Changes of Knee Phenotypes Following Osteotomy Around the Knee in Patients with Valgus or Varus Deformities—A Retrospective Cross-Sectional Study
Abstract
1. Introduction
2. Materials and Methods
2.1. Demographics
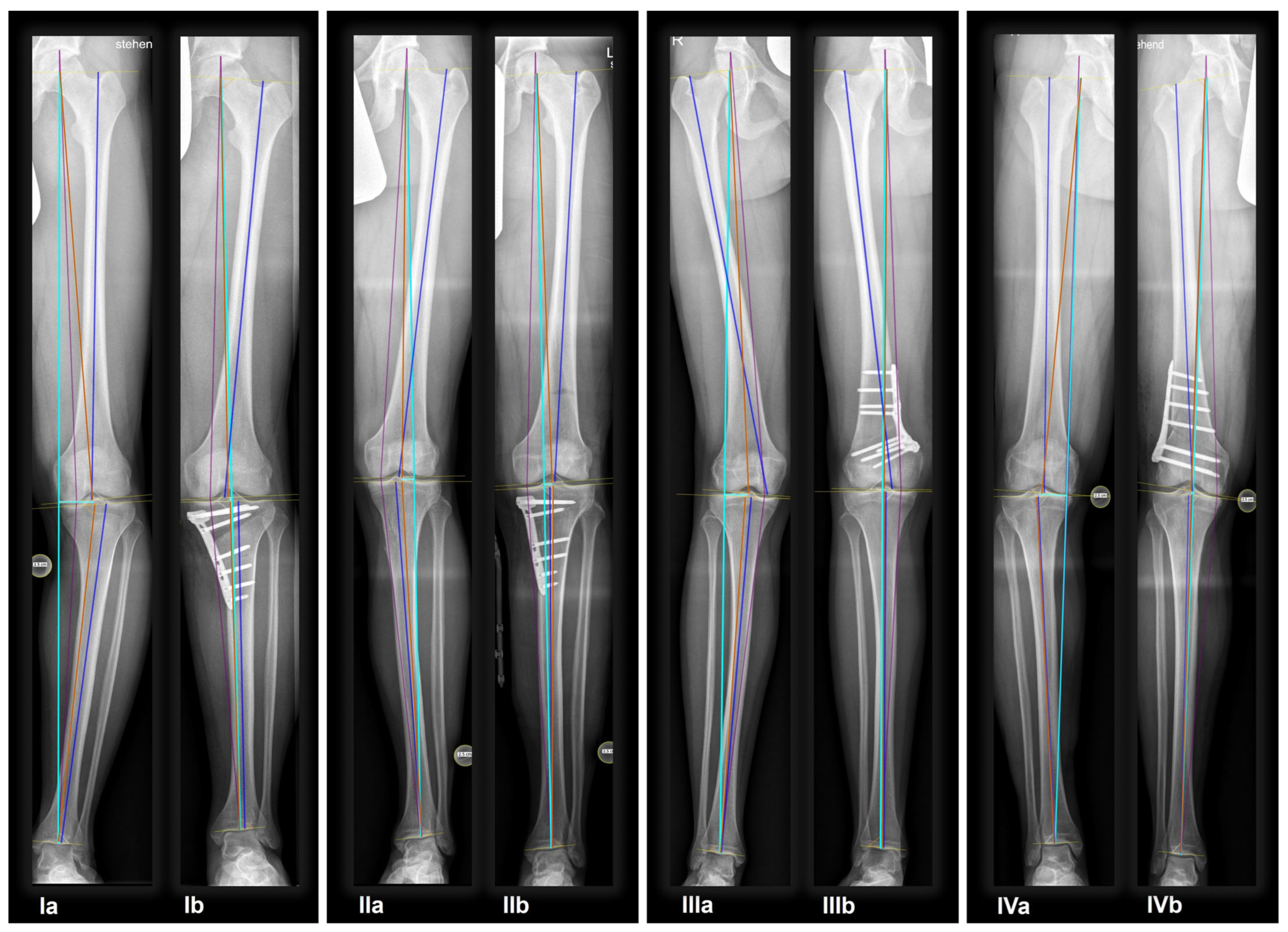
2.2. Radiographic Assessment
2.3. AI Software
2.4. Statistical Analysis
3. Results
3.1. Osteotomies
3.2. Hirschmann’s Phenotype Classification
3.3. Influences on Postoperative Radiographic Parameters
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Micicoi, G.; Grasso, F.; Kley, K.; Favreau, H.; Khakha, R.; Ehlinger, M.; Jacquet, C.; Ollivier, M. Osteotomy around the knee is planned toward an anatomical bone correction in less than half of patients. Orthop. Traumatol. Surg. Res. 2021, 107, 102897. [Google Scholar] [CrossRef] [PubMed]
- Dawson, M.J.; Ollivier, M.; Menetrey, J.; Beaufils, P. Osteotomy around the painful degenerative varus knee: A 2022 ESSKA formal consensus. Knee Surg. Sports Traumatol. Arthrosc. 2022, 31, 3041–3043. [Google Scholar] [CrossRef] [PubMed]
- Ramazanian, T.; Yan, S.; Rouzrokh, P.; Wyles, C.C.; O Byrne, T.J.; Taunton, M.J.; Maradit Kremers, H. Distribution and Correlates of Hip-Knee-Ankle Angle in Early Osteoarthritis and Preoperative Total Knee Arthroplasty Patients. J. Arthroplast. 2022, 37, S170–S175. [Google Scholar] [CrossRef] [PubMed]
- Cooke, D.; Scudamore, A.; Li, J.; Wyss, U.; Bryant, T.; Costigan, P. Axial lower-limb alignment: Comparison of knee geometry in normal volunteers and osteoarthritis patients. Osteoarthr. Cartil. 1997, 5, 39–47. [Google Scholar] [CrossRef]
- Radler, C.; Antonietti, G.; Ganger, R.; Grill, F. Recurrence of axial malalignment after surgical correction in congenital femoral deficiency and fibular hemimelia. Int. Orthop. 2011, 35, 1683–1688. [Google Scholar] [CrossRef]
- Micicoi, G.; Jacquet, C.; Sharma, A.; LiArno, S.; Faizan, A.; Kley, K.; Parratte, S.; Ollivier, M. Neutral alignment resulting from tibial vara and opposite femoral valgus is the main morphologic pattern in healthy middle-aged patients: An exploration of a 3D-CT database. Knee Surg. Sports Traumatol. Arthrosc. 2021, 29, 849–858. [Google Scholar] [CrossRef]
- Nakayama, H.; Schröter, S.; Yamamoto, C.; Iseki, T.; Kanto, R.; Kurosaka, K.; Kambara, S.; Yoshiya, S.; Higa, M. Large correction in opening wedge high tibial osteotomy with resultant joint-line obliquity induces excessive shear stress on the articular cartilage. Knee Surg. Sports Traumatol. Arthrosc. 2018, 26, 1873–1878. [Google Scholar] [CrossRef]
