Effects of Resistance Training on Pain, Muscle Strength, and Function in Patients Undergoing Total Knee Arthroplasty: A Systematic Review and Meta-Analysis
Abstract
1. Introduction
2. Materials and Methods
2.1. Eligibility Criteria and Exclusion Criteria
2.2. Search Strategy
2.3. Data Collection
2.4. Assessment of Risk of Bias and Certainty of Evidence
2.5. Statistical Analysis
3. Results
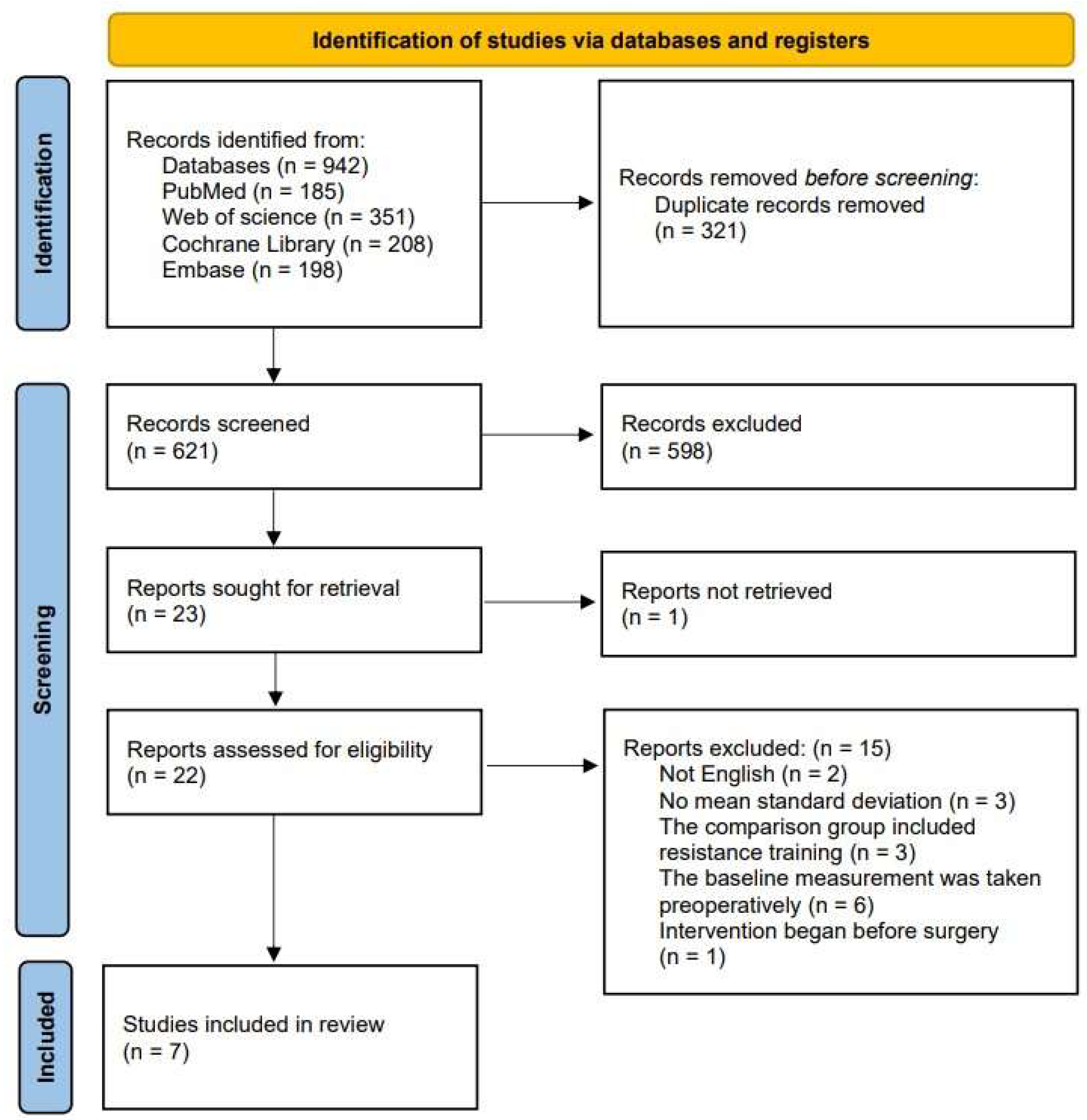
3.1. Research Selection Process
3.2. General Characteristics of Included Studies
3.3. Risk of Bias in Studies
3.4. Meta-Analysis Results
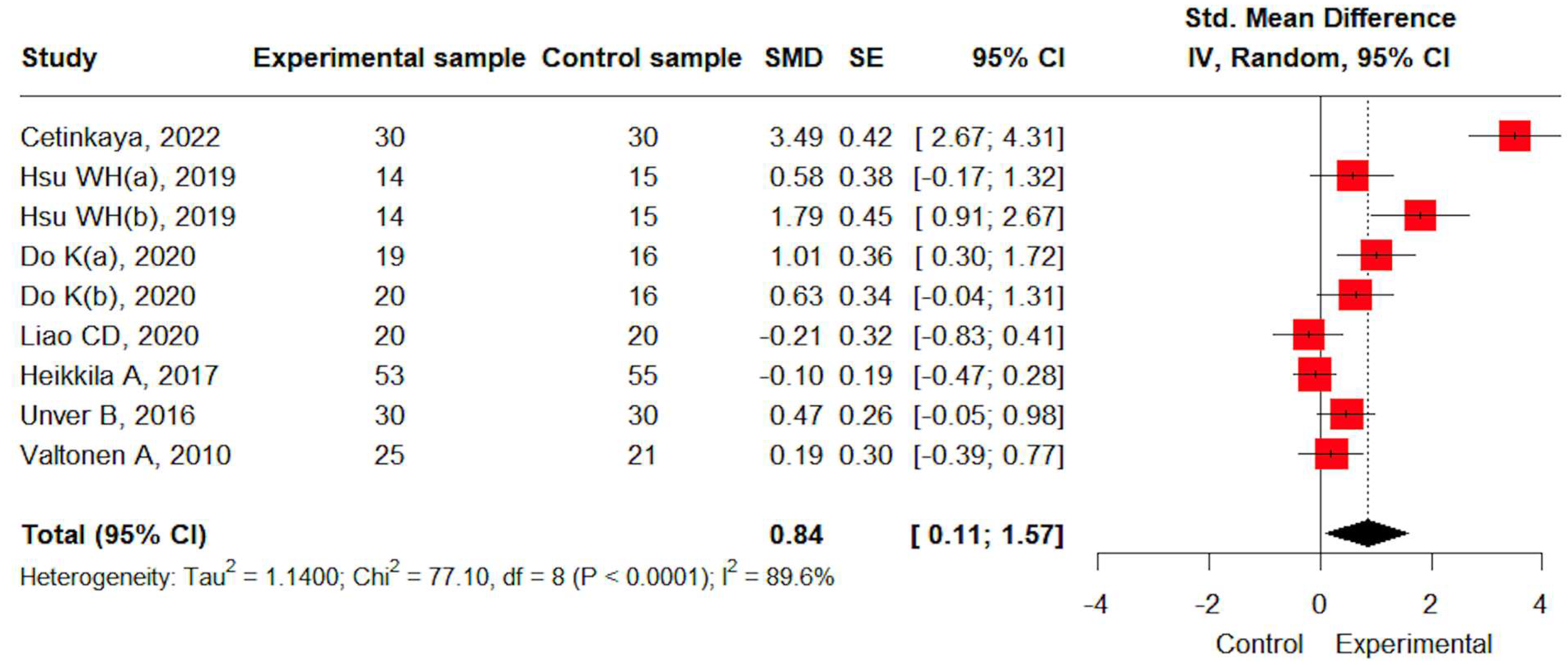
3.4.1. Pain
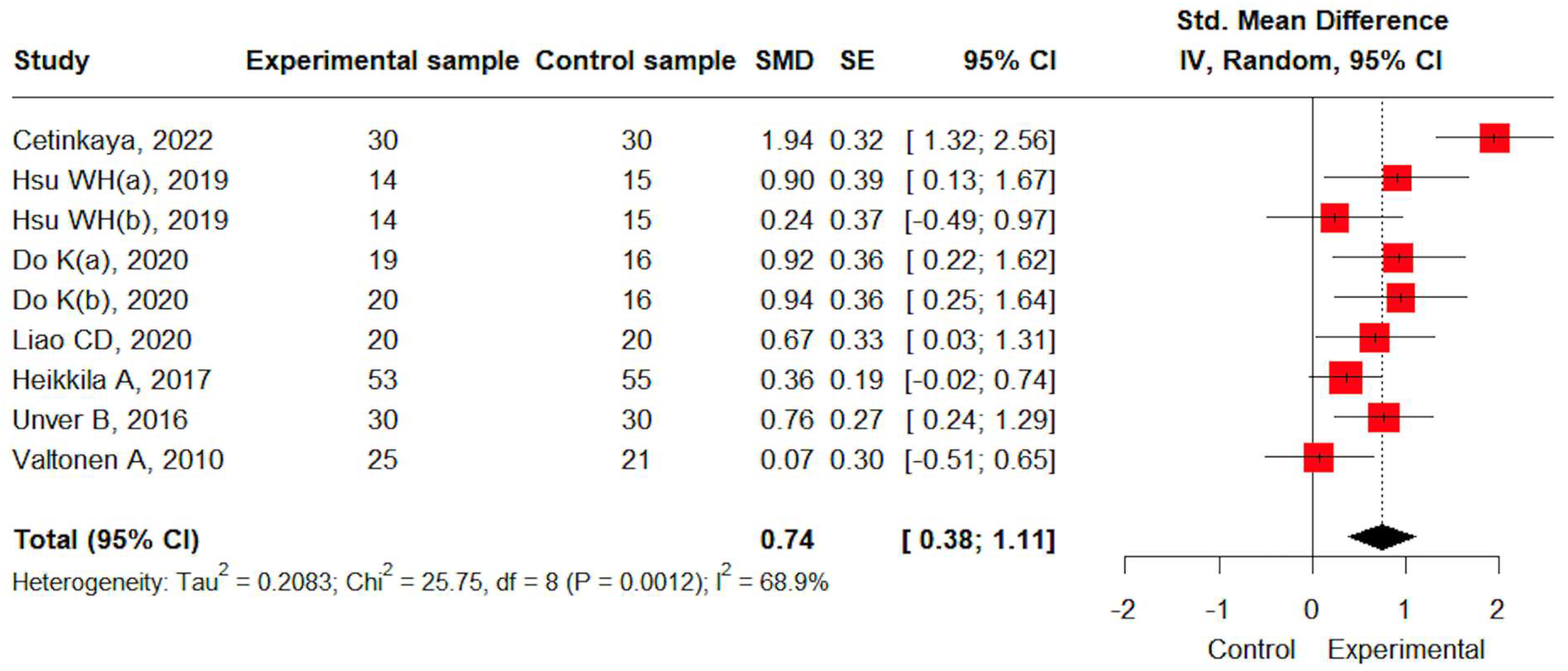
3.4.2. Muscle Strength
3.4.3. Self-Reported Function
3.4.4. Performance-Based Function
3.5. Subgroup Analysis
3.6. Sensitivity Analysis
3.7. Certainty of Evidence
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| OA | Osteoarthritis |
| TKA | Total Knee Arthroplasty |
| RCTs | Randomized Clinical Trials |
| BMI | Body Mass Index |
| WOMAC | Western Ontario and MacMaster Universities Osteoarthritis Index |
| KOOS | Knee Injury and Osteoarthritis Outcome Score |
| VAS | Visual Analogue Scale |
| ADL | Activities of Daily Living |
| HSS | Hospital for Special Surgery |
| ROB 2 | Risk of Bias 2 |
| SMD | Standardized Mean Difference |
| CIs | Confidence Intervals |
| 1RM | One Repetition Maximum |
References
- Neuprez, A.; Neuprez, A.H.; Kurth, W.; Gillet, P.; Bruyère, O.; Reginster, J.Y. Profile of osteoarthritic patients undergoing hip or knee arthroplasty, a step toward a definition of the “need for surgery”. Aging Clin. Exp. Res. 2018, 30, 315–321. [Google Scholar] [CrossRef] [PubMed]
- Hamilton, D.F.; Beard, D.J.; Barker, K.L.; Macfarlane, G.J.; Tuck, C.E.; Stoddart, A.; Wilton, T.; Hutchinson, J.D.; Murray, G.D.; Simpson, A.H.R.W.; et al. Targeting rehabilitation to improve outcomes after total knee arthroplasty in patients at risk of poor outcomes: Randomised controlled trial. BMJ 2020, 371, m3576. [Google Scholar] [CrossRef]
- Ho, D.M.; Huo, M.H. Are critical pathways and implant standardization programs effective in reducing costs in total knee replacement operations? J. Am. Coll. Surg. 2007, 205, 97–100. [Google Scholar] [CrossRef] [PubMed]
