Computer Use and Compressive Neuropathies of the Upper Limbs: A Hidden Risk?
Abstract
1. Introduction
2. Methodology
3. Epidemiology of Compressive Neuropathies of the Upper Limb in Computer Users
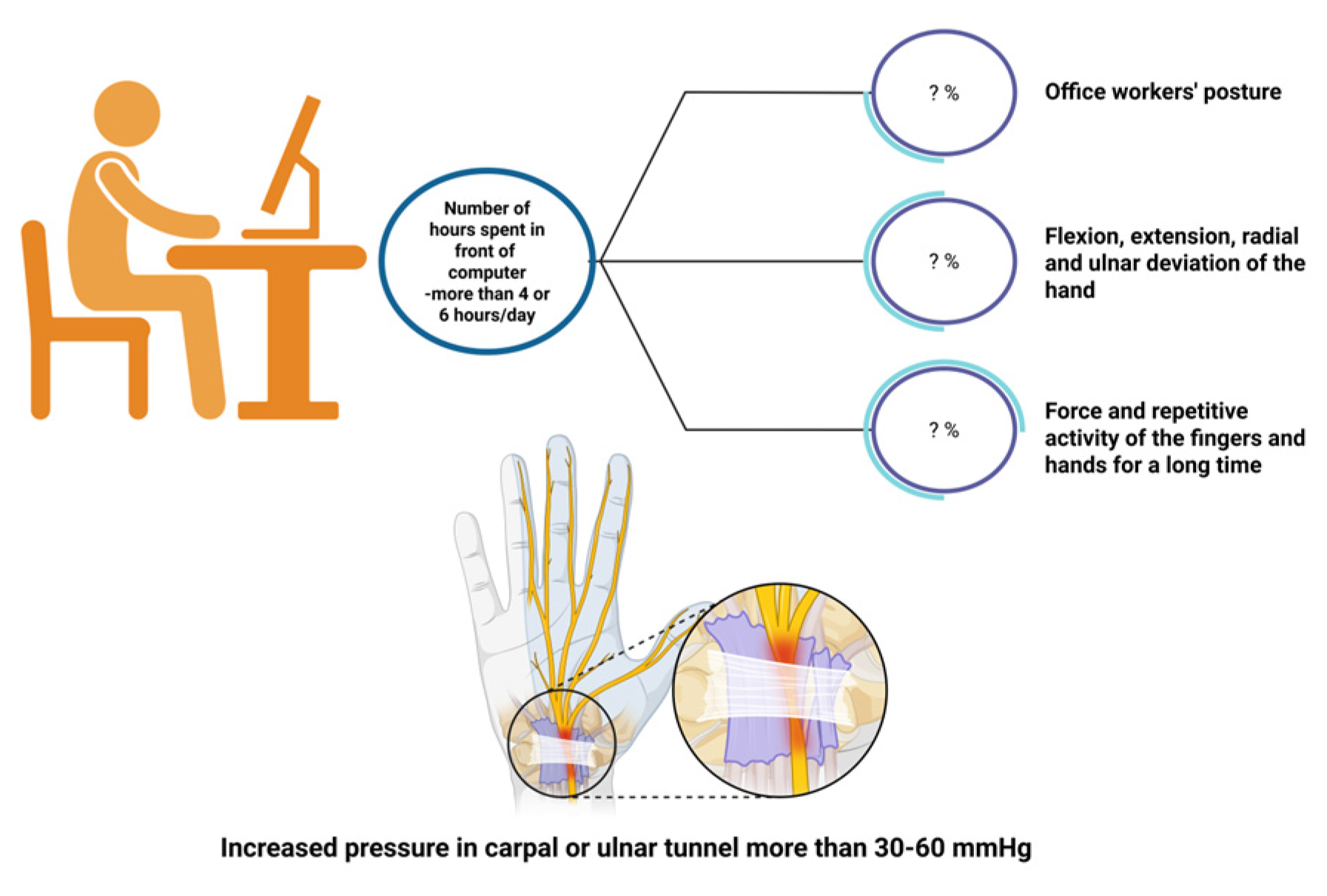
4. Pathophysiological Mechanisms of Compressive Neuropathies of the Upper Limbs
5. Risk Factors Associated with Computer Use—What Do the Studies Show?
6. Others Risk Factors and Compressive Neuropathies
7. Diagnostic Considerations for Median and Ulnar Neuropathy in Computer Users
8. Computer Work-Related Management and Prevention Recommendations
9. Discussions
10. Future Directions and Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| AAOS | American Academy of Orthopedic Surgeons |
| ACGIH | American Conference of Governmental Industrial Hygienists |
| BCTQ | Boston Carpal Tunnel Syndrome Questionnaire |
| BMI | Body Mass Index |
| CTS | Carpal Tunnel Syndrome |
| CMAP | Compound Muscle Action Potential |
| CuTS | Cubital Tunnel Syndrome |
| DCS | Double Crush Syndrome |
| EDX | Electrodiagnosis |
| HAL | Hand-Activity Level |
| MNW | Median Neuropathy at the Wrist |
| MRI | Magnetic Resonance Imaging |
| NCS | Nerve Conduction Studies |
| NMUS | Neuromuscular Ultrasound |
| TLV | Threshold Limit Value |
| UNE | Ulnar Neuropathy at the Elbow |
| UNW | Ulnar Neuropathy at the Wrist |
| WMSDs | Work-related Musculoskeletal Disorders |
References
- Feng, B.; Chen, K.; Zhu, X.; Ip, W.-Y.; Andersen, L.L.; Page, P.; Wang, Y. Prevalence and risk factors of self-reported wrist and hand symptoms and clinically confirmed carpal tunnel syndrome among office workers in China: A cross-sectional study. BMC Public Health 2021, 21, 57. [Google Scholar] [CrossRef] [PubMed]
- Threesittidath, K.; Chaibal, S.; Nitayarak, H. Effects of 1-hour computer use on ulnar and median nerve conduction velocity and muscle activity in office workers. J. Occup. Health 2024, 66, uiae023. [Google Scholar] [CrossRef] [PubMed]
- Malik, T.; Malik, A.; Abd-Elsayed, A. Pathophysiology of Work-Related Neuropathies. Biomedicines 2023, 11, 1745. [Google Scholar] [CrossRef] [PubMed]
- Ali, K.M.; Sathiyasekaran, B.W.C. Computer Professionals and Carpal Tunnel Syndrome (CTS). Int. J. Occup. Saf. Ergon. 2006, 12, 319–325. [Google Scholar] [CrossRef] [PubMed]
- Sonoo, M.; Menkes, D.L.; Bland, J.D.P.; Burke, D. Nerve conduction studies and EMG in carpal tunnel syndrome: Do they add value? Clin. Neurophysiol. Pract. 2018, 3, 78–88. [Google Scholar] [CrossRef] [PubMed]
- Atroshi, I.; Gummesson, C.; Johnsson, R.; Ornstein, E.; Ranstam, J.; Rosén, I. Prevalence of carpal tunnel syndrome in a general population. JAMA 1999, 282, 153–158. [Google Scholar] [CrossRef] [PubMed]
