Virtual Reality Gaming and Its Impact and Effectiveness in Improving Eye–Hand Coordination and Attention Concentration in the Oldest-Old Population
Abstract
1. Introduction
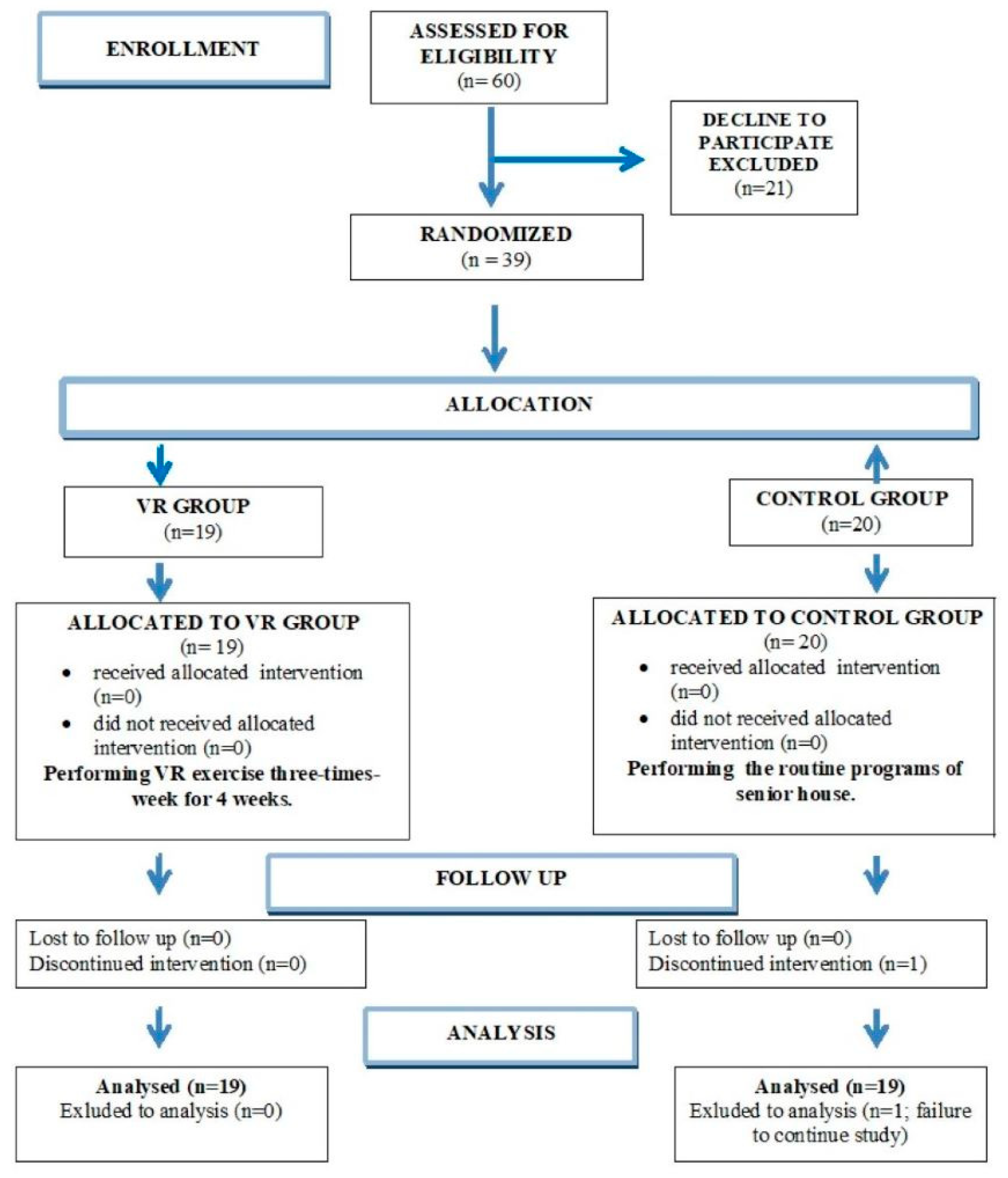
2. Materials and Methods
2.1. Participants
2.2. Study Design Intervention
2.3. Outcome Measures
2.3.1. Eye–Hand Coordination and Attention Concentration Measurements (T0/T1)
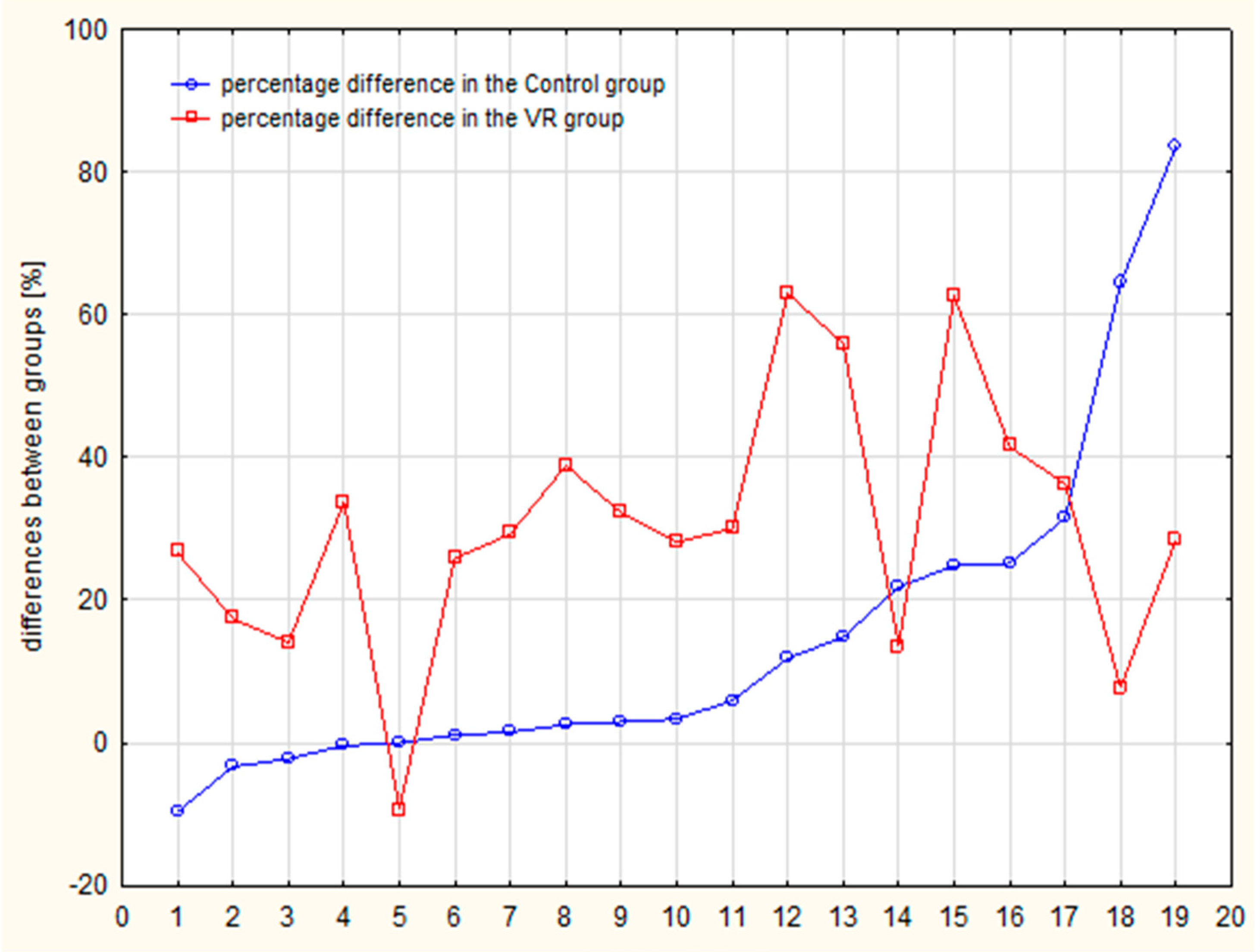
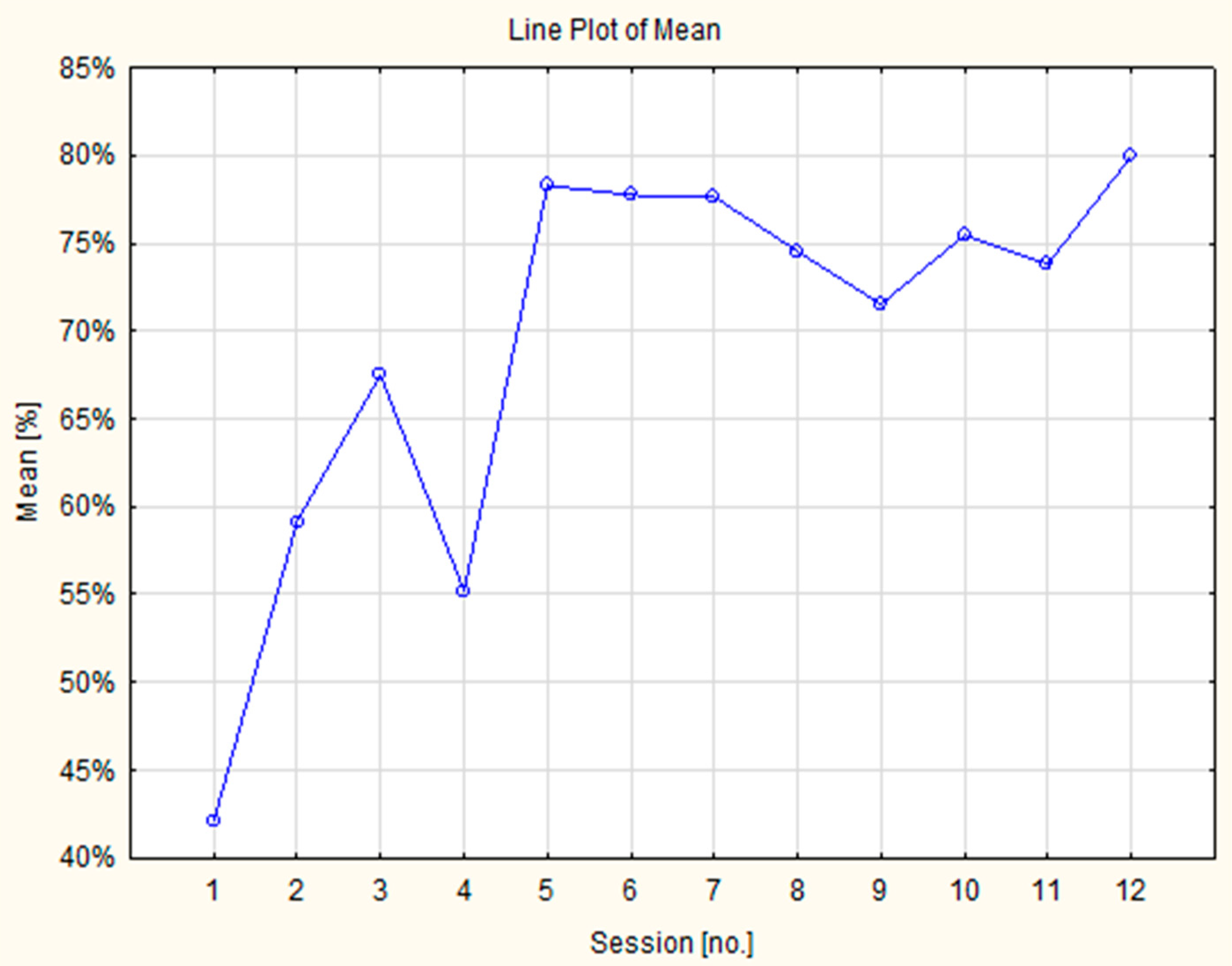
2.3.2. Control of the Effectiveness of “Good Cuts” During a Gaming in the Intervention Group
2.4. Statistical Analysis
3. Results
| Cross Visual Motor Test (% of 90 Light Stimulus) | Groups | |||
|---|---|---|---|---|
| VR Group T0 (Before) | VR Group T1 (After) | Control Group T0 (Before) | Control Group T1 (After) | |
| Mean (SD) | 45.1 (21.6) | 75.5 (15.4) | 17.3 (21.8) | 32.0 (32.9) |
| Median (Q1–Q3) | 42.2 (28.9–64.8) | 77.4 (66.3–88.5) | 8.5 (3.3–19.3) | 9.6 (4.8–69.3) |
| Statistical analyses | ||||
| Test | Comparison | p value | D effect | |
| U Mann Whitney | VR group in T0 vs. control group in T0 | 0.0003 | 1.281 * | |
| VR group in T1 vs. control group in T1 | 0.0003 | 1.692 * | ||
| Paired Wilcoxon | VR group in T0 vs. VR group in T1 | 0.0002 | 1.689 ** | |
| control group in T0 vs. control group in T1 | 0.0065 | 0.615 ** | ||
4. Discussion
5. Limitations
6. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- WHO. Ageing and Health 2024. Available online: https://www.who.int/news-room/fact-sheets/detail/ageing-and-health (accessed on 20 January 2025).
- Residential Population Forecast for Poland for 2023-2060, Central Statistical Office. Available online: https://stat.gov.pl/files/gfx/portalinformacyjny/pl/defaultaktualnosci/5469/12/1/1/prognoza_ludnosci_rezydujacej_dla_polski_na_lata_2023-2060.pdf (accessed on 19 June 2025).
