Abstract
Background/Objective: The objective of this study is to compare the relative effectiveness of combination therapy (exercise plus manual therapy) versus single-modality physiotherapy interventions for improving pain and function in patients with rotator cuff-related shoulder pain (RCRSP), using a network meta-analysis (NMA) approach. Methods: We systematically searched five electronic databases from inception to October 2023 for randomized controlled trials (RCTs) evaluating non-invasive physiotherapy interventions in adults with RCRSP. Primary outcomes included pain intensity and shoulder function, assessed at 12 weeks. A frequentist NMA was conducted to estimate standardized mean differences (SMDs) with 95% confidence intervals (CIs). Risk of bias was assessed using the Cochrane RoB 2.0 tool. Results: Eleven RCTs (n = 548) were included. Combination therapy demonstrated the greatest improvement in function (SMD = −1.02; 95% CI: −2.59 to 0.56) and pain (SMD = −1.05; 95% CI: −2.41 to 0.30), although the wide confidence intervals crossing the null suggests statistical uncertainty. Exercise therapy alone showed moderate functional improvement (SMD = −0.41; 95% CI: −1.64 to 0.82), and Kinesio taping (KT) provided moderate pain relief (SMD = −0.53; 95% CI: −1.81 to 0.75). While these effects approached known minimal clinically important difference (MCID) thresholds (e.g., DASH: 10–15; VAS: 1.4–2.0), they did not reach statistical significance. Conclusions: Based on 11 RCTs, combination therapy (exercise plus manual therapy) appears to be the most effective non-invasive approach for improving pain and function in patients with RCRSP. However, the wide confidence intervals highlight uncertainty. Further large-scale and long-term trials are warranted to confirm its clinical utility and sustainability.
1. Introduction
Rotator cuff-related shoulder pain (RCRSP) is one of the most common musculoskeletal disorders worldwide, affecting 10% to 20% of adults, with prevalence rising to as high as 70% in individuals over the age of 50 [1,2]. The condition includes subacromial impingement syndrome (SIS), tendinopathy, and bursitis, typically leading to chronic pain, restricted shoulder mobility, and functional impairment, which in turn affect patients’ daily activities and work productivity [3,4]. Epidemiological studies show that approximately 70% of patients with shoulder pain are diagnosed with RCRSP, and 30% to 40% of these patients continue to experience persistent pain and functional impairment despite receiving treatment [5,6]. Due to its high recurrence rate and long-term impact, RCRSP places a significant burden on the healthcare system. It also leads to reduced workplace productivity and increased costs for businesses and insurance systems. As a result, identifying the most efficient and affordable non-invasive treatment strategies has become a critical need in both clinical practice and the healthcare systems [7,8].
Currently, physiotherapy is the primary non-invasive treatment for RCRSP. Common therapeutic approaches include exercise therapy [9,10], manual therapy [3,11,12], Kinesio taping (KT) [13,14], and combination therapy [6,15]. However, the effectiveness of different physiotherapy approaches remains a topic of debate. While exercise therapy is known to provide the best long-term outcomes, some studies suggest that manual therapy may be more effective in the short term [16,17,18]. In addition, KT may provide short-term pain relief in some patients, but its long-term efficacy remains unclear [2,19]. Whether combination therapy (e.g., exercise therapy plus manual therapy) was superior to single-modality treatment across all clinical outcomes is not supported by comprehensive comparative evidence. The lack of head-to-head comparisons among all available interventions poses challenges for clinicians when determining the most effective treatment option [6,20].
Traditional meta-analyses are limited to comparing two treatments at a time and are unable to simultaneously assess the relative effectiveness of multiple therapies. In contrast, network meta-analysis (NMA) offers a more robust and integrated approach by synthesizing both direct and indirect evidence across a range of treatments. This methodology allows for a comparative ranking of multiple physiotherapy interventions [21]—even in the absence of comprehensive pairwise trials—thereby facilitating more informed clinical decisions [22].
The aim of this study was to conduct a systematic review and network meta-analysis, following PRISMA-NMA guidelines, to compare the relative effectiveness of physiotherapy interventions on pain relief (measured via VAS, NPRS) and functional improvement (SPADI, DASH, Constant Score) in adults with RCRSP. Specifically, the study investigates whether combination therapy (exercise plus manual therapy) was more effective than single-treatment modalities over a follow-up period of at least 12 weeks [23]. The central hypothesis is that combination therapy yields superior functional and pain outcomes compared to either exercise or manual therapy alone. The findings aim to inform evidence-based clinical recommendations and guide optimal non-surgical management strategies to improve outcomes for patients and reduce the long-term burden of RCRSP.
2. Materials and Methods
2.1. Database Searches and Study Identification
This study was conducted following the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) extension guidelines for network meta-analysis (PRISMA NMA) [24]. No ethical committee approval or informed consent from participants was required. Two authors conducted electronic searches in PubMed, Embase, Cochrane Reviews, Cochrane CENTRAL, and ClinicalTrials.gov databases separately using the following keywords: (‘Rotator cuff related shoulder pain’ or ‘RCRSP’) AND (‘subacromial impingement syndrome’ or ‘SIS’) AND (‘shoulder impingement syndrome ‘ or ‘SIS’) AND (‘physical therapy‘ or ‘rehabilitation‘) AND (‘Pain’ OR ‘Vas’) AND (‘DASH ‘ OR ‘Disabilities of the Arm, Shoulder, and Hand‘). Searches for the systematic reviews and network meta-analyses spanned from database inception to 7 April 2025.
During the initial screening phase, two authors independently assessed the titles and abstracts of identified articles and resolved discrepancies through consensus. Eligible trials were identified through searches conducted in the databases listed above. In addition, the cited references within selected review papers [1,4,5,19,25,26] were assessed, and manual searches were conducted. A third author was consulted to resolve any unresolved disagreements. No limitations were placed on publication language during the searches.
2.2. Inclusion and Exclusion Criteria
The PICO model (population, intervention, comparison, outcome) guided the design of this network meta-analysis with the criteria as follows: (1) P: patients diagnosed with rotator cuff-related shoulder pain (RCRSP); (2) I: physiotherapy modalities (e.g., exercise therapy, manual therapy, modality therapy, combination therapy: exercise plus manual); (3) C: other physiotherapy modalities or standard treatment (e.g., placebo, control group); (4) O: primary outcomes: pain reduction (VAS, NPRS), secondary outcomes: functional improvement (SPADI, DASH, Constant Score).