- Healy, W.L.; Della Valle, C.J.; Iorio, R.; Berend, K.R.; Cushner, F.D.; Dalury, D.F.; Lonner, J.H. Complications of total knee arthroplasty: Standardized list and definitions of the Knee Society. Clin. Orthop. Relat. Res. 2013, 471, 215–220. [Google Scholar] [CrossRef]
- Paravlic, A.H.; Meulenberg, C.J.; Drole, K. The Time Course of Quadriceps Strength Recovery After Total Knee Arthroplasty Is Influenced by Body Mass Index, Sex, and Age of Patients: Systematic Review and Meta-Analysis. Front. Med. 2022, 9, 865412. [Google Scholar] [CrossRef] [PubMed]
- Furu, M.; Ito, H.; Nishikawa, T.; Nankaku, M.; Kuriyama, S.; Ishikawa, M.; Nakamura, S.; Azukizawa, M.; Hamamoto, Y.; Matsuda, S. Quadriceps strength affects patient satisfaction after total knee arthroplasty. J. Orthop. Sci. 2016, 21, 38–43. [Google Scholar] [CrossRef]
- Mizner, R.L.; Petterson, S.C.; Snyder-Mackler, L. Quadriceps strength and the time course of functional recovery after total knee arthroplasty. J. Orthop. Sports Phys. Ther. 2005, 35, 424–436. [Google Scholar] [CrossRef]
- Currier, B.S.; Mcleod, J.C.; Banfield, L.; Beyene, J.; Welton, N.J.; D’Souza, A.C.; Keogh, J.A.J.; Lin, L.; Coletta, G.; Yang, A.; et al. Resistance training prescription for muscle strength and hypertrophy in healthy adults: A systematic review and Bayesian network meta-analysis. Br. J. Sports Med. 2023, 57, 1211–1220. [Google Scholar] [CrossRef]
- Lim, J.H.; Choi, A.Y.; Kim, B.G. The Effects of Resistance Training on Pain, Strength, and Function in Osteoarthritis: Systematic Review and Meta-Analysis. J. Pers. Med. 2024, 14, 1130. [Google Scholar] [CrossRef]
- Jette, D.U.; Hunter, S.J.; Burkett, L.; Langham, B.; Logerstedt, D.S.; Piuzzi, N.S.; Poirier, N.M.; Radach, L.J.L.; Ritter, J.E.; Scalzitti, D.A.; et al. Physical Therapist Management of Total Knee Arthroplasty. Phys. Ther. 2020, 100, 1603–1631. [Google Scholar] [CrossRef]
- Wei, G.; Shang, Z.; Li, Y.; Wu, Y.; Zhang, L. Effects of lower-limb active resistance exercise on mobility, physical function, knee strength and pain intensity in patients with total knee arthroplasty: A systematic review and meta-analysis. BMC Musculoskelet. Disord. 2024, 25, 730. [Google Scholar] [CrossRef] [PubMed]
- Wang, J.; Zhu, R.; Xu, X.T.; Liu, S.; Li, Z.; Guo, C.; Tao, X.; Qian, L.; Charles, R.; Fang, L. Effects of strength training on functional ambulation following knee replacement: A systematic review, meta-analysis, and meta-regression. Sci. Rep. 2023, 13, 10728. [Google Scholar] [CrossRef]