- MacDessi, S.J.; Griffiths-Jones, W.; Harris, I.A.; Bellemans, J.; Chen, D.B. Coronal Plane Alignment of the Knee (CPAK) classification. Bone Jt. J. 2021, 103-B, 329–337. [Google Scholar] [CrossRef]
- Hirschmann, M.T.; Moser, L.B.; Amsler, F.; Behrend, H.; Leclerq, V.; Hess, S. Functional knee phenotypes: A novel classification for phenotyping the coronal lower limb alignment based on the native alignment in young non-osteoarthritic patients. Knee Surg. Sports Traumatol. Arthrosc. 2019, 27, 1394–1402. [Google Scholar] [CrossRef]
- Huber, S.; Mitterer, J.A.; Vallant, S.M.; Simon, S.; Hanak-Hammerl, F.; Schwarz, G.M.; Klasan, A.; Hofstaetter, J.G. Gender-specific distribution of knee morphology according to CPAK and functional phenotype classification: Analysis of 8739 osteoarthritic knees prior to total knee arthroplasty using artificial intelligence. Knee Surg. Sports Traumatol. Arthrosc. 2023, 31, 4220–4230. [Google Scholar] [CrossRef]
- Franceschetti, E.; Campi, S.; Giurazza, G.; Tanzilli, A.; Gregori, P.; Laudisio, A.; Hirschmann, M.T.; Samuelsson, K.; Papalia, R. Mechanically aligned total knee arthroplasty does not yield uniform outcomes across all coronal plane alignment of the knee (CPAK) phenotypes. Knee Surg. Sports Traumatol. Arthrosc. 2024, 32, 3261–3271. [Google Scholar] [CrossRef] [PubMed]
- Paley, D. Principles of Deformity Correction; Springer: Berlin/Heidelberg, Germany, 2002; ISBN 978-3-642-63953-1. [Google Scholar]
- Mitterer, J.A.; Huber, S.; Schwarz, G.M.; Simon, S.; Pallamar, M.; Kissler, F.; Frank, B.J.H.; Hofstaetter, J.G. Fully automated assessment of the knee alignment on long leg radiographs following corrective knee osteotomies in patients with valgus or varus deformities. Arch. Orthop. Trauma Surg. 2023, 144, 1029–1038. [Google Scholar] [CrossRef] [PubMed]
- Steve Bogart SankeyMATIC. 2014. Available online: https://sankeymatic.com/build/ (accessed on 23 October 2023).
- Cohen, J. Statistical Power Analysis for the Behavioral Sciences; Lawrence Erlbaum Associates, Publishers: New York, NY, USA, 2013; Volume 7, ISBN 9781134742707. [Google Scholar]