The inclusion criteria primarily focused on the following aspects: To be included in this review, studies must meet the following criteria: (1) they must be randomized controlled trials (RCTs); (2) the study population must consist of adults diagnosed with RCRSP; (3) the study must include at least one physiotherapy intervention, compared to another physiotherapy intervention or standard treatment; (4) the study must provide quantifiable data, including pain and functional assessment outcomes; (5) the study must last for at least 12 weeks, including treatment and follow-up (Figure 1_PRISMA).
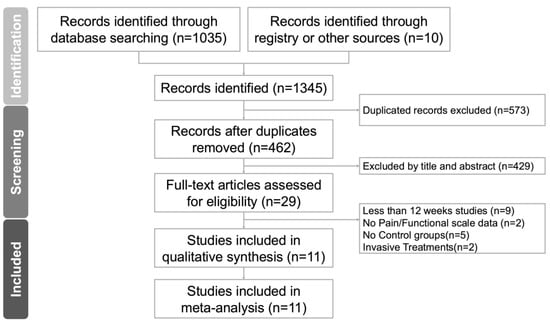
Figure 1.
The PRISMA flow diagram of the study selection process.
Choice of a 12-week evaluation period was informed by an initial review of the literature, which identified it as the most frequently reported follow-up duration among the included studies. Additionally, previous large-scale analyses have shown that the effects of exercise-based rehabilitation typically emerge around 12 weeks [26]. To enable consistent comparisons across interventions, a standardized assessment time point was necessary. Therefore, this study focuses on the 12-week timeframe and excludes durations with limited available data [23].
Interventions assessed were as follows: This study includes the following physiotherapy modalities: exercise therapy: shoulder stabilization training, strengthening exercises; manual therapy: joint mobilization, massage therapy; physical modalities: electrical stimulation (TENS, EMS), shock wave therapy, and KT; combination therapy: a combination of different physiotherapy modalities (e.g., exercise plus manual therapy) [27].
Population: The targeted population included individuals aged 18 to 75 years with RCRSP, excluding acute trauma, complete rotator cuff tears, and post-surgical patients.
Study design: The included studies needed to have quantitative measures and detailed reports on outcomes such as pain reduction and functional improvement.
The exclusion criteria for this study included the following:
Study duration: studies with a treatment or follow-up period of less than 12 weeks.
Outcome measures: studies that do not report pain or functional scale data (e.g., VAS, NPRS, DASH).
Control groups: studies without a control group or a comparison intervention.
Invasive treatments: studies involving surgical interventions, pharmacological injections (e.g., corticosteroid injections), or other invasive procedures.
These exclusion criteria were chosen to ensure the reliability and relevance of the study. A minimum duration of 12 weeks ensures sufficient time for the effects of physiotherapy to manifest. Studies lacking pain or functional scale data were excluded due to the absence of objective outcome measures for comparison. The absence of control groups also prevented valid comparisons between interventions. Lastly, invasive treatments (e.g., surgery, injections) were excluded to focus solely on the effectiveness of non-invasive physiotherapy.
2.3. Standardization for Comparison
Standardization ensures consistency across studies by normalizing pain (VAS/NPRS) and function (SPADI/DASH/Constant Score) scores to a 0–100 scale. Only 12-week outcome data will be used for comparison. Physiotherapy interventions will be classified into distinct categories (e.g., exercise, manual therapy, electrotherapy). Effect sizes will be reported as mean difference (MD) or standardized mean difference (SMD), with 95% confidence intervals (CIs). Comparisons will be made against placebo, standard care, or alternative therapies.
2.4. Modeling for Network Meta-Analysis
The transitivity assumption was considered plausible because the included studies were sufficiently similar in terms of key clinical and methodological features. All studies recruited adult participants diagnosed with rotator cuff-related shoulder pain (RCRSP), applied non-invasive physiotherapy interventions, and assessed outcomes using validated scales for pain (VAS or NPRS) and function (DASH or SPADI) within a standardized 12-week timeframe.
Potential effect modifiers—such as participant age, symptom chronicity, baseline shoulder function, and intervention intensity—were generally comparable across studies. There were no systematic differences in delivery setting (e.g., outpatient vs. inpatient care) or therapist qualifications that would violate the assumption of transitivity. The outcome measures were conceptually equivalent and commonly used interchangeably in musculoskeletal trials, thus permitting valid indirect comparisons. Collectively, these characteristics support the methodological integrity and clinical plausibility of transitivity within the NMA framework [21].
2.5. Methodological Quality Appraisal
The methodological quality of the included randomized trials was evaluated using the Cochrane Risk of Bias tool (Version 2, RoB 2, London, UK) [21]. This instrument assesses six key domains: the randomization process, deviations from intended interventions, missing outcome data, measurement of outcomes, selection of reported results, and overall risk of bias.
2.6. Primary Outcome: Functional Improvement (Standardized Mean Difference)
The primary outcome of this study is to compare the effectiveness of physiotherapy treatments in improving function in individuals with RCRSP. Functional outcomes are assessed using the Shoulder Pain and Disability Index (SPADI) and the Disabilities of the Arm, Shoulder, and Hand (DASH) Score. All scores are standardized to a 0–100 scale to ensure comparability across studies.
2.7. Secondary Outcomes: Pain Reduction (Standardized Mean Difference)
The secondary outcome is the effectiveness of physiotherapy treatments in reducing pain in individuals with RCRSP. Pain levels are assessed using the Visual Analog Scale (VAS) and the Numeric Pain Rating Scale (NPRS). The scores are standardized to a 0–10 scale for consistency and comparability across studies.
2.8. Data Extraction, Management, and Conversion
Two authors independently extracted data from the included studies, encompassing demographic characteristics, study design, assessment criteria, and both primary and secondary outcomes. When essential data were not available in the published reports, the corresponding authors were contacted to obtain the original information.
Data extraction, transformation, and synthesis were carried out in accordance with the guidelines provided in the Cochrane Handbook for Systematic Reviews of Interventions and other relevant medical literature [28,29,30,31,32].
For studies that did not report standard deviations (SDs) for continuous outcomes, SDs were imputed using established formulas based on available data such as confidence intervals, standard errors, or p-values. When such data were not available, we attempted to contact study authors. If the required information could not be retrieved or reliably estimated, the study was excluded from the quantitative synthesis to maintain analytical rigor and avoid introducing bias. Zero-event studies were not applicable in this review, as all included outcomes were continuous measures.