- Lleva, J.M.C.; Munakomi, S.; Chang, K.-V. Ulnar Neuropathy. In StatPearls; StatPearls Publishing: Treasure Island, FL, USA, 2023. Available online: https://www.ncbi.nlm.nih.gov/books/NBK534226/ (accessed on 6 May 2025).
- An, T.W.; Evanoff, B.A.; Boyer, M.I.; Osei, D.A. The Prevalence of Cubital Tunnel Syndrome: A Cross-Sectional Study in a U.S. Metropolitan Cohort. J. Bone Jt. Surg. Am. 2017, 99, 408–416. [Google Scholar] [CrossRef] [PubMed]
- Dupont, C.; Cloutier, G.E.; Prevost, Y.; Dion, M.A. Ulnar-Tunnel Syndrome at the Wrist. A Report of Four Cases Ulnar-Nerve Compression at the Wrist. J. Bone Jt. Surg. Am. 1965, 47, 757–761. [Google Scholar] [CrossRef]
- Novak, C.B.; Mackinnon, S.E. Multilevel nerve compression and muscle imbalance in work-related neuromuscular disorders. Am. J. Ind. Med. 2002, 41, 343–352. [Google Scholar] [CrossRef] [PubMed]
- Ochoa-Cacique, D.; Córdoba-Mosqueda, M.E.; Aguilar-Calderón, J.R.; García-González, U.; Ibarra-De la Torre, A.; Reyes-Rodríguez, V.A.; Lomelí-Ramírez, J.d.J.; Medina-Carrillo, Ó.; Sánchez-Calderón, M.D.; Castañeda-Ramírez, E.A. Double crush syndrome: Epidemiology, diagnosis, and treatment results. Neurochirurgie 2021, 67, 165–169. [Google Scholar] [CrossRef] [PubMed]
- Hagberg, M.; Morgenstern, H.; Kelsh, M. Impact of occupations and job tasks on the prevalence of carpal tunnel syndrome. Scand. J. Work Environ. Health 1992, 18, 337–345. [Google Scholar] [CrossRef] [PubMed]
- Hegmann, K.T.; Thiese, M.S.; Wood, E.M.; Garg, A.; Kapellusch, J.M.; Foster, J.; Biggs, J.; Edwards, H.; Wertsch, J.; Kendall, R. Impacts of differences in epidemiological case definitions on prevalence for upper-extremity musculoskeletal disorders. Hum. Factors 2014, 56, 191–202. [Google Scholar] [CrossRef] [PubMed]
- Lee, I.-H.; Kim, Y.-K.; Kang, D.-M.; Kim, S.-Y.; Kim, I.-A.; Kim, E.-M. Distribution of age, gender, and occupation among individuals with carpal tunnel syndrome based on the National Health Insurance data and National Employment Insurance data. Ann. Occup. Environ. Med. 2019, 31, e31. [Google Scholar] [CrossRef] [PubMed]
- Alavi, S.S.; Abbasi, M.; Mehrdad, R. Risk Factors for Upper Extremity Musculoskeletal Disorders Among Office Workers in Qom Province, Iran. Iran. Red Crescent Med. J. 2016, 18, e29518. [Google Scholar] [CrossRef] [PubMed]
- Ortiz-Hernández, L.; Tamez-González, S.; Martínez-Alcántara, S.; Méndez-Ramírez, I. Computer use increases the risk of musculoskeletal disorders among newspaper office workers. Arch. Med. Res. 2003, 34, 331–342. [Google Scholar] [CrossRef] [PubMed]
- Clarke Stevens, J.; Witt, J.C.; Smith, B.E.; Weaver, A.L. The frequency of carpal tunnel syndrome in computer users at a medical facility. Neurology 2001, 56, 1568–1570. [Google Scholar] [CrossRef] [PubMed]