- Tseng, T.H.; Wang, H.Y.; Tzeng, S.C.; Hsu, K.H.; Wang, J.H. Knee-ankle joint line angle: A significant contributor to high-degree knee joint line obliquity in medial opening wedge high tibial osteotomy. J. Orthop. Surg. Res. 2022, 17, 79. [Google Scholar] [CrossRef]
- Mullaji, A.; Bhoskar, R.; Singh, A.; Haidermota, M. Valgus arthritic knees can be classified into nine phenotypes. Knee Surg. Sports Traumatol. Arthrosc. 2022, 30, 2895–2904. [Google Scholar] [CrossRef]
- Ji, W.; Luo, C.; Zhan, Y.; Xie, X.; He, Q.; Zhang, B. A residual intra-articular varus after medial opening wedge high tibial osteotomy (HTO) for varus osteoarthritis of the knee. Arch. Orthop. Trauma Surg. 2019, 139, 743–750. [Google Scholar] [CrossRef]
- Charre, D.; An, J.S.; Khakha, R.; Kley, K.; Şahbat, Y.; Ollivier, M. ‘One millimetre equals one degree’ is a major source of inaccuracy in planning osteotomies around the knee for metaphyseal deformities compared to the digital planning. Knee Surg. Sports Traumatol. Arthrosc. 2024, 32, 987–999. [Google Scholar] [CrossRef]
- Kley, K.; Bin Abd Razak, H.R.; Khakha, R.S.; Wilson, A.J.; van Heerwaarden, R.; Ollivier, M. Soft-Tissue Management and Neurovascular Protection During Opening-Wedge High Tibial Osteotomy. Arthrosc. Tech. 2021, 10, e419–e422. [Google Scholar] [CrossRef]
- Ollivier, M.; Claes, S.; Mabrouk, A.; Elson, D.; Espejo-Reina, A.; Predescu, V.; Schröter, S.; Van heerwarden, R.; Menetrey, J.; Beaufils, P.; et al. Surgical strategy and complication management of osteotomy around the painful degenerative varus knee: ESSKA Formal Consensus Part II. Knee Surg. Sports Traumatol. Arthrosc. 2024, 32, 2194–2205. [Google Scholar] [CrossRef]
- Dawson, M.; Elson, D.; Claes, S.; Predescu, V.; Khakha, R.; Espejo-Reina, A.; Schröter, S.; van Heerwarden, R.; Menetrey, J.; Beaufils, P.; et al. Osteotomy around the painful degenerative varus knee has broader indications than conventionally described but must follow a strict planning process: ESSKA Formal Consensus Part I. Knee Surg. Sports Traumatol. Arthrosc. 2024, 32, 1891–1901. [Google Scholar] [CrossRef]
- Liu, L.M.; Lei, K.; Du, D.; Lin, Y.; Pan, Z.; Guo, L. Functional knee phenotypes appear to be more suitable for the Chinese OA population compared with CPAK classification: A study based on 3D CT reconstruction models. Knee Surgery, Sport. Traumatol. Arthrosc. 2024, 32, 1264–1274. [Google Scholar] [CrossRef]