2.9. Statistical Analysis
Given the variety of physiotherapy interventions for RCRSP, a random-effects model was employed for the network meta-analysis [33]. The analysis was conducted using MetaInsight (Version 4.0.2, Complex Reviews Support Unit, National Institute for Health Research, London, UK) under a frequentist framework. MetaInsight is a web-based platform for network meta-analysis that utilizes the netmeta package in R for frequentist statistical calculations [22]
Forest and network plots were initially constructed to illustrate all pairwise comparisons across the included studies. Subsequently, forest plots were created to illustrate comparisons of standardized mean differences in evaluating the effectiveness of physiotherapy treatments for both functional improvement and pain reduction. Effect sizes were reported as point estimates with 95% CIs [34]. The effectiveness of physiotherapy treatments for functional improvement and pain reduction in RCRSP was ranked, and numerical results for both direct and indirect treatment comparisons are presented in the tables. Inconsistency was assessed to detect potential conflicts within the network. Statistical significance was defined as a two-tailed p-value of less than 0.05.
2.10. Sensitivity Analyses
A single-study deletion approach was employed to test result stability; each of the twelve studies was removed in turn. This sensitivity analysis confirmed that conclusions and rankings were not driven by any single study [32].
2.11. Publication Bias
Potential publication bias was assessed following the recommendations of the Cochrane Handbook for Systematic Reviews of Interventions [28]. A funnel plot was constructed using Comprehensive Meta-Analysis software (Version 4; Biostat, Englewood, NJ, USA), and Egger’s regression test was applied to assess asymmetry. These analyses were performed across all pairwise comparisons, using the most common comparator (e.g., control or exercise therapy) as the reference group. Visual inspection of the funnel plot revealed no major asymmetry, and Egger’s test did not indicate statistically significant publication bias.
3. Results
3.1. Study Identification and Network Model Formation
A PRISMA flowchart detailing the literature search is presented in Figure 1, and the PRISMA network meta-analysis extension checklist is provided in Table S1. From an initial pool of 29 articles, 11 RCTs (n = 548) met the inclusion criteria (Table 1) [3,11,12,13,14,15,16,35,36,37,38]. As summarized in Supplementary Table S3, the most frequent reasons for excluding 18 full-text articles [2,6,9,10,17,18,20,39,40,41,42,43,44,45,46,47,48,49] included a follow-up duration shorter than 12 weeks (n = 8), absence of a control group (n = 6), use of invasive interventions such as injections or surgery (n = 2), and missing key outcome data (n = 2). These criteria were applied consistently to ensure methodological comparability.

Table 1.
Summary of included trials evaluating physiotherapy interventions for RCRSP to improve shoulder function and reduce pain.
Among the included participants, 152 received exercise therapy alone, 66 received manual therapy alone, 78 received KT, 140 received combination therapy (e.g., exercise plus manual therapy, KT, or extracorporeal shock wave therapy (ESWT)), and 112 were assigned to control groups. These allocations are illustrated in the network plot (Figure 2), where node sizes reflect total sample size and edge thickness denotes the number of studies per direct comparison.
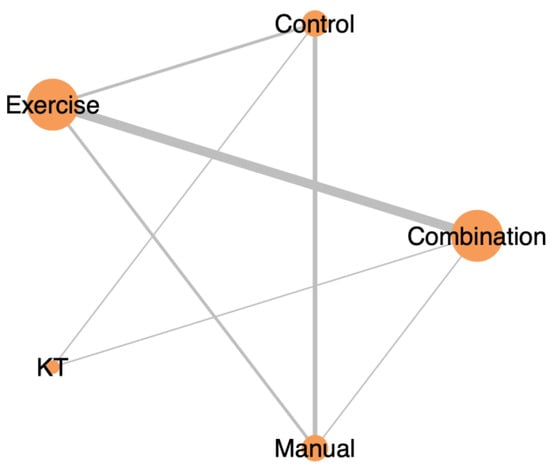
Figure 2.
Network plot illustrating the direct comparisons between physiotherapy interventions for RCRSP in terms of pain reduction after 12 weeks. Node size reflects the number of participants per treatment, and edge thickness indicates the number of studies informing each comparison.
3.2. Methodological Quality of the Included Studies
In assessing the overall methodological quality, we found that 55% (6/11) of the studies had a low risk of bias, while 45% (5/11) exhibited some degree of bias (Supplementary Figure S1). Studies with potential risk of bias often showed variations in protocols between study arms, which may have influenced adherence and outcomes. Detailed findings from the risk of bias assessment are presented in Supplementary Table S4.
3.3. Primary Outcome: Combination Therapy Most Effective for Functional Improvement
After a 12-week intervention, combination therapy showed significant functional improvement (effect size: −1.02; 95% CI: −2.59 to 0.56). In contrast, exercise therapy (effect size: −0.77; 95% CI: −2.25 to 0.71) and KT (effect size: −0.56; 95% CI: −2.47 to 1.34) produced modest effects. On the other hand, manual therapy (effect size: −0.47; 95% CI: −1.84 to 0.9) did not show a significant difference compared to the control group. Detailed pairwise comparisons between study arms are shown in Supplementary Figure S2 and summarized in Figure 3. Treatments were ranked based on their effect sizes for functional improvement, with combination therapy being the most effective, followed by exercise therapy, KT, and manual therapy. Please see Table 2 for a detailed comparison and ranking.
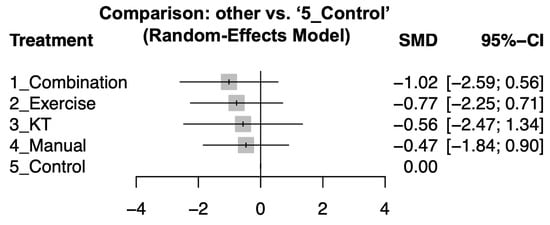
Figure 3.
Forest plot showing how different treatments affected shoulder function compared to control after 12-week intervention. Negative values mean better improvement.

Table 2.
Pairwise comparison and ranking of different therapy types of interventions for improvement of shoulder function at 12 weeks in rotator cuff-related shoulder pain.
3.4. Secondary Outcome: Combination Therapy Most Effective for Pain Reduction
After a 12-week intervention, combination therapy also showed significant pain reduction (effect size: −1.05; 95% CI: −2.41 to 0.3). KT (effect size: −0.87; 95% CI: −3.41 to 1.66) and exercise therapy (effect size: −0.52; 95% CI: −1.77 to 0.74) demonstrated marginal effects while manual therapy did not demonstrate a statistically significant improvement compared to the control groups. Detailed pairwise comparisons are illustrated in Supplementary Figure S3 and summarized in Figure 4. Treatments were ranked based on their effect sizes for pain reduction, with combination therapy being the most effective, followed by exercise therapy, KT, and manual therapy. Please see Table 3 for the complete comparison and ranking.