- Chen, X.; Li, X.; Zhu, Z.; Wang, H.; Yu, Z.; Bai, X. Effects of progressive resistance training for early postoperative fast-track total hip or knee arthroplasty: A systematic review and meta-analysis. Asian J. Surg. 2021, 44, 1245–1253. [Google Scholar] [CrossRef]
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. BMJ 2021, 372, n71. [Google Scholar] [CrossRef]
- Chandler, J.; Cumpston, M.; Li, T.; Page, M.J.; Welch, V.J.H.W. Cochrane Handbook for Systematic Reviews of Interventions; Wiley: Hoboken, NJ, USA, 2019. [Google Scholar]
- Guyatt, G.; Oxman, A.D.; Akl, E.A.; Kunz, R.; Vist, G.; Brozek, J.; Norris, S.; Falck-Ytter, Y.; Glasziou, P.; DeBeer, H.; et al. GRADE guidelines: 1. Introduction-GRADE evidence profiles and summary of findings tables. J. Clin. Epidemiol. 2011, 64, 383–394. [Google Scholar] [CrossRef] [PubMed]
- Cohen, J. Statistical Power Analysis for the Behavioral Sciences, 2nd ed.; Routledge: New York, NY, USA, 1988. [Google Scholar]
- Higgins, J.P.; Thompson, S.G.; Deeks, J.J.; Altman, D.G. Measuring inconsistency in meta-analyses. BMJ 2003, 327, 557–560. [Google Scholar] [CrossRef]
- Çetinkaya, F.; Karakoyun, A. The effects of elastic band exercise on the pain, kinesiophobia, functional, and psychological status after total knee arthroplasty: A randomized controlled trial. Clin. Rheumatol. 2022, 41, 3179–3188. [Google Scholar] [CrossRef] [PubMed]
- Hsu, W.H.; Hsu, W.B.; Shen, W.J.; Lin, Z.R.; Chang, S.H.; Hsu, R.W. Twenty-four-week hospital-based progressive resistance training on functional recovery in female patients post total knee arthroplasty. Knee 2019, 26, 729–736. [Google Scholar] [CrossRef]
- Do, K.; Yim, J. Effects of Muscle Strengthening around the Hip on Pain, Physical Function, and Gait in Elderly Patients with Total Knee Arthroplasty: A Randomized Controlled Trial. Healthcare 2020, 8, 489. [Google Scholar] [CrossRef]
- Liao, C.D.; Chiu, Y.S.; Ku, J.W.; Huang, S.W.; Liou, T.H. Effects of Elastic Resistance Exercise on Postoperative Outcomes Linked to the ICF Core Sets for Osteoarthritis after Total Knee Replacement in Overweight and Obese Older Women with Sarcopenia Risk: A Randomized Controlled Trial. J. Clin. Med. 2020, 9, 2194. [Google Scholar] [CrossRef]