- An, J.S.; Jacquet, C.; Loddo, G.; Mabrouk, A.; Koga, H.; Argenson, J.N.; Ollivier, M. Deformity in valgus knee malalignment is not only in the femur but also in tibia or both, based on demographic and morphological analysis before and after knee osteotomies. Knee Surg. Sports Traumatol. Arthrosc. 2024, 32, 1087–1095. [Google Scholar] [CrossRef]
- Sakai, M.; Akasaki, Y.; Akiyama, T.; Horikawa, T.; Okazaki, K.; Hamai, S.; Tsushima, H.; Kawahara, S.; Kurakazu, I.; Kubota, K.; et al. Similar short-term KOOS between open-wedge high tibial osteotomy and total knee arthroplasty in patients over age 60: A propensity score–matched cohort study. Mod. Rheumatol. 2023, 33, 623–628. [Google Scholar] [CrossRef] [PubMed]
- Akçaalan, S.; Akkaya, M.; Dogan, M.; Valdivielso, A.A.; Zeiton, M.A.; Mohammad, H.R.; Sangaletti, R.; Benazzo, F.; Kara, S.; Gehrke, T.; et al. Do age, gender, and region affect tibial slope? A multi-center study. Arch. Orthop. Trauma Surg. 2023, 143, 6983–6991. [Google Scholar] [CrossRef] [PubMed]
- Brouwer, G.M.; Van Tol, A.W.; Bergink, A.P.; Belo, J.N.; Bernsen, R.M.D.; Reijman, M.; Pols, H.A.P.; Bierma-Zeinstra, S.M.A. Association between valgus and varus alignment and the development and progression of radiographic osteoarthritis of the knee. Arthritis Rheum. 2007, 56, 1204–1211. [Google Scholar] [CrossRef] [PubMed]
- Harris, C.; Nadeem, F.; Hargreaves, M.; Campbell, C.; Momaya, A.; Casp, A. Obesity does not impact complications and conversion to total knee arthroplasty after high tibial osteotomy: A systematic review. Knee Surg. Sports Traumatol. Arthrosc. 2024, 32, 666–677. [Google Scholar] [CrossRef]
- Siboni, R.; Beaufils, P.; Boisrenoult, P.; Steltzlen, C.; Pujol, N. Opening-wedge high tibial osteotomy without bone grafting in severe varus osteoarthritic knee. Rate and risk factors of non-union in 41 cases. Orthop. Traumatol. Surg. Res. 2018, 104, 473–476. [Google Scholar] [CrossRef]
- Na, Y.G.; Lee, B.K.; Choi, J.U.; Lee, B.H.; Sim, J.A. Change of joint-line convergence angle should be considered for accurate alignment correction in high tibial osteotomy. Knee Surg. Relat. Res. 2021, 33, 4. [Google Scholar] [CrossRef]
- Sohn, S.; Koh, I.J.; Kim, M.S.; In, Y. Risk factors and preventive strategy for excessive coronal inclination of tibial plateau following medial opening-wedge high tibial osteotomy. Arch. Orthop. Trauma Surg. 2022, 142, 561–569. [Google Scholar] [CrossRef]