- Thomsen, J.F.; Gerr, F.; Atroshi, I. Carpal tunnel syndrome and the use of computer mouse and keyboard: A systematic review. BMC Musculoskelet. Disord. 2008, 9, 134. [Google Scholar] [CrossRef] [PubMed]
- Shiri, R.; Falah-Hassani, K. Computer use and carpal tunnel syndrome: A meta-analysis. J. Neurol. Sci. 2015, 349, 15–19. [Google Scholar] [CrossRef] [PubMed]
- Mediouni, Z.; de Roquemaurel, A.; Dumontier, C.; Becour, B.; Garrabe, H.; Roquelaure, Y.; Descatha, A. Is carpal tunnel syndrome related to computer exposure at work? A review and meta-analysis. J. Occup. Environ. Med. 2014, 56, 204–208. [Google Scholar] [CrossRef] [PubMed]
- Bibi, M.; Khan, B. Carpal Tunnel Syndrome and use of computer keyboard and mouse; a systematic review. Rehman J. Health Sci. 2019, 1, 25–27. [Google Scholar]
- Mediouni, Z.; Bodin, J.; Dale, A.M.; Herquelot, E.; Carton, M.; Leclerc, A.; Fouquet, N.; Dumontier, C.; Roquelaure, Y.; Evanoff, B.A.; et al. Carpal tunnel syndrome and computer exposure at work in two large complementary cohorts. BMJ Open 2015, 5, e008156. [Google Scholar] [CrossRef] [PubMed]
- Bhanderi, D.; Mishra, D.; Parikh, S.; Sharma, D. Computer Use and Carpal Tunnel Syndrome: A Case-control Study. Indian J. Occup. Environ. Med. 2017, 21, 109–114. [Google Scholar] [CrossRef] [PubMed]
- Atroshi, I.; Gummesson, C.; Ornstein, E.; Johnsson, R.; Ranstam, J. Carpal tunnel syndrome and keyboard use at work: A population-based study. Arthritis Rheum. 2007, 56, 3620–3625. [Google Scholar] [CrossRef] [PubMed]
- Bibi, M.; Khan, B.; Ahmad, S.R.; Hassanat, A.; Ijaz, R.; Usman, H. Prevalence of carpal tunnel syndrome in computer operators of Peshawar. Rehman J. Health Sci. 2019, 1, 21–23. [Google Scholar]
- Demissie, B.; Yenew, C.; Alemu, A.; Bantie, B.; Sume, B.W.; Deml, Y.A.; Tegegne, E. Carpal tunnel syndrome and its associated factors among computer user bankers in South Gondar Zone, Northwest Ethiopia, 2021: A cross sectional study. BMC Musculoskelet. Disord. 2023, 24, 828. [Google Scholar] [CrossRef] [PubMed]
- Kurane, S.C.; Sakate, S. Prevalence of Carpal Tunnel Syndrome Among Computer-Using Non-teaching Staff From Select Educational Institutes at Sangli. Cureus 2025, 17, e81000. [Google Scholar] [CrossRef] [PubMed]
- Ganeriwal, A.; Biswas, D.; Srivastava, T. The effects of working hours on nerve conduction test in computer operators. Malays. Orthop. J. 2013, 7, 1–6. [Google Scholar] [CrossRef] [PubMed]
- Permissible Exposure Limits—Important Note Regarding the ACGIH TLV|OSHA.gov|Occupational Safety and Health Administration. Available online: https://www.osha.gov/annotated-pels/note (accessed on 25 January 2025).