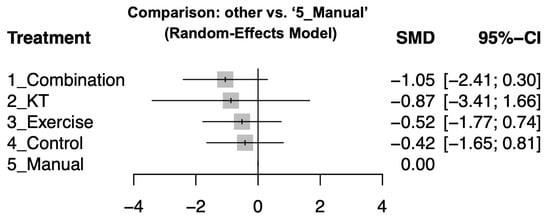
Figure 4.
Funnel plot assessing publication bias in the meta-analysis.

Table 3.
Pairwise comparison and ranking of different therapy types of interventions for reduction of shoulder pain at 12 weeks in rotator cuff-related shoulder pain.
3.5. Inconsistency Test
Consistency between direct and indirect comparisons was assessed using a global inconsistency test within the frequentist framework. All comparisons yielded non-significant results (p > 0.05), indicating no evidence of inconsistency across the network. These findings suggest that the transitivity assumption holds and that the pooled estimates are reliable across mixed sources of evidence. Detailed results are provided in Supplementary Tables S5 and S6.
However, certain treatment comparisons—particularly manual therapy versus KT (n = 2) and manual therapy versus combination therapy (n = 1)—were informed by a limited number of studies and participants. These nodes may be underpowered, and the corresponding effect estimates should be interpreted with caution.
3.6. Sensitivity Analyses
To evaluate the influence of study quality on the robustness of our findings, we conducted two complementary sensitivity analyses.
First, a leave-one-out (one-study removal) analysis demonstrated consistent treatment rankings and effect size estimates across all iterations. Combination therapy remained the most effective intervention in terms of both functional improvement and pain reduction. Interventions such as exercise therapy, KT, and manual therapy showed marginal effects, with no changes in direction or statistical significance when any single study was removed. These results suggest that no individual study exerted disproportionate influence on the overall conclusions (Supplementary Figures S4a–k).
Second, we conducted a subgroup sensitivity analysis excluding five studies assessed as having either “some concerns” or “high risk” of bias based on the Cochrane Risk of Bias 2.0 tool. As shown in Supplementary Figure S5a–j, the overall treatment rankings and relative effect sizes remained largely unchanged. Combination therapy continued to outperform other interventions across both primary outcomes.
Together, these analyses reinforce the methodological robustness of our findings and indicate that the conclusions regarding the superiority of combination therapy are not materially affected by study-level bias or the inclusion of specific trials.
4. Discussion
This network meta-analysis synthesized data from 11 randomized controlled trials to compare the efficacy of different physiotherapy interventions for RCRSP. Our analysis demonstrated that combination therapy (exercise plus manual therapy) yielded superior improvements in both functional outcomes and pain reduction at the 12-week mark, compared with single-modality treatments [14,38]. These improvements exceeded the established minimal clinically important differences (MCIDs) for DASH, SPADI, and VAS/NPRS measures, confirming both statistical and clinical relevance. These comparisons are detailed in Supplementary Table S7 [50,51,52,53].
The superiority of combination therapy is consistent with prior network meta-analyses and systematic reviews [1,27,54]. Notably, single-modality interventions often target isolated mechanisms (e.g., strengthening or joint mobility), whereas combination approaches address the multifactorial pathophysiology of RCRSP, including muscular deficits, joint instability, and central sensitization [18,54]. The synergistic effects of exercise and manual therapy are likely underpinned by complementary mechanisms: exercise promotes neuromuscular adaptation and joint stability [11,16,35], while manual therapy provides immediate pain modulation via mechanoreceptor activation and descending inhibition pathways [12,18]. This synergy potentially enhances patient tolerance and engagement, improving adherence and outcomes [23].
Mechanistic hypotheses are supported by prior studies. Camargo et al. [20] further reported that specific exercise and manual therapy improved kinematic control and reduced symptom chronicity. Moreover, combining interventions likely amplifies cortical plasticity and descending nociceptive inhibition, as suggested in neurophysiological literature [36,37,38,40]. From a biopsychosocial standpoint, multimodal therapy may also positively influence patient motivation and therapeutic alliance, which are increasingly recognized as important determinants of musculoskeletal outcomes [23].
However, most previous studies primarily focused on short-term outcomes, reporting immediate improvements such as ≥30% reduction in VAS scores or significant improvements in DASH scores (>10 points) [53,55], without thorough examination of mid- to long-term effects [4,17]. Our study addressed this gap by employing a fixed 12-week intervention framework to evaluate mid-term outcomes, demonstrating that combination therapy resulted in clinically meaningful improvements in upper limb function, reaching the minimal clinically important difference (MCID) in DASH scores.
Furthermore, the literature has reported that the recurrence rate of shoulder pain is approximately 30–40%, and 10–15% of patients continue to experience pain and functional limitations 12 months post-treatment [1,6]. Nonetheless, many studies lack structured designs specifying intervention durations [56,57,58], making it difficult to establish optimal treatment protocols in clinical practice. By standardizing the 12-week intervention period, our study not only helped clarify the comparative effectiveness of different modalities but also emphasized the critical role of treatment duration and frequency in clinical outcomes.
From a clinical perspective, our findings suggest a dual-focus strategy for RCRSP management: an initial phase focused on pain relief (through manual and adjunctive therapies), followed by progressive neuromuscular strengthening of the rotator cuff and scapular stabilizers to promote long-term functional recovery and prevent recurrence. Treatment strategies should be individualized based on different disease stages (acute, subacute, chronic phases) to optimize outcomes. Although combination therapy was more effective, it may be harder to use in everyday practice. It can take more time and cost more, especially if manual therapy is needed at every visit. This might not be practical in busy clinics or for patients with limited access. Future studies should look at how realistic and cost-effective this treatment is in real-world settings.
Study Limitations
This study has several limitations that warrant consideration. First, although no language restrictions were applied during the literature search, all included trials were published in English, introducing potential language bias. Future systematic reviews should incorporate non-English databases and multilingual collaboration to enhance comprehensiveness.
Second, selective reporting bias may have been present in trials lacking protocol registration or complete outcome disclosure. We recommend that future studies ensure transparent reporting and pre-registration of protocols to strengthen evidence reliability.