- Begum, F.A.; Kayani, B.; Magan, A.A.; Chang, J.S.; Haddad, F.S. Current concepts in total knee arthroplasty. Bone Jt. Open 2021, 2, 397–404. [Google Scholar] [CrossRef]
- Cherian, J.J.; Kapadia, B.H.; Banerjee, S.; Jauregui, J.J.; Issa, K.; Mont, M.A. Mechanical, anatomical, and kinematic axis in TKA: Concepts and practical applications. Curr. Rev. Musculoskelet. Med. 2014, 7, 89–95. [Google Scholar] [CrossRef]

| Patient Demographics | |||||
|---|---|---|---|---|---|
| Total | Medial Opening HTO | Medial Closing HTO | Medial Closing DFO | Lateral Closing DFO | |
| Proc/Pat | 214/188 | 130/115 | 15/14 | 54/44 | 15/15 |
| Sex (m/f) | 115/73 | 85/30 | 5/9 | 15/29 | 10/5 |
| Age (years) | 42 [14 to 65] | 45 [15 to 65] | 27 [16 to 53] | 33.5 [14 to 57] | 45 [21 to 53] |
| BMI (kg/m2) | 26.8 [17.7 to 39.8] | 27.0 [18.0 to 37.8] | 28.4 [21.2 to 38.0] | 26.7 [18.3 to 39.8] | 28.9 [23.4 to 38.5] |
| Osteotomies Around the Knee: n = 214 | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Total | Medial Opening HTO | Medial Closing HTO | Medial Closing DFO | Lateral Closing DFO | ||||||
| Alignment (by HKA) | ||||||||||
| Pre | Post | Pre | Post | Pre | Post | Pre | Post | Pre | Post | |
| Varus knee (<−3°) | 136 (63.6%) | 16 (7.4%) | 122 (93.8%) | 1 (0.8%) | - | 2 (13.3%) | - | 12 (22.2%) | 14 (93.3%) | 1 (6.7%) |
| Neutral (>−3°; <3°) | 16 (7.4%) | 157 (73.4%) | 8 (6.2%) | 94 (72.3%) | 2 (13.3%) | 11 (73.3%) | 5 (9.3%) | 40 (74.1%) | 1 (0.7%) | 12 (80.0%) |
| Valgus knee (>3) | 62 (30.0%) | 41 (19.2%) | - | 35 (26.9%) | 13 (86.7%) | 2 (13.3%) | 49 (90.7%) | 2 (3.7%) | - | 2 (13.3%) |
| Pre- and Postoperative Radiographic Parameters | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Total | Medial Opening HTO | Medial Closing HTO | Medial Closing DFO | Lateral Closing DFO | ||||||
| Pre | Post | Pre | Post | Pre | Post | Pre | Post | Pre | Post | |
| HKA (°) | −2.4 ± 6.7 | 0.7 ± 2.8 | −6.4 ± 2.5 | 1.6 ± 2.3 | 5.2 ± 3.1 | 0.3 ± 2.7 | 6.7 ± 3.4 | −1.3 ± 2.7 | −7.5 ± 3.4 | 0.7 ± 3.2 |
| MAD (mm) | 8.7 ± 23.7 | −2.6 ± 9.9 | 22.8 ± 9.1 | −5.4 ± 8.2 | −18.2 ± 10.9 | −0.7 ± 9.8 | −23.1 ± 12.3 | 3.7 ± 10.0 | 28.2 ± 13.6 | −3.2 ± 11.8 |
| mLPFA (°) | 87.6 ± 7.5 | 86.7 ± 5.9 | 88.2 ± 5.5 | 86.9 ± 5.8 | 88.1 ± 5.6 | 88.0 ± 5.4 | 85.3 ± 11.5 | 86.3 ± 6.0 | 89.2 ± 3.7 | 85.0 ± 6.0 |
| mLDFA (°) | 87.2 ± 3.5 | 87.7 ± 2.9 | 88.4 ± 1.8 | 87.5 ± 2.0 | 86.1 ± 2.1 | 85.1 ± 2.4 | 83.3 ± 2.7 | 89.9 ± 3.3 | 92.6 ± 3.8 | 84.5 ± 3.4 |