- Kozak, A.; Schedlbauer, G.; Wirth, T.; Euler, U.; Westermann, C.; Nienhaus, A. Association between work-related biomechanical risk factors and the occurrence of carpal tunnel syndrome: An overview of systematic reviews and a meta-analysis of current research. BMC Musculoskelet. Disord. 2015, 16, 231. [Google Scholar] [CrossRef] [PubMed]
- Rotaru-Zavaleanu, A.-D.; Lungulescu, C.V.; Bunescu, M.G.; Vasile, R.C.; Gheorman, V.; Gresita, A.; Dinescu, V.C. Occupational Carpal Tunnel Syndrome: A scoping review of causes, mechanisms, diagnosis, and intervention strategies. Front. Public Health 2024, 12, 1407302. [Google Scholar] [CrossRef] [PubMed]
- Conlon, C.F.; Rempel, D.M. Upper extremity mononeuropathy among engineers. J. Occup. Environ. Med. 2005, 47, 1276–1284. [Google Scholar] [CrossRef] [PubMed]
- Nainzadeh, N.K.; Ilizarov, S.; Piligian, G.; Dropkin, J.; Breyre, A. Ulnar neuropathy at the elbow in computer keyboard operators. Work 2011, 39, 93–101. [Google Scholar] [CrossRef] [PubMed]
- Andersen, J.H.; Frost, P.; Fuglsang-Frederiksen, A.; Johnson, B.; Svendsen, S.W. Computer use and ulnar neuropathy: Results from a case-referent study. Work 2012, 41 (Suppl. S1), 2434–2437. [Google Scholar] [CrossRef] [PubMed]
- Roquelaure, Y.; Ha, C.; Leclerc, A.; Touranchet, A.; Sauteron, M.; Melchior, M.; Imbernon, E.; Goldberg, M. Epidemiologic surveillance of upper-extremity musculoskeletal disorders in the working population. Arthritis Care Res. 2006, 55, 765–778. [Google Scholar] [CrossRef] [PubMed]
- Gozke, E.; Dortcan, N.; Kocer, A.; Cetinkaya, M.; Akyuz, G.; Us, O. Ulnar nerve entrapment at wrist associated with carpal tunnel syndrome. Neurophysiol. Clin. 2003, 33, 219–222. [Google Scholar] [CrossRef] [PubMed]
- Doughty, C.T.; Bowley, M.P. Entrapment Neuropathies of the Upper Extremity. Med. Clin. N. Am. 2019, 103, 357–370. [Google Scholar] [CrossRef] [PubMed]
- Gupta, R.; Nassiri, N.; Hazel, A.; Bathen, M.; Mozaffar, T. Chronic nerve compression alters Schwann cell myelin architecture in a murine model. Muscle Nerve 2012, 45, 231–241. [Google Scholar] [CrossRef] [PubMed]
- Gupta, R.; Truong, L.; Bear, D.; Chafik, D.; Modafferi, E.; Hung, C.T. Shear stress alters the expression of myelin-associated glycoprotein (MAG) and myelin basic protein (MBP) in Schwann cells. J. Orthop. Res. 2005, 23, 1232–1239. [Google Scholar] [CrossRef] [PubMed]
- Mackinnon, S.E.; Dellon, A.L.; Hudson, A.R.; Hunter, D.A. Chronic human nerve compression—A histological assessment. Neuropathol. Appl. Neurobiol. 1986, 12, 547–565. [Google Scholar] [CrossRef] [PubMed]
- Berger, B.L.; Gupta, R. Demyelination secondary to chronic nerve compression injury alters Schmidt-Lanterman incisures. J. Anat. 2006, 209, 111–118. [Google Scholar] [CrossRef] [PubMed]
- Gupta, R.; Steward, O. Chronic nerve compression induces concurrent apoptosis and proliferation of Schwann cells. J. Comp. Neurol. 2003, 461, 174–186. [Google Scholar] [CrossRef] [PubMed]
- Maeda, Y.; Kettner, N.; Holden, J.; Lee, J.; Kim, J.; Cina, S.; Malatesta, C.; Gerber, J.; McManus, C.; Im, J.; et al. Functional deficits in carpal tunnel syndrome reflect reorganization of primary somatosensory cortex. Brain 2014, 137 Pt 6, 1741–1752. [Google Scholar] [CrossRef] [PubMed]
- Napadow, V.; Kettner, N.; Ryan, A.; Kwong, K.K.; Audette, J.; Hui, K.K.S. Somatosensory cortical plasticity in carpal tunnel syndrome—A cross-sectional fMRI evaluation. Neuroimage 2006, 31, 520–530. [Google Scholar] [CrossRef] [PubMed]
- Ma, H.; Lu, Y.; Hua, X.; Shen, Y.; Zheng, M.; Xu, W. A Longitudinal fMRI Research on Neural Plasticity and Sensory Outcome of Carpal Tunnel Syndrome. Neural Plast. 2017, 2017, 5101925. [Google Scholar] [CrossRef] [PubMed]
- Bamac, B.; Colak, S.; Dundar, G.; Selekler, H.M.; Taşkiran, Y.; Colak, T.; Balci, E. Influence of the long term use of a computer on median, ulnar and radial sensory nerves in the wrist region. Int. J. Occup. Med. Environ. Health 2014, 27, 1026–1035. [Google Scholar] [CrossRef] [PubMed]
- Kurtul, S.; Mazican, N. Prevalence and risk factors for self-reported symptoms of carpal tunnel syndrome among hospital office workers: A cross-sectional study. Int. J. Occup. Saf. Ergon. 2023, 29, 461–465. [Google Scholar] [CrossRef] [PubMed]
- Andersen, J.H.; Thomsen, J.F.; Overgaard, E.; Lassen, C.F.; Brandt, L.P.A.; Vilstrup, I.; Kryger, A.I.; Mikkelsen, S. Computer use and carpal tunnel syndrome: A 1-year follow-up study. JAMA 2003, 289, 2963–2969. [Google Scholar] [CrossRef] [PubMed]
- Oveisi, E.; Khanlari, P.; Ebrahimzadeh-Afrouzi, M. Carpal tunnel syndrome severity, hand discomfort, and usability among three types of computer mouse. Work 2024, 77, 873–882. [Google Scholar] [CrossRef] [PubMed]
- Lundborg, G.; Gelberman, R.H.; Minteer-Convery, M.; Lee, Y.F.; Hargens, A.R. Median nerve compression in the carpal tunnel—Functional response to experimentally induced controlled pressure. J. Hand Surg. 1982, 7, 252–259. [Google Scholar] [CrossRef] [PubMed]
- Keir, P.J.; Bach, J.M.; Rempel, D. Effects of computer mouse design and task on carpal tunnel pressure. Ergonomics 1999, 42, 1350–1360. [Google Scholar] [CrossRef] [PubMed]
- Toosi, K.K.; Impink, B.G.; Baker, N.A.; Boninger, M.L. Effects of computer keyboarding on ultrasonographic measures of the median nerve. Am. J. Ind. Med. 2011, 54, 826–833. [Google Scholar] [CrossRef] [PubMed]
- Werner, C.O.; Ohlin, P.; Elmqvist, D. Pressures recorded in ulnar neuropathy. Acta Orthop. 1985, 56, 404–406. [Google Scholar] [CrossRef] [PubMed]
- Aleksenko, D.; Varacallo, M.A. Guyon Canal Syndrome. In StatPearls; StatPearls Publishing: Treasure Island, FL, USA, 2023. Available online: https://www.ncbi.nlm.nih.gov/books/NBK431063/ (accessed on 6 May 2025).
