The Role of Minimally Invasive Adrenalectomy for Large Adrenal Tumors (≥6 cm): Evidence from a 10-Year Retrospective Study
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design and Population
2.2. Surgical Techniques
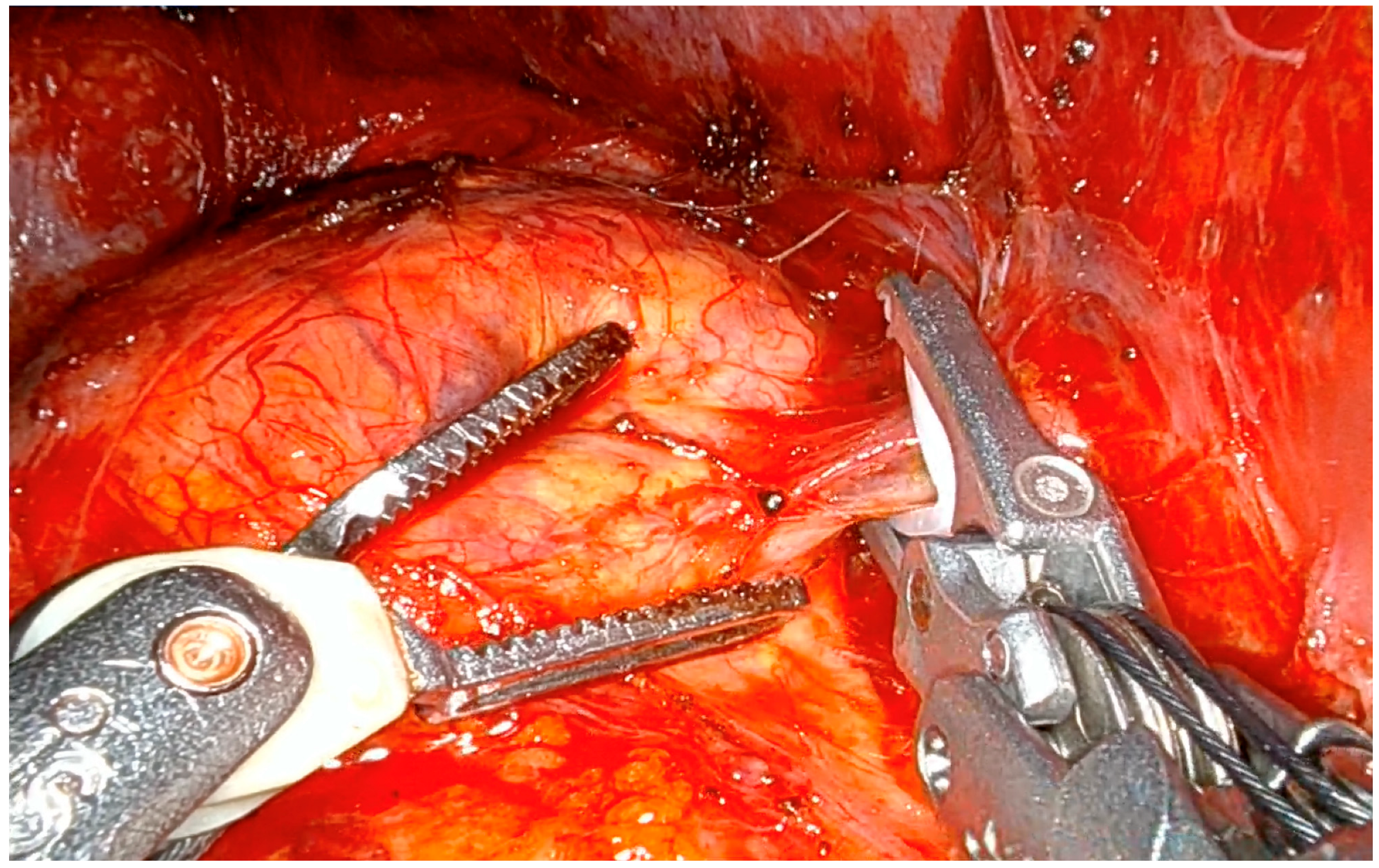
2.2.1. Lateral Transabdominal Adrenalectomy (Both Laparoscopic and Robotic)
2.2.2. Posterior Retroperitoneoscopic Adrenalectomy
2.2.3. Postoperative Course
2.3. Statistical Analysis
3. Results
3.1. Characteristics of the Study Population
3.2. Intraoperative and Postoperative Outcomes
3.3. Diagnostic Workup and Oncological Outcomes of ACC Patients
3.4. Multivariate Analyses
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Gagner, M.; Lacroix, A.; Bolté, E. Laparoscopic adrenalectomy in Cushing’s syndrome and pheochromocytoma. N. Engl. J. Med. 1992, 327, 1033. [Google Scholar] [CrossRef] [PubMed]
- Higashihara, E.; Tanaka, Y.; Horie, S.; Aruga, S.; Nutahara, K.; Homma, Y.; Minowada, S.; Aso, Y. A case report of laparoscopic adrenalectomy. Jpn. J. Urol. 1992, 83, 1130–1133. [Google Scholar] [CrossRef] [PubMed]
- Heger, P.; Probst, P.; Hüttner, F.J.; Gooßen, K.; Proctor, T.; Müller-Stich, B.P.; Strobel, O.; Büchler, M.W.; Diener, M.K. Evaluation of Open and Minimally Invasive Adrenalectomy: A Systematic Review and Network Meta-analysis. World J. Surg. 2017, 41, 2746–2757. [Google Scholar] [CrossRef] [PubMed]
- Pogorzelski, R.; Toutounchi, S.; Krajewska, E.; Fiszer, P.; Kącka, A.; Piotrowski, M.; Szostek, M.; Wołoszko, T.; Celejewski, K.; Ambroziak, U.; et al. The usefulness of laparoscopic adrenalectomy in the treatment of adrenal neoplasms—A single-centre experience. Endokrynol. Pol. 2017, 68, 407–410. [Google Scholar] [CrossRef] [PubMed]
- Li, J.; Wang, Y.; Chang, X.; Han, Z. Laparoscopic adrenalectomy (LA) vs open adrenalectomy (OA) for pheochromocytoma (PHEO): A systematic review and meta-analysis. Eur. J. Surg. Oncol. 2020, 46, 991–998. [Google Scholar] [CrossRef] [PubMed]
- Shen, W.T.; Lim, R.C.; Siperstein, A.E.; Clark, O.H.; Schecter, W.P.; Hunt, T.K.; Horn, J.K.; Duh, Q.Y. Laparoscopic vs. open adrenalectomy for the treatment of primary hyperaldosteronism. Arch. Surg. Chic. Ill 1960 1999, 134, 628–631; discussion 631–632. [Google Scholar] [CrossRef] [PubMed]
- Hazzan, D.; Shiloni, E.; Golijanin, D.; Jurim, O.; Gross, D.; Reissman, P. Laparoscopic vs open adrenalectomy for benign adrenal neoplasm. Surg. Endosc. 2001, 15, 1356–1358. [Google Scholar] [CrossRef] [PubMed]