- Heikkilä, A.; Sevander-Kreus, N.; Häkkinen, A.; Vuorenmaa, M.; Salo, P.; Konsta, P.; Ylinen, J. Effect of total knee replacement surgery and postoperative 12 month home exercise program on gait parameters. Gait. Posture 2017, 53, 92–97. [Google Scholar] [CrossRef] [PubMed]
- Unver, B.; Bakirhan, S.; Karatosun, V. Does a weight-training exercise programme given to patients four or more years after total knee arthroplasty improve mobility: A randomized controlled trial. Arch. Gerontol. Geriatr. 2016, 64, 45–50. [Google Scholar] [CrossRef]
- Valtonen, A.; Pöyhönen, T.; Sipilä, S.; Heinonen, A. Effects of aquatic resistance training on mobility limitation and lower-limb impairments after knee replacement. Arch. Phys. Med. Rehabil. 2010, 91, 833–839. [Google Scholar] [CrossRef]
- Hold, M. Strength and balance training before implantation of a total knee replacement. Z. Orthop. Unfallchir. 2024, 162, 12. [Google Scholar]
- Chen, H.; Du Shan-shan, F.L.J.; Jiang, J.; Liang, X.Y.; Zhen, P.; Li, X.S.; Liu, J. Effects of combination therapy on the movement function of lower extremity after total knee arthroplasty in the elderly. Chin. J. Tissue Eng. Res. 2017, 21, 4939. [Google Scholar]
- Vuorenmaa, M.; Ylinen, J.; Piitulainen, K.; Salo, P.; Kautiainen, H.; Pesola, M.; Häkkinen, A. Efficacy of a 12-month, monitored home exercise programme compared with normal care commencing 2 months after total knee arthroplasty: A randomized controlled trial. J. Rehabil. Med. 2014, 46, 166–172. [Google Scholar] [CrossRef] [PubMed]
- Trudelle-Jackson, E.; Hines, E.; Medley, A.; Thompson, M. Exploration of Habitual Walking Behavior and Home-Based Muscle Power Training in Individuals with Total Knee Arthroplasty. J. Phys. Act. Health 2020, 17, 331–338. [Google Scholar] [CrossRef]
- Husby, V.S.; Foss, O.A.; Husby, O.S.; Winther, S.B. Randomized controlled trial of maximal strength training vs. standard rehabilitation following total knee arthroplasty. Eur. J. Phys. Rehabil. Med. 2018, 54, 371–379. [Google Scholar] [CrossRef]
- Shabbir, M.; Umar, B.; Ehsan, S.; Munir, S.; Bunin, U.; Sarfraz, K. Comparison of functional training and strength training in improving knee extension lag after first four weeks of total knee replacement. Biomed. Res. 2017, 28, 5623–5627. [Google Scholar]
- Fung, V.; Ho, A.; Shaffer, J.; Chung, E.; Gomez, M. Use of Nintendo Wii Fit™ in the rehabilitation of outpatients following total knee replacement: A preliminary randomised controlled trial. Physiotherapy 2012, 98, 183–188. [Google Scholar] [CrossRef]