- Shapiro, L.M.; Kamal, R.N.; Management of Carpal Tunnel Syndrome Work Group; American Academy of Orthopaedic Surgeons. American Academy of Orthopaedic Surgeons/ASSH Clinical Practice Guideline Summary Management of Carpal Tunnel Syndrome. J. Am. Acad. Orthop. Surg. 2024, 33, e356–e366. [Google Scholar] [CrossRef] [PubMed]
- Graham, B.; Peljovich, A.E.; Afra, R.; Cho, M.S.; Gray, R.; Stephenson, J.; Gurman, A.; MacDermid, J.; Mlady, G.; Patel, A.T.; et al. The American Academy of Orthopaedic Surgeons Evidence-Based Clinical Practice Guideline on Management of Carpal Tunnel Syndrome. J. Bone Jt. Surg. Am. 2016, 98, 1750–1754. [Google Scholar] [CrossRef] [PubMed]
- Lal, S.; Bairwa, J.; Saini, M.K.; Tak, M.S.; Bhati, M. Osteochondroma of Distal End Radius Presenting as Carpal Tunnel Syndrome: A Case Report. J. Orthop. Case Rep. 2024, 14, 57–61. [Google Scholar] [CrossRef] [PubMed]
- Shiri, R. Arthritis as a risk factor for carpal tunnel syndrome: A meta-analysis. Scand. J. Rheumatol. 2016, 45, 339–346. [Google Scholar] [CrossRef] [PubMed]
- Roy, U.; Srivastava, A.K.; Cartwright, M.S.; Panwar, A.; Shahil, P. A Case of Suspected Carpal Tunnel Syndrome: Ultrasonography Prior to the Scalpel. Cureus 2024, 16, e65823. [Google Scholar] [CrossRef] [PubMed]
- Pourmemari, M.H.; Shiri, R. Diabetes as a risk factor for carpal tunnel syndrome: A systematic review and meta-analysis. Diabet. Med. 2016, 33, 10–16. [Google Scholar] [CrossRef] [PubMed]
- Choi, J.H.; Kim, H.R.; Song, K.H. Musculoskeletal complications in patients with diabetes mellitus. Korean J. Intern. Med. 2022, 37, 1099–1110. [Google Scholar] [CrossRef] [PubMed]
- Osiak, K.; Elnazir, P.; Walocha, J.A.; Pasternak, A. Carpal tunnel syndrome: State-of-the-art review. Folia Morphol. 2022, 81, 851–862. [Google Scholar] [CrossRef] [PubMed]
- Zimmerman, M.; Nilsson, P.; Rydberg, M.; Dahlin, L. Risk of hand and forearm conditions due to vibrating hand-held tools exposure: A retrospective cohort study from Sweden. BMJ Open 2024, 14, e080777. [Google Scholar] [CrossRef] [PubMed]
- Razavi, A.S.; Karimi, N.; Bashiri, F. The relationship of serum lipid profiles and obesity with the severity of carpal tunnel syndrome. Pan. Afr. Med. J. 2021, 39, 90. [Google Scholar] [CrossRef] [PubMed]
- Lewańska, M.; Wagrowska-Koski, E.; Walusiak-Skorupa, J. Etiological factors for developing carpal tunnel syndrome in people who work with computers. Med. Pract. Work Health Saf. 2013, 64, 37–45. [Google Scholar] [CrossRef] [PubMed]
- Lawson, I.J. Is carpal tunnel syndrome caused by work with vibrating tools? Occup. Med. 2020, 70, 8–10. [Google Scholar] [CrossRef] [PubMed]
- Wiberg, A.; Ng, M.; Schmid, A.B.; Smillie, R.W.; Baskozos, G.; Holmes, M.V.; Künnapuu, K.; Mägi, R.; Bennett, D.L.; Furniss, D. A genome-wide association analysis identifies 16 novel susceptibility loci for carpal tunnel syndrome. Nat. Commun. 2019, 10, 1030. [Google Scholar] [CrossRef] [PubMed]
- Kamolz, L.-P.; Beck, H.; Haslik, W.; Högler, R.; Rab, M.; Schrögendorfer, K.F.; Frey, M. Carpal tunnel syndrome: A question of hand and wrist configurations? J. Hand Surg. 2004, 29, 321–324. [Google Scholar] [CrossRef] [PubMed]
- Ferry, S.; Hannaford, P.; Warskyj, M.; Lewis, M.; Croft, P. Carpal tunnel syndrome: A nested case-control study of risk factors in women. Am. J. Epidemiol. 2000, 151, 566–574. [Google Scholar] [CrossRef] [PubMed]
- Rozali, Z.I.; Noorman, F.M.; De Cruz, P.K.; Feng, Y.K.; Razab, H.W.; Sapuan, J.; Singh, R.; Sikkandar, F.M. Impact of carpal tunnel syndrome on the expectant woman’s life. Asia Pac. Fam. Med. 2012, 11, 1. [Google Scholar] [CrossRef] [PubMed]
- Duan, X.; Zhang, T.; Wang, K. Causal relationship between hypothyroidism and peripheral neuropathy: A Mendelian randomization study of European ancestry. Front. Endocrinol. 2024, 15, 1436823. [Google Scholar] [CrossRef] [PubMed]