- Eells, M.; Kane, R.L.; Kane, R.A. Assessing Older Persons: Measures, Meaning, and Practical Application; Oxford University Press: England, UK, 2004. [Google Scholar]
- Mazurek, J.; Szcześniak, D.; Urbańska, K.; Dröes, R.-M.; Rymaszewska, J. Met and unmet care needs of older people with dementia living at home: Personal and informal carers’ perspectives. Dementia 2017, 18, 1963–1975. [Google Scholar] [CrossRef] [PubMed]
- Mazurek, J.; Szcześniak, D.; Trypka, E.; Lion, K.M.; Wallner, R.; Rymaszewska, J. Needs of Older People Attending Day Care Centres in Poland. Healthcare 2020, 8, 310. [Google Scholar] [CrossRef] [PubMed]
- Pei, Y.C.; Chou, S.W.; Lin, P.S.; Lin, Y.-C.; Hsu, T.H.; Wong, A.M. Eye-hand coordination of elderly people who practice Tai Chi Chuan. J. Formos. Med. Assoc. 2008, 107, 103–110. [Google Scholar] [CrossRef] [PubMed]
- Boisseau, E.; Scherzer, P.; Cohen, H. Eye-hand coordination in aging and in Parkinson’s disease. Aging Neuropsychol. Cognit. 2002, 9, 266–275. [Google Scholar] [CrossRef]
- Guan, J.; Wade, M.G. The effect of aging on adaptive eye-hand coordination. J. Gerontol. B Psychol. Sci. Soc. Sci. 2000, 55, 151–162. [Google Scholar] [CrossRef]
- Van Halewyck, F.; Lavrysen, A.; Levin, O.; Boisgontier, M.P.; Elliott, D.; Helsen, W.F. Both age and physical activity level impact on eye-hand coordination. Hum. Mov. Sci. 2014, 36, 80–96. [Google Scholar] [CrossRef] [PubMed]
- Dunsky, A. The Effect of Balance and Coordination Exercises on Quality of Life in Older Adults: A Mini-Review. Front. Aging Neurosci. 2019, 11, 318. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Gao, K.L.; Ng, S.S.; Kwok, J.W.; Chow, R.; Tsang, W. Eye-hand coordination and its relationship with sensori-motor impairments in stroke survivors. J. Rehabil. Med. 2010, 42, 368–373. [Google Scholar] [CrossRef]
- Crawford, J.D.; Medendorp, W.P.; Marotta, J.J. Spatial transformations for eye-hand coordination. J. Neurophysiol. 2004, 92, 10–19. [Google Scholar] [CrossRef]