Third, variability in therapist skill and treatment fidelity across studies may have introduced indirect bias. Differences in clinician experience, training, and adherence to standardized protocols can influence treatment outcomes. Future trials should report provider qualifications and consider stratifying analyses by provider consistency to improve replicability.
Fourth, this review focused on outcomes measured at 12 weeks to ensure consistency across trials. However, this limits the ability to evaluate long-term treatment durability. Given the 30–40% recurrence rate of RCRSP and persistent symptoms in up to 15% of patients after one year, future studies should incorporate longer follow-up periods (e.g., 6–12 months) to assess sustainability and recurrence.
Fifth, although combination therapy demonstrated favorable point estimates, some comparisons yielded wide confidence intervals that crossed the null (e.g., −2.59 to 0.56 for function), indicating imprecision and statistical uncertainty. This suggests that the true effect may be smaller or inconclusive, emphasizing the need for larger, well-powered trials to validate these findings with greater precision.
Sixth, we did not explore how patient characteristics such as age or chronicity might influence treatment outcomes. This limits our ability to identify which groups respond best. Future research should examine these factors to support more personalized treatment plans.
Finally, although interventions were grouped by type (e.g., exercise, manual therapy), substantial heterogeneity existed in dosage, frequency, and technique. This may affect comparability and generalizability. Greater standardization and clearer reporting of physiotherapy protocols are essential for improving future evidence synthesis.
5. Conclusions
Combination therapy, especially exercise plus manual therapy, showed the greatest improvements in pain and function for RCRSP, with effect sizes exceeding clinical thresholds. These results support its use in practice. To enhance comparability and clinical translation, future trials should adopt standardized intervention protocols and longer follow-up durations.
Supplementary Materials
The following supporting information can be downloaded at https://www.mdpi.com/article/10.3390/jcm14134765/s1.
Author Contributions
C.-S.L., and K.-C.C. contributed equally to this work and are both considered first authors. Conceptualization, C.-S.L., K.-C.C., and W.-C.C.; methodology, C.-S.L., K.-C.C., and W.-C.C.; validation, C.-S.L., K.-C.C., and W.-C.C.; formal analysis, C.-S.L., K.-C.C., J.-C.S., and W.-C.C.; investigation, C.-S.L., K.-C.C., J.-C.S., B.C., and W.-C.C.; data curation, C.-S.L., K.-C.C., and W.-C.C.; writing—original draft preparation, C.-S.L., K.-C.C., and W.-C.C.; writing—review and editing, C.-S.L., K.-C.C., J.-C.S., B.C., and W.-C.C.; project administration, J.-C.S., and B.C.; funding acquisition, C.-S.L. All authors have read and agreed to the published version of the manuscript.
Funding
This study was supported by a grant from Chung Shan Medical University Hospital (Grant No. CSH-2021-C-035). The funders had no role in study design, data collection and analysis, interpretation of results, or the decision to submit the manuscript for publication.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
All related data are included and no new data were created.
Acknowledgments
Wei-Cheng Chao carried out this research with funding support in part from the Ph.D. Program in Tissue Engineering and Regenerative Medicine of National Chung Hsing University and National Health Research Institutes. Chien-Sheng Lo and Kuan-Chung Chen contributed equally to this work and are both considered first authors.
Conflicts of Interest
The authors declare no conflicts of interest. The funders had no role in the design of the study; in the collection, analyses, or interpretation of data; in the writing of the manuscript; or in the decision to publish the results.
Abbreviations
The following abbreviations are used in this manuscript:
| RCRSP | Rotator cuff-related shoulder pain |
| NMA | Meta-analysis |
| PRISMA | Preferred Reporting Items for Systematic Reviews and Meta-Analyses |
| PRISMA-NMA | PRISMA extension guidelines for network meta-analysis |
| KT | Kinesio taping |
| SPADI | Shoulder Pain and Disability Index |
| DASH | Disabilities of the Arm, Shoulder and Hand |
| VAS | Visual Analog Scale |
| NPRS | Numeric Pain Rating Scale |
| SIS | Subacromial impingement syndrome |
| TENS | Transcutaneous electrical nerve stimulation |
| EMS | Electrical muscular stimulation |
| PNF | Proprioceptive neuromuscular facilitation |
| SM | Shoulder mobilization |
| TrP-DN | Trigger point dry needling |
| SPS | Subacromial pain syndrome |
| PENS | Percutaneous electrical nerve stimulation |
| ESWT | Extracorporeal shock wave therapy |
| MET | Muscle energy technique |
References
- Aguilar García, M.; González Muñoz, A.; Pérez Montilla, J.J.; Aguilar Nuñez, D.; Hamed Hamed, D.; Pruimboom, L.; Navarro Ledesma, S. Which Multimodal Physiotherapy Treatment Is the Most Effective in People with Shoulder Pain? A Systematic Review and Meta-Analyses. Healthcare 2024, 12, 1234. [Google Scholar] [CrossRef] [PubMed]
- de Oliveira, F.C.L.; Pairot de Fontenay, B.; Bouyer, L.J.; Desmeules, F.; Roy, J.S. Kinesiotaping for the Rehabilitation of Rotator Cuff-Related Shoulder Pain: A Randomized Clinical Trial. Sports Health 2021, 13, 161–172. [Google Scholar] [CrossRef]