- Karne, S.S.; Bhalerao, N.S. Carpal Tunnel Syndrome in Hypothyroidism. J. Clin. Diagn. Res. 2016, 10, OC36–OC38. [Google Scholar] [CrossRef] [PubMed]
- Roshanzamir, S.; Mortazavi, S.; Dabbaghmanesh, A. Does Hypothyroidism Affect Post-Operative Outcome of Patients Undergoing Carpal Tunnel Release? Electron. Physician 2016, 8, 2977–2981. [Google Scholar] [CrossRef] [PubMed]
- Papanas, N.; Stamatiou, I.; Papachristou, S. Carpal Tunnel Syndrome in Diabetes Mellitus. Curr. Diabetes Rev. 2021, 18, e010921196025. [Google Scholar] [CrossRef] [PubMed]
- Drăghici, N.C.; Leucuța, D.C.; Ciobanu, D.M.; Stan, A.D.; Lupescu, T.D.; Mureșanu, D.F. Clinical Utility of Boston-CTS and Six-Item CTS Questionnaires in Carpal Tunnel Syndrome Associated with Diabetic Polyneuropathy. Diagnostics 2022, 13, 4. [Google Scholar] [CrossRef] [PubMed]
- Becker, J.; Nora, D.B.; Gomes, I.; Stringari, F.F.; Seitensus, R.; Panosso, J.S.; Ehlers, J.A.C. An evaluation of gender, obesity, age and diabetes mellitus as risk factors for carpal tunnel syndrome. Clin. Neurophysiol. 2002, 113, 1429–1434. [Google Scholar] [CrossRef] [PubMed]
- Shiri, R.; Pourmemari, M.H.; Falah-Hassani, K.; Viikari-Juntura, E. The effect of excess body mass on the risk of carpal tunnel syndrome: A meta-analysis of 58 studies. Obes. Rev. 2015, 16, 1094–1104. [Google Scholar] [CrossRef] [PubMed]
- Landau, M.E.; Barner, K.C.; Campbell, W.W. Effect of body mass index on ulnar nerve conduction velocity, ulnar neuropathy at the elbow, and carpal tunnel syndrome. Muscle Nerve 2005, 32, 360–363. [Google Scholar] [CrossRef] [PubMed]
- Lampainen, K.; Hulkkonen, S.; Ryhänen, J.; Curti, S.; Shiri, R. Is Smoking Associated with Carpal Tunnel Syndrome? A Meta-Analysis. Healthcare 2022, 10, 1988. [Google Scholar] [CrossRef] [PubMed]
- Chauhan, M.; Anand, P.; Das, J.M. Cubital Tunnel Syndrome. In StatPearls; StatPearls Publishing: Treasure Island, FL, USA, 2023. Available online: https://www.ncbi.nlm.nih.gov/books/NBK538259/ (accessed on 22 June 2025).
- Davids, F.A.; Ramtin, S.; Razi, A.; Ring, D.; Teunis, T.; Reichel, L.M.; Kraan, G.A.; Muhl, P.; Gilbert, R.S.; Siff, T.; et al. Variation in Interpretation of Provocative Tests for Carpal Tunnel Syndrome. J. Hand Surg. 2024, in press. [Google Scholar] [CrossRef] [PubMed]
- Beekman, R.; Schreuder, A.H.C.M.L.; Rozeman, C.A.M.; Koehler, P.J.; Uitdehaag, B.M.J. The diagnostic value of provocative clinical tests in ulnar neuropathy at the elbow is marginal. J. Neurol. Neurosurg. Psychiatry 2009, 80, 1369–1374. [Google Scholar] [CrossRef] [PubMed]
- Kleggetveit, I.P.; Jørum, E. Diagnosis of carpal tunnel syndrome. Scand. J. Pain 2018, 18, 333–337. [Google Scholar] [CrossRef] [PubMed]
- American Association of Electrodiagnostic Medicine; American Academy of Neurology; American Academy of Physical Medicine and Rehabilitation. Practice parameter for electrodiagnostic studies in carpal tunnel syndrome: Summary statement. Muscle Nerve 2002, 25, 918–922. [Google Scholar] [CrossRef] [PubMed]
- Zivkovic, S.; Gruener, G.; Arnold, M.; Winter, C.; Nuckols, T.; Narayanaswami, P. Quality measures in electrodiagnosis: Carpal tunnel syndrome—An AANEM Quality Measure Set. Muscle Nerve 2020, 61, 460–465. [Google Scholar] [CrossRef] [PubMed]
- Pelosi, L.; Arányi, Z.; Beekman, R.; Bland, J.; Coraci, D.; Hobson-Webb, L.D.; Padua, L.; Podnar, S.; Simon, N.; van Alfen, N.; et al. Expert consensus on the combined investigation of ulnar neuropathy at the elbow using electrodiagnostic tests and nerve ultrasound. Clin. Neurophysiol. 2021, 132, 2274–2281. [Google Scholar] [CrossRef] [PubMed]
- Katzberg, H.D.; Bril, V.; Breiner, A. Ultrasound in Neuromuscular Disorders. J. Clin. Neurophysiol. 2016, 33, 80–85. [Google Scholar] [CrossRef] [PubMed]
- Aseem, F.; Williams, J.W.; Walker, F.O.; Cartwright, M.S. Neuromuscular ultrasound in patients with carpal tunnel syndrome and normal nerve conduction studies. Muscle Nerve 2017, 55, 913–915. [Google Scholar] [CrossRef] [PubMed]