- Materazzi, G.; Rossi, L. Robot-assisted adrenalectomy: State of the art. Updates Surg. 2021, 73, 1131–1146. [Google Scholar] [CrossRef] [PubMed]
- Guazzoni, G.; Montorsi, F.; Bocciardi, A.; Da Pozzo, L.; Rigatti, P.; Lanzi, R.; Pontiroli, A. Transperitoneal laparoscopic versus open adrenalectomy for benign hyperfunctioning adrenal tumors: A comparative study. J. Urol. 1995, 153, 1597–1600. [Google Scholar] [CrossRef] [PubMed]
- Zografos, G.N.; Farfaras, A.; Vasiliadis, G.; Pappa, T.; Aggeli, C.; Vassilatou, E.; Kaltsas, G.; Piaditis, G. Laparoscopic resection of large adrenal tumors. JSLS 2010, 14, 364–368. [Google Scholar] [CrossRef] [PubMed]
- Walz, M.K.; Alesina, P.F.; Wenger, F.A.; Deligiannis, A.; Szuczik, E.; Petersenn, S.; Ommer, A.; Groeben, H.; Peitgen, K.; Janssen, O.E.; et al. Posterior retroperitoneoscopic adrenalectomy--results of 560 procedures in 520 patients. Surgery 2006, 140, 943–948; discussion 948–950. [Google Scholar] [CrossRef] [PubMed]
- Kook, Y.; Choi, H.R.; Kang, S.-W.; Kim, J.K.; Lee, C.R.; Lee, J.; Jeong, J.J.; Nam, K.-H.; Chung, W.Y. Laparoscopic adrenalectomy: Comparison of outcomes between posterior retroperitoneoscopic and transperitoneal adrenalectomy with 10 years’ experience. Gland Surg. 2021, 10, 2104–2112. [Google Scholar] [CrossRef] [PubMed]
- Balla, A.; Palmieri, L.; Meoli, F.; Corallino, D.; Ortenzi, M.; Ursi, P.; Guerrieri, M.; Quaresima, S.; Paganini, A.M. Are Adrenal Lesions of 6 cm or More in Diameter a Contraindication to Laparoscopic Adrenalectomy? A Case-Control Study. World J. Surg. 2020, 44, 810–818. [Google Scholar] [CrossRef] [PubMed]
- Parente, A.; Verhoeff, K.; Wang, Y.; Wang, N.; Wang, Z.; Śledziński, M.; Hellmann, A.; Raffaelli, M.; Pennestrì, F.; Sywak, M.; et al. Robotic and Laparoscopic Adrenalectomy for Pheochromocytoma: An International Multicenter Study. Eur. Urol. Focus 2024, 11, 118–125. [Google Scholar] [CrossRef] [PubMed]
- Dalvi, A.N.; Thapar, P.M.; Thapar, V.B.; Rege, S.A.; Deshpande, A.A. Laparoscopic adrenalectomy for large tumours: Single team experience. J. Minimal Access Surg. 2012, 8, 125–128. [Google Scholar] [CrossRef] [PubMed]
- Hobart, M.G.; Gill, I.S.; Schweizer, D.; Sung, G.T.; Bravo, E.L. Laparoscopic adrenalectomy for large-volume (> or = 5 cm) adrenal masses. J. Endourol. 2000, 14, 149–154. [Google Scholar] [CrossRef]
- MacGillivray, D.C.; Whalen, G.F.; Malchoff, C.D.; Oppenheim, D.S.; Shichman, S.J. Laparoscopic resection of large adrenal tumors. Ann. Surg. Oncol. 2002, 9, 480–485. [Google Scholar] [CrossRef] [PubMed]