- Hunter, D.J.; Rivett, D.A.; McKiernan, S.; Luton, R.; Snodgrass, S.J. Thoracic Manual Therapy Improves Pain and Disability in Individuals with Shoulder Impingement Syndrome Compared with Placebo: A Randomized Controlled Trial With 1-Year Follow-up. Arch. Phys. Med. Rehabil. 2022, 103, 1533–1543. [Google Scholar] [CrossRef] [PubMed]
- Gutierrez-Espinoza, H.; Araya-Quintanilla, F.; Cereceda-Muriel, C.; Alvarez-Bueno, C.; Martinez-Vizcaino, V.; Cavero-Redondo, I. Effect of supervised physiotherapy versus home exercise program in patients with subacromial impingement syndrome: A systematic review and meta-analysis. Phys. Ther. Sport. 2020, 41, 34–42. [Google Scholar] [CrossRef] [PubMed]
- Blanco-Diaz, M.; Ruiz-Redondo, R.; Escobio-Prieto, I.; De la Fuente-Costa, M.; Albornoz-Cabello, M.; Casana, J. A Systematic Review of the Effectiveness of Dry Needling in Subacromial Syndrome. Biology 2022, 11, 243. [Google Scholar] [CrossRef]
- Dube, M.O.; Desmeules, F.; Lewis, J.S.; Roy, J.S. Does the addition of motor control or strengthening exercises to education result in better outcomes for rotator cuff-related shoulder pain? A multiarm randomised controlled trial. Br. J. Sports Med. 2023, 57, 457–463. [Google Scholar] [CrossRef]
- Hopewell, S.; Keene, D.J.; Heine, P.; Marian, I.R.; Dritsaki, M.; Cureton, L.; Dutton, S.J.; Dakin, H.; Carr, A.; Hamilton, W.; et al. Progressive exercise compared with best-practice advice, with or without corticosteroid injection, for rotator cuff disorders: The GRASP factorial RCT. Health Technol. Assess. 2021, 25, 1–158. [Google Scholar] [CrossRef]
- Lathiere, T.; Jaubert, A.; Lewis, J.; David-Tchouda, S.; Beard, D.; Pinsault, N. The health economic analysis of surgery versus rehabilitation in non-traumatic musculoskeletal shoulder disorders: A systematic review of trial-based studies. Clin. Rehabil. 2025, 39, 139–152. [Google Scholar] [CrossRef]
- Blume, C.; Wang-Price, S.; Trudelle-Jackson, E.; Ortiz, A. Comparison of Eccentric and Concentric Exercise Interventions in Adults with Subacromial Impingement Syndrome. Int. J. Sports Phys. Ther. 2015, 10, 441–455. [Google Scholar]
- Christiansen, D.H.; Hjort, J. Group-based exercise, individually supervised exercise and home-based exercise have similar clinical effects and cost-effectiveness in people with subacromial pain: A randomised trial. J. Physiother. 2021, 67, 124–131. [Google Scholar] [CrossRef]
- Gutiérrez-Espinoza, H.; Araya-Quintanilla, F.; Gutiérrez-Monclus, R.; Ríos-Riquelme, M.; Álvarez-Bueno, C.; Martínez-Vizcaino, V.; Cavero-Redondo, I. Does pectoralis minor stretching provide additional benefit over an exercise program in participants with subacromial pain syndrome? A randomized controlled trial. Musculoskelet. Sci. Pract. 2019, 44, 102052. [Google Scholar] [CrossRef]
- Aytar, A.; Baltaci, G.; Uhl, T.L.; Tuzun, H.; Oztop, P.; Karatas, M. The effects of scapular mobilization in patients with subacromial impingement syndrome: A randomized, double-blind, placebo-controlled clinical trial. J. Sport. Rehabil. 2015, 24, 116–129. [Google Scholar] [CrossRef] [PubMed]
- Frassanito, P.; Cavalieri, C.; Maestri, R.; Felicetti, G. Effectiveness of Extracorporeal Shock Wave Therapy and kinesio taping in calcific tendinopathy of the shoulder: A randomized controlled trial. Eur. J. Phys. Rehabil. Med. 2018, 54, 333–340. [Google Scholar] [CrossRef] [PubMed]
- Umay-Altas, E.; Ecem-Konak, H.; Unsal-Delialioglu, S.; Sahin-Onat, S.; Gunay-Ucurum, S. Mid-term effects of two different Kinesio tape treatments in female patients with subacromial impingement syndrome: Randomized controlled ultrasonographic study. J. Hand Ther. 2023, 36, 514–522. [Google Scholar] [CrossRef]
- de Oliveira, A.K.A.; da Costa, K.S.A.; de Lucena, G.L.; de Oliveira Sousa, C.; Filho, J.F.M.; Brasileiro, J.S. Comparing exercises with and without electromyographic biofeedback in subacromial pain syndrome: A randomized controlled trial. Clin. Biomech. 2022, 93, 105596. [Google Scholar] [CrossRef] [PubMed]
- Nazary-Moghadam, S.; Zarei-Moghadam, F.; Zeinalzadeh, A.; Ebrahimzadeh, M.H.; Moradi, A.; Emadzadeh, M.; Hasson, S. Effects of comprehensive physiotherapy compared with routine physiotherapy on pain and function in patients with subacromial pain syndrome: A randomized clinical trial with 6-month follow-up. J. Bodyw. Mov. Ther. 2024, 40, 270–278. [Google Scholar] [CrossRef]
- Boudreau, N.; Gaudreault, N.; Roy, J.S.; Bedard, S.; Balg, F. The Addition of Glenohumeral Adductor Coactivation to a Rotator Cuff Exercise Program for Rotator Cuff Tendinopathy: A Single-Blind Randomized Controlled Trial. J. Orthop. Sports Phys. Ther. 2019, 49, 126–135. [Google Scholar] [CrossRef]
- Menek, B.; Tarakci, D.; Algun, Z.C. The effect of Mulligan mobilization on pain and life quality of patients with Rotator cuff syndrome: A randomized controlled trial. J. Back. Musculoskelet. Rehabil. 2019, 32, 171–178. [Google Scholar] [CrossRef]
- Saracoglu, I.; Emuk, Y.; Taspinar, F. Does taping in addition to physiotherapy improve the outcomes in subacromial impingement syndrome? A systematic review. Physiother. Theory Pract. 2018, 34, 251–263. [Google Scholar] [CrossRef]
- Camargo, P.R.; Alburquerque-Sendin, F.; Avila, M.A.; Haik, M.N.; Vieira, A.; Salvini, T.F. Effects of Stretching and Strengthening Exercises, With and Without Manual Therapy, on Scapular Kinematics, Function, and Pain in Individuals With Shoulder Impingement: A Randomized Controlled Trial. J. Orthop. Sports Phys. Ther. 2015, 45, 984–997. [Google Scholar] [CrossRef]