- Duijff, S.; Klaassen, P.; Beemer, F.; de Veye, H.S.; Vorstman, J.; Sinnema, G. Intelligence and visual motor integration in 5-year-old children with 22q11-deletion syndrome. Res. Dev. Disabil. 2012, 33, 334–340. [Google Scholar] [CrossRef]
- Inzelberg, R.; Schechtman, E.; Hocherman, S. Visuo-motor coordination deficits and motor impairments in Parkinson’s disease. PLoS ONE 2008, 3, e3663. [Google Scholar] [CrossRef] [PubMed]
- Wang, H.; Naghavi, M.; Allen, C.; Barber, R.M.; Bhutta, Z.A.; Carter, A.; Casey, D.C.; Charlson, F.J.; Zian Chen, A.; Coates, M.M.; et al. GBD 2015 Mortality and Causes of Death Collaborators. Global, regional, and national life expectancy, all-cause mortality, and cause-specific mortality for 249 causes of death, 1980-2015: A systematic analysis for the Global Burden of Disease Study 2015. Lancet 2016, 388, 1459–1544. [Google Scholar] [CrossRef] [PubMed]
- Wimo, A.; Jönsson, L.; Bond, J.; Prince, M.; Winblad, B.; Alzheimer Disease International. The worldwide economic impact of dementia 2010. Alzheimers Dement. 2013, 9, 1–11. [Google Scholar] [CrossRef]
- Lee, K.; Junghans, B.M.; Ryan, M.; Khuu, S.; Suttle, C.M. Development of a novel approach to the assessment of eye-hand coordination. J. Neurosci. Methods 2014, 228, 50–56. [Google Scholar] [CrossRef] [PubMed]
- Chan, P.T.; Chang, W.C.; Chiu, H.L.; Kao, C.-C.; Liu, D.; Chu, H.; Chou, K.-R. Effect of interactive cognitive-motor training on eye-hand coordination and cognitive function in older adults. BMC Geriatr. 2019, 19, 27. [Google Scholar] [CrossRef]
- Chu, H.Y.; Chan, H.S.; Chen, M.F. Effects of Horticultural Activities on Attitudes toward Aging, Sense of Hope and Hand-Eye Coordination in Older Adults in Residential Care Facilities. Int. J. Environ. Res. Public Health 2021, 18, 6555. [Google Scholar] [CrossRef]
