
| Calculated_ANB | II_Age > 21-I_0 < Age < 13 | 2.05 | 1.59 | 2.51 | 0 |
| Calculated_ANB | II_0 < Age < 13-I_14 < Age < 20 | 2.28 | 1.92 | 2.65 | 0 |
| Calculated_ANB | II_14 < Age < 20-I_14 < Age < 20 | 2.22 | 1.88 | 2.55 | 0 |
| Calculated_ANB | II_Age > 21-I_14 < Age < 20 | 2.09 | 1.7 | 2.49 | 0 |
| Calculated_ANB | II_0 < Age < 13-I_Age > 21 | 2.42 | 1.95 | 2.88 | 0 |
| Calculated_ANB | II_14 < Age < 20-I_Age > 21 | 2.35 | 1.91 | 2.79 | 0 |
| Calculated_ANB | II_Age > 21-I_Age > 21 | 2.23 | 1.74 | 2.71 | 0 |
| Calculated_ANB | II_Female_0 < Age < 13-I_Female_0 < Age < 13 | 2.2 | 1.55 | 2.85 | 0 |
| Calculated_ANB | II_Female_14 < Age < 20-I_Female_0 < Age < 13 | 2.29 | 1.69 | 2.9 | 0 |
| Calculated_ANB | II_Female_Age > 21-I_Female_0 < Age < 13 | 2.09 | 1.43 | 2.74 | 0 |
| Calculated_ANB | II_Male_0 < Age < 13-I_Female_0 < Age < 13 | 2.38 | 1.68 | 3.09 | 0 |
| Calculated_ANB | II_Male_14 < Age < 20-I_Female_0 < Age < 13 | 2.01 | 1.31 | 2.71 | 0 |
| Calculated_ANB | II_Male_Age > 21-I_Female_0 < Age < 13 | 2.07 | 1.18 | 2.96 | 0 |
| Calculated_ANB | II_Female_0 < Age < 13-I_Female_14 < Age < 20 | 2.27 | 1.73 | 2.81 | 0 |
| Calculated_ANB | II_Female_14 < Age < 20-I_Female_14 < Age < 20 | 2.36 | 1.88 | 2.84 | 0 |
| Calculated_ANB | II_Female_Age > 21-I_Female_14 < Age < 20 | 2.16 | 1.61 | 2.7 | 0 |
| Calculated_ANB | II_Male_0 < Age < 13-I_Female_14 < Age < 20 | 2.45 | 1.85 | 3.06 | 0 |
| Calculated_ANB | II_Male_14 < Age < 20-I_Female_14 < Age < 20 | 2.08 | 1.49 | 2.67 | 0 |
| Calculated_ANB | II_Male_Age > 21-I_Female_14 < Age < 20 | 2.14 | 1.32 | 2.95 | 0 |
| Calculated_ANB | II_Female_0 < Age < 13-I_Female_Age > 21 | 2.33 | 1.7 | 2.97 | 0 |
| Calculated_ANB | II_Female_14 < Age < 20-I_Female_Age > 21 | 2.42 | 1.84 | 3.01 | 0 |
| Calculated_ANB | II_Female_Age > 21-I_Female_Age > 21 | 2.22 | 1.58 | 2.86 | 0 |
| Calculated_ANB | II_Male_0 < Age < 13-I_Female_Age > 21 | 2.51 | 1.82 | 3.2 | 0 |
| Calculated_ANB | II_Male_14 < Age < 20-I_Female_Age > 21 | 2.14 | 1.46 | 2.82 | 0 |
| Calculated_ANB | II_Male_Age > 21-I_Female_Age > 21 | 2.2 | 1.32 | 3.08 | 0 |
| Calculated_ANB | II_Female_0 < Age < 13-I_Male_0 < Age < 13 | 2.12 | 1.38 | 2.87 | 0 |
| Calculated_ANB | II_Female_14 < Age < 20-I_Male_0 < Age < 13 | 2.21 | 1.51 | 2.91 | 0 |
| Calculated_ANB | II_Female_Age > 21-I_Male_0 < Age < 13 | 2.01 | 1.26 | 2.76 | 0 |
| Calculated_ANB | II_Male_0 < Age < 13-I_Male_0 < Age < 13 | 2.3 | 1.51 | 3.09 | 0 |
| Calculated_ANB | II_Male_14 < Age < 20-I_Male_0 < Age < 13 | 1.93 | 1.15 | 2.71 | 0 |
| Calculated_ANB | II_Male_Age > 21-I_Male_0 < Age < 13 | 1.99 | 1.03 | 2.95 | 0 |