- Natkaniec, M.; Pędziwiatr, M.; Wierdak, M.; Major, P.; Migaczewski, M.; Matłok, M.; Budzyński, A.; Rembiasz, K. Laparoscopic Transperitoneal Lateral Adrenalectomy for Large Adrenal Tumors. Urol. Int. 2016, 97, 165–172. [Google Scholar] [CrossRef] [PubMed]
- Miller, B.S.; Gauger, P.G.; Hammer, G.D.; Doherty, G.M. Resection of adrenocortical carcinoma is less complete and local recurrence occurs sooner and more often after laparoscopic adrenalectomy than after open adrenalectomy. Surgery 2012, 152, 1150–1157. [Google Scholar] [CrossRef] [PubMed]
- Wu, K.; Liu, Z.; Liang, J.; Tang, Y.; Zou, Z.; Zhou, C.; Zhang, F.; Lu, Y. Laparoscopic versus open adrenalectomy for localized (stage 1/2) adrenocortical carcinoma: Experience at a single, high-volumecenter. Surgery 2018, 164, 1325–1329. [Google Scholar] [CrossRef]
- Fassnacht, M.; Tsagarakis, S.; Terzolo, M.; Tabarin, A.; Sahdev, A.; Newell-Price, J.; Pelsma, I.; Marina, L.; Lorenz, K.; Bancos, I.; et al. European Society of Endocrinology clinical practice guidelines on the management of adrenal incidentalomas, in collaboration with the European Network for the Study of Adrenal Tumors. Eur. J. Endocrinol. 2023, 189, G1–G42. [Google Scholar] [CrossRef] [PubMed]
- Charlson, M.E.; Pompei, P.; Ales, K.L.; MacKenzie, C.R. A new method of classifying prognostic comorbidity in longitudinal studies: Development and validation. J. Chronic Dis. 1987, 40, 373–383. [Google Scholar] [CrossRef] [PubMed]
- Daabiss, M. American Society of Anaesthesiologists physical status classification. Indian J. Anaesth. 2011, 55, 111–115. [Google Scholar] [CrossRef] [PubMed]
- Dindo, D.; Demartines, N.; Clavien, P.-A. Classification of surgical complications: A new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann. Surg. 2004, 240, 205–213. [Google Scholar] [CrossRef] [PubMed]
- Slankamenac, K.; Graf, R.; Barkun, J.; Puhan, M.A.; Clavien, P.-A. The comprehensive complication index: A novel continuous scale to measure surgical morbidity. Ann. Surg. 2013, 258, 1–7. [Google Scholar] [CrossRef] [PubMed]
- Rashid, R.; Sohrabi, C.; Kerwan, A.; Franchi, T.; Mathew, G.; Nicola, M.; Agha, R.A. The STROCSS 2024 guideline: Strengthening the reporting of cohort, cross-sectional, and case-control studies in surgery. Int. J. Surg. 2024, 110, 3151–3165. [Google Scholar] [CrossRef] [PubMed]