- Sepehrikia, M.; Abedanzadeh, R.; Saemi, E. Brain gym exercises improve Eye-Hand coordination in elderly males. Somatosens. Mot. Res. 2024, 41, 191–196. [Google Scholar] [CrossRef]
- Zioga, T.; Ferentinos, A.; Konsolaki, E.; Nega, C.; Kourtesis, P. Video Game Skills across Diverse Genres and Cognitive Functioning in Early Adulthood: Verbal and Visuospatial Short-Term and Working Memory, Hand-Eye Coordination, and Empathy. Behav. Sci. 2024, 14, 874. [Google Scholar] [CrossRef]
- Tao, G.; Garrett, B.; Taverner, T.; Cordingley, E.; Sun, C. Immersive virtual reality health games: A narrative review of game design. J. Neuroeng. Rehabil. 2021, 18, 31. [Google Scholar] [CrossRef]
- Peng, Y.; Wang, Y.; Zhang, L.; Zhang, Y.; Sha, L.; Dong, J.; He, Y. Virtual reality exergames for improving physical function, cognition and depression among older nursing home residents: A systematic review and meta-analysis. Geriatr. Nurs. 2024, 57, 31–44. [Google Scholar] [CrossRef]
- Moret, B.; Nucci, M.; Campana, G. Effects of exergames on mood and cognition in healthy older adults: A randomized pilot study. Front. Psychol. 2022, 13, 1018601. [Google Scholar] [CrossRef] [PubMed]
- Ren, Y.; Lin, C.; Zhou, Q.; Zhang, Y.; Wang, G.; Lu, A. Effectiveness of virtual reality games in improving physical function, balance and reducing falls in balance-impaired older adults: A systematic review and meta-analysis. Arch. Gerontol. Geriatr. 2023, 108, 104924. [Google Scholar] [CrossRef] [PubMed]
- Cieślik, B.; Wrzeciono, A.; Mazurek, J.; Federico, S.; Szczepańska-Gieracha, J.; Kiper, P. Balance board or motion capture? A meta-analysis exploring the effectiveness of commercially available virtual reality exergaming in enhancing balance and functional mobility among the elderly. Games Health J. 2024, 13, 407–418. [Google Scholar] [CrossRef] [PubMed]