| mMPTA (°) | 86.4 ± 4.2 | 90.1 ± 3.3 | 83.9. ± 2.9 | 91.1 ± 3.3 | 93.0 ± 1.9 | 86.1 ± 1.9 | 90.0 ± 2.4 | 89.4 ± 2.6 | 88.1 ± 1.6 | 88.4 ± 2.0 |
| mLDTA (°) | 87.5 ± 3.8 | 85.9 ± 4.2 | 87.9 ± 3.8 | 86.2 ± 4.0 | 85.8 ± 2.9 | 85.0 ± 3.0 | 86.9 ± 3.7 | 85.1 ± 4.4 | 87.9 ± 3.7 | 86.3 ± 4.9 |
| JLCA (°) | −1.6 ± 2.0 | −1.6 ± 2.0 | −2.0 ± 1.7 | −2.1 ± 1.8 | −1.8 ± 1.3 | −0.6 ± 0.9 | −0.2 ± 2.0 | −0.6 ± 2.0 | −3.1 ± 2.0 | −2.9 ± 1.3 |
| aHKA (°) | −0.8 ± 6.1 | 2.4 ± 3.7 | −4.5 ± 2.9 | 3.6 ± 3.2 | 6.9 ± 3.1 | 1.0 ± 2.4 | 6.7 ± 3.3 | −0.5 ± 3.2 | −4.4 ± 3.7 | 3.8 ± 4.0 |
| JLO (°) | 173.6 ± 4.6 | 177.9 ± 5.0 | 172.3 ± 3.8 | 178.6 ± 4.4 | 179.1 ± 2.4 | 171.1 ± 3.1 | 173.3 ± 3.9 | 179.3 ± 5.0 | 180.7 ± 4.6 | 172.9 ± 3.8 |
| Postoperative CPAK | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| I | II | III | IV | V | VI | VII | VIII | IX | |||
 |  |  |  |  |  |  |  |  | |||
| Preoperative CPAK | HTO | I 96 (66.2%) | 2 (2.1%) | 18 (18.7%) | 15 (15.6%) | 2 (2.1%) | 14 (14.6%) | 34 (4.6%) | - | 2 (2.1%) | 9 (9.4%) |
| II 21 (14.5%) | - | 2 (9.5%) | 5 (23.8%) | 1 (4.8%) | - | 13 (61.9%) | - | - | - | ||
| III 3 (2.1%) | - | - | 2 (66.7%) | - | - | 1 (33.3%) | - | - | - | ||
| IV 6 (4.1%) | - | - | - | - | 1 (16.7%) | 3 (50.0%) | - | - | 2 (33.3%) | ||
| V 6 (4.1%) | - | - | - | - | - | 4 (66.7%) | - | - | 2 (33.3%) | ||
| VI 11 (7.6%) | 1 (9.1%) | 4 (36.4%) | 6 (54.5%) | - | - | - | - | - | - | ||
| IX 2 (1.4%) | 1 (50.0%) | - | - | - | 1 (50.0%) | - | - | - | - | ||
| Total 145 | 4 (2.8%) | 24 (16.5%) | 28 (19.3%) | 3 (2.1%) | 16 (11.0%) | 55 (37.9%) | - | 2 (1.4%) | 13 (9.0%) | ||
| DFO | I1 (1.4%) | - | - | 1 (100%) | - | - | - | - | - | - | |
| II 3 (4.4%) | - | 1 (33.3%) | 1 (33.3%) | 1 (33.3%) | - | - | - | - | - | ||
| III 44 (63.8%) | 3 (6.8%) | 5 (11.4%) | 4 (9.1%) | 8 (18.2%) | 12 (27.3%) | 5 (11.4%) | 5 (11.4%) | 1 (2.3%) | 1 (2.3%) | ||
| IV 8 (11.6%) | - | 2 (25.0%) | 6 (75.0%) | - | - | - | - | - | - | ||
| V 2 (2.9%) | - | - | 2 (100%) | - | - | - | - | - | - | ||
| VI 7 (10.1%) | - | - | - | 1 (14.3%) | 1 (14.3%) | - | 2 (28.6%) | 2 (28.6%) | 1 (14.3%) | ||
| VII 4 (5.8%) | - | - | 2 (50.0%) | - | - | 1 (25.0%) | 1 (25.0%) | - | - | ||
| Total 69 | 4 (5.5%) | 9 (12.3%) | 17 (23.3%) | 10 (13.7%) | 14 (19.2%) | 6 (8.2%) | 8 (11.0%) | 3 (4.1%) | 2 (2.7%) | ||