| Calculated_ANB | II_Female_0 < Age < 13-I_Male_14 < Age < 20 | 2.12 | 1.5 | 2.73 | 0 |
| Calculated_ANB | II_Female_14 < Age < 20-I_Male_14 < Age < 20 | 2.21 | 1.65 | 2.76 | 0 |
| Calculated_ANB | II_Female_Age > 21-I_Male_14 < Age < 20 | 2 | 1.39 | 2.61 | 0 |
| Calculated_ANB | II_Male_0 < Age < 13-I_Male_14 < Age < 20 | 2.3 | 1.63 | 2.96 | 0 |
| Calculated_ANB | II_Male_14 < Age < 20-I_Male_14 < Age < 20 | 1.92 | 1.27 | 2.58 | 0 |
| Calculated_ANB | II_Male_Age > 21-I_Male_14 < Age < 20 | 1.98 | 1.12 | 2.84 | 0 |
| Calculated_ANB | II_Female_0 < Age < 13-I_Male_Age > 21 | 2.38 | 1.38 | 3.38 | 0 |
| Calculated_ANB | II_Female_14 < Age < 20-I_Male_Age > 21 | 2.47 | 1.5 | 3.44 | 0 |
| Calculated_ANB | II_Female_Age > 21-I_Male_Age > 21 | 2.27 | 1.27 | 3.27 | 0 |
| Calculated_ANB | II_Male_0 < Age < 13-I_Male_Age > 21 | 2.56 | 1.53 | 3.6 | 0 |
| Calculated_ANB | II_Male_14 < Age < 20-I_Male_Age > 21 | 2.19 | 1.16 | 3.22 | 0 |
| Calculated_ANB | II_Male_Age > 21-I_Male_Age > 21 | 2.25 | 1.08 | 3.42 | 0 |
| (A) | ||||||
| Class | I | II | ||||
| Calculated_ANB | Calculated_ANB | |||||
| NL-ML angle | −0.173 * | −0.05 | ||||
| NL-NSL angle | 0.336 ** | 0.108 | ||||
| PFHAFH ratio | −0.065 | −0.013 | ||||
| Gonial angle | −0.276 ** | 0.005 | ||||
| Facial axis | −0.219 ** | −0.035 | ||||
| SNA angle | −0.282 ** | −0.047 | ||||
| SNB angle | −0.364 ** | −0.274 ** | ||||
| ANB angle | 0.112 | 0.430 ** | ||||
| ANBind | −0.255 ** | −0.028 | ||||
| SN-Ba angle | 0.162 * | 0.216 ** | ||||
| SN-Pg angle | −0.395 ** | −0.302 ** | ||||
| S-N mm | 0.12 | 0.052 | ||||
| Go-Me (mm_ | 0.011 | −0.059 | ||||
| Wits appraisal | 0.177 * | 0.574 ** | ||||
| ML-NSL angle | 0.008 | 0.005 | ||||
| +1/NL angle | −0.155 | −0.209 ** | ||||
| +1/SNL angle | −0.259 ** | −0.242 ** | ||||
| +1/NA angle | −0.137 | −0.245 ** | ||||
| +1/NA (mm) | 0.06 | −0.151 * | ||||
| −1/ML (anatomic) | 0.377 ** | 0.334 ** | ||||
| −1/NB angle | 0.253 ** | 0.240 ** | ||||
| −1/NB (mm) | 0.003 | 0.152 * | ||||
| Interincisal angle | −0.107 | −0.047 | ||||
| (B) | ||||||
| Class I | Calculated_ANB | |||||
| Female | Male | |||||
| 0 < Age_13 | 14 < Age < 20 | Age > 21 | 0 < Age_13 | 14 < Age < 20 | Age > 21 | |
| NL-ML angle | −0.519 ** | −0.022 | 0.021 | −0.26 | −0.133 | −0.443 |
| NL-NSL angle | 0.439 * | 0.436 ** | 0.627 ** | 0.287 | 0.033 | 0.144 |
| PFH/AFH | 0.146 | −0.195 | −0.241 | −0.203 | 0.146 | 0.503 |
| Gonial angle | −0.643 ** | −0.254 | −0.074 | −0.312 | −0.139 | −0.467 |
| Facial axis | 0.412 * | −0.510 ** | −0.378 | −0.33 | −0.011 | −0.012 |
| SNA angle | −0.225 | −0.426 ** | −0.545 ** | −0.482 | 0.169 | −0.072 |
| SNB angle | −0.297 | −0.509 ** | −0.612 ** | −0.516 * | 0.032 | −0.072 |