- Donatini, G.; Caiazzo, R.; Do Cao, C.; Aubert, S.; Zerrweck, C.; El-Kathib, Z.; Gauthier, T.; Leteurtre, E.; Wemeau, J.-L.; Vantyghem, M.C.; et al. Long-term survival after adrenalectomy for stage I/II adrenocortical carcinoma (ACC): A retrospective comparative cohort study of laparoscopic versus open approach. Ann. Surg. Oncol. 2014, 21, 284–291. [Google Scholar] [CrossRef]
- Cicek, M.C.; Gunseren, K.O.; Senol, K.; Vuruskan, H.; Yavascaoglu, I. Is 6 cm Diameter an Upper Limit for Adrenal Tumors to Perform Laparoscopic Adrenalectomy? J. Laparoendosc. Adv. Surg. Tech. 2021, 31, 301–305. [Google Scholar] [CrossRef] [PubMed]
- Agrusa, A.; Romano, G.; Frazzetta, G.; Chianetta, D.; Sorce, V.; Di Buono, G.; Gulotta, G. Laparoscopic adrenalectomy for large adrenal masses: Single team experience. Int. J. Surg. 2014, 12 (Suppl. S1), S72–S74. [Google Scholar] [CrossRef] [PubMed]
- Feo, C.V.; Portinari, M.; Maestroni, U.; Del Rio, P.; Severi, S.; Viani, L.; Pravisani, R.; Soliani, G.; Zatelli, M.C.; Ambrosio, M.R.; et al. Applicability of laparoscopic approach to the resection of large adrenal tumours: A retrospective cohort study on 200 patients. Surg. Endosc. 2016, 30, 3532–3540. [Google Scholar] [CrossRef]
- Sharma, R.; Ganpule, A.; Veeramani, M.; Sabnis, R.B.; Desai, M. Laparoscopic management of adrenal lesions larger than 5 cm in diameter. Urol. J. 2009, 6, 254–259. [Google Scholar] [PubMed]
- Prakobpon, T.; Santi-Ngamkun, A.; Usawachintachit, M.; Ratchanon, S.; Sowanthip, D.; Panumatrassamee, K. Laparoscopic transperitoneal adrenalectomy in the large adrenal tumor from single center experience. BMC Surg. 2021, 21, 68. [Google Scholar] [CrossRef] [PubMed]
- Chen, Y.; Scholten, A.; Chomsky-Higgins, K.; Nwaogu, I.; Gosnell, J.E.; Seib, C.; Shen, W.T.; Suh, I.; Duh, Q.-Y. Risk Factors Associated With Perioperative Complications and Prolonged Length of Stay After Laparoscopic Adrenalectomy. JAMA Surg. 2018, 153, 1036–1041. [Google Scholar] [CrossRef] [PubMed]
- Mihai, I.; Boicean, A.; Teodoru, C.A.; Grigore, N.; Iancu, G.M.; Dura, H.; Bratu, D.G.; Roman, M.D.; Mohor, C.I.; Todor, S.B.; et al. Laparoscopic Adrenalectomy: Tailoring Approaches for the Optimal Resection of Adrenal Tumors. Diagnostics 2023, 13, 3351. [Google Scholar] [CrossRef] [PubMed]
- Tiberio, G.A.M.; Solaini, L.; Arru, L.; Merigo, G.; Baiocchi, G.L.; Giulini, S.M. Factors influencing outcomes in laparoscopic adrenal surgery. Langenbecks Arch. Surg. 2013, 398, 735–743. [Google Scholar] [CrossRef] [PubMed]