| 145 | Preoperative HTO: n = 132 | Postoperative HTO: n = 128 | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| VAR mLDFA6° | VAR mLDFA3° | NEU mLDFA0° | VAL mLDFA3° | VAL mLDFA6° | VARmLDFA6° | VARmLDFA3° | NEUmLDFA0° | VALmLDFA3° | VALmLDFA6° | ||||
| Varus (85.6%) | VARmMPTA6° | 1 (3.6%) | 8 (28.6%) | 17 (60.7%) | 2 (7.1%) | - | Varus (2.3%) | VARmMPTA6° | - | - | - | - | - |
| VARmMPTA3° | 6 (10.5%) | 23 (40.4%) | 26 (45.6%) | 2 (3.5%) | - | VARmMPTA3° | - | - | - | 1 (100%) | - | ||
| NEUmMPTA0° | 1 (3.9%) | 18 (69.2%) | 7 (26.9%) | - | - | NEUmMPTA0° | - | - | 1 (100%) | - | - | ||
| VALmMPTA3° | - | 1 (50.0%) | 1 (50.0%) | - | - | VALmMPTA3° | - | - | - | - | 1 (100%) | ||
| VALmMPTA6° | - | - | - | - | - | VALmMPTA6° | - | - | - | - | - | ||
| Neutral (7.6%) | VARmMPTA6° | - | - | - | - | - | Neutral (79.7%) | VARmMPTA6° | - | - | - | 1 (100%) | - |
| VARmMPTA3° | - | - | 1 (100%) | - | - | VARmMPTA3° | - | - | 4 (33.3%) | 7 (58.3%) | 1 (8.3%) | ||
| NEUmMPTA0° | - | 1 (25.0%) | 2 (50.0%) | 1 (25.0%) | - | NEUmMPTA0° | - | - | 12 (48.0%) | 13 (52.0%) | - | ||
| VALmMPTA3° | - | 1 (25.0%) | 3 (75.0%) | - | - | VALmMPTA3° | - | - | 17 (53.1%) | 15 (46.9%) | - | ||
| VALmMPTA6° | - | 1 (100%) | - | - | - | VALmMPTA6° | - | - | 12 (37.5%) | 19 (59.4%) | 1 (3.1%) | ||
| Valgus (6.8%) | VARmMPTA6° | - | - | - | - | - | Valgus (18.0%) | VARmMPTA6° | - | - | - | - | - |
| VARmMPTA3° | - | - | - | - | - | VARmMPTA3° | - | - | - | - | - | ||
| NEUmMPTA0° | - | - | - | - | - | NEUmMPTA0° | - | - | - | - | 1 (100%) | ||
| VALmMPTA3° | - | - | - | 1 (100%) | - | VALmMPTA3° | - | - | 5 (50.0%) | 5 (50.0%) | - | ||
| VALmMPTA6° | - | - | 6 (75.0%) | 2 (25.0%) | - | VALmMPTA6° | - | - | 6 (50.0%) | 6 (50.0%) | - | ||
| Preoperative DFO: n = 60 | Postoperative DFO: n = 63 | ||||||||||||
| VARmLDFA6° | VARmLDFA3° | NEUmLDFA0° | VALmLDFA3° | VALmLDFA6° | VARmLDFA6° | VARmLDFA3° | NEUmLDFA0° | VALmLDFA3° | VALmLDFA6° | ||||
| Varus (20.0%) | VARmMPTA6° | - | - | - | - | - | Varus (15.9%) | VARmMPTA6° | - | - | - | - | - |
| VARmMPTA3° | 1 (100%) | - | - | - | - | VARmMPTA3° | - | - | 1 (50.0%) | - | 1 (50.0%) | ||
| NEUmMPTA0° | 4 (57.1%) | 3 (42.9%) | - | - | - | NEUmMPTA0° | - | - | - | 1 (25.0%) | 3 (75.0%) | ||
| VALmMPTA3° | 2 (50.0%) | 2 (50.0%) | - | - | - | VALmMPTA3° | - | - | - | 1 (25.0%) | 3 (75.0%) | ||
| VALmMPTA6° | - | - | - | - | - | VALmMPTA6° | - | - | - | - | - | ||