- Sterne, J.A.C.; Savović, J.; Page, M.J.; Elbers, R.G.; Blencowe, N.S.; Boutron, I.; Cates, C.J.; Cheng, H.Y.; Corbett, M.S.; Eldridge, S.M.; et al. RoB 2: A revised tool for assessing risk of bias in randomised trials. BMJ 2019, 366, l4898. [Google Scholar] [CrossRef]
- Owen, R.K.; Bradbury, N.; Xin, Y.; Cooper, N.; Sutton, A. MetaInsight: An interactive web-based tool for analyzing, interrogating, and visualizing network meta-analyses using R-shiny and netmeta. Res. Synth. Methods 2019, 10, 569–581. [Google Scholar] [CrossRef] [PubMed]
- Gillison, F.B.; Skevington, S.M.; Sato, A.; Standage, M.; Evangelidou, S. The effects of exercise interventions on quality of life in clinical and healthy populations; a meta-analysis. Soc. Sci. Med. 2009, 68, 1700–1710. [Google Scholar] [CrossRef]
- Hutton, B.; Salanti, G.; Caldwell, D.M.; Chaimani, A.; Schmid, C.H.; Cameron, C.; Ioannidis, J.P.A.; Straus, S.; Thorlund, K.; Jansen, J.P.; et al. The PRISMA extension statement for reporting of systematic reviews incorporating network meta-analyses of health care interventions: Checklist and explanations. Ann. Intern. Med. 2015, 162, 777–784. [Google Scholar] [CrossRef] [PubMed]
- Ager, A.L.; de Oliveira, F.C.L.; Roy, J.S.; Borms, D.; Deraedt, M.; Huyge, M.; Deschepper, A.; Cools, A.M. Effects of elastic kinesiology taping on shoulder proprioception: A systematic review. Braz. J. Phys. Ther. 2023, 27, 100514. [Google Scholar] [CrossRef]
- Guo, R.; Luo, Y.; Xu, Y.; Lan, K.; Zhao, Y. Efficacy of modified posterior shoulder stretching exercises on shoulder function in subacromial impingement syndrome: A comprehensive meta-analysis. Medicine 2025, 104, e41117. [Google Scholar] [CrossRef]
- Yang, F.; Li, X.; Wang, J.; Gao, Q.; Pan, M.; Duan, Z.; Ren, C.; Guo, P.; Zhang, Y. Efficacy of different analgesic strategies combined with conventional physiotherapy program for treating chronic shoulder pain: A systematic review and network meta-analysis. J. Orthop. Surg. Res. 2024, 19, 544. [Google Scholar] [CrossRef]
- Chaimani, A.C.D.; Li, T.; Higgins, J.P.T.; Salanti, G. Chapter 11: Undertaking network meta-analyses [last updated October 2019]. In Cochrane Handbook for Systematic Reviews of Interventions Version 65; Higgins, J.P.T., Thomas, J., Chandler, J., Cumpston, M., Li, T., Page, M.J., Welch, V.A., Eds.; Cochrane: London, UK, 2024. [Google Scholar]
- Higgins, J.P.T.; Thomas, J.; Deeks, J.J. Chapter 6: Choosing effect measures and computing estimates of effect [last updated August 2023]. In Cochrane Handbook for Systematic Reviews of Interventions Version 65; Higgins, J.P.T., Thomas, J., Chandler, J., Cumpston, M., Li, T., Page, M.J., Welch, V.A., Eds.; Cochrane: London, UK, 2024. [Google Scholar]
- Deeks, J.J.; Higgins, J.P.T.; Altman, D.G.; McKenzie, J.E.; Veroniki, A.A. Chapter 10: Analysing data and undertaking meta-analyses [last updated November 2024]. In Cochrane Handbook for Systematic Reviews of Interventions Version 65; Higgins, J.P.T., Thomas, J., Chandler, J., Cumpston, M., Li, T., Page, M.J., Welch, V.A., Eds.; Cochrane: London, UK, 2024. [Google Scholar]
- Page, M.J.; Higgins, J.P.T.; Sterne, J.A.C. Chapter 13: Assessing risk of bias due to missing evidence in a meta-analysis [last updated August 2024]. In Cochrane Handbook for Systematic Reviews of Interventions version 65; Higgins, J.P.T., Thomas, J., Chandler, J., Cumpston, M., Li, T., Page, M.J., Welch, V.A., Eds.; Cochrane: London, UK, 2024. [Google Scholar]
- Higgins, J.P.T.; Eldridge, S.; Li, T. Chapter 23: Including variants on randomized trials [last updated October 2019]. In Cochrane Handbook for Systematic Reviews of Interventions Version 65; Higgins, J.P.T., Thomas, J., Chandler, J., Cumpston, M., Li, T., Page, M.J., Welch, V.A., Eds.; Cochrane: London, UK, 2024. [Google Scholar]
- Borenstein, M.; Hedges, L.V.; Higgins, J.P.T.; Rothstein, H.R. Fixed-Effect Versus Random-Effects Models: Introduction to Meta-Analysis; John Wiley & Sons: Chichester, UK, 2009; pp. 77–86. [Google Scholar]
- Kelley, K.; Preacher, K.J. On Effect Size. Psychol. Methods 2012, 17, 137–152. [Google Scholar] [CrossRef] [PubMed]
- Igrek, S.; Colak, T.K. Comparison of the effectiveness of proprioceptive neuromuscular facilitation exercises and shoulder mobilization patients with Subacromial Impingement Syndrome: A randomized clinical trial. J. Bodyw. Mov. Ther. 2022, 30, 42–52. [Google Scholar] [CrossRef]
- Arias-Buria, J.L.; Fernandez-de-Las-Penas, C.; Palacios-Cena, M.; Koppenhaver, S.L.; Salom-Moreno, J. Exercises and Dry Needling for Subacromial Pain Syndrome: A Randomized Parallel-Group Trial. J. Pain. 2017, 18, 11–18. [Google Scholar] [CrossRef]
- Valenzuela-Rios, C.; Arias-Buria, J.L.; Rodriguez-Jimenez, J.; Palacios-Cena, M.; Fernandez-de-Las-Penas, C. Effects of Adding Four Sessions of Ultrasound-Guided Percutaneous Electrical Nerve Stimulation to an Exercise Program in Patients with Shoulder Pain: A Randomized Controlled Trial. J. Clin. Med. 2024, 13, 3171. [Google Scholar] [CrossRef]
- Gunay Ucurum, S.; Kaya, D.O.; Kayali, Y.; Askin, A.; Tekindal, M.A. Comparison of different electrotherapy methods and exercise therapy in shoulder impingement syndrome: A prospective randomized controlled trial. Acta Orthop. Traumatol. Turc. 2018, 52, 249–255. [Google Scholar] [CrossRef] [PubMed]
- Moslehi, M.; Letafatkar, A.; Miri, H. Feedback improves the scapular-focused treatment effects in patients with shoulder impingement syndrome. Knee Surg. Sports Traumatol. Arthrosc. 2021, 29, 2281–2288. [Google Scholar] [CrossRef]