- Chen, P.J.; Hsu, H.F.; Chen, K.M.; Belcastro, F. VR exergame interventions among older adults living in long-term care facilities: A systematic review with Meta-analysis. Ann. Phys. Rehabil. Med. 2023, 66, 101702. [Google Scholar] [CrossRef]
- Di Fabio, R.P.; Greany, J.F.; Emasithi, A.; Wyman, J.F. Eye-head coordination during postural perturbation as a predictor of falls in community-dwelling elderly women. Arch. Phys. Med. Rehabil. 2002, 83, 942–951. [Google Scholar] [CrossRef]
- O’Rielly, J.L.; Ma-Wyatt, A. Changes to online control and eye-hand coordination with healthy ageing. Hum. Mov. Sci. 2018, 59, 244–257. [Google Scholar] [CrossRef]
- Rutkowski, S.; Jakóbczyk, A.; Abrahamek, K.; Nowakowska, A.; Nowak, M.; Liska, D.; Batalik, L.; Colombo, V.; Sacco, M. Training using a commercial immersive virtual reality system on hand–eye coordination and reaction time in students: A randomized controlled trial. Virtual Real. 2024, 28, 7. [Google Scholar] [CrossRef]
- Smith, A.P. Twenty-five years of research on the behavioural malaise associated with influenza and the common cold. Psychoneuroendocrinology 2013, 38, 744–751. [Google Scholar] [CrossRef]
- Recommendation by the American Heart Association Target Heart Rates Chart|American Heart Association. Available online: https://www.heart.org/en/healthy-living/fitness/fitness-basics/target-heart-rates (accessed on 20 January 2025).
- Campo-Prieto, P.; Cancela-Carral, J.M.; Rodríguez-Fuentes, G. Feasibility and Effects of an Immersive Virtual Reality Exergame Program on Physical Functions in Institutionalized Older Adults: A Randomized Clinical Trial. Sensors 2022, 22, 6742. [Google Scholar] [CrossRef]
- Sushil, C.; Sharma, G.; Salam, A.A.; Jha, D.; Mittal, A.P. Playing Action Video Games a Key to Cognitive Enhancement. Procedia Comput. Sci. 2016, 84, 115–122. [Google Scholar] [CrossRef]