- Parnaby, C.N.; Chong, P.S.; Chisholm, L.; Farrow, J.; Connell, J.M.; O’ Dwyer, P.J. The role of laparoscopic adrenalectomy for adrenal tumours of 6 cm or greater. Surg. Endosc. 2008, 22, 617–621. [Google Scholar] [CrossRef] [PubMed]
- NIH state-of-the-science statement on management of the clinically inapparent adrenal mass (“incidentaloma”). NIH Consens. State Sci. Statements 2002, 19, 1–25.
- Mihai, I.; Dura, H.; Teodoru, C.A.; Todor, S.B.; Ichim, C.; Grigore, N.; Mohor, C.I.; Mihetiu, A.; Oprinca, G.; Bacalbasa, N.; et al. Intraoperative Ultrasound: Bridging the Gap between Laparoscopy and Surgical Precision during 3D Laparoscopic Partial Nephrectomies. Diagnostics 2024, 14, 942. [Google Scholar] [CrossRef] [PubMed]
- Mihai, I.; Boicean, A.; Dura, H.; Teodoru, C.A.; Bratu, D.G.; Ichim, C.; Todor, S.B.; Bacalbasa, N.; Bereanu, A.S.; Hașegan, A. Intraoperative Ultrasound Guidance in Laparoscopic Adrenalectomy: A Retrospective Analysis of Perioperative Outcomes. Diagnostics 2025, 15, 898. [Google Scholar] [CrossRef] [PubMed]
- Gan, L.; Meng, C.; Li, K.; Lei, P.; Li, J.; Wu, J.; Li, Y. Safety and effectiveness of minimally invasive adrenalectomy versus open adrenalectomy in patients with large adrenal tumors (≥5 cm): A meta-analysis and systematic review. Int. J. Surg. 2022, 104, 106779. [Google Scholar] [CrossRef] [PubMed]
- Cooper, A.B.; Habra, M.A.; Grubbs, E.G.; Bednarski, B.K.; Ying, A.K.; Perrier, N.D.; Lee, J.E.; Aloia, T.A. Does laparoscopic adrenalectomy jeopardize oncologic outcomes for patients with adrenocortical carcinoma? Surg. Endosc. 2013, 27, 4026–4032. [Google Scholar] [CrossRef] [PubMed]
- Machado, N.O.; Al Qadhi, H.; Al Wahaibi, K.; Rizvi, S.G. Laparoscopic Adrenalectomy for Large Adrenocortical Carcinoma. JSLS 2015, 19, e2015.00036. [Google Scholar] [CrossRef] [PubMed]
- Brix, D.; Allolio, B.; Fenske, W.; Agha, A.; Dralle, H.; Jurowich, C.; Langer, P.; Mussack, T.; Nies, C.; Riedmiller, H.; et al. Laparoscopic versus open adrenalectomy for adrenocortical carcinoma: Surgical and oncologic outcome in 152 patients. Eur. Urol. 2010, 58, 609–615. [Google Scholar] [CrossRef] [PubMed]
- Lombardi, C.P.; Raffaelli, M.; De Crea, C.; Boniardi, M.; De Toma, G.; Marzano, L.A.; Miccoli, P.; Minni, F.; Morino, M.; Pelizzo, M.R.; et al. Open versus endoscopic adrenalectomy in the treatment of localized (stage I/II) adrenocortical carcinoma: Results of a multiinstitutional Italian survey. Surgery 2012, 152, 1158–1164. [Google Scholar] [CrossRef] [PubMed]