- Cartwright, M.S.; Hobson-Webb, L.D.; Boon, A.J.; Alter, K.E.; Hunt, C.H.; Flores, V.H.; Werner, R.A.; Shook, S.J.; Thomas, T.D.; Primack, S.J.; et al. Evidence-based guideline: Neuromuscular ultrasound for the diagnosis of carpal tunnel syndrome. Muscle Nerve 2012, 46, 287–293. [Google Scholar] [CrossRef] [PubMed]
- Pelosi, L.; Arányi, Z.; Beekman, R.; Bland, J.; Coraci, D.; Hobson-Webb, L.D.; Padua, L.; Podnar, S.; Simon, N.; van Alfen, N.; et al. Expert consensus on the combined investigation of carpal tunnel syndrome with electrodiagnostic tests and neuromuscular ultrasound. Clin. Neurophysiol. 2022, 135, 107–116. [Google Scholar] [CrossRef] [PubMed]
- Shook, S.J.; Ginsberg, M.; Narayanaswami, P.; Beekman, R.; Dubin, A.H.; Katirji, B.; Swaminathan, B.; Werner, R.A.; Cartwright, M.S. Evidence-based guideline: Neuromuscular ultrasound for the diagnosis of ulnar neuropathy at the elbow. Muscle Nerve 2022, 65, 147–153. [Google Scholar] [CrossRef] [PubMed]
- Carroll, T.J.; Chirokikh, A.; Thon, J.; Jones, C.M.C.; Logigian, E.; Ketonis, C. Diagnosis of Ulnar Neuropathy at the Elbow Using Ultrasound—A Comparison to Electrophysiologic Studies. J. Hand Surg. 2023, 48, 1229–1235. [Google Scholar] [CrossRef] [PubMed]
- Onen, M.R.; Kayalar, A.E.; Ilbas, E.N.; Gokcan, R.; Gulec, I.; Naderi, S. The role of wrist magnetic resonance imaging in the differential diagnosis of the carpal tunnel syndrome. Turk. Neurosurg. 2015, 25, 701–706. [Google Scholar] [CrossRef] [PubMed]
- Ahmed, I.; Shaukat, M.Z. Computer users’ ergonomics and quality of life–evidence from a developing country. Int. J. Inj. Control Saf. Promot. 2018, 25, 154–161. [Google Scholar] [CrossRef] [PubMed]
- Trillos-Chacón, M.C.; Castillo-M, J.A.; Tolosa-Guzman, I.; Medina, A.F.S.; Ballesteros, S.M. Strategies for the prevention of carpal tunnel syndrome in the workplace: A systematic review. Appl. Ergon. 2021, 93, 103353. [Google Scholar] [CrossRef] [PubMed]
- de Waal, A.; Killian, A.; Gagela, A.; Baartzes, J.; de Klerk, S. Therapeutic Approaches for the Prevention of Upper Limb Repetitive Strain Injuries in Work-Related Computer Use: A Scoping Review. J. Occup. Rehabil. 2024, 35, 234–267. [Google Scholar] [CrossRef] [PubMed]
- Meals, C.; Koenigsberg, E.S. Ergonomic Strategies for Computer Users with Upper Limb Problems. J. Hand Surg. 2015, 40, 1688–1691. [Google Scholar] [CrossRef] [PubMed]
- Hoe, V.C.W.; Urquhart, D.M.; Kelsall, H.L.; Sim, M.R. Ergonomic design and training for preventing work-related musculoskeletal disorders of the upper limb and neck in adults. Cochrane Database Syst. Rev. 2012, 2012, CD008570. [Google Scholar] [CrossRef] [PubMed]
- O’Connor, D.; Page, M.J.; Marshall, S.C.; Massy-Westropp, N. Ergonomic positioning or equipment for treating carpal tunnel syndrome. Cochrane Database Syst. Rev. 2012, 2012, CD009600. [Google Scholar] [CrossRef] [PubMed]
- Łach, P.; Cygańska, A.K. Effectiveness Of Prevention Exercises Protocol Among Office Workers with Symptoms of Carpal Tunnel Syndrome. Int. J. Occup. Med. Environ. Health 2024, 37, 45–57. [Google Scholar] [CrossRef] [PubMed]
- Ekinci, Y.; Uysal, S.A.; Kabak, V.Y.; Duger, T. Does ergonomics training have an effect on body posture during computer usage? J. Back Musculoskelet. Rehabil. 2019, 32, 191–195. [Google Scholar] [CrossRef] [PubMed]
- Çupi, B.; Šarac, I.; Jovanović, J.J.; Jovanović, S.; Petrović-Oggiano, G.; Debeljak-Martačić, J. Occupational and non-occupational risk factors correlating with the severity of clinical manifestations of carpal tunnel syndrome and related work disability among workers who work with a computer. Arch. Ind. Hyg. Toxicol. 2023, 74, 252–272. [Google Scholar] [CrossRef] [PubMed]