| ANB angle | −0.058 | 0.185 | 0.043 | 0.078 | 0.28 | −0.422 |
| ANBind | −0.530 ** | −0.179 | −0.327 | −0.411 | 0.051 | −0.448 |
| SN-Ba angle | 0.299 | 0.289 * | 0.502 ** | 0.009 | −0.217 | −0.048 |
| SN-Pg angle | −0.314 | −0.556 ** | −0.537 ** | −0.502 * | −0.031 | −0.192 |
| S-N (mm) | 0.29 | 0.013 | 0.059 | 0.221 | 0.166 | 0.132 |
| Go-Me (mm) | 0.397 * | −0.075 | −0.07 | 0.007 | 0.035 | 0.12 |
| Wits appraisal (mm) | 0.281 | 0.185 | 0.219 | 0.339 | −0.051 | -0.771 * |
| ML-NSL angle | −0.314 | 0.182 | 0.243 | −0.027 | −0.067 | −0.347 |
| +1/NL angle | 0.187 | −0.268 | −0.269 | −0.435 | −0.11 | 0.572 |
| +1/SNL angle | 0.001 | −0.435 ** | −0.352 | −0.483 * | −0.083 | 0.467 |
| +1/NA angle | 0.152 | −0.175 | −0.226 | −0.279 | −0.26 | 0.743 * |
| +1/NA (mm) | 0.081 | 0.207 | 0.031 | −0.171 | −0.03 | 0.392 |
| −1/ML (anatomic) | 0.551 ** | 0.264 | 0.338 | −0.182 | 0.514 ** | 0.587 |
| −1/NB angle | 0.234 | 0.189 | 0.38 | −0.257 | 0.501 ** | 0.144 |
| −1/NB (mm) | −0.193 | 0.166 | −0.138 | −0.268 | 0.169 | −0.156 |
| Interincisal angle | −0.242 | 0.009 | −0.106 | 0.337 | −0.380 * | −0.695 |
| (C) | ||||||
| Class II | Calculated_ANB | |||||
| Female | Male | |||||
| 0 < Age_13 | 14 < Age < 20 | Age > 21 | 0 < Age_13 | 14 < Age < 20 | Age > 21 | |
| NL-ML angle | −0.171 | 0.064 | −0.049 | −0.191 | −0.216 | 0.086 |
| NL-NSL angle | 0.19 | 0.002 | 0.069 | 0.051 | 0.256 | 0.535 |
| PFH/AFH | 0.265 | −0.076 | −0.012 | 0.107 | 0.033 | −0.335 |
| Gonial angle | −0.017 | −0.026 | −0.054 | −0.13 | 0.05 | 0.247 |
| Facial axis | 0.023 | −0.041 | −0.075 | 0.021 | −0.258 | 0.058 |
| SNA angle | −0.044 | −0.03 | 0.044 | −0.317 | −0.012 | 0.127 |
| SNB angle | −0.249 | −0.285 * | −0.205 | −0.364 * | −0.201 | −0.369 |
| ANB angle | 0.447 ** | 0.554 ** | 0.407 ** | 0.137 | 0.403 * | 0.673 * |
| ANBind | −0.115 | 0.054 | 0.067 | −0.349 | 0.017 | 0.432 |
| SN-Ba angle | 0.286 | 0.163 | 0.166 | 0.187 | 0.288 | 0.286 |
| SN-Pg angle | −0.222 | −0.404 ** | −0.247 | −0.28 | −0.191 | −0.327 |
| S-N (mm) | −0.035 | 0.041 | 0.338 * | 0.004 | −0.224 | 0.155 |
| Go-Me (mm) | −0.084 | −0.055 | 0.216 | −0.183 | −0.279 | 0.291 |
| Wits appraisal (mm) | 0.468 ** | 0.629 ** | 0.438 ** | 0.667 ** | 0.481 ** | 0.853 ** |
| ML-NSL angle | −0.145 | 0.051 | −0.004 | −0.129 | 0.032 | 0.331 |
| +1/NL angle | −0.172 | −0.136 | −0.456 ** | −0.106 | −0.441 * | −0.296 |
| +1/SNL angle | −0.214 | −0.162 | −0.411 ** | −0.09 | −0.439 * | −0.412 |
| +1/NA angle | −0.231 | −0.147 | −0.433 ** | −0.024 | −0.626 ** | −0.449 |
| +1/NA (mm) | −0.300 * | 0.036 | −0.360 * | 0.15 | −0.521 ** | −0.37 |
| −1/ML (anatomic) | 0.394 ** | 0.357 ** | 0.117 | 0.502 ** | 0.14 | 0.643 * |