| Parameter | Group A (<6 cm) N = 197 (73.2%) | Group B (≥6 cm) N = 72 (26.8%) | p Value |
|---|---|---|---|
| Age, mean ± SD (years) | 52 ± 13.6 | 55.5 ± 13.5 | 0.058 |
| BMI, mean ± SD (kg/m2) | 27.6 ± 6.8 | 27.9 ± 6.7 | 0.795 |
| Female, n. (%) | 75 (38.1) | 38 (54.2) | 0.018 |
| Male, n. (%) | 123 (61.9) | 41 (45.8) | |
| Comorbidity, n. (%) | 180 (91.4) | 67 (93.1) | 0.655 |
| Charlson comorbidity index, mean ± SD | 1.9 ± 1.8 | 2.4 ± 2.0 | 0.049 |
| ASA score, n. (%) | <0.001 | ||
| 1 | 1 (0.5) | 5 (6.9) | |
| 2 | 113 (56.3) | 26 (34.7) | |
| 3 | 82 (42.1) | 48 (58.3) | |
| 4 | 2 (1) | 0 (0) | |
| Prior abdominal surgery, n. (%) | 93 (47.2) | 28 (38.9) | 0.224 |
| Hormonal hypersecretion, n (%) | 131 (66.5) | 30 (41.7) | <0.001 |
| Catecholamine, n (%) | 51 (25.9) | 19 (26.4) | |
| Aldosterone, n (%) | 38 (19.3) | 2 (2.8) | |
| Cortisol, n (%) | 41 (20.8) | 9 (12.5) | |
| Cortisol + Aldosterone, n (%) | 1 (0.5) | 0 | |
| Catecholamine + Androgen, n (%) | 0 | 1 (1.4) | |
| Surgical approach | <0.001 | ||
| Laparoscopic LTA, n. (%) | 149 (75.6) | 69 (95.8) | |
| PRA, n. (%) | 43 (21.8) | 1 (1.4) | |
| Robotic LTA, n. (%) | 5 (2.5) | 2 (2.8) | |
| Tumor location: | 0.055 | ||
| Right, n. (%) | 95 (48.2) | 45 (62.5) | |
| Left, n. (%) | 95 (48.2) | 23 (31.9) | |
| Bilateral, n. (%) | 7 (3.6) | 4 (5.6) | |
| Genetic mutation, n. (%) | 12 (6.1) | 7 (9.7) | 0.303 |
| 21-OHD, n. (%) | 0 (0) | 1 (1.4) | |
| MEN2A, n. (%) | 5 (2.5) | 4 (5.6) | |
| MEN2B, n. (%) | 2 (1) | 0 (0) | |
| NF1, n. (%) | 3 (1.5) | 1 (1.4) | |
| VHL, n. (%) | 2 (1) | 0 (0) | |
| Maffucci syndrome, n. (%) | 0 (0) | 1 (1.4) | |
| Tumor size (major lesion), mean ± SD (cm) | 3.6 ± 1.3 | 7.6 ± 1.8 | <0.001 |
| Histology | <0.001 | ||
| Cortical adenoma or cyst, n. (%) | 131 (66.5) | 28 (38.9) | |
| With AMH, n (%) | 6 (4.6) | 2 (2.8) | |
| Pheochromocytoma, n. (%) | 45 (22.8) | 17 (23.6) | |
| Adrenal malignancies, n. (%) | 10 (5.1) | 9 (12.5) | |
| ACC, n.(%) | 4 (2) | 2 (2.8) | |
| Angiosarcoma, n. (%) | 0 | 1 (1.4) | |
| Adrenal metastasis, n. (%) | 6 (3) | 6 (8.3) | |
| Myelolipoma, n. (%) | 1 (0.5) | 14 (19.4) | |
| Others, n. (%) | 10 (5.1) | 4 (5.6) | |
| Lymphoma, n. (%) | 0 | 2 (2.8) | |
| Ganglioneuroma, n. (%) | 3 (1.5) | 2 (2.8) | |
| Angiomyolipoma, n. (%) | 1 (0.5) | 0 | |
| Hemangioma, n. (%) | 1 (0.5) | 0 | |
| Lymphangioma, n. (%) | 3 (1.5) | 0 | |
| Fibrous solitary tumor, n. (%) | 2 (1) | 0 |