- Chiang, C.L.; Liao, C.Y.; Kuo, H.W. Postures of upper extremity correlated with carpal tunnel syndrome (CTS). Int. J. Occup. Med. Environ. Health 2017, 30, 281–290. [Google Scholar] [CrossRef] [PubMed]
- Sherif Sirajudeen, M.; Saad Mohamed Siddik, S. Knowledge of Computer Ergonomics among Computer Science Engineering and Information Technology Students in Karnataka, India. Asian J. Pharm. Res. Health Care 2017, 9, 64–70. [Google Scholar] [CrossRef] [PubMed]



| First Author/Ref. | Type of Study | Sample Size | Conclusions |
|---|---|---|---|
| Thomsen J.F et al. (2008) [18] | Systematic review | 8 studies | -Epidemiological data on the link between computer use and CTS remain inconclusive, as no definitive study has yet clarified the relationship |
| Shiri R et al. (2014) [19] | Meta-analysis | 12 studies | -Excessive computer use, particularly prolonged mouse use, may be a minor occupational risk factor for CTS. Further prospective studies in office workers are needed, using objective measures of device use and CTS confirmation via NCS. |
| Mediouni Z et al. (2014) [20] | Meta-analysis | 6 studies | -No overall link was found between computer use and CTS, though specific work conditions may still pose an increased risk. |
| Bibi M et al. (2019) [21] | Systematic review | 8 studies | Prolonged keyboard and mouse use are considered key contributing factors in the development of CTS. |
| First Author/Ref. | Type of Study | Sample Size | Prevalence of CTS (%) | Confirmed with NCS |
|---|---|---|---|---|
| Mediouni Z et al. (2015) [22] | Observational longitudinal cohort study (3 years) | 1551 (Cosali study) 711 (PrediCTS study) | 2.3% 4.3% | No Yes |
| Bhanderi J et al. (2017) [23] | Case–control study (1.5 years) | 411 (137 cases and 274 controls) | - | No |
| Bibi M et al. (2019) [25] | Cross-sectional study | 247 | 15.5% | No |
| Feng B et al. (2021) [1] | Cross-sectional study | 969 | 9.6% | No |
| Demissie B et al. (2023) [26] | Cross-sectional study | 422 | 11.7% | No |
| Kurane et al. (2025) [27] | Cross-sectional study | 150 | 64.54% | No |
| First Author/Ref. | Type of Study | Sample Size | Confirmed with NCS | Conclusions |
|---|---|---|---|---|
| Conlon FC et al. (2005) [32] | Cross-sectional study (1 year) | 202 | yes | -13.9% prevalance of upper extremity entrapment neuropaty at the wrist; -Prevalence of UNW 1.8% (right), 2.9% (left). -Prevalance of CTS 10.3% (right), 3.4% (left); -The risk of entrapment neuropathy increased with increasing hours of computer use per week. |
| Nainzadeh NK et al. (2011) [33] | Case series (4 years) | 148 | yes | -Prevalance of UNE was identified 74.5% (105); -Of the 105 with UNE, 41 had co-existing CTS; |
| Andersen JH et al. (2012) [34] | Case-referent study (6 years) | 546 UNE | yes | -A negative exposure-response relation between hours of daily computer use and ulnar neuropathy; |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Vulpoi, G.-A.; Bistriceanu, C.E.; Bîrsanu, L.; Palade, C.-M.; Cuciureanu, D.I. Computer Use and Compressive Neuropathies of the Upper Limbs: A Hidden Risk? J. Clin. Med. 2025, 14, 5237. https://doi.org/10.3390/jcm14155237
Vulpoi G-A, Bistriceanu CE, Bîrsanu L, Palade C-M, Cuciureanu DI. Computer Use and Compressive Neuropathies of the Upper Limbs: A Hidden Risk? Journal of Clinical Medicine. 2025; 14(15):5237. https://doi.org/10.3390/jcm14155237
Chicago/Turabian StyleVulpoi, Georgiana-Anca, Cătălina Elena Bistriceanu, Lenuța Bîrsanu, Codrina-Madalina Palade, and Dan Iulian Cuciureanu. 2025. "Computer Use and Compressive Neuropathies of the Upper Limbs: A Hidden Risk?" Journal of Clinical Medicine 14, no. 15: 5237. https://doi.org/10.3390/jcm14155237
APA StyleVulpoi, G.-A., Bistriceanu, C. E., Bîrsanu, L., Palade, C.-M., & Cuciureanu, D. I. (2025). Computer Use and Compressive Neuropathies of the Upper Limbs: A Hidden Risk? Journal of Clinical Medicine, 14(15), 5237. https://doi.org/10.3390/jcm14155237