| −1/NB angle | 0.207 | 0.331 ** | −0.012 | 0.209 | 0.107 | 0.648 * |
| −1/NB (mm) | 0.05 | 0.253 * | 0.073 | 0.021 | 0.066 | 0.454 |
| Interincisal angle | 0.007 | −0.17 | 0.238 | −0.168 | 0.219 | −0.452 |
| (A) | ||||
| Comp.1 | Comp.2 | Comp.3 | Comp.4 | |
| Standard deviation | 1.10 | 0.80 | 0.65 | 0.42 |
| Proportion of Variance | 0.43 | 0.23 | 0.15 | 0.06 |
| Cumulative Proportion | 0.43 | 0.66 | 0.82 | 0.886 |
| (B) | ||||
| Parameter | Comp.1 | Comp.2 | Comp.3 | Comp.4 |
| NL-ML angle | 0.31 | 0.19 | 0.19 | 0.26 |
| NL-NSL | 0.16 | −0.09 | 0.03 | −0.41 |
| PFH/AFH | −0.36 | −0.12 | −0.17 | 0.05 |
| Gonial angle | 0.20 | 0.16 | 0.26 | 0.17 |
| Facial axis | −0.33 | −0.06 | −0.04 | −0.17 |
| SNA angle | 0.00 | −0.01 | −0.06 | 0.13 |
| SNB angle | −0.27 | 0.01 | 0.01 | 0.33 |
| ANB angle | 0.23 | −0.02 | −0.33 | 0.19 |
| Calculated_ANB | 0.17 | −0.14 | −0.41 | −0.14 |
| SN-Ba angle | 0.12 | −0.07 | 0.06 | −0.50 |
| SN-Pg angle | −0.37 | −0.01 | 0.02 | 0.28 |
| S-N (mm) | −0.01 | −0.02 | −0.10 | −0.03 |
| Go-Me (mm) | −0.06 | −0.07 | −0.03 | 0.01 |
| Wits appraisal (mm) | 0.07 | −0.03 | −0.34 | −0.06 |
| ML-NSL angle | 0.38 | 0.14 | 0.19 | 0.05 |
| +1/NL angle | −0.18 | 0.38 | 0.02 | −0.18 |
| +1/SNL angle | −0.20 | 0.34 | −0.02 | −0.02 |
| +1/NA angle | −0.16 | 0.39 | 0.11 | −0.23 |
| +1/NA (mm) | −0.10 | 0.39 | 0.09 | −0.15 |
| −1/ML (anatomic) | −0.03 | 0.10 | −0.43 | −0.10 |
| −1/NB angle | 0.13 | 0.23 | −0.33 | 0.12 |
| −1/NB (mm) | 0.14 | 0.25 | −0.22 | 0.20 |
| Interincisal angle | −0.03 | −0.42 | 0.24 | 0.03 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Midlej, K.; Proff, P.; Watted, N.; Iraqi, F.A. Cross-Sectional Study of Variations in Cephalometric Parameters in Arab Orthodontic Patients with Skeletal Class I and II. J. Clin. Med. 2025, 14, 5292. https://doi.org/10.3390/jcm14155292
Midlej K, Proff P, Watted N, Iraqi FA. Cross-Sectional Study of Variations in Cephalometric Parameters in Arab Orthodontic Patients with Skeletal Class I and II. Journal of Clinical Medicine. 2025; 14(15):5292. https://doi.org/10.3390/jcm14155292
Chicago/Turabian StyleMidlej, Kareem, Peter Proff, Nezar Watted, and Fuad A. Iraqi. 2025. "Cross-Sectional Study of Variations in Cephalometric Parameters in Arab Orthodontic Patients with Skeletal Class I and II" Journal of Clinical Medicine 14, no. 15: 5292. https://doi.org/10.3390/jcm14155292
APA StyleMidlej, K., Proff, P., Watted, N., & Iraqi, F. A. (2025). Cross-Sectional Study of Variations in Cephalometric Parameters in Arab Orthodontic Patients with Skeletal Class I and II. Journal of Clinical Medicine, 14(15), 5292. https://doi.org/10.3390/jcm14155292