| Neutral (10.0 %) | VARmMPTA6° | - | - | - | - | - | Neutral (79.4%) | VARmMPTA6° | - | - | - | - | - |
| VARmMPTA3° | - | - | - | - | - | VARmMPTA3° | - | - | - | 1 (33.3) | 2 (66.7%) | ||
| NEUmMPTA0° | - | - | 3 (60.0%) | 2 (40.0%) | - | NEUmMPTA0° | - | - | 3 (15.0%) | 16 (80.0%) | 1 (5.0%) | ||
| VALmMPTA3° | - | - | - | 1 (100%) | - | VALmMPTA3° | - | - | 8 (34.8%) | 12 (52.2%) | 3 (13.0%) | ||
| VALmMPTA6° | - | - | - | - | - | VALmMPTA6° | - | - | 1 (25.0%) | 2 (50.0%) | 1 (25.0%) | ||
| Valgus (70.0%) | VARmMPTA6° | - | - | - | - | - | Valgus (4.5%) | VARmMPTA6° | - | - | - | - | - |
| VARmMPTA3° | - | - | - | - | 1 (100%) | VARmMPTA3° | - | - | - | - | 1 (100%) | ||
| NEUmMPTA0° | - | - | - | 3 (50.0%) | 3 (50.0%) | NEUmMPTA0° | - | - | - | - | - | ||
| VALmMPTA3° | 1 (3.6%) | - | 2 (7.1%) | 19 (67.9%) | 6 (21.4%) | VALmMPTA3° | - | - | - | - | 2 (100%) | ||
| VALmMPTA6° | - | - | 2 (28.6%) | 5 (71.4%) | - | VALmMPTA6° | - | - | - | - | - | ||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Mitterer, J.A.; Huber, S.; Pallamar, M.; Simon, S.; Nolte, J.; Chiari, C.; Hofstaetter, J.G. Changes of Knee Phenotypes Following Osteotomy Around the Knee in Patients with Valgus or Varus Deformities—A Retrospective Cross-Sectional Study. J. Clin. Med. 2025, 14, 4684. https://doi.org/10.3390/jcm14134684
Mitterer JA, Huber S, Pallamar M, Simon S, Nolte J, Chiari C, Hofstaetter JG. Changes of Knee Phenotypes Following Osteotomy Around the Knee in Patients with Valgus or Varus Deformities—A Retrospective Cross-Sectional Study. Journal of Clinical Medicine. 2025; 14(13):4684. https://doi.org/10.3390/jcm14134684
Chicago/Turabian StyleMitterer, Jennyfer A., Stephanie Huber, Matthias Pallamar, Sebastian Simon, Jan Nolte, Catharina Chiari, and Jochen G. Hofstaetter. 2025. "Changes of Knee Phenotypes Following Osteotomy Around the Knee in Patients with Valgus or Varus Deformities—A Retrospective Cross-Sectional Study" Journal of Clinical Medicine 14, no. 13: 4684. https://doi.org/10.3390/jcm14134684
APA StyleMitterer, J. A., Huber, S., Pallamar, M., Simon, S., Nolte, J., Chiari, C., & Hofstaetter, J. G. (2025). Changes of Knee Phenotypes Following Osteotomy Around the Knee in Patients with Valgus or Varus Deformities—A Retrospective Cross-Sectional Study. Journal of Clinical Medicine, 14(13), 4684. https://doi.org/10.3390/jcm14134684