- Ramadhana, A.B.; Chen, H.L. A Commercial off-the-Shelf Immersive virtual reality game: Its Effect on Engineering Students. Educ. Inf. Technol. 2023, 28, 12319–12335. [Google Scholar] [CrossRef]
- Rutkowski, S.; Adamczyk, M.; Pastuła, A.; Gos, E.; Luque-Moreno, C.; Rutkowska, A. Training Using a Commercial Immersive Virtual Reality System on Hand-Eye Coordination and Reaction Time in Young Musicians: A Pilot Study. Int. J. Environ. Res. Public Health 2021, 18, 1297. [Google Scholar] [CrossRef]
- Arroyo, A.; Periáñez, J.A.; Ríos-Lago, M.; Lubrini, G.; Andreo, J.; Benito-León, J.; Louis, E.D.; Romero, J.P. Components determining the slowness of information processing in Parkinson’s disease. Brain Behav. 2021, 11, e02031. [Google Scholar] [CrossRef] [PubMed]
- Arroyo-Ferrer, A.; Andreo, J.; Periáñez, J.A.; Ríos-Lago, M.; Lubrini, G.; Herreros-Rodríguez, J.; García-Caldentey, J.; Romero, J.P. Computerized Simple Reaction Time and Balance in Nondemented Parkinson’s Patients. Neurodegener. Dis. 2020, 20, 193–199. [Google Scholar] [CrossRef] [PubMed]
- Cieślik, B.; Mazurek, J.; Wrzeciono, A.; Maistrello, L.; Szczepańska-Gieracha, J.; Conte, P.; Kiper, P. Examining technology-assisted rehabilitation for older adults’ functional mobility: A network meta-analysis on efficacy and acceptability. Digit. Med. 2023, 6, 159. [Google Scholar] [CrossRef]
- Mazurek, J.; Cieślik, B.; Wrzeciono, A.; Gajda, R.; Szczepańska-Gieracha, J. Immersive Virtual Reality Therapy Is Supportive for Orthopedic Rehabilitation among the Elderly: A Randomized Controlled Trial. J. Clin. Med. 2023, 12, 7681. [Google Scholar] [CrossRef]
- Matys-Popielska, K.; Popielski, K.; Sibilska-Mroziewicz, A. Study of the Possibility of Using Virtual Reality Application in Rehabilitation among Elderly Post-Stroke Patients. Sensors 2024, 24, 2745. [Google Scholar] [CrossRef]