- Codine, P.H.; Dellemme, Y.; Denis-Laroque, F.; Herisson, C.H. The use of low velocity submaximal eccentric contractions of the hamstring for recovery of full extension after total knee replacement: A randomized controlled study. Isokinet. Exerc. Sci. 2004, 12, 215–218. [Google Scholar] [CrossRef]
- Tanaka, R.; Hayashizaki, T.; Taniguchi, R.; Kobayashi, J.; Umehara, T. Effect of an intensive functional rehabilitation program on the recovery of activities of daily living after total knee arthroplasty: A multicenter, randomized, controlled trial. J. Orthop. Sci. 2020, 25, 285–290. [Google Scholar] [CrossRef] [PubMed]
- Risso, A.M.; van der Linden, M.L.; Bailey, A.; Gallacher, P.; Gleeson, N. Exploratory insights into novel prehabilitative neuromuscular exercise-conditioning in total knee arthroplasty. BMC Musculoskelet. Disord. 2022, 23, 547. [Google Scholar] [CrossRef]
- Mau-Moeller, A.; Behrens, M.; Finze, S.; Bruhn, S.; Bader, R.; Mittelmeier, W. The effect of continuous passive motion and sling exercise training on clinical and functional outcomes following total knee arthroplasty: A randomized active-controlled clinical study. Health Qual. Life Outcomes 2014, 12, 68. [Google Scholar] [CrossRef]
- Li, Z.; Li, B.; Wang, G.; Wang, K.; Chen, J.; Liang, Y.; Tang, X.; Yang, Y. Impact of enhanced recovery nursing combined with limb training on knee joint function and neurological function after total knee arthroplasty in patients with knee osteoarthritis. Am. J. Transl. Res. 2021, 13, 6864–6872. [Google Scholar]
- Jakobsen, T.L.; Kehlet, H.; Husted, H.; Petersen, J.; Bandholm, T. Early progressive strength training to enhance recovery after fast-track total knee arthroplasty: A randomized controlled trial. Arthritis Care. Res. 2014, 66, 1856–1866. [Google Scholar] [CrossRef] [PubMed]
- Jacksteit, R.; Stöckel, T.; Behrens, M.; Feldhege, F.; Bergschmidt, P.; Bader, R.; Mittelmeier, W.; Skripitz, R.; Mau-Moeller, A. Low-Load Unilateral and Bilateral Resistance Training to Restore Lower Limb Function in the Early Rehabilitation After Total Knee Arthroplasty: A Randomized Active-Controlled Clinical Trial. Front. Med. 2021, 8, 628021. [Google Scholar] [CrossRef]