| Parameter | Group A (<6 cm) N = 197 (73.2%) | Group B (≥6 cm) N = 72 (28.8%) | p Value |
|---|---|---|---|
| Operative time, mean ± SD (min) | 97.8 ± 50.5 | 120 ± 56.2 | 0.002 |
| Associated surgeries, n. (%) | 23 (11.7) | 7 (9.7) | 0.652 |
| Conversion to open, n. (%) | 5 (2.5) | 6 (8.3) | 0.075 |
| Reason for conversion | 0.143 | ||
| Technical difficulties, n. (%) | 1 (0.5) | 4 (5.6) | |
| Hemodynamic instability, n. (%) | 0 (0) | 2 (2.8) | |
| Others, n. (%) | 4 (2) | 0 (0) | |
| Intraoperative complications | 2 (1%) | 2 (2.8%) | 0.646 |
| No complications, n. (%) | 195 (99.0) | 70 (97.2) | |
| Hemorrhage, n. (%) | 0 (0) | 1 (1.4) | |
| Iatrogenic damage, n. (%) | 1 (0.5) | 0 (0) | |
| Others, n. (%) | 1 (0.5) | 1 (1.4) | |
| Blood transfusions, n. (%) | 2 (1.0) | 3 (4.2) | 0.236 |
| Postoperative ICU, n. (%) | 106 (53.8) | 42 (58.3) | 0.508 |
| Length of ICU stay, mean ± SD (days) | 1 ± 0.2 | 1.1 ± 0.4 | 0.406 |
| Length of hospital stay, mean ± SD (days) | 3.1 ± 1.7 | 3.5 ± 2.3 | 0.112 |
| Postoperative complications, n. (%) | 19 (9.6) | 8 (11.1) | 0.723 |
| Clavien–Dindo classification | 0.975 | ||
| Grade 1, n. (%) | 6 (3) | 2 (2.8) | |
| Grade 2, n. (%) | 10 (5.1) | 6 (8.3) | |
| Grade 3a, n. (%) | 1 (0.5) | 0 | |
| Grade 4a, n. (%) | 2 (1) | 0 | |
| Comprehensive Complications Index, mean ± SD | 2.0 ± 6.7 | 2.1 ± 6.1 | 0.857 |
| Readmission at 30 days, n. (%) | 4 (2) | 1 (1.4) | 0.730 |
| Adrenal-related mortality, n (%) | 0 | 0 | NA |
| Parameter | Coefficient | p-Value | Odds Ratio | 95% CI | |
|---|---|---|---|---|---|
| Inferior | Superior | ||||
| Tumor size ≥ 6 cm | 0.149 | 0.768 | 1.161 | 0.432 | 3.117 |
| Age | −0.027 | 0.197 | 0.973 | 0.934 | 1.014 |
| Gender | 0.091 | 0.838 | 0.745 | 0.455 | 2.637 |
| ASA score | 0.525 | 0.240 | 1.691 | 0.704 | 4.063 |
| Charlson comorbidity index | 0.282 | 0.056 | 1.326 | 0.993 | 1.771 |
| Hormonal hypersecretion | 0.378 | 0.426 | 1.459 | 0.575 | 3.701 |
| Tumor location (unilateral or bilateral) | −0.223 | 0.851 | 0.800 | 0.078 | 8.162 |
| Surgical approach | −0.064 | 0.841 | 0.938 | 0.503 | 1.749 |
| Histology | 0.091 | 0.658 | 1.096 | 0.731 | 1.642 |
| Parameter | Coefficient | p-Value | Odds Ratio | 95% CI | |
|---|---|---|---|---|---|
| Inferior | Superior | ||||
| Tumor size ≥ 6 cm | 1.758 | 0.031 | 5.800 | 1.177 | 28.595 |
| Age | 0.008 | 0.842 | 1.008 | 0.928 | 1.096 |
| Gender | 0.855 | 0.266 | 2.351 | 0.522 | 10.587 |
| ASA score | 1.662 | 0.057 | 5.271 | 0.950 | 29.253 |