- Jansen, L.; de Zande, E.V.; de Korne, D.F.; Andringa, G. Feasibility of implementing immersive and non-interactive virtual reality interventions in elderly populations: A scoping review. Geriatr. Nurs. 2024, 61, 217–227. [Google Scholar] [CrossRef]


| Groups (N) | Age (Years) | Sex (Women/Men) | Weight (kg) | Height * (cm) | BMI (kg/m2) |
|---|---|---|---|---|---|
| All cases (38) | 87.2 (±6.3) | 29/9 | 68 (±14.5) | 157.4 (±10.2) | 27.7 (±6.4) |
| VR group (19) | 88.0 (±6.4) | 14/5 | 70.8 (±8.3) | 161.4 (±8.3) | 27.2 (±6.6) |
| Control group (19) | 86.4 (±6.3) | 15/4 | 65.1 (±12.2) | 153.5 (±10.6) | 28.2 (±6.4) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Grzywacz, Ż.; Jaśniewicz, J.; Koziarska, A.; Borzucka, D.; Majorczyk, E. Virtual Reality Gaming and Its Impact and Effectiveness in Improving Eye–Hand Coordination and Attention Concentration in the Oldest-Old Population. J. Clin. Med. 2025, 14, 4651. https://doi.org/10.3390/jcm14134651
Grzywacz Ż, Jaśniewicz J, Koziarska A, Borzucka D, Majorczyk E. Virtual Reality Gaming and Its Impact and Effectiveness in Improving Eye–Hand Coordination and Attention Concentration in the Oldest-Old Population. Journal of Clinical Medicine. 2025; 14(13):4651. https://doi.org/10.3390/jcm14134651
Chicago/Turabian StyleGrzywacz, Żaneta, Justyna Jaśniewicz, Anna Koziarska, Dorota Borzucka, and Edyta Majorczyk. 2025. "Virtual Reality Gaming and Its Impact and Effectiveness in Improving Eye–Hand Coordination and Attention Concentration in the Oldest-Old Population" Journal of Clinical Medicine 14, no. 13: 4651. https://doi.org/10.3390/jcm14134651
APA StyleGrzywacz, Ż., Jaśniewicz, J., Koziarska, A., Borzucka, D., & Majorczyk, E. (2025). Virtual Reality Gaming and Its Impact and Effectiveness in Improving Eye–Hand Coordination and Attention Concentration in the Oldest-Old Population. Journal of Clinical Medicine, 14(13), 4651. https://doi.org/10.3390/jcm14134651