- Jiao, S.; Feng, Z.; Dai, T.; Huang, J.; Liu, R.; Meng, Q. High-Intensity Progressive Rehabilitation Versus Routine Rehabilitation After Total Knee Arthroplasty: A Randomized Controlled Trial. J. Arthroplast. 2024, 39, 665–671. [Google Scholar] [CrossRef]
- Hägg, G.M. Human muscle fibre abnormalities related to occupational load. Eur. J. Appl. Physiol. 2000, 83, 159–165. [Google Scholar] [CrossRef]
- Belavy, D.L.; Van Oosterwijck, J.; Clarkson, M.; Dhondt, E.; Mundell, N.L.; Miller, C.T.; Owen, P.J. Pain sensitivity is reduced by exercise training: Evidence from a systematic review and meta-analysis. Neurosci. Biobehav. Rev. 2021, 120, 100–108. [Google Scholar] [CrossRef]
- Coury, H.J.; Moreira, R.F.; Dias, N.B. Evaluation of the effectiveness of workplace exercise in controlling neck, shoulder and low back pain: A systematic review. Braz. J. Phys. Ther. 2009, 13, 461–479. [Google Scholar] [CrossRef]
- Monsegue, A.P.; Emans, P.; van Loon, L.J.C.; Verdijk, L.B. Resistance exercise training to improve post-operative rehabilitation in knee arthroplasty patients: A narrative review. Eur. J. Sport Sci. 2024, 24, 938–949. [Google Scholar] [CrossRef] [PubMed]
- Judd, D.L.; Eckhoff, D.G.; Stevens-Lapsley, J.E. Muscle strength loss in the lower limb after total knee arthroplasty. Am. J. Phys. Med. Rehabil. 2012, 91, 220–226. [Google Scholar] [CrossRef] [PubMed]
- Pua, Y.H.; Seah, F.J.T.; Clark, R.A.; Poon, C.L.L.; Tan, J.W.M.; Chong, H.C. Factors associated with gait speed recovery after total knee arthroplasty: A longitudinal study. Semin. Arthritis Rheum. 2017, 46, 544–551. [Google Scholar] [CrossRef]
- Wang, H.; Ma, B.; Wang, G.; Wang, P.; Long, H.; Niu, S.; Dong, C.; Zhang, H.; Zhao, Z.; Ma, Q.; et al. Dose-Response Relationships of Resistance Training in Adults with Knee Osteoarthritis: A Systematic Review and Meta-analysis. J. Geriatr. Phys. Ther. 2024, 47, 97–109. [Google Scholar] [CrossRef]
- Messier, S.P.; Mihalko, S.L.; Beavers, D.P.; Nicklas, B.J.; DeVita, P.; Carr, J.J.; Hunter, D.J.; Lyles, M.; Guermazi, A.; Bennell, K.L.; et al. Effect of High-Intensity Strength Training on Knee Pain and Knee Joint Compressive Forces Among Adults with Knee Osteoarthritis: The START Randomized Clinical Trial. JAMA 2021, 325, 646–657. [Google Scholar] [CrossRef]