| Charlson comorbidity index | 0.022 | 0.930 | 1.023 | 0.620 | 1.688 |
| Hormonal hypersecretion | −0.388 | 0.632 | 0.678 | 0.138 | 3.327 |
| Tumor location (unilateral or bilateral) | 0.853 | 0.526 | 2.346 | 0.168 | 32.808 |
| Surgical approach | 0.184 | 0.772 | 1.202 | 0.347 | 4.157 |
| Histology | 0.029 | 0.927 | 1.030 | 0.548 | 1.935 |
| Parameter | Coefficient | p-Value | 95% CI | |
|---|---|---|---|---|
| Inferior | Superior | |||
| Tumor size ≥ 6 cm | 0.248 | 0.344 | −0.268 | 0.764 |
| Age | −0.011 | 0.332 | −0.034 | 0.011 |
| Gender | 0.203 | 0.378 | −0.251 | 0.657 |
| ASA score | 0.416 | 0.062 | −0.021 | 0.853 |
| Charlson comorbidity index | 0.211 | 0.015 | 0.041 | 0.381 |
| Hormonal hypersecretion | −0.276 | 0.239 | −0.737 | 0.185 |
| Tumor location (unilateral or bilateral) | 3.231 | <0.001 | 2.037 | 4.424 |
| Surgical approach | −0.193 | 0.207 | −0.494 | 0.108 |
| Histology | 0.051 | 0.630 | −0.157 | 0.259 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Rossi, L.; Becucci, C.; Della Posta, O.; Papini, P.; Palma, F.; Cammarata, M.; Sacco, L.; Dekova, K.; Ajdini, S.; Ambrosini, C.E.; et al. The Role of Minimally Invasive Adrenalectomy for Large Adrenal Tumors (≥6 cm): Evidence from a 10-Year Retrospective Study. J. Clin. Med. 2025, 14, 5176. https://doi.org/10.3390/jcm14155176
Rossi L, Becucci C, Della Posta O, Papini P, Palma F, Cammarata M, Sacco L, Dekova K, Ajdini S, Ambrosini CE, et al. The Role of Minimally Invasive Adrenalectomy for Large Adrenal Tumors (≥6 cm): Evidence from a 10-Year Retrospective Study. Journal of Clinical Medicine. 2025; 14(15):5176. https://doi.org/10.3390/jcm14155176
Chicago/Turabian StyleRossi, Leonardo, Chiara Becucci, Ortensia Della Posta, Piermarco Papini, Francesca Palma, Mattia Cammarata, Luisa Sacco, Klaudiya Dekova, Suela Ajdini, Carlo Enrico Ambrosini, and et al. 2025. "The Role of Minimally Invasive Adrenalectomy for Large Adrenal Tumors (≥6 cm): Evidence from a 10-Year Retrospective Study" Journal of Clinical Medicine 14, no. 15: 5176. https://doi.org/10.3390/jcm14155176
APA StyleRossi, L., Becucci, C., Della Posta, O., Papini, P., Palma, F., Cammarata, M., Sacco, L., Dekova, K., Ajdini, S., Ambrosini, C. E., & Materazzi, G. (2025). The Role of Minimally Invasive Adrenalectomy for Large Adrenal Tumors (≥6 cm): Evidence from a 10-Year Retrospective Study. Journal of Clinical Medicine, 14(15), 5176. https://doi.org/10.3390/jcm14155176