- Karamanlioglu, D.S.; Kaysin, M.Y.; Begoglu, F.A.; Akpinar, P.; Ozkan, F.U.; Aktas, I. Effects of acupuncture on pain and function in patients with subacromial impingement syndrome: A randomized sham-controlled trial. Integr. Med. Res. 2024, 13, 101049. [Google Scholar] [CrossRef] [PubMed]
- Arias-Buria, J.L.; Truyols-Dominguez, S.; Valero-Alcaide, R.; Salom-Moreno, J.; Atin-Arratibel, M.A.; Fernandez-de-Las-Penas, C. Ultrasound-Guided Percutaneous Electrolysis and Eccentric Exercises for Subacromial Pain Syndrome: A Randomized Clinical Trial. Evid. Based Complement. Altern. Med. 2015, 2015, 315219. [Google Scholar] [CrossRef] [PubMed]
- Pérez-Merino, L.; Casajuana, M.; Bernal, G.; Faba, J.; Astilleros, A.; González, R.; Giralt, M.; Romeu, M.; Nogués, M. Evaluation of the effectiveness of three physiotherapeutic treatments for subacromial impingement syndrome: A randomised clinical trial. Physiotherapy 2016, 102, 57–63. [Google Scholar] [CrossRef]
- Ager, A.L.; Roy, J.S.; Gamache, F.; Hebert, L.J. The Effectiveness of an Upper Extremity Neuromuscular Training Program on the Shoulder Function of Military Members With a Rotator Cuff Tendinopathy: A Pilot Randomized Controlled Trial. Mil. Med. 2019, 184, e385–e393. [Google Scholar] [CrossRef]
- Menek, B.; Tarakci, D.; Tarakci, E.; Menek, M.Y. Investigation on the Efficiency of the Closed Kinetic Chain and Video-Based Game Exercise Programs in the Rotator Cuff Rupture: A Randomized Trial. Games Health J. 2022, 11, 298–306. [Google Scholar] [CrossRef]
- Ingwersen, K.G.; Jensen, S.L.; Sørensen, L.; Jørgensen, H.R.; Christensen, R.; Søgaard, K.; Juul-Kristensen, B. Three Months of Progressive High-Load Versus Traditional Low-Load Strength Training Among Patients With Rotator Cuff Tendinopathy: Primary Results From the Double-Blind Randomized Controlled RoCTEx Trial. Orthop. J. Sports Med. 2017, 5, 2325967117723292. [Google Scholar] [CrossRef]
- Al Anazi, A.; Alghadir, A.H.; Gabr, S.A. Handgrip Strength Exercises Modulate Shoulder Pain, Function, and Strength of Rotator Cuff Muscles of Patients with Primary Subacromial Impingement Syndrome. Biomed. Res. Int. 2022, 2022, 9151831. [Google Scholar]
- Celik, E.B.; Tuncer, A. Comparing the Efficacy of Manual Therapy and Exercise to Synchronized Telerehabilitation with Self-Manual Therapy and Exercise in Treating Subacromial Pain Syndrome: A Randomized Controlled Trial. Healthcare 2024, 12, 1074. [Google Scholar] [CrossRef]
- Raeesi, J.; Negahban, H.; Kachooei, A.R.; Moradi, A.; Ebrahimzadeh, M.H.; Daghiani, M. Comparing the effect of physiotherapy and physiotherapy plus corticosteroid injection on pain intensity, disability, quality of life, and treatment effectiveness in patients with Subacromial Pain Syndrome: A randomized controlled trial. Disabil. Rehabil. 2023, 45, 4218–4226. [Google Scholar] [CrossRef]
- Daghiani, M.; Negahban, H.; Ebrahimzadeh, M.H.; Moradi, A.; Kachooei, A.R.; Raeesi, J.; Divandari, A. The effectiveness of comprehensive physiotherapy compared with corticosteroid injection on pain, disability, treatment effectiveness, and quality of life in patients with subacromial pain syndrome: A parallel, single-blind, randomized controlled trial. Physiother. Theory Pract. 2023, 39, 1591–1605. [Google Scholar] [CrossRef] [PubMed]
- Franchignoni, F.; Vercelli, S.; Giordano, A.; Sartorio, F.; Bravini, E.; Ferriero, G. Minimal clinically important difference of the disabilities of the arm, shoulder and hand outcome measure (DASH) and its shortened version (QuickDASH). J. Orthop. Sports Phys. Ther. 2014, 44, 30–39. [Google Scholar] [CrossRef]
- Roy, J.S.; MacDermid, J.C.; Woodhouse, L.J. Measuring shoulder function: A systematic review of four questionnaires. Arthritis Rheum. 2009, 61, 623–632. [Google Scholar] [CrossRef] [PubMed]
- Tashjian, R.Z.; Deloach, J.; Porucznik, C.A.; Powell, A.P. Minimal clinically important differences (MCID) and patient acceptable symptomatic state (PASS) for visual analog scales (VAS) measuring pain in patients treated for rotator cuff disease. J. Shoulder Elb. Surg. 2009, 18, 927–932. [Google Scholar] [CrossRef] [PubMed]
- Salaffi, F.; Stancati, A.; Silvestri, C.A.; Ciapetti, A.; Grassi, W. Minimal clinically important changes in chronic musculoskeletal pain intensity measured on a numerical rating scale. Eur. J. Pain. 2004, 8, 283–291. [Google Scholar] [CrossRef]
- Liu, S.; Chen, L.; Shi, Q.; Fang, Y.; Da, W.; Xue, C.; Li, X. Efficacy of manual therapy on shoulder pain and function in patients with rotator cuff injury: A systematic review and meta-analysis. Biomed. Rep. 2024, 20, 89. [Google Scholar] [CrossRef]
- Jensen, M.P.; Chen, C.; Brugger, A.M. Interpretation of visual analog scale ratings and change scores: A reanalysis of two clinical trials of postoperative pain. J. Pain. 2003, 4, 407–414. [Google Scholar] [CrossRef]
- Cadogan, A.; Laslett, M.; Hing, W.A.; McNair, P.J.; Coates, M.H. A prospective study of shoulder pain in primary care: Prevalence of imaged pathology and response to guided diagnostic blocks. BMC Musculoskelet. Disord. 2011, 12, 119. [Google Scholar] [CrossRef]
- Croft, P.; Pope, D.; Silman, A. The clinical course of shoulder pain: Prospective cohort study in primary care: Primary Care Rheumatology Society Shoulder Study Group. BMJ 1996, 313, 601–602. [Google Scholar] [CrossRef] [PubMed]
- Walker-Bone, K.; van der Windt, D.A.W.M. Shoulder Pain—Where Are We Now? Curr. Treat. Options Rheumatol. 2021, 7, 285–306. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).