- Silva, N.L.; Oliveira, R.B.; Fleck, S.J.; Leon, A.C.; Farinatti, P. Influence of strength training variables on strength gains in adults over 55 years-old: A meta-analysis of dose-response relationships. J. Sci. Med. Sport 2014, 17, 337–344. [Google Scholar] [CrossRef]
- Khalafi, M.; Kheradmand, S.; Habibi Maleki, A.; Symonds, M.E.; Rosenkranz, S.K.; Batrakoulis, A. The Effects of Concurrent Training Versus Aerobic or Resistance Training Alone on Body Composition in Middle-Aged and Older Adults: A Systematic Review and Meta-Analysis. Healthcare 2025, 13, 776. [Google Scholar] [CrossRef]
- Juhl, C.; Christensen, R.; Roos, E.M.; Zhang, W.; Lund, H. Impact of exercise type and dose on pain and disability in knee osteoarthritis: A systematic review and meta-regression analysis of randomized controlled trials. Arthritis. Rheumatol. 2014, 66, 622–636. [Google Scholar] [CrossRef]
- Leveritt, M.; Abernethy, P.J.; Barry, B.K.; Logan, P.A. Concurrent strength and endurance training. A review. Sports Med. 1999, 28, 413–427. [Google Scholar] [CrossRef]
- Wilson, J.M.; Marin, P.J.; Rhea, M.R.; Wilson, S.M.; Loenneke, J.P.; Anderson, J.C. Concurrent training: A meta-analysis examining interference of aerobic and resistance exercises. J. Strength Cond. Res. 2012, 26, 2293–2307. [Google Scholar] [CrossRef] [PubMed]
- Chang, C.B.; Yoo, J.H.; Koh, I.J.; Kang, Y.G.; Seong, S.C.; Kim, T.K. Key factors in determining surgical timing of total knee arthroplasty in osteoarthritic patients: Age, radiographic severity, and symptomatic severity. J. Orthop. Traumatol. 2010, 11, 21–27. [Google Scholar] [CrossRef] [PubMed]
| Outcome | Subgroup | Study | Effect Size (SMD [95% CI]) | I2 | Test for Subgroup Difference | |
|---|---|---|---|---|---|---|
| Pain | Comparison group | [19,20,21,22,24] | Other intervention | 1.08 [0.20; 1.97] | 89.8% | p = 0.023 |
| [23,25] | No intervention | −0.01 [−0.33; 0.31] | 0% | |||
| Intervention Duration | [19,21,24] | ~11 weeks | 1.38 [0.02; 2.74] | 92.6% | p = 0.199 | |
| [20,22,23,25] | 12 weeks~ | 0.39 [−0.26; 1.04] | 77.2% | |||
| Intervention type | [19,20,21,22,25] | Resistance only | 1.05 [0.14; 1.96] | 90.2% | p = 0.101 | |
| [23,24] | Multicomponent | 0.16 [−0.39; 0.71] | 66.8% | |||
| Muscle strength | Comparison group | [20,24] | Other intervention | 1.52 [0.59; 2.46] | 77.4% | p = 0.022 |
| [23,25] | No intervention | 0.32 [−0.10; 0.75] | 34.4% | |||
| Intervention Duration | [20,23,25] | ~11 weeks | 1.12 [0.14; 2.10] | 87.1% | p = 0.580 | |
| [24] | 12 weeks~ | 0.80 [0.28; 1.33] | - | |||
| Intervention type | [20,25] | Resistance only | 1.48 [0.43; 2.52] | 80.4% | p = 0.101 | |
| [23,24] | Multicomponent | 0.46 [−0.17; 1.08] | 73.5% | |||
| Self-reported function | Comparison group | [19,20,21,22,24] | Other intervention | 1.77 [0.15; 3.38] | 93.9% | p = 0.102 |
| [25] | No intervention | 0.33 [−0.25; 0.92] | - | |||
| Intervention Duration | [19,21,24] | ~11 weeks | 2.05 [−0.79; 4.90] | 96.3% | p = 0.542 | |
| [20,22,25] | 12 weeks~ | 1.10 [−0.02; 2.22] | 84.7% | |||
| Intervention type | [19,20,21,22,25] | Resistance only | 1.80 [0.22; 3.39] | 93.3% | p = 0.041 | |
| [24] | Multicomponent | 0.06 [−0.44; 0.57] | - | |||
| Performance-based function | Comparison group | [19,20,21,22,24] | Other intervention | 0.92 [0.53; 1.31] | 59.2% | p = 0.011 |
| [23,25] | No intervention | 0.27 [−0.05; 0.59] | 0% | |||
| Intervention Duration | [19,21,24] | ~11 weeks | 1.14 [0.60; 1.68] | 66.9% | p = 0.014 | |
| [20,22,23,25] | 12 weeks~ | 0.39 [0.14; 0.65] | 0% | |||
| Intervention type | [19,20,21,22,25] | Resistance only | 0.81 [0.34; 1.28] | 72.6% | p = 0.345 | |
| [23,24] | Multicomponent | 0.52 [0.13; 0.91] | 34.4% |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lim, J.; Kim, B. Effects of Resistance Training on Pain, Muscle Strength, and Function in Patients Undergoing Total Knee Arthroplasty: A Systematic Review and Meta-Analysis. J. Clin. Med. 2025, 14, 4979. https://doi.org/10.3390/jcm14144979
Lim J, Kim B. Effects of Resistance Training on Pain, Muscle Strength, and Function in Patients Undergoing Total Knee Arthroplasty: A Systematic Review and Meta-Analysis. Journal of Clinical Medicine. 2025; 14(14):4979. https://doi.org/10.3390/jcm14144979
Chicago/Turabian StyleLim, Jaehyun, and Byeonggeun Kim. 2025. "Effects of Resistance Training on Pain, Muscle Strength, and Function in Patients Undergoing Total Knee Arthroplasty: A Systematic Review and Meta-Analysis" Journal of Clinical Medicine 14, no. 14: 4979. https://doi.org/10.3390/jcm14144979
APA StyleLim, J., & Kim, B. (2025). Effects of Resistance Training on Pain, Muscle Strength, and Function in Patients Undergoing Total Knee Arthroplasty: A Systematic Review and Meta-Analysis. Journal of Clinical Medicine, 14(14), 4979. https://doi.org/10.3390/jcm14144